Highlights
► Antigen-presenting cells (APCs) are important targets of filovirus infection in vivo. ► APCs are postulated to be major sites of virus replication and to promote inflammation. ► Understanding of filovirus–APC interactions will suggest novel therapeutic approaches. ► This review summarizes our current knowledge of filovirus–APC interactions.
Keywords: Filovirus, Ebola virus, Marburg virus, Antigen presenting cell, Macrophage, Dendritic cell, Interferon
Abstract
The filoviruses, Ebola virus (EBOV) and Marburg virus (MARV), are highly lethal zoonotic agents of concern as emerging pathogens and potential bioweapons. Antigen-presenting cells (APCs), particularly macrophages and dendritic cells, are targets of filovirus infection in vivo. Infection of these cell types has been proposed to contribute to the inflammation, activation of coagulation cascades and ineffective immune responses characteristic of filovirus hemorrhagic fever. However, many aspects of filovirus–APC interactions remain to be clarified. Among the unanswered questions: What determines the ability of filoviruses to replicate in different APC subsets? What are the cellular signaling pathways that sense infection and lead to production of copious quantities of cytokines, chemokines and tissue factor? What are the mechanisms by which innate antiviral responses are disabled by these viruses, and how may these mechanisms contribute to inadequate adaptive immunity? A better understanding of these issues will clarify the pathogenesis of filoviral hemorrhagic fever and provide new avenues for development of therapeutics.
1. Introduction
Filoviruses are enveloped, negative-sense RNA viruses most notable for their ability to cause severe, often lethal, infections in humans. Filoviruses are zoonotic pathogens that are likely use bats as reservoir hosts (Negredo et al., 2011, Towner et al., 2007). Infection in humans frequently results in filoviral hemorrhagic fever (FHF), a syndrome typically associated with an abrupt onset of fever, myalgias, headache, and gastrointestinal symptoms (reviewed in Kortepeter et al., 2011). A rash and changes in coagulation are common; bleeding is also frequently seen but is not a universal manifestation. Fatal outcomes correlate with increasing viremia over time and are associated with shock and disseminated intravascular coagulation (Geisbert and Hensley, 2004). Zoonotic pathogens, filoviruses have caused a number of outbreaks, some of which have been associated with fatality rates approaching 90 percent in confirmed cases (Sanchez et al., 2007). It is this lethality that makes filoviruses of concern as emerging pathogens and as potential bioweapons.
The filoviruses have been classified into two genera, the ebolaviruses and marburgviruses. Several species of EBOV have been identified, including Zaire Ebola virus (EBOV), Sudan virus (SUDV), Tai Forest (formerly Ivory Coast) virus (TAFV), Bundibugyo virus (BDBV) and Reston virus (RESTV). Only one species of MARV has been identified, although this is classified into two clades represented by Marburg virus (MARV) and Ravn virus (RAVV). A new filovirus, Lloviu virus (LLOV) has also been detected in bats and has been suggested to represent a new filovirus genus (Kuhn et al., 2010, Negredo et al., 2011). Among these viruses, there is variability in terms of virulence typically displayed in humans or animal models. Most notably, Reston virus has never caused a documented human death, despite confirmed exposures (http://www.who.int/mediacentre/factsheets/fs103/en/).
Fatal filovirus disease, which has been best studied in the context of Zaire EBOV infection, is characterized by a failure of the infected host to clear the infection, excessive host inflammation, activation of coagulation cascades and lymphocyte apoptosis (reviewed in Bray, 2005, Geisbert and Hensley, 2004). To develop effective countermeasures, a greater understanding is needed as to how these viruses trigger inflammatory responses and modulate both innate and adaptive immune responses such that virus infection is not controlled. This review will focus upon interactions of filoviruses with antigen-presenting cells (APCs), particularly macrophages and dendritic cells (DCs). These cells typically play central roles in the detection of invading pathogens and in the promotion of innate and adaptive immune responses. As is detailed below, macrophages and DCs are targets of filovirus infection in vivo. Their susceptibility and characteristic responses to infection have led to the proposals that these cell types play central roles in filoviral pathogenesis (Bray and Geisbert, 2005, Schnittler and Feldmann, 1998). However, many aspects of filovirus–APC interactions require additional study, and the contributions of specific APC cell types to viral pathogenesis remain incompletely defined.
2. Antigen-presenting cells
APCs are found throughout the body and serve as sentinels. They continuously sample the host environment for the presence of pathogens and present antigens to promote either tolerance or the induction of an adaptive immune response.
Phagocytic mononuclear cells (PMCs), also found throughout the body, can function as APCs, and these cells can be infected by filoviruses. Pathology tissue sections from EBOV-infected humans and non-human primates have consistently identified PMCs staining positive for EBOV antigen/nucleic acid (Connolly et al., 1999, Davis et al., 1997, Geisbert et al., 2003b, Geisbert et al., 2003c, Geisbert et al., 1992, Gibb et al., 2001, Ryabchikova et al., 1999, Wyers et al., 1999, Zaki et al., 1999). EBOV-infectable APCs (Table 1 ) can be broadly divided into three main types: monocytes, macrophages and DCs, each of which can be further subdivided. For example, DCs can be classified as conventional and plasmacytoid DCs (cDCs and pDCs). The criteria used to define monocytes, macrophages and DCs are in constant evolution (Randolph et al., 2008, Steinman and Idoyaga, 2010a, Steinman and Idoyaga, 2010b) and although various markers for PMCs have been identified, there is considerable overlap, in most, if not all of the markers used to identify each PMC subtype (Ferenbach and Hughes, 2008, Hume, 2008). However, typically, monocytes are identified as CD14+ blood-borne mononuclear cells (Gautier et al., 2009a) that can present antigen and also, especially under inflammatory conditions, enter tissues to differentiate into macrophages or dendritic cells (Geissmann et al., 2010, Randolph et al., 2008). Macrophages are considered highly phagocytic, contain a large number of lysosomes and vacuoles important for breaking down ingested antigens, are found mostly in tissues and can express cell surface CD14 as well as other receptors involved in phagocytosis (Table 1) (Geissmann et al., 2010, Steinman, 2011). On the other hand, cDCs express a large number of MHC II molecules, are considered relatively less phagocytic, but are highly stimulatory for T cells and can express several accessory and phagocytic receptors which are typically used to identify them. pDCs express the surface marker CD123, but not CD14, and when stimulated secrete copious amounts of type I interferon (see Table 1) (Colonna et al., 2004).
Table 1.
Antigen-presenting cells associated with filovirus infection.
| APC | Typical identifying markers2 | References |
|---|---|---|
| Monocytea | Blood borne phagocytic mononuclear cell, CD14+ | Gautier et al. (2009b) |
| Macrophagea | Phagocytic mononuclear cell, CD14+, MMR/CD206, CD68+ | Allavena et al., 2004, Morris et al., 2011, Robinson et al., 2006, Shabo and Svanvik, 2011 |
| Conventional dendritic cella | Phagocytic mononuclear cell, CD14-/lo, CD1b or c, BDCA-3, CD34+, DEC-205, Langerin | Crowley et al., 1989, Mortellaro et al., 2010, Piccioli et al., 2007, MacDonald et al., 2002) |
| Plasmacytoid dendritic cell | Phagocytic, mononuclear cell, CD14−, CD123+, BDCA-2, BDCA-4 | MacDonald et al. (2002) |
Infectable by EBOV.
Human markers.
The extent to which filovirus infection affects APC function has been a major area of interest. As part of their surveillance function, DCs and macrophages play a scavenger role by eliminating antigens such as unwanted dysfunctional cells. These innocuous antigens are then presented by the scavenger APC to induce specific T cell tolerance to that antigen. Potential pathogens are identified by APCs via cell-encoded pattern recognition receptors (PRRs) of the Toll-like receptor (TLR), RIG-I-like receptor and NOD-like receptor families (Baum and Garcia-Sastre, 2010, Janeway and Medzhitov, 2002, Medzhitov et al., 1997). For example, TLR3 and RIG-I can respond to products of virus replication, such as dsRNA and 5′-triphosphate containing RNAs, respectively. This engagement of APC PRRs leads to their activation. When activated by inflammatory signals such as those induced from inflammatory cytokine receptors or PRRs, macrophages and DCs differentiate into immune effectors with somewhat different roles. In general, both cell types secrete inflammatory cytokines further increasing the inflammatory response, but macrophages become better at killing endocytosed pathogens, while DCs become potent stimulators of the adaptive immune responses such as CD8 killer T cell responses (Doherty and Zinkernagel, 1975).
3. Viruses and virus-like particles
Because of their extreme lethality, filoviruses require biosafety level 4 (BSL4) containment, hampering the study of live viruses. Virus-like particles (VLPs) can be generated experimentally and can serve as surrogates for replication competent viruses, allowing the study of several aspects of the virus replication cycle, including virus assembly, release and entry into target cells. In their most basic form, filoviral VLPs can be generated by the expression in mammalian cells of the filoviral matrix protein VP40. VP40 expressed in this manner buds from the plasma membrane in the form of filamentous membrane-bound virus-like particles (VLPs) (Bavari et al., 2002, Jasenosky et al., 2001, Noda et al., 2002, Swenson et al., 2004, Watanabe et al., 2004). Co-expression of the filoviral membrane-associated glycoprotein (GP) results in incorporation of GP into the VLPs, enhances budding of VP40 and increases VLP formation (Bavari et al., 2002).
