INTRODUCTION
Incidental durotomies are common intra-operative occurrences during spinal surgery, with a reported incidence ranging from 3 to 16 per cent.[1-3] Although most tears have no long-term sequelae and are easily sealed intra-operatively using sutures and/or patching substances such as fibrin glue[3, 4], a variety of intra-operative, postoperative, or long-term complications can occur. These include severe headache, persistent leak (duro-cutaneous fistula), pseudomeningocele formation, nerve root entrapment, meningitis, and arachnoiditis.[1, 3-6] Although some patients improve with bedrest, blood patches, or the placement of a subarachnoid drain, reoperation is occasionally required to repair the dura.
Many previous studies have been performed, examining various risk factors and treatment of unintended durotomy. They have suggested that these can occur irrespective of a surgeon's abilities or experience.[7] Studies have also suggested that unintended durotomies are associated with the age of the patient [8], the type of procedure performed[1, 9, 10], primary vs. revision surgery[3, 6, 8, 11], patient gender, experience level of the surgeon[7], and the presence of pre-existing conditions such as ossified posterior longitudinal ligament[6],diabetes, osteoporosis, arthritis[7] and ossification of the ligamenta flavum.[12] However, these studies are largely limited by study design, methodology, or sample size.
The purpose of the current study was to, use a prospectively collected data registry of more than 1500 patients to examine the rate of unintended durotomy during spine surgery, while determining the associated risk factors using univariate and multivariate log-binomial analysis. We hypothesized that increased surgical invasiveness, revision surgery, diabetes and age were significant risk factors for unintended durotomy during spine surgery.
MATERIALS and METHODS
Data Source
We examined prospective data from a cohort of patients undergoing spinal surgery between January 1st 2003 and December 31st 2004 at two academic hospitals: a university based medical center, and a hospital serving as the only Level I trauma center in a large multi-state area. All patients undergoing spine surgery during these two years were enrolled in the registry and were followed over a two-year period with IRB approval from the XXXX. Detailed information regarding patient demographics, medical co-morbidity, disease severity, surgical invasiveness, and adverse occurrences were recorded prospectively using previous published methods.[13, 14]
Surgical Invasiveness
The Surgical Invasiveness Index is a previously validated instrument that accounts for the number of levels decompressed, fused, or instrumented, posteriorly and anteriorly.[13, 14] It ranges from 0 to 48, with a higher score indicating greater invasiveness. The index is the sum of 6 weighted surgical components: anterior decompression (ad), anterior fusion (af), anterior instrumentation (ai), posterior decompression (pd), posterior fusion (pf), and posterior instrumentation (pi). The weights for each component represent the number of vertebral levels at which each component is performed [14]. For example, in a C5 – C6 anterior discectomy, with fusion and plating, the surgical invasiveness index is 5 [ad=1 (one disc) + af = 2 (two vertebrae fused) + ai = 2 (plating of 2 vertebrae)]. For our purpose, we categorized the score into six groups: 1-5, 6-10, 11-15, 16-20, 21-25, greater than 25.
Exclusion Criteria
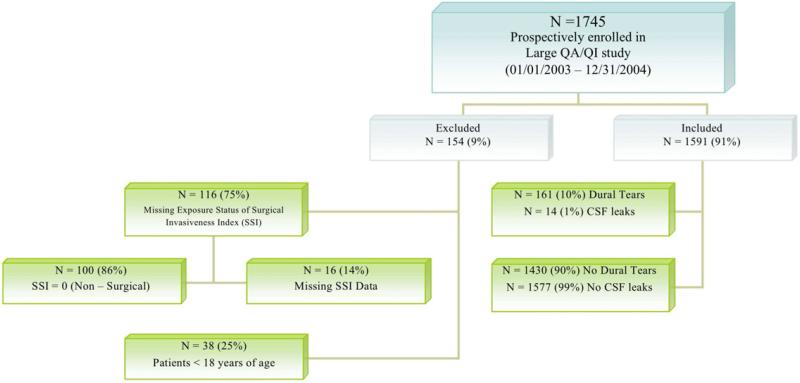
We excluded patients younger than 18 years of age and those with missing surgical invasiveness data. We also excluded patients whose surgical invasiveness index was either missing or equal to zero (closed casting, hardware removal, placement of halo) (Figure 1).