VLPs that contain only VP40 do not readily infect cells, because they lack the viral attachment protein, GP. However, VLPs possessing both VP40 and GP can bind to and infect permissive cells, including macrophages and DCs (Martinez et al., 2010). VLPs can therefore be used to model the earliest interactions between filoviruses and host cells. Filovirus VLPs have been found to elicit APC responses and also have proven effective as vaccines in animal models. VLPs can also elicit, when given only 1–3 days prior to infection with mouse-adapted EBOV, natural killer cell responses that protect mice from lethal challenge (reviewed in Warfield and Aman, 2011). Therefore, the specific interaction of filoviral VLPs with APCs has been of interest and will be discussed alongside interactions of replication-competent filoviruses in this review.
4. Macrophages and DCs are targets of filovirus infection in vivo
As indicated above, in vivo filovirus infection of macrophages has been demonstrated in a number of studies that have examined post-mortem tissues from human victims or tissues from experimentally-infected rodents and non-human primates (Connolly et al., 1999, Davis et al., 1997, Geisbert et al., 2003b, Geisbert et al., 2003c, Geisbert et al., 1992, Gibb et al., 2001, Ryabchikova et al., 1999, Wyers et al., 1999, Zaki et al., 1999) (Table 1). Of course, as has been noted by other authors, the presence of viral antigen or nucleic acid in cells does not necessarily indicate that the cells are productively infected such that they produce new infectious virus particles (Bradfute and Bavari, 2011). It should be possible to resolve this gap in knowledge; for example, one could isolate infected macrophages and DCs from infected animals and incubate the cells ex vivo to determine whether they produce new infectious virus. Even lacking this information, the prominence of macrophage infection in vivo and the ability of these cells to support virus replication in vitro (discussed below), clearly justifies studies to characterize in detail macrophage-filovirus infection. Similarly, in the case of DCs, while infection has been demonstrated in experimentally infected NHPs (Geisbert et al., 2003b), additional studies are needed to define the frequency of DC infection and the impact of infection on DC function in vivo.
5. Productive replication of filoviruses in macrophages and conventional DCs
Substantial data indicate that macrophages and conventional DCs support the productive replication of filoviruses. For example, Feldmann et al. isolated adherent cells from human PBMCs and grew these for 7 days until they acquired a macrophage-like morphology. These cells, which stained positively with anti-CD14 antibody, were productively infected by MARV, and the infection stimulated TNFα release from these cells (Feldmann et al., 1996). A separate study supports the view that adherent macrophages are productively infected by multiple different filoviruses, including MARV, ZEBOV and REBOV (Stroher et al., 2001). Interestingly, the same study found that freshly isolated non-adherent monocytes were also productively infected (Stroher et al., 2001). This observation contrasts with other studies, described below, indicating that monocytes are relatively resistant to EBOV entry. In the studyby Stroher et al., infections were performed at high multiplicity (MOI = 10), and the monocytes were washed after infection. On day 2 post-infection, significant viral antigen was detected in the cells and productive virus replication was demonstrated with kinetics of growth similar in both macrophages and monocytes, supporting the view that monocytes are infectable (Stroher et al., 2001). Previous studies have demonstrated that plated monocytes can slowly and spontaneously differentiate into macrophages in culture (Bennett and Cohn, 1966, Johnson et al., 1977, Zuckerman et al., 1979). Monocyte infection by filoviruses might also accelerate differentiation towards a macrophage phenotype, for example by triggering the secretion of inflammatory cytokines. However, the inoculum in the former study was washed from the cells. Given the somewhat contradictory state of the literature on infection of monocytes and the prominent role of APCs during infection, it would be worth revisiting whether or not monocytes are less permissive for filovirus infection than other APCs.
The permissiveness of primary human monocyte-derived DCs for EBOV infection in vitro has now been demonstrated in several studies (Bosio et al., 2003, Mahanty et al., 2003, Martinez et al., 2010). Interestingly, the infected cells exhibited relatively little cell death over six days of infection (Mahanty et al., 2003). This sustained ability to survive while infected could offer the virus opportunities to disseminate in vivo.
An interesting question is whether the efficiency of infection or replication within APCs or other cell types by a particular filovirus is related to the capacity of that virus to cause lethal disease. Different filoviruses can exhibit significant differences in their relative replication rates in cell culture. For example, RESTV, which appears to be attenuated for humans, exhibits delayed replication kinetics in Vero cells as compared to EBOV. BEBOV, which has been associated with lower lethality in humans, replicates productively in primary human macrophages (Gupta et al., 2010). However, relative to EBOV, BDBV replicated more slowly, induced lower levels of cytokines and induced less apoptosis. In mice or guinea pigs, EBOV is not lethal unless it possesses adaptive genetic changes that can be acquired by serial passage in this species (Bray et al., 1999, Ebihara et al., 2006). These adaptive changes confer enhanced ability of these viruses to replicate in the macrophages of the appropriate species (mouse or guinea pig) (Ebihara et al., 2005, Mateo et al., 2011). It would therefore be of interest to systematically examine in the macrophages and DCs of human or non-human primate origin replication rates of filoviruses with different virulence potentials.
It should be noted that not all DCs are readily infected by filoviruses. In one interesting example, plasmacytoid DCs, purified from human blood were not readily infected by ZEBOV and western blotting with polyclonal anti-EBOV sera did not detect viral protein expression (Leung et al., 2011a). In contrast, the same sera readily detected viral antigen in monocyte-derived DCs infected with ZEBOV. As noted earlier, the relative permissiveness of monocytes for filovirus entry has also been questioned.
6. Filovirus entry into APCs
One aspect of virus-host interactions that appears to contribute to tropism toward specific types of APCs is the viral entry process. A general view of filoviral entry has been developed. Briefly, filovirus entry is mediated by the viral surface glycoprotein (GP) (Bar et al., 2006), a type I transmembrane protein cleaved by furin proteases into GP1 and GP2 subunits (Neumann et al., 2002, Neumann et al., 2007, Volchkov et al., 1998, Wool-Lewis and Bates, 1999). An N-terminal region of GP1 (residues 57–149) has been defined as a receptor-binding domain (Dube et al., 2009, Kaletsky et al., 2007, Kuhn et al., 2006, Lee and Saphire, 2009), while GP2 contains the hydrophobic fusion peptide and heptad repeats that mediate viral membrane fusion (Ito et al., 1999, Watanabe et al., 2000, Weissenhorn et al., 1998). Both subunits contain multiple N-linked glycans, and the C-terminal mucin-like domain in GP1 is extensively modified with O-linked glycans.
Following attachment to host cells, EBOV particles undergo endocytosis (Bar et al., 2006). Although different endocytic pathway(s) have been implicated in EBOV entry, including entry via clathrin-coated pits and caveolae, recent studies support macropinocytosis as important for filovirus entry (Bhattacharyya et al., 2010, Chandran et al., 2005, Empig and Goldsmith, 2002, Mulherkar et al., 2011, Nanbo et al., 2010, Saeed et al., 2010). Internalized virus eventually localizes to acidified endosomes containing activated cysteine protease cathepsins L (Cat L) and B (Cat B) (Aleksandrowicz et al., 2011, Chandran et al., 2005, Kaletsky et al., 2007, Schornberg et al., 2006). These enzymes cleave GP, priming it for the conformational changes that will fuse viral and endosomal membranes (Chandran et al., 2005, Dube et al., 2009, Kaletsky et al., 2007, Schornberg et al., 2006, Wong et al., 2010). Cleavage also makes GP competent to interact with the essential host entry factor Niemann-Pick type C 1 protein (NPC-1) (Carette et al., 2011, Cote et al., 2011). A putative fusion peptide located at residues 524–539 within GP2 has been identified and is important for viral-host cell membrane fusion (Ito et al., 1999). While low pH and cathepsin cleavage are required for fusion to occur, neither alone is sufficient to trigger fusion (Bale et al., 2011).
Many cellular factors have been implicated as potential receptors for the virus, some of which likely function as attachment factors while others may be required for subsequent steps (Table 2 ). Cell surface lectins are potential attachment factors that may contribute to efficient infection of macrophages and DCs, as some are highly expressed on these cells (Bosio et al., 2003, Geisbert et al., 2003b, Geisbert et al., 1992, Schnittler and Feldmann, 1998). For example, the C-type lectin DC-SIGN is expressed on DCs, subsets of macrophages and other cell types. DC-SIGN and the related DC-SIGNR can bind, likely through high mannose carbohydrates on GP, EBOV and MARV GP and promote infection (Lin et al., 2003, Marzi et al., 2007, Simmons et al., 2003). Other C-type lectins may also contribute to virus entry. For example, human macrophage galactose- and N-acetylgalactosamine-specific C-type lectin (hMGL), which is also present on macrophages and DCs, was also shown to promote EBOV infection (Takada et al., 2004). hMGL interaction with GP requires the GP mucin-like domain, however the mucin-like domain is not required for viral entry (Hood et al., 2010, Kaletsky et al., 2007). LSectin is another lectin that can bind GP, although its specificity is for N-acetyl-glucosamine (Dominguez-Soto et al., 2007, Gramberg et al., 2005, Gramberg et al., 2008). How the abundance of these various factors influences permissiveness of specific cell types, including macrophages and DCs, remains to be fully evaluated.
Table 2.
Filovirus receptors and attachment factors reported in the literature.
| Identified receptor/attachment factor for filovirus | Assay type (pseudotype/filovirus) and target cell | Reference |
|---|---|---|
| Human macrophage galactose and N-acetylgalactosamine C-type lectin (hMGL) | VSV pseudotyped with Ebola GP/K562 cells; Ebola Zaire virus /K562 cells transfected with hMGL | Takada et al. (2004) |
| DC-SIGN/L-SIGN |
|
Alvarez et al. (2002), Lin et al. (2003) |
| LSECtin |
|
Dominguez-Soto et al., 2007, Gramberg et al., 2005, Gramberg et al., 2008 |
| Beta-integrin | VSV pseudotyped with Ebola GP/293 cells | Takada et al. (2000) |
| T-cell immunoglobulin and mucin domain 1 (TIM-1) | VSV pseudotyped with Ebola or Marburg GP/Vero cells, 293T cells expressing TIM-1, renal epithelial cell lines, HuH-7 | Kondratowicz et al. (2011) |
| Folate receptor alpha | HIV pseudotyped with Ebola or Marburg GP/Jurkat cells expressing the folate receptor alpha; Ebola Zaire virus/Jurkat cells overexpressing Folate receptor alpha | Chan et al. (2001) |
| Tyro3 family members | MLV and VSV pseudotyped with Ebola or Marburg GP/Jurkat cells | Shimojima et al. (2006) |
| Niemann-Pick disease type C 1 protein (NPC-1) |
|
Carette et al., 2011, Cote et al., 2011 |
Other receptors and entry factors might also contribute to APC infection. T cell immunoglobulin mucin-1 (TIM-1), a recently discovered receptor for EBOV entry, is expressed on some, but not all permissive cells (Kondratowicz et al., 2011). TIM-1 is part of a family of TIM proteins that regulate T cell activation, tolerance and removal of apoptotic cells (Kobayashi et al., 2007, Rodriguez-Manzanet et al., 2009). Interestingly, TIM-1 is not expressed at appreciable levels on macrophages, but may be expressed on DCs (Kobayashi et al., 2007, Xiao et al., 2011). In contrast, a related protein, TIM-4, is expressed on DCs and macrophages (Kobayashi et al., 2007). Both TIM-1 and TIM-4 can bind phosphatidylserine, allowing them to interact with apoptotic bodies (Kuchroo et al., 2008). Given the functional and structural similarity between TIM-1 and TIM-4 and the presence of cell-surface TIM-4 on macrophages, TIM-4 is also a candidate EBOV entry factor for APCs.
As noted above, NPC-1 has also been demonstrated to be a host factor required for filovirus entry. Although NPC-1 is ubiquitously expressed, NPC-1 is expressed at different levels in different tissues, with high expression in the liver (Garver et al., 2005). Therefore, it is possible that expression levels may influence tropism of filoviruses toward different tissues or cells types. Questions that might be asked in this regard include whether different stimuli can change NPC-1 levels in APCs, whether such changes affect filovirus entry efficiency and how well NPC-1 levels correlate with filovirus tropism in vivo.
As noted earlier, some studies suggest that EBOV replicates in both monocytes and macrophages (Stroher et al., 2001), and studies using GP-pseudotyped lentiviruses suggest that primary human monocytes are significantly less permissive for GP-mediated entry than are primary human macrophages (Yonezawa et al., 2005). Similar results have been obtained when EBOV VLPs are used to infect monocytes or DCs (Martinez and Basler, unpublished observation). This may be due to a difference in binding of virus to a cell surface receptor, since the human monocytic line THP-1 was found to bind the EBOV GP receptor-binding domain (RBD) with lower efficiency as compared to differentiated THP-1 cells which exhibit a macrophage-like phenotype (Dube et al., 2008). Enhanced infection of the macrophage-like cells was associated with increased adherence of the cells to a substrate, a property acquired as monocytes differentiate to macrophages. A number of non-adherent cells were found to be incompetent for GP-mediated entry, however, adherence correlates with permissiveness for entry (Dube et al., 2008). In 293F cells, adherence also results in the upregulation of an RBD-binding activity on the cell surface (Dube et al., 2010). The identity of this RBD-binding factor and its relationship for the permissiveness of monocytes versus macrophages for filovirus infection will be of interest.
The preferential tropism of EBOVs for macrophages and DCs versus monocytes may have important implications on the pathogenesis of infection. Circulating monocytes attracted by chemokines to a focus of inflammation will extravasate from the blood into the inflamed tissue. Once in the tissue, monocytes would likely differentiate into either macrophages or DCs enabling more efficient infection by EBOV. It would therefore be important to determine whether inhibiting the differentiation, trafficking or development of monocytes would impact the pathogenesis of EBOV infection.
The apparent block to ZEBOV replication in plasmacytoid DCs (pDCs) also appears to be at the level of cell entry (Leung et al., 2011a). This also has implications for viral pathogenesis because pDCs have the capacity to produce large amounts of the antiviral cytokine IFNα in response to infection (Reizis et al., 2011). That there was a block to infection was, in fact, first suggested by the observation that addition of infectious Zaire EBOV to primary pDCs purified from human blood did not induce enhanced IFNα production (Leung et al., 2011a). Experiments comparing viral protein synthesis in cDCs versus pDCs then demonstrated robust viral protein production in the conventional DCs, but no newly synthesized viral protein was detected by western blot in the virus-exposed pDCs. Entry assays, performed with EBOV virus-like particles, indicated that EBOV GP is unable to successfully mediate entry into pDCs, although binding of the EBOV VLPs to the surface of cDCs and pDCs was comparable (Leung et al., 2011a). This suggests that the resistance to infection is downstream of cell surface binding. Perhaps strategies could be identified that would overcome this block, resulting in enhanced IFNα production and suppression of virus replication.
7. Consequences of APC infection with filoviruses
Given that macrophages and DCs are major targets of filoviruses in vivo, and that these cells normally function in defense against pathogens, understanding how these cells respond to filovirus infection is of obvious interest.
7.1. Macrophage and monocyte responses
Infection of monocytes or macrophages with replication competent EBOV or MARV results in cytokine and chemokine production as early as 3–6 h post-infection (Gupta et al., 2001, Hensley et al., 2002, Stroher et al., 2001). Inactivated viruses also induce cytokines/chemokines ((Hensley et al., 2002, Stroher et al., 2001). Recent microarray analyses confirm and expand upon these observations, demonstrating the early upregulation of 88 cellular genes in primary human macrophages in the first six hours after infection (Wahl-Jensen et al., 2011). Among the upregulated genes were inflammatory cytokines including chemokines. Ebola virus-like particles (VLPs) elicited similar responses to live virus, providing the VLPs possessed GP (Stroher et al., 2001, Wahl-Jensen et al., 2011). Therefore, these early macrophage proinflammatory responses do not require virus replication but do require GP, although the mechanism by which GP exerts these effects is not well defined. In contrast, sustained cytokine production (over the course of 48 h and longer) only occurs with live virus infection, suggesting that this sustained response requires virus replication (Gupta et al., 2001, Hensley et al., 2002). Interestingly, most in vitro studies of EBOV-infected monocytes, macrophages or PBMC report little IFNαβ response in the infected cultures (Gupta et al., 2001, Stroher et al., 2001). Even in the one study in which significant IFNα was present, viral titers increased significantly after IFNα was detected (Hensley et al., 2002). This suggests a model in which filoviruses effectively counter antiviral innate immunity by suppressing the IFNαβ responses. As discussed below, this suppression occurs both at the level of IFNαβ production as well as cellular responses to exogenous IFNs. This would allow sustained replication in macrophages, resulting in ongoing secretion of chemokines and cytokines.
Because the in vitro cytokine response of macrophages correlates with in vivo manifestations of infection, where macrophages are major targets of infection and disease is characterized by excessive cytokine responses, it has been proposed that macrophages are major sources of inflammatory responses in filoviral HF (Bray and Geisbert, 2005). To evaluate this model directly, additional in vitro, ex vivo and in vivo studies could be performed. For example, few studies examining macrophage cytokine responses to infection have determined what percentage of cells are infected at different time points post infection, and studies to determine whether the cells that are actually infected are the major source of cytokines have not been published. Given that either virus or VLPs trigger rapid cytokine responses that could activate nearby cells, bystander effects of infection could significantly contribute to the inflammatory response. Specific cell types in infected animals could be characterized in more detail to define whether macrophages are in fact major sources of cytokines in vivo. Whether other cell types also contribute to the overall response in vivo and whether the cytokine-producing cells are infected, as indicated by the presence of viral nucleic acid or viral antigen, could also be determined.
EBOV infection is associated with disseminated intravascular coagulation (DIC), a syndrome in which coagulation is activated in a manner that leads to consumption of coagulation factors, production of microthrombi and ultimately to bleeding (Levi and Ten Cate, 1999). Tissue factor (TF) is a member of the cytokine receptor family that activates coagulation cascades during DIC (Levi and Ten Cate, 1999, Ruf, 2004). Studies in NHPs demonstrated coagulation abnormalities and fibrin deposition, which occurs due to activation of coagulation, during the course of EBOV infection (Geisbert et al., 2003c). Fibrin deposition was associated histologically with monocytes/macrophages in the tissues of infected animals. TF mRNA and protein were also associated with infected PBMCs and with macrophages in infected tissues. In vitro, monocytes and macrophages also produced TF mRNA and protein following infection with EBOV Treatments designed to either block TF function or otherwise reduce coagulation have therapeutic benefit in infected NHPs, demonstrating the importance of this pathway for pathogenesis (Geisbert et al., 2003a, Hensley et al., 2007). There are multiple mechanisms by which TF expression can be upregulated, including by cytokines, but the available data suggest upregulation is induced directly by EBOV infection (Geisbert et al., 2003c). As with cytokine studies, it would be of interest to define the mechanisms by which filoviruses trigger TF expression. Such studies may suggest new strategies to reduce DIC during infection.