Figure.
Inclusion and Exclusion criteria
Dural Tear and Risk Factor Definitions
We defined “unintended dural opening” as an inadvertent opening of the dura during the procedure with CSF extravasation or bulging of the arachnoid layer. We defined “CSF leak” as the egress of CSF from the skin incision requiring additional treatment (Table 1). In trauma patients, dural tears secondary to trauma and not iatrogenic causes were not included in this analysis as they did not fit into the definition of “unintended dural opening”.
Table 1.
Dural Tears Adverse Occurrence (AO)
| Dural Tear Complications | Prevalence |
|---|---|
|
unintended dural opening The dura was inadvertently opened during the procedure, with CSF extravasation or bulging of the arachnoid layer. |
161 (10%) |
|
CSF leak The patient developed a leak of cerebrospinal fluid from the skin incision after the procedure, requiring additonal diagnostic tests, or requiring prolongation of wound care or bed rest or antibiotics, or requiring lumbar drain placement, or requiring repeat surgery. Criteria: (1) clear liquid draining from incision with beta-transferrin present in fluid or CSF symptoms (postural headache OR posterior neck pain or stiffness OR nausea OR photosensititivty OR visual symptoms OR tinnitus OR vertigo); AND (2) paraspinal spinal fluid collection on imaging studies; AND (3) requires treatment (bed rest, drain, or surgery). |
14 (0.88%) |
Risk factors assessed include age, gender, smoking status, alcohol abuse, drug use, diabetes, body mass index (BMI), medical co-morbidity (Charlson), previous spinal surgery, primary diagnosis (degenerative, trauma, neoplasm, other), level of surgery (cervical, thoracic, lumbosacral), surgical approach (anterior, posterior, combined).
The presence or absence of an unintended durotomy was prospectively recorded in all surgical spine patients from 2003-2004. However, some information about their risk factors, such as smoking status and alcohol use, were missing. On average per co-morbidity field, our registry was missing 7.43% of the data. We assumed that missing data on risk factors were not clinically significant and were therefore coded as “no” or “absent” for the risk. To test this assumption, we performed the analysis both with and without patients in whom data were missing and confirmed that the results and conclusions were unaffected. Therefore, we present our main findings including those who had missing risk factor data.
Statistical Analysis
Categorical data are presented as the number of cases and percentages. For categorical values, Pearson's Chi-square or Fisher's exact tests (where cell counts were low) were used to assess the effect of various risk factors. Relative risk (RR) and 95% confidence intervals (95% CI) were calculated for each of the categorical variables using univariate and multivariate log-binomial regression analysis. Stepwise multivariate log-binomial analysis was used to examine the association between risk factors and medical complication, adjusting for confounding risk factors. In the model we included risk factors that were deemed of clinical importance by the study investigators to contribute to SSI, were a known confounder, or had a univariate association of p < 0.10. Because surgical approach and the number of operated vertebral levels are a component of the invasiveness index, they were excluded from the multivariate model.
Statistical analysis was performed using SAS 9.2 software (SAS Inc., Cary, NC) with hypothesis testing using a 2-tailed test of significance and an alpha level of p< 0.05.
Source of Funding
The creation and maintenance of this registry was supported by grants from the NIH/NIAMS 5K23AR48979 and 5P60-AR48093 and supported in part by the Spine End-Results Research Fund at the University of Washington Medical Center through a gift from Synthes Spine (Paoli, PA)
RESULTS
Patient Characteristics
We identified 1745 patients from hospital admissions, pre-operative clinical visits, and/or surgical case logs for eligibility (Figure 1). Nine percent (154) were excluded. Of these, 116 (6.6%) had missing or zero invasiveness score and 38 were less than 18 years of age. Those with missing or invasiveness scores of zero had undergone casting, closed reduction, hardware removal, or percutaneous vertebral augmentation under general anesthesia.