7.2. DC responses
Some studies suggest a different outcome for infection of DCs as compared to macrophages. For example, in a study by Hensley et al., little inflammatory cytokine secretion was detected following EBOV-infection of DCs whereas an EBOV-infected mixed monocyte/macrophage cell culture produced significant levels of cytokines (Hensley et al., 2002). Although both DC and macrophage/monocyte APCs are productively infected by EBOV, this study reveals an intriguing difference in the DC versus macrophage responses to infection. In studies that examined DC function following ZEBOV infection, the virus induced relatively little cytokine production and little to no IFNαβ (Bosio et al., 2003, Mahanty et al., 2003). Instead of effectively activating DCs, EBOV infection induced “aberrant” DC maturation, evidenced by upregulation of cell surface CD40 and CD80, only small increases in CD86 and HLA-DR, an absence of CD11c and CD83 upregulation and a failure to decrease CCR5 (Bosio et al., 2003). EBOV infection also inhibited the ability of DCs to stimulate T cell proliferation (Bosio et al., 2003, Mahanty et al., 2003). Based on these observations, it has been argued that EBOV suppression of DC function prevents initiation of adaptive immune responses and facilitates uncontrolled, systemic virus replication (Bray and Geisbert, 2005).
7.3. Activation of macrophages and DCs by VLPs
As noted above, filoviral VLPs possessing the GP and VP40 can be used to assess the earliest interactions of cells and virus. The infection of macrophages with ZEBOV VLPs results in upregulation of a number of cellular genes including genes for chemokines and cytokines produced during ZEBOV infection in vivo (Wahl-Jensen et al., 2011, Wahl-Jensen et al., 2005a). Several studies demonstrate that ZEBOV VLPs efficiently stimulate DCs to secrete inflammatory cytokines such as IL-6, IL-10, macrophage inflammatory protein (MIP)-1, TNF-alpha, IL-8, IL-6 and IL-12 and to upregulate MHC I, MHC II, CD86, CD80 and stimulating T cells (Bosio et al., 2004, Martinez et al., 2007, Warfield et al., 2003, Warfield et al., 2007, Ye et al., 2006). The presence of EBOV GP on the VLPs is important for the DC response, as VLPs made by expressing VP40 alone do not stimulate DCs (Bosio et al., 2004, Martinez et al., 2007, Wahl-Jensen et al., 2011, Ye et al., 2006). VLPs have been demonstrated to stimulate the MAPK and NF-κB signaling pathways as well as cytokine secretion from DCs, and this requires the highly glycosylated mucin-like domain of GP (Martinez et al., 2007, Okumura et al., 2010). Taken together, these studies suggest that EBOV GP is sufficient to elicit the activation of DCs, and this may promote the efficacy of VLPs as vaccines. This type of response, however, differs from the situation with actual virus, which, as described above, does not stimulate DCs effectively. The implication is that virus replication results in production of factors that suppress DC maturation and function. Interestingly, inactivated EBOV also did not stimulate sustained macrophage or DC cytokine secretion, and did not upregulate costimulatory marker upregulation in DCs and did not stimulate DCs to activate T cells (Bosio et al., 2003, Gupta et al., 2001, Hensley et al., 2002, Mahanty et al., 2003). EBOV particles inactivated with gamma irradiation possess additional components, including RNA and several viral proteins that are not present in VLPs. Whether particular components of the inactivated virus particle arrest DC stimulation remains to be determined. It will also be important to determine whether inactivated virus and VLPs have comparable efficiencies of entry. Whether differences in the content of cellular factors present in VLPs and inactivated virus might account for differences in cellular responses is also of interest.
The mechanisms by which macrophages and DCs recognize and respond to VLPs and virus remain to be fully defined. Pattern recognition receptors respond to pathogen associated molecular patterns (PAMPs) and damage-associated molecular patterns (DAMPs) and activate cellular responses to these stimuli. Defining VLP and filovirus-associated PAMPs, the PRRs that recognize them and signaling pathways modulated by them will provide insight into mechanisms which influence VLP vaccine efficacy and may suggest ways to modulate host responses so as to mitigate the impact of virus infection in vivo.
GP is required for macrophage and DC responses to VLPs, and removal from GP of the heavily glycosylated mucin-like domain from GP significantly attenuated DC responses to VLPs, despite the fact that the mucin-deleted GP still mediates efficient entry into cells (Martinez et al., 2007, Wahl-Jensen et al., 2011). The responses elicited include cytokine and chemokine secretion, activation of MAP kinase and NF-κB signaling pathways and activation of a number of cellular transcription factors (Martinez et al., 2007). The fact that the mucin domain is required for activation of MAP kinase and NF-κB signaling but not for entry suggests that it is not the entry process itself that triggers signaling. Rather GP is somehow involved, either directly or indirectly, in triggering the host cell responses.
GP has pleiotropic effects on host cells which might contribute to the effects of virus and VLPs on macrophage and DC function. These include the induction of MAPK and other signaling pathways (Martinez et al., 2007, Zampieri et al., 2007). GP also masks surface molecules, including class I MHC and beta integrins, which may influence the ability of infected cells to trigger immune responses (Simmons et al., 2002; Reynard et al., 2009; Francica et al., 2010, Takada et al., 2000). GP also promotes the cell-rounding, detachment, and eventual cytotoxicity in certain adherent cell types (Francica et al., 2009, Ray et al., 2004, Sullivan et al., 2005, Yang et al., 2000). Importantly, GP was demonstrated to activate an NF-κB-responsive reporter gene in HEK293 cells expressing TLR4, but not cells lacking TLR4; the TLR4-dependent response was dependent upon the mucin-like domain (Okumura et al., 2010). Induction of cytokine and IFNβ mRNA in the human monocytic cell line THP-1 was also dependent upon the presence of the mucin-like domain. Consistent with a model in which GP activates TLR4, the two proteins can be co-immunoprecipitated (Okumura et al., 2010). These data point to TLR4 as a PRR for detection of filovirus GP, although a role for other PRRs in the APC response to VLPs has not been excluded. It would be of interest to determine the response of TLR4-deficient macrophages and DCs to VLPs and filovirus infection. In vivo studies examining the interaction of TLR4-deficient mice to VLP vaccination and filovirus infection will also be of interest.
8. Filoviruses counter the innate antiviral IFN response
A number of studies have documented the relative lack of IFNαβ production by infected macrophages, DCs and other cells (Bosio et al., 2003, Gupta et al., 2001, Harcourt et al., 1998, Hartman et al., 2008b, Mahanty et al., 2003). The absence of IFNαβ production and the ability of filoviruses to also block cellular responses to exogenously added IFNαβ likely helps to sustain virus replication in these cells, promoting cytokine secretion by macrophages. Because the cellular signaling pathways that trigger IFNαβ production and the pathways activated by exogenously added IFNαβ have each been implicated in DC maturation, the filoviral mechanisms that block these pathways could contribute to the inhibition of DC maturation and function, thereby promoting suppression of adaptive immune responses.
Normally, production of IFNαβ by these APCs and the subsequent induction of interferon stimulated genes (ISGs) are typical early responses to viral infection. Recognition of the single-stranded RNA genomes of negative-stranded viruses, such as those of filoviruses, can be mediated by TLRs in the plasma membrane or endosomes, or by RIG-I like receptors (RLRs) in the cytosol, which detect the viral RNA produced after virus entry and replication (reviewed in Baum and Garcia-Sastre, 2010). These independent pathways result both in the phosphorylation and activation of the transcription factors IRF3 and/or IRF7, which in combination with other transcription factors create a transcription complex that binds to IFNαβ gene promoters and leads to IFNαβ expression. In the case of negative-strand RNA virus infection of cDCs, IFN production is currently thought to result largely from the recognition of cytosolic viral RNA by RIG-I, ultimately leading to the activation of TBK1/IKKε. These kinases in turn phosphorylate the transcription factor IRF3 and/or IRF7.
9. Filovirus VP35 inhibits IFN production
Cells infected with wild-type EBOV or MARV do not exhibit upregulated expression of IFN-inducible genes (Hartman et al., 2008b, Kash et al., 2006). This can be accounted for, at least in part, by the fact that filoviruses interfere with cellular IFNαβ production through the function of their VP35 protein (Basler et al., 2003, Basler et al., 2000, Gupta et al., 2001, Harcourt et al., 1998, Hartman et al., 2008a). VP35 is a multifunctional viral protein, which in addition to acting as an IFN-antagonist, plays roles as a structural protein and as an essential component of the viral RNA polymerase complex, where it interacts with the viral nucleoprotein and the catalytic subunit of the viral polymerase, the L protein (reviewed in Basler and Amarasinghe, 2009). Several mechanisms have been identified by which VP35 can inhibit induction of IFNαβ responses. VP35 has been demonstrated to inhibit the RIG-I signaling pathway (Cardenas et al., 2006). The RIG-I pathway plays a critical role in inducing IFNαβ production in response to a number of RNA viruses and can be activated by RNA extracted from EBOV-infected cells, suggesting its relevance to EBOV infection (Habjan et al., 2008). Inhibition of RIG-I would prevent activation of IRF-3 and impair induction of IFNαβ gene transcription (Basler et al., 2003, Basler et al., 2000, Cardenas et al., 2006, Hartman et al., 2008a). In addition, VP35 has been demonstrated to interact with the kinases IKKε and TBK1, which lie downstream of RIG-I and are required for IRF-3 activation in most cells. This interaction can disrupt kinase-IRF-3 or IRF-7 interaction, and prevent the phosphorylation required to activate the transcription factors (Prins et al., 2009). In addition, VP35 has been found to promote SUMOylation of IRF-7, impairing its ability to stimulate transcription (Chang et al., 2009). Finally, VP35 is a dsRNA binding protein, and the ability of VP35 to bind dsRNA appears to be required for its full anti-IFNαβ function (Cardenas et al., 2006, Kimberlin et al., 2010, Leung et al., 2009, Leung et al., 2010). Specifically, point mutations which disrupt VP35 dsRNA binding activity substantially impair VP35 inhibition of IFNαβ responses without significantly affecting VP35’s ability to function as a component of the viral RNA polymerase machinery (Hartman et al., 2008a, Leung et al., 2010, Prins et al., 2010).
These data may be explained by the ability of VP35 to sequester dsRNA molecules produced during the course of infection, preventing their recognition by RIG-I (Basler and Amarasinghe, 2009). However, this does not exclude other possible mechanisms. The identification of mutant VP35s with defects in function has allowed the study of their function in the context of virus replication. Such studies clearly demonstrate a critical role for VP35 in viral replication and pathogenesis in mice (Hartman et al., 2006, Hartman et al., 2008a, Hartman et al., 2008b) and guinea pigs (Prins et al.). Because NHPs mimic severe human disease better than do rodent models, it will be important to verify the importance of VP35 IFN-antagonist activity in NHP models as well.
VP35 can suppress IFN production in macrophages and cDCs. Using recombinant Venezuelan equine encephalitis virus replicon particles (VRP) that express VP35, VP35 expression was demonstrated to completely inhibit secretion of IFNα as compared to a VRP encoding GFP (Bosio et al., 2003). Similar results were obtained with a system in which VP35 was expressed from a negative-strand RNA virus, the paramyxovirus Newcastle disease virus (NDV). When infected with a NDV that expresses luciferase, cDCs and monocyte-derived macrophages respond with robust IFNαβ production, and express several interferon-induced genes (ISGs) (Leung et al., 2011b). In contrast, cDC and macrophages infected with NDV encoding VP35 produce much less IFNαβ. Interestingly, in addition to inhibiting the production of IFN, VP35 expressed in the context of NDV also inhibits TNFα production in cDC (Leung et al., 2011b). This is consistent with studies performed in cells other than APCs. For example, a significant increase in expression of genes related to IFNαβ responses as well as an increase in the chemokine RANTES was noted in the liver cell line HepG2 infected with a ZEBOV bearing a mutation that disrupts dsRNA binding and VP35 IFN-antagonist function, (Hartman et al., 2008b). The extent to which VP35 may modulate expression of other cytokines and chemokines in the context of actual filovirus-infected APCs remains to be defined, but could be addressed by using VP35-mutant viruses.
The RIG-I pathway likely serves as a major activator of cDC maturation in response to non-segmented negative-strand RNA virus infection (Lopez et al., 2006). Therefore, viral proteins such as VP35 that inhibit RIG-I signaling may effectively inhibit this process. Whether the RIG-I-inhibitory function of VP35 can fully account for the aberrant activation of EBOV-infected DCs remains to be determined. Experiments using herpes simplex virus type 1 (HSV-1) recombinants that either express or do not express VP35 support a role for VP35 in inhibition of cDC cell surface marker upregulation and inhibition of IL-6, IL-12, TNFα and IFNαβ production. This study also used expression of VP35 from lentiviral vectors to demonstrate that VP35 can also impair LPS-induced CD80 and CD86 upregulation and cytokine expression (Jin et al., 2009). In this experiment, a mutant VP35 lacking dsRNA binding activity functioned like wild-type VP35, consistent with a model in which VP35 can inhibit IFN responses independently of dsRNA and independently of the RIG-I signaling pathway (Chang et al., 2009, Jin et al., 2009, Leung et al., 2010). Whether the pathways that activate DCs in response to the large DNA virus HSV-1 accurately mimic the pathways activated by filoviruses remains to be determined, and the relevance of VP35 inhibition of TLR signaling to actual filovirus infection also remains to be demonstrated. However, given the results obtained with the HSV-1 based system, the impact of VP35 upon DC maturation and function should be investigated in the context of infection with wild-type and VP35-mutant filoviruses.
10. Inhibition of the pDC IFNα response
In contrast to what was seen in cDCs and macrophages, when the EBOV VP35 protein was delivered to pDCs via a recombinant NDV, it was ineffective at countering pDC IFNα production. The induction of IFNα in this system is TLR7-dependent. Consistent with the induction of IFNα by NDV-VP35, VP35 did not detectably inhibit signaling by a TLR7 signaling system reconstituted in 293T cells (Leung et al., 2011a). However, as described above, EBOV fails to enter and activate pDCs, at least in vitro (Leung et al., 2011a). Failure to trigger an early pDC IFNα response in vivo may therefore facilitate the systemic dissemination of EBOV in infected individuals.
11. Filoviruses inhibit IFN signaling
IFNs (IFNαβ or IFNγ) signal through the IFNαβ or IFNγ receptors, respectively, to activate Jak-STAT signaling cascades, turning on hundreds of genes and inducing an antiviral state. In addition to inhibiting the production of IFNαβ from infected cells, filoviruses also encode mechanisms that can prevent infected cells from responding to exogenously added IFNs (Harcourt et al., 1998, Harcourt et al., 1999, Kash et al., 2006, Valmas et al., 2010). This has the obvious potential to block the antiviral effects of IFNs, potentially allowing the virus to replicate in APCs and other cells. In addition, IRF-7 is an IFNαβ-induced gene, and its upregulation primes cells to produce more IFNα in response to infection. By impairing IFN signaling, the viruses may therefore indirectly suppress IFNαβ production as well. Finally, IFNαβ has numerous effects on immune cells, including the macrophages and DCs that are targets of filovirus infection. For example, IFNαβ can promote monocyte differentiation into DCs, modulate macrophage cytokine production and promote the maturation of immature DCs such that they exhibit enhanced ability to stimulate CD8 T cell responses (reviewed in Hervas-Stubbs et al., 2011). Therefore, inhibiting IFN signaling may suppress the maturation or activation of infected macrophages and DCs.
For EBOV, inhibition of IFN-triggered signaling has been attributed to the ability of VP24 to bind to karyopherin-α1 (KPNA1), the nuclear localization signal receptor for activated STAT1 (Reid et al., 2006, Reid et al., 2007). This prevents the nuclear transport of STAT1 hetero- and homodimers mediated by a subset of the cellular karyopherin-α (KPNA) nuclear transport factor family, and the ensuing expression of IFN-induced antiviral genes. Mutations in VP24 that attenuate binding to karyopherin reduce the ability of VP24 to inhibit STAT1-dependent reporter activity (Mateo et al., 2010).
In addition to inhibiting STAT1 translocation, the VP24 interaction with the C-terminal region of KPNAs could also impact the nuclear import of other proteins. In an attempt to determine if VP24 has a larger role in altering the interaction between KPNAs and cellular proteins, a proteomics study was performed to identify additional KPNA-dependent cargo whose nuclear import might be affected by VP24 (Shabman et al., 2011). Co-immunoprecipitation studies demonstrate that hnRNP C1/C2 interacts with multiple KPNA family members. Interaction with hnRNP C1/C2 occurs through the same KPNA1 C-terminal region (amino acids 424–457) that binds VP24 and phospho-STAT1. The ability of hnRNP C1/C2 to bind KPNA1 is diminished in the presence of VP24, and cells transiently expressing VP24 redistribute hnRNP C1/C2 from the nucleus to the cytoplasm. These data demonstrate that the impact of EBOV VP24 upon nuclear import extends beyond STAT1. However, the effect of these functions of VP24 upon normal APC function has not been examined but will be an area of future investigation.
For MARV, the VP40 protein carries an IFN-antagonist function (Valmas and Basler, 2011, Valmas et al., 2010). When IFNαβ is added to MARV-infected cells, the normal phosphorylation of STAT1 and STAT2 is abrogated, resulting in an absence of IFN responses (Kash et al., 2006). The loss of STAT phosphorylation correlates with an absence of activation of receptor-associated Jak family tyrosine kinases. Expression of the MARV VP40 is sufficient to recapitulate these phenotypes. Current data suggest that it targets Jak1 function, although this may occur indirectly, through interaction with other cellular factors. Jak1 associates with a variety of cellular growth factor and cytokine receptors, and MARV VP40 was demonstrated to inhibit phosphorylation of STAT1 and STAT3 in response to IL-6 (Valmas et al., 2010). Therefore, the impact of MARV VP40 upon cellular signaling pathways could extend beyond IFN-induced antiviral responses.
12. An APC-centric view of filoviral HF
Ultimately, it will be necessary to integrate the various mechanisms which influence APC-filovirus interactions into pathogenesis in vivo. A model, similar to what has been proposed by others (Bray, 2005), that incorporates available data and which places APCs as the heart of filoviral pathogenesis is illustrated by Fig. 1 . In this model, filovirus infection is postulated to usurp normal APC function in order to establish a feedback loop that, if not broken, leads to unfettered virus production and hemorrhagic fever.
Fig. 1.