The mean surgical invasiveness score was 8.4 (range, 1 – 48). Patients were mostly male (914/1591 -57%,) with a mean age of 49.5 years, a mean Charlson score of 1.2, and a mean BMI of 27.7 (table 2). Nearly two-thirds had a degenerative condition (991/1591 - 62%), followed by treatment for trauma (372/1591 -23%). Most of the operations were performed using a posterior approach (934/1591 - 59%), followed by a combined approach (365/1591 - 23%). The mean follow- up was 17.1 months (range, 0.43 – 65.5 months).
Table 2.
Univariate Analysis of Relative Risk for unintended durotomy during Spine Surgery
| Risk Factors | Dural Tear 161 (10%) | No Dural Tear 1430 (90%) | RR of Dural Tear | 95% CI | p-value |
|---|---|---|---|---|---|
| Length of Follow-Up1 (months), mean (sd) | 22.4 (19.0) | 16.5 (16.1) | |||
| Age (yr), mean (sd) | 54.6 (14.6) | 49.0 (16.0) | < 0.001* | ||
| 18 - 39 | 26 (6%) | 405 (94%) | 1.00 | - | 0.002* |
| 40 - 64 | 94 (11%) | 765 (89%) | 1.81 | 1.19 – 2.76 | |
| ≥65 | 41 (14%) | 260 (86%) | 2.26 | 1.41 – 3.61 | |
| Gender | |||||
| Male | 82 (9%) | 832 (91%) | 1.00 | - | 0.08 |
| Female | 79 (12%) | 598 (88%) | 1.30 | 0.97 – 1.74 | |
| Smoking | |||||
| No | 119 (11%) | 984 (89%) | 1.00 | - | 0.18 |
| Yes | 42 (9%) | 446 (91%) | 0.80 | 0.57 – 1.12 | |
| Alcohol | |||||
| No | 93 (10%) | 830 (90%) | 1.00 | - | 0.95 |
| Yes | 68 (10%) | 600 (90%) | 1.01 | 0.75 – 1.36 | |
| Drug Use | |||||
| No | 149 (10%) | 1275 (90%) | 1.00 | - | 0.18 |
| Yes | 12 (7%) | 155 (93%) | 0.69 | 0.39 – 1.21 | |
| Diabetes | |||||
| No | 134 (9%) | 1278 (91%) | 1.00 | - | 0.02* |
| Yes | 27 (15%) | 152 (85%) | 1.59 | 1.08 – 2.33 | |
| BMI | 28.5 (7.2) | 27.6 (6.4) | 0.13 | ||
| Underweight (< 18.5) | 10 (7%) | 130 (93%) | 1.00 | - | 0.47 |
| Normal (18.5 - < 25) | 47 (9%) | 463 (91%) | |||
| Overweight (25 - < 30) | 54 (11%) | 449 (89%) | 1.22 | 0.86 – 1.74 | |
| Obese (30 - < 35) | 28 (10%) | 240 (90%) | 1.19 | 0.78 – 1.83 | |
| ≥ 35 | 22 (13%) | 148 (87%) | 1.48 | 0.93 – 2.34 | |
| Charlson Comorbidity Adjusted for Diabetes, mean (sd) | 1.4 (1.7) | 1.2 (1.6) | 0.16 | ||
| 0 | 63 (9%) | 618 (91%) | 1.00 | - | 0.35 |
| 1 | 34 (10%) | 315 (90%) | 1.05 | 0.71 – 1.57 | |
| 2 | 25 (13%) | 169 (87%) | 1.39 | 0.90 – 2.15 | |
| 3 | 13 (10%) | 122 (90%) | 1.04 | 0.59 – 1.84 | |
| ≥ 4 | 22 (14%) | 138 (86%) | 1.49 | 0.94 – 2.34 | |
| Diagnosis Group | |||||
| Degenerative | 131 (13%) | 860 (87%) | 1.00 | - | < 0.001 |
| Trauma | 14 (4%) | 358 (96%) | 0.28 | 0.17 – 0.49 | |
| Neoplasm | 8 (7%) | 109 (93%) | 0.52 | 0.26 – 1.03 | |
| Infection | 6 (10%) | 53 (90%) | 1.30 | 0.60 – 2.82 | |
| Other | 2 (4%) | 50 (96%) | 0.29 | 0.07 – 1.14 | |
| Diagnosis Level | |||||
| Lumbosacral | 124 (16%) | 643 (84%) | 1.00 | - | < 0.001 |
| Cervical | 26 (4%) | 556 (96%) | 0.27 | 0.18 – 0.42 | |
| Thoracic | 11 (5%) | 229 (95%) | 0.28 | 0.16 – 0.52 | |
| Revision | |||||
| No | 99 (8%) | 1207 (92%) | 1.00 | - | < 0.001 |
| Yes | 62 (22%) | 223 (78%) | 2.87 | 2.15 – 3.84 | |
| Surgical Approach | |||||
| Posterior | 90 (10%) | 844 (90%) | 1.00 | - | < 0.001 |