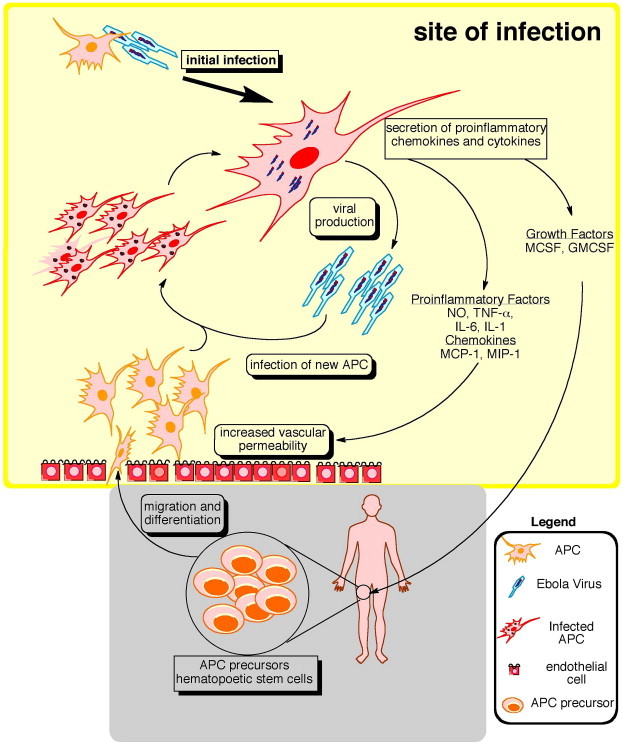
Mucous membrane associated antigen-presenting cells (APCs) provide the initial targets for filovirus infection. Infected and deregulated macrophages are major targets of infection, producing progeny virus and secreting factors conducive to the recruitment of more targets for infection. Secreted growth, chemotactic and proinflammatory factors increase monocyte production, migration and extravasation into the inflamed tissue where they differentiate into highly permissive APCs. At the same time, the proinflammatory response promotes vascular permeability and tissue factor expression on macrophages which promotes disseminated intravascular coagulation.
Filoviruses presumably first encounter APC targets early in the infection process. Infected APCs are thought to actively produce infectious virus and help disseminate the virus by trafficking to secondary lymphoid organs such as the spleen. Secreted chemokines from EBOV-infected monocyte/macrophages, such as MIP-1α, presumably recruit APCs to the site of inflammation enabling further APC infection. Furthermore, growth factors normally secreted during inflammation may play a role in stimulating the production of new leukocytes from the bone marrow providing further targets of EBOV infection. Macrophage colony-stimulating factor (M-CSF), which stimulates stem cells to differentiate into macrophages, as well as other related cell types, was found at higher levels in individuals that eventually succumbed to EBOV infection as compared to survivors, while granulocyte macrophage colony-stimulating factor was found at similar levels (Wauquier et al., 2010). Furthermore, EBOV infection is associated with lymphopenia and the production of immature and atypical leukocytes from the bone marrow (Geisbert and Hensley, 2004).
On the other hand, in vitro filovirus-infected DCs are productively infected and functionally deregulated, unable to upregulate co-stimulatory molecules or stimulate lymphocytes, especially naïve T cells. Lymphocytes, in effect, lose the support of the APC most potent at stimulating naïve lymphocyte activation and development. This might contribute to the massive lymphocyte apoptosis consistently seen in both human and nonhuman primate EBOV infections (Geisbert et al., 2000, Geisbert et al., 2003b, Geisbert et al., 2003c, Geisbert et al., 2003d, Mahanty et al., 2003, Wauquier et al., 2010).
Inflammatory cytokines further amplify the recruitment of newly formed APCs by affecting the vasculature of the infected individual. For example TNFα activates endothelial cells leading to the upregulation of E-selectin, ICAM-1 or VCAM-1 (Wahl-Jensen et al., 2005b) which are important in facilitating chemotaxis and extravasation of immune cells across endothelial cells. The initial infection presumably localizes the secretion of inflammatory cytokines where proximal endothelial cells facilitate recruitment of leukocytes including APCs (Vestweber, 2002). Therefore, chemokines secreted by infected APCs may attract more APCs to extravasate from the blood into the inflamed tissue; and this feedback loop, unless broken leads to the productive infection of more APCs.
Unchecked virus replication and concomitant inflammatory cytokine production is thought to promote endothelial leakage and shock (Aleksandrowicz et al., 2008). This may occur due to the effects of specific viral gene products. For example, endothelial cells bind EBOV GP pseudotyped viral particles and can be infected by EBOV (Yang et al., 1998), and it has been proposed that the EBOV glycoprotein is a determinant of vascular cell injury (Yang et al., 2000). It has also been shown that GP-expressing VLPs bind and disrupt the host endothelial barrier function (Wahl-Jensen et al., 2005b). Interestingly, the secreted glycoprotein sGP facilitates recovery of the endothelial barrier after it has been disrupted by TNF-α (Falzarano et al., 2007, Wahl-Jensen et al., 2005b). However, other studies suggest that EBOV infection of endothelial cells does not cause significant endothelial cell death and that endothelial cell infection occurs only late in the course of infection (Geisbert et al., 2003d). Furthermore, researchers studying tissues from fatal cases of filovirus HF from the initial outbreaks in 1967 and 1975 were not able to identify any vascular lesions (Gear et al., 1975). Further studies using non-human primates did not find significant destruction of the vascular endothelium (Geisbert et al., 2003d). However, supernatants from filovirus-infected monocytes/macrophages or soluble mediators such TNF-α plus IFN-γ can cause disruption of an in vitro endothelial barrier (Aleksandrowicz et al., 2008, Feldmann and Klenk, 2004) linking APC response to infection with endothelial cell leakage (Feldmann et al., 1996). Taken together, the unchecked production of EBOV expressing GP and the secretion of inflammatory cytokines potentially disturb the balance of fluid volume distributed between vasculature and the interstitium (Feldmann et al., 2003, Schnittler and Feldmann, 2003). Moreover, the release of nitric oxide from infected monocytes/macrophages and endothelium (Sanchez et al., 2004) may further disturb this vasculature homeostasis.
13. Further defining the contribution of APCs to filoviral pathogenesis in humans and non-human primates
Ultimately, this and similar models of filoviral pathogenesis, require validation in animal models. Relatively straightforward experiments could test the functional status of APCs in infected animals through intracellular or extracellular staining for EBOV gene products and cellular factors (e.g. cytokines). Ideally, such experiments would quantify the frequency of infection of different APC types and the cytokines secreted by different cells types. Isolation of in vivo infected APCs and testing their ability to process antigen and stimulate an EBOV antigen-specific response ex vivo would provide a more clear understanding their functional status and allow comparison to studies performed in cells infected in vitro. Given the copious production of cytokines, chemokines and possibly viral products, it is possible that APCs and other immune cells that are not directly infected will exhibit altered function. Therefore, it will also be important to assess the functional status of uninfected APCs and lymphocytes from the same infected animals. For example, it might prove fruitful to assess the ability of T cells to respond to either allo- or superantigens from competent non-infected MHC-compatible or incompatible APCs. Such studies would not only inform our understanding of APCs but also better describe the status of the adaptive immune response. This is particularly important in NHPs, which most closely mimic severe human infections. Functional T cells have been shown to be present in EBOV-infected mice (Bradfute et al., 2008). Hopefully, by more precisely defining filovirus–APC interactions from the molecular perspective and the contribution of these interactions to pathogenesis in vivo, new specific and precisely targeted therapeutic interventions can be designed.
14. Are filovirus–APC interactions different in reservoir hosts?
Substantial evidence points to bats as filovirus reservoirs. They support filovirus replication but do not exhibit symptoms of disease following experimental inoculation (Swanepoel et al., 2007). Live MARV has been isolated from Rousettus aegyptiacus bats from a cave which was the site of several human infections, and viral genetic material was also detected in Hipposideros species bats (Towner et al., 2009). In addition, the genome of a novel EBOV, Lloviu virus (LLOV), has been found in Schreiber’s long-fingered bats (Miniopterus schreibersii) (classified as a microbat) in Spain (Negredo et al., 2011). Finally, Myotis lucifugus and Myotis velifer incautus (both microbats) possesses integrated homologs of filoviral genes in their genomes, suggesting at least historical infection with filoviruses (see below) (Belyi et al., 2010).
It has long been thought that the natural reservoir hosts of these viruses cannot be as susceptible to lethal infection as are many primates, otherwise filoviruses could not persist in nature. The basis by which reservoir hosts, such as bats, are able to serve as filovirus reservoirs and presumably avoid lethal infection is therefore a question at the heart of filovirus biology. Understanding how filoviruses interact with the innate and adaptive immune systems of reservoir hosts, including the APCs of reservoir hosts, is therefore important. Specific questions that could be asked include whether filoviruses infect and replicate in reservoir host APCs in vivo, whether they elicit different responses in reservoir host APCs as compared to human APCs and whether the potency of innate immune evasion mechanisms differs in reservoir hosts as compared with primate cells. It is possible that filoviruses have evolved to a relatively symbiotic relationship with bats, such that suppression of innate immunity is sufficient to maintain infection and virus transmission to new individuals but is not as absolute as in species that develop HF.
Such studies in bats will be complicated by the potential diversity of species that may serve as hosts (bats, which are classified in the Order Chiroptera, account for about 20 percent of all mammalian species). In addition there is a need to develop reagents that can be used in relevant bat species. In this regard, bats are of increasing interest to the research community, because they are likely reservoirs of a number of other emerging zoonotic viruses including the SARS coronavirus, other coronaviruses, rabies viruses, novel lysaviruses, astroviruses and adenoviruses (Bennett, 2006). Because of their prominence as hosts of zoonotic viruses, efforts have begun to characterize the innate and adaptive immune responses of various bats (e.g. Fujii et al., 2010, He et al., 2010, Kepler et al., 2010, Omatsu et al., 2008). In the long run, studies that compare virus-host APC interactions in reservoirs hosts versus humans will shed significant new light on the molecular determinants of pathogenesis.
Acknowledgements
This work is supported by NIH Grants to C.F.B. R01AI059536 and U54AI057158 (Northeast Biodefense Center–Lipkin).
References
- Aleksandrowicz P., Marzi A., Biedenkopf N., Beimforde N., Becker S., Hoenen T., Feldmann H., Schnittler H.J. Ebola virus enters host cells by macropinocytosis and clathrin-mediated endocytosis. Journal of Infectious Diseases. 2011;204(Suppl 3):S957–967. doi: 10.1093/infdis/jir326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aleksandrowicz P., Wolf K., Falzarano D., Feldmann H., Seebach J., Schnittler H. Viral haemorrhagic fever and vascular alterations. Hamostaseologie. 2008;28:77–84. [PubMed] [Google Scholar]
- Allavena P., Chieppa M., Monti P., Piemonti L. From pattern recognition receptor to regulator of homeostasis: the double-faced macrophage mannose receptor. Critical Reviews in Immunology. 2004;24:179–192. doi: 10.1615/critrevimmunol.v24.i3.20. [DOI] [PubMed] [Google Scholar]
- Alvarez C.P., Lasala F., Carrillo J., Muniz O., Corbi A.L., Delgado R. C-type lectins DC-SIGN and L-SIGN mediate cellular entry by Ebola virus in cis and in trans. Journal of Virology. 2002;76:6841–6844. doi: 10.1128/JVI.76.13.6841-6844.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bale S., Liu T., Li S., Wang Y., Abelson D., Fusco M., Woods V.L., Jr., Ollmann Saphire E. Ebola Virus Glycoprotein Needs an Additional Trigger, beyond Proteolytic Priming for Membrane Fusion. PLoS Negl Trop Dis. 2011;5:e1395. doi: 10.1371/journal.pntd.0001395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bar S., Takada A., Kawaoka Y., Alizon M. Detection of cell-cell fusion mediated by Ebola virus glycoproteins. Journal of Virology. 2006;80:2815–2822. doi: 10.1128/JVI.80.6.2815-2822.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Basler C.F., Amarasinghe G.K. Evasion of interferon responses by Ebola and Marburg viruses. Journal of Interferon and Cytokine Research. 2009;29:511–520. doi: 10.1089/jir.2009.0076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Basler C.F., Mikulasova A., Martinez-Sobrido L., Paragas J., Muhlberger E., Bray M., Klenk H.D., Palese P., Garcia-Sastre A. The Ebola virus VP35 protein inhibits activation of interferon regulatory factor 3. Journal of Virology. 2003;77:7945–7956. doi: 10.1128/JVI.77.14.7945-7956.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Basler C.F., Wang X., Muhlberger E., Volchkov V., Paragas J., Klenk H.D., Garcia-Sastre A., Palese P. The Ebola virus VP35 protein functions as a type I IFN antagonist. Proc Natl Acad Sci U S A. 2000;97:12289–12294. doi: 10.1073/pnas.220398297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baum A., Garcia-Sastre A. Induction of type I interferon by RNA viruses: cellular receptors and their substrates. Amino Acids. 2010;38:1283–1299. doi: 10.1007/s00726-009-0374-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bavari S., Bosio C.M., Wiegand E., Ruthel G., Will A.B., Geisbert T.W., Hevey M., Schmaljohn C., Schmaljohn A., Aman M.J. Lipid raft microdomains: a gateway for compartmentalized trafficking of Ebola and Marburg viruses. The Journal of experimental medicine. 2002;195:593–602. doi: 10.1084/jem.20011500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Belyi V.A., Levine A.J., Skalka A.M. Unexpected inheritance. multiple integrations of ancient bornavirus and ebolavirus/marburgvirus sequences in vertebrate genomes. PLoS Pathogens. 2010;6:e1001030. doi: 10.1371/journal.ppat.1001030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bennett M. Bats and human emerging diseases. Epidemiology and Infection. 2006;134:905–907. doi: 10.1017/S0950268806006674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bennett W.E., Cohn Z.A. The isolation and selected properties of blood monocytes. Journal of Experimental Medicine. 1966;123:145–160. doi: 10.1084/jem.123.1.145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bhattacharyya S., Warfield K.L., Ruthel G., Bavari S., Aman M.J., Hope T.J. Ebola virus uses clathrin-mediated endocytosis as an entry pathway. Virology. 2010;401:18–28. doi: 10.1016/j.virol.2010.02.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bosio C.M., Aman M.J., Grogan C., Hogan R., Ruthel G., Negley D., Mohamadzadeh M., Bavari S., Schmaljohn A. Ebola and Marburg viruses replicate in monocyte-derived dendritic cells without inducing the production of cytokines and full maturation. Journal of Infectious Diseases. 2003;188:1630–1638. doi: 10.1086/379199. [DOI] [PubMed] [Google Scholar]
- Bosio C.M., Moore B.D., Warfield K.L., Ruthel G., Mohamadzadeh M., Aman M.J., Bavari S. Ebola and Marburg virus-like particles activate human myeloid dendritic cells. Virology. 2004;326:280–287. doi: 10.1016/j.virol.2004.05.025. [DOI] [PubMed] [Google Scholar]
- Bradfute S.B., Bavari S. Correlates of immunity to filovirus infection. Viruses. 2011;3:982–1000. doi: 10.3390/v3070982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bradfute S.B., Warfield K.L., Bavari S. Functional CD8+ T cell responses in lethal Ebola virus infection. Journal of Immunology. 2008;180:4058–4066. doi: 10.4049/jimmunol.180.6.4058. [DOI] [PubMed] [Google Scholar]
- Bray M. Pathogenesis of viral hemorrhagic fever. Current Opinion in Immunology. 2005;17:399–403. doi: 10.1016/j.coi.2005.05.001. [DOI] [PubMed] [Google Scholar]
- Bray M., Davis K., Geisbert T., Schmaljohn C., Huggins J. A mouse model for evaluation of prophylaxis and therapy of Ebola hemorrhagic fever. Journal of Infectious Diseases. 1999;179(Suppl 1):S248–258. doi: 10.1086/514292. [DOI] [PubMed] [Google Scholar]
- Bray M., Geisbert T.W. Ebola virus: the role of macrophages and dendritic cells in the pathogenesis of Ebola hemorrhagic fever. The international journal of biochemistry & cell biology. 2005;37:1560–1566. doi: 10.1016/j.biocel.2005.02.018. [DOI] [PubMed] [Google Scholar]
- Cardenas W.B., Loo Y.M., Gale M., Jr., Hartman A.L., Kimberlin C.R., Martinez-Sobrido L., Saphire E.O., Basler C.F. Ebola virus VP35 protein binds double-stranded RNA and inhibits alpha/beta interferon production induced by RIG-I signaling. Journal of Virology. 2006;80:5168–5178. doi: 10.1128/JVI.02199-05. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carette J.E., Raaben M., Wong A.C., Herbert A.S., Obernosterer G., Mulherkar N., Kuehne A.I., Kranzusch P.J., Griffin A.M., Ruthel G., Cin P.D., Dye J.M., Whelan S.P., Chandran K., Brummelkamp T.R. Ebola virus entry requires the cholesterol transporter Niemann-Pick C1. Nature. 2011;477:340–343. doi: 10.1038/nature10348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chan S.Y., Empig C.J., Welte F.J., Speck R.F., Schmaljohn A., Kreisberg J.F., Goldsmith M.A. Folate receptor-alpha is a cofactor for cellular entry by Marburg and Ebola viruses. Cell. 2001;106:117–126. doi: 10.1016/s0092-8674(01)00418-4. [DOI] [PubMed] [Google Scholar]
- Chandran K., Sullivan N.J., Felbor U., Whelan S.P., Cunningham J.M. Endosomal proteolysis of the Ebola virus glycoprotein is necessary for infection. Science. 2005;308:1643–1645. doi: 10.1126/science.1110656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chang T.H., Kubota T., Matsuoka M., Jones S., Bradfute S.B., Bray M., Ozato K. Ebola Zaire virus blocks type I interferon production by exploiting the host SUMO modification machinery. PLoS Pathogens. 2009;5:e1000493. doi: 10.1371/journal.ppat.1000493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Colonna M., Trinchieri G., Liu Y.J. Plasmacytoid dendritic cells in immunity. Nature Immunology. 2004;5:1219–1226. doi: 10.1038/ni1141. [DOI] [PubMed] [Google Scholar]
- Connolly B.M., Steele K.E., Davis K.J., Geisbert T.W., Kell W.M., Jaax N.K., Jahrling P.B. Pathogenesis of experimental Ebola virus infection in guinea pigs. The Journal of infectious diseases. 1999;179:S203–217. doi: 10.1086/514305. [DOI] [PubMed] [Google Scholar]
- Cote M., Misasi J., Ren T., Bruchez A., Lee K., Filone C.M., Hensley L., Li Q., Ory D., Chandran K., Cunningham J. Small molecule inhibitors reveal Niemann-Pick C1 is essential for Ebola virus infection. Nature. 2011 doi: 10.1038/nature10380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crowley M., Inaba K., Witmer-Pack M., Steinman R.M. The cell surface of mouse dendritic cells: FACS analyses of dendritic cells from different tissues including thymus. Cellular Immunology. 1989;118:108–125. doi: 10.1016/0008-8749(89)90361-4. [DOI] [PubMed] [Google Scholar]
- Davis K.J., Anderson A.O., Geisbert T.W., Steele K.E., Geisbert J.B., Vogel P., Connolly B.M., Huggins J.W., Jahrling P.B., Jaax N.K. Pathology of experimental Ebola virus infection in African green monkeys. Involvement of fibroblastic reticular cells. Archives of pathology & laboratory medicine. 1997;121:805–819. [PubMed] [Google Scholar]