| Anterior | 7 (2%) | 285 (98%) | 0.25 | 0.12 – 0.53 | |
| Combined | 64 (18%) | 301 (82%) | 1.82 | 1.35 – 2.45 | |
| Invasiveness Index, mean (sd) | 11.3 (9.9) | 8.2 (7.1) | < 0.001 | ||
| 1 - 5 | 65 (9%) | 668 (91%) | 1.00 | - | < 0.001 |
| 6 - 10 | 27 (7%) | 383 (93%) | 0.74 | 0.48 – 1.14 | |
| 11 – 15 | 28 (12%) | 212 (88%) | 1.32 | 0.87 – 2.00 | |
| 16 - 20 | 13 (14%) | 79 (86%) | 1.59 | 0.92 – 2.77 | |
| 21 - 25 | 9 (19%) | 38 (81%) | 2.16 | 1.15 – 4.06 | |
| > 25 | 19 (28%) | 50 (72%) | 3.11 | 1.98 – 4.86 | |
RR=Relative Risk, CI = confidence intervals
There were 161 (10%) unintended durotomies during the study period. Fourteen (0.9% of total, 8.7% of patients with unintended durotomy) developed leakage of CSF through the skin incision requiring additional treatment (Table 1).
The results of our univariate analysis are presented in Table 2 and suggest that age, diabetes, degenerative diagnosis, lumbar surgery, revision surgery and elevated surgical invasiveness are significant risk factors for unintended durotomy during spine surgery. The multivariate analysis results demonstrate that age, revision surgery, degenerative diagnosis, lumboar surgery and elevated surgical invasiveness are significant risk factors for unintended durotomy (Table 3). The strongest risk factor for unintended durotomy in the univariate and multivariate analysis was revision surgery (RR 2.21, CI 2.63 – 2.98).
TABLE 3.
Significant Risk Factors for Unintended Durotomy during spine spine surgery after step-wise multivariate log-binomial regression analysis
| RR | p | 95% CI | |
|---|---|---|---|
| Age 40-64 (ref age 18-40) | 1.67 | <0.016 | 1.12 – 2.59 |
| Age >65 (ref age 18-40) | 1.81 | <0.015 | 1.13 – 2.94 |
| Cervical surgery (ref: lumbar surgery) | 0.39 | <0.001 | 1.63 – 2.98 |
| Surgical Invasiveness (ref score 0-5) | 1.56 | <0.038 | 0.99 -2.34 |
| Revision (ref: primary) | 2.21 | <0.001 | 2.63 – 2.98 |
DISCUSSION
Unintended durotomy is a fairly common occurrence during spine surgery with a reported incidence ranging from 1% to 14%.[3, 6] Reported risk factors have included: revision surgery, ossification of the PLL, surgeon training and patient age, though these are inconsistently reported between studies. Revision surgery, based on literature review, is the most commonly reported risk factor. Although there are several studies that attempt to examine the incidence and associated risk factors, they are limited by small numbers, retrospective data collection and lack of multivariate analysis.
Khan, et al reported what appears to be the largest series of dural tears in the literature (10.6% of 3183 patients over a 10 year period).[1] Similarly, Cammisa et al reported a 3.1% incidence in 2144 patients[4] and Wang et al reported a 14% dural tear rate in 641 patients.[3] These three studies have large numbers and describe the treatment and sequelae of unintended durotomy. However, they are all retrospective studies with limited statistical analysis. In addition, risk factor assessment was largely qualitative and without statistical analysis.
Hamallah, et al retrospectively reviewed the medical records of 1994 patients and reported a 1% incidence of CSF leak after cervical spine surgery.[6] They did identify several risk factors with elevated relative risk values. However not all risk factors carried statistically significant confidence intervals. For example, they reported that patients with revision anterior surgery were 2.75 times more likely to have a CSF leak than those with primary anterior cervical surgery, but the 95% confidence intervals ranged from 0.85 to 8.93. They did identify male gender, and ossification of the posterior longitudinal ligament as statistically significant risk factors with valid confidence intervals. While this study did statistically assess the effect of potential risk factors, it appears to have utilized univariate and not multivariate analysis. Thus the potential confounding effect of other co-variates was not controlled for.
We found one prospective study specifically examining dural tears in our literature search. Tafazal and Sell reported on prospectively gathered data for 1549 cases across 14 institutions in the United Kingdom. They reported a 3.5% incidence for primary microdiscectomies and 13.2% for revision microdiscectomies. However the authors acknowledged that much of their data was “estimated” and that one participating surgeon freely admitted guessing.[11]
The XXXX Spine End Results Registry 2003-2004 is a prospective observational cohort of all patients undergoing spine surgery from Jan 1, 2003 to Dec 31, 2004. Detailed information regarding patient demographics, medical co-morbidity, disease severity, surgical invasiveness, and adverse occurrences were prospectively recorded.[13, 14]
The multivariate analysis of these data demonstrate that revision surgery, age, degenerative diagnosis, lumbosacral surgery and elevated surgical invasiveness were significant risk factors for unintended durotomy during spine surgery. Patients with revision surgery were 2.21 times more likely to have an unintended durotomy than patients undergoing primary spine surgery. Interestingly, the results of our univariate analysis suggests diabetes as a significant risk factor. Although this was not statistically demonstrated in the multivariate analysis (p<0.081; CI 0.94 – 1.98), this may gain statistical significance with a greater sample population. Age has been previously suggested to be a risk factor for unintended durotomy. Though the appearance of the dura was not recorded in our registry, it is our anecdotal observation that in elderly patients, the dura tends to have a more friable appearance and this may predispose it to unintended durotomy. Revision status has also been also been identified as a risk factor as scar tissue can obscure anatomy and dissection. We also reported a higher rate of unintended durotomy in the lumbar spine. This is not altogether surprising as in general, surgeons are more likely to manipulate and retract dura around the cauda equina instead of the spinal cord itself. Finally, elevated surgical invasiveness as a risk factor is somewhat intuitive. Clearly there is more exposure and likelihood for an unintended durotomy with a three level laminectomy compared to a microdiscectomy.
Although this study was a retrospective multivariate analysis of prospective data on 1591 patients, there are some weaknesses. In this registry of patients, many data points were recorded as categorical rather than continuous variables. Thus, the severity of potential co-variates was not assessed. For example, smoking history was recorded as “yes” or “no” without any mention of smoking rate or duration. Similarly, diabetes was recorded as “yes” or “no”. Average glucose and Hemoglobin A1c values were not recorded and severity of diabetes as a risk factor was not accounted for. Secondly, this was an observational study. Although there were a large number of trauma patients, the majority of these surgeries were elective. As such, patients with numerous co-morbidities may have been selected against for surgery, thus blunting the potential influence of these co-morbidities.
The major weakness of this study is that detailed information surrounding the actual unintended durotomy are lacking. At academic training institutions such as ours, attending surgeons are assisted by fellows, and residents with varying levels of surgical experience. Intuitively, the experience level of the surgeon seems likely to influence the rate of unintended durotomy. This analysis does not account for experience level of the surgeon at the moment of unintended durotomy. In addition, we did not prospectively record detailed information surrounding the CSF leak. Information regarding timing of CSF leak (during decompression or instrumentation) or the type of instrument associated with the dural tear is lacking in this data registry. Operative reports were retrospectively reviewed for assessment, however this information was not consistently available.
The present study, using multivariate analysis on a prospective cohort of 1591 patients demonstrates that revision surgery, age, degenerative diagnosis, lumbar surgery and elevated surgical invasiveness are significant risk factors with revision surgery being the strongest co-variate. This study also suggests that diabetes and age may be risk factors for unintended durotomy. These data can be utilized by clinicians for surgical decision-making and counseling patients on risks and complications.
Acknowledgments
Supported by grants from the NIH/NIAMS 5K23AR48979 and 5P60-AR48093 and supported in part by the Spine End-Results Research Fund at the University of Washington Medical Center through a gift from Synthes Spine (Paoli, PA)
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Khan MH, et al. Postoperative management protocol for incidental dural tears during degenerative lumbar spine surgery: a review of 3,183 consecutive degenerative lumbar cases. Spine (Phila Pa 1976) 2006;31(22):2609–13. doi: 10.1097/01.brs.0000241066.55849.41. [DOI] [PubMed] [Google Scholar]
- 2.Sin AH, et al. Predictive factors for dural tear and cerebrospinal fluid leakage in patients undergoing lumbar surgery. J Neurosurg Spine. 2006;5(3):224–7. doi: 10.3171/spi.2006.5.3.224. [DOI] [PubMed] [Google Scholar]
- 3.Wang JC, Bohlman HH, Riew KD. Dural tears secondary to operations on the lumbar spine. Management and results after a two-year-minimum follow-up of eighty-eight patients. J Bone Joint Surg Am. 1998;80(12):1728–32. doi: 10.2106/00004623-199812000-00002. [DOI] [PubMed] [Google Scholar]
- 4.Cammisa FP, Jr., et al. Incidental durotomy in spine surgery. Spine (Phila Pa 1976) 2000;25(20):2663–7. doi: 10.1097/00007632-200010150-00019. [DOI] [PubMed] [Google Scholar]
- 5.Brookfield K, et al. Delayed symptoms of cerebrospinal fluid leak following lumbar decompression. Orthopedics. 2008;31(8):816. [PubMed] [Google Scholar]
- 6.Hannallah D, et al. Cerebrospinal fluid leaks following cervical spine surgery. J Bone Joint Surg Am. 2008;90(5):1101–5. doi: 10.2106/JBJS.F.01114. [DOI] [PubMed] [Google Scholar]
- 7.Pechlivanis I, et al. Perioperative complication rate of lumbar disc microsurgery depending on the surgeon's level of training. Cen Eur Neurosurg. 2009;70(3):137–42. doi: 10.1055/s-0029-1216361. [DOI] [PubMed] [Google Scholar]
- 8.Jankowitz BT, et al. Effect of fibrin glue on the prevention of persistent cerebral spinal fluid leakage after incidental durotomy during lumbar spinal surgery. Eur Spine J. 2009;18(8):1169–74. doi: 10.1007/s00586-009-0928-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Stolke D, Sollmann WP, Seifert V. Intra- and postoperative complications in lumbar disc surgery. Spine (Phila Pa 1976) 1989;14(1):56–9. doi: 10.1097/00007632-198901000-00011. [DOI] [PubMed] [Google Scholar]
- 10.Teli M, et al. Higher risk of dural tears and recurrent herniation with lumbar micro-endoscopic discectomy. Eur Spine J. 19(3):443–50. doi: 10.1007/s00586-010-1290-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Tafazal SI, Sell PJ. Incidental durotomy in lumbar spine surgery: incidence and management. Eur Spine J. 2005;14(3):287–90. doi: 10.1007/s00586-004-0821-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Epstein NE. The frequency and etiology of intraoperative dural tears in 110 predominantly geriatric patients undergoing multilevel laminectomy with noninstrumented fusions. J Spinal Disord Tech. 2007;20(5):380–6. doi: 10.1097/BSD.0b013e31802dabd2. [DOI] [PubMed] [Google Scholar]
- 13.Mirza SK, et al. Towards standardized measurement of adverse events in spine surgery: conceptual model and pilot evaluation. BMC Musculoskelet Disord. 2006:53. doi: 10.1186/1471-2474-7-53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Mirza SK, et al. Development of an index to characterize the “invasiveness” of spine surgery: validation by comparison to blood loss and operative time. Spine (Phila Pa 1976) 2008;33(24):2651–61. doi: 10.1097/BRS.0b013e31818dad07. discussion 2662. [DOI] [PubMed] [Google Scholar]