- Doherty P.C., Zinkernagel R.M. H-2 compatibility is required for T-cell-mediated lysis of target cells infected with lymphocytic choriomeningitis virus. Journal of Experimental Medicine. 1975;141:502–507. doi: 10.1084/jem.141.2.502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dominguez-Soto A., Aragoneses-Fenoll L., Martin-Gayo E., Martinez-Prats L., Colmenares M., Naranjo-Gomez M., Borras F.E., Munoz P., Zubiaur M., Toribio M.L., Delgado R., Corbi A.L. The DC-SIGN-related lectin LSECtin mediates antigen capture and pathogen binding by human myeloid cells. Blood. 2007;109:5337–5345. doi: 10.1182/blood-2006-09-048058. [DOI] [PubMed] [Google Scholar]
- Dube D., Brecher M.B., Delos S.E., Rose S.C., Park E.W., Schornberg K.L., Kuhn J.H., White J.M. The primed ebolavirus glycoprotein (19-kilodalton GP1,2): sequence and residues critical for host cell binding. Journal of Virology. 2009;83:2883–2891. doi: 10.1128/JVI.01956-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dube D., Schornberg K.L., Shoemaker C.J., Delos S.E., Stantchev T.S., Clouse K.A., Broder C.C., White J.M. Cell adhesion-dependent membrane trafficking of a binding partner for the ebolavirus glycoprotein is a determinant of viral entry. Proc Natl Acad Sci U S A. 2010;107:16637–16642. doi: 10.1073/pnas.1008509107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dube D., Schornberg K.L., Stantchev T.S., Bonaparte M.I., Delos S.E., Bouton A.H., Broder C.C., White J.M. Cell adhesion promotes Ebola virus envelope glycoprotein-mediated binding and infection. Journal of Virology. 2008;82:7238–7242. doi: 10.1128/JVI.00425-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ebihara H., Groseth A., Neumann G., Kawaoka Y., Feldmann H. The role of reverse genetics systems in studying viral hemorrhagic fevers. Thrombosis and haemostasis. 2005;94:240–253. doi: 10.1160/TH05-05-0335. [DOI] [PubMed] [Google Scholar]
- Ebihara H., Takada A., Kobasa D., Jones S., Neumann G., Theriault S., Bray M., Feldmann H., Kawaoka Y. Molecular determinants of Ebola virus virulence in mice. PLoS Pathogens. 2006;2:e73. doi: 10.1371/journal.ppat.0020073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Empig C.J., Goldsmith M.A. Association of the Caveola Vesicular System with Cellular Entry by Filoviruses. Journal of Virology. 2002;76:5266–5270. doi: 10.1128/JVI.76.10.5266-5270.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Falzarano D., Krokhin O., Van Domselaar G., Wolf K., Seebach J., Schnittler H.J., Feldmann H. Ebola sGP–the first viral glycoprotein shown to be C-mannosylated. Virology. 2007;368:83–90. doi: 10.1016/j.virol.2007.06.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Feldmann H., Bugany H., Mahner F., Klenk H.D., Drenckhahn D., Schnittler H.J. Filovirus-induced endothelial leakage triggered by infected monocytes/macrophages. Journal of Virology. 1996;70:2208–2214. doi: 10.1128/jvi.70.4.2208-2214.1996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Feldmann H., Jones S., Klenk H.D., Schnittler H.J. Ebola virus: from discovery to vaccine. Nature Reviews Immunology. 2003;3:677–685. doi: 10.1038/nri1154. [DOI] [PubMed] [Google Scholar]
- Feldmann H., Klenk H.D. Horizon Bioscience; Wymondham: 2004. Ebola and Marburg viruses: molecular and cellular biology. [Google Scholar]
- Ferenbach D., Hughes J. Macrophages and dendritic cells: what is the difference? Kidney International. 2008;74:5–7. doi: 10.1038/ki.2008.189. [DOI] [PubMed] [Google Scholar]
- Francica J.R., Matukonis M.K., Bates P. Requirements for cell rounding and surface protein down-regulation by Ebola virus glycoprotein. Virology. 2009;383:237–247. doi: 10.1016/j.virol.2008.10.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Francica J.R., Varela-Rohena A., Medvec A., Plesa G., Riley J.L., Bates P. Steric shielding of surface epitopes and impaired immune recognition induced by the ebola virus glycoprotein. PLoS Pathogens. 2010;6 doi: 10.1371/journal.ppat.1001098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fujii H., Watanabe S., Yamane D., Ueda N., Iha K., Taniguchi S., Kato K., Tohya Y., Kyuwa S., Yoshikawa Y., Akashi H. Functional analysis of Rousettus aegyptiacus “signal transducer and activator of transcription 1” (STAT1) Developmental and Comparative Immunology. 2010;34:598–602. doi: 10.1016/j.dci.2010.01.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garver W.S., Xie C., Repa J.J., Turley S.D., Dietschy J.M. Niemann-Pick C1 expression is not regulated by the amount of cholesterol flowing through cells in the mouse. Journal of Lipid Research. 2005;46:1745–1754. doi: 10.1194/jlr.M500130-JLR200. [DOI] [PubMed] [Google Scholar]
- Gautier E.L., Jakubzick C., Randolph G.J. Regulation of the migration and survival of monocyte subsets by chemokine receptors and its relevance to atherosclerosis. Arteriosclerosis, Thrombosis, and Vascular Biology. 2009;29:1412–1418. doi: 10.1161/ATVBAHA.108.180505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gautier E.L., Jakubzick C., Randolph G.J. Regulation of the migration and survival of monocyte subsets by chemokine receptors and its relevance to atherosclerosis. Arteriosclerosis, thrombosis, and vascular biology. 2009;29:1412–1418. doi: 10.1161/ATVBAHA.108.180505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gear J.S., Cassel G.A., Gear A.J., Trappler B., Clausen L., Meyers A.M., Kew M.C., Bothwell T.H., Sher R., Miller G.B., Schneider J., Koornhof H.J., Gomperts E.D., Isaacson M., Gear J.H. Outbreake of Marburg virus disease in Johannesburg. Br Med J. 1975;4:489–493. doi: 10.1136/bmj.4.5995.489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Geisbert T.W., Hensley L.E. Ebola virus: new insights into disease aetiopathology and possible therapeutic interventions. Expert reviews in molecular medicine [electronic resource]. 2004;6:1–24. doi: 10.1017/S1462399404008300. [DOI] [PubMed] [Google Scholar]
- Geisbert T.W., Hensley L.E., Gibb T.R., Steele K.E., Jaax N.K., Jahrling P.B. Apoptosis induced in vitro and in vivo during infection by Ebola and Marburg viruses. Laboratory Investigation; A Journal of Technical Methods and, Pathology. 2000;80:171–186. doi: 10.1038/labinvest.3780021. [DOI] [PubMed] [Google Scholar]
- Geisbert T.W., Hensley L.E., Jahrling P.B., Larsen T., Geisbert J.B., Paragas J., Young H.A., Fredeking T.M., Rote W.E., Vlasuk G.P. Treatment of Ebola virus infection with a recombinant inhibitor of factor VIIa/tissue factor: a study in rhesus monkeys. Lancet. 2003;362:1953–1958. doi: 10.1016/S0140-6736(03)15012-X. [DOI] [PubMed] [Google Scholar]
- Geisbert T.W., Hensley L.E., Larsen T., Young H.A., Reed D.S., Geisbert J.B., Scott D.P., Kagan E., Jahrling P.B., Davis K.J. Pathogenesis of Ebola hemorrhagic fever in cynomolgus macaques: evidence that dendritic cells are early and sustained targets of infection. The American journal of pathology. 2003;163:2347–2370. doi: 10.1016/S0002-9440(10)63591-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Geisbert T.W., Jahrling P.B., Hanes M.A., Zack P.M. Association of Ebola-related Reston virus particles and antigen with tissue lesions of monkeys imported to the United States. Journal of comparative pathology. 1992;106:137–152. doi: 10.1016/0021-9975(92)90043-t. [DOI] [PubMed] [Google Scholar]
- Geisbert T.W., Young H.A., Jahrling P.B., Davis K.J., Kagan E., Hensley L.E. Mechanisms underlying coagulation abnormalities in ebola hemorrhagic fever: overexpression of tissue factor in primate monocytes/macrophages is a key event. The Journal of infectious diseases. 2003;188:1618–1629. doi: 10.1086/379724. [DOI] [PubMed] [Google Scholar]
- Geisbert T.W., Young H.A., Jahrling P.B., Davis K.J., Larsen T., Kagan E., Hensley L.E. Pathogenesis of Ebola hemorrhagic fever in primate models: evidence that hemorrhage is not a direct effect of virus-induced cytolysis of endothelial cells. The American journal of pathology. 2003;163:2371–2382. doi: 10.1016/S0002-9440(10)63592-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Geissmann F., Manz M.G., Jung S., Sieweke M.H., Merad M., Ley K. Development of monocytes, macrophages, and dendritic cells. Science. 2010;327:656–661. doi: 10.1126/science.1178331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gibb T.R., Bray M., Geisbert T.W., Steele K.E., Kell W.M., Davis K.J., Jaax N.K. Pathogenesis of experimental Ebola Zaire virus infection in BALB/c mice. Journal of Comparative Pathology. 2001;125:233–242. doi: 10.1053/jcpa.2001.0502. [DOI] [PubMed] [Google Scholar]
- Gramberg T., Hofmann H., Moller P., Lalor P.F., Marzi A., Geier M., Krumbiegel M., Winkler T., Kirchhoff F., Adams D.H., Becker S., Munch J., Pohlmann S. LSECtin interacts with filovirus glycoproteins and the spike protein of SARS coronavirus. Virology. 2005;340:224–236. doi: 10.1016/j.virol.2005.06.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gramberg T., Soilleux E., Fisch T., Lalor P.F., Hofmann H., Wheeldon S., Cotterill A., Wegele A., Winkler T., Adams D.H., Pohlmann S. Interactions of LSECtin and DC-SIGN/DC-SIGNR with viral ligands: Differential pH dependence, internalization and virion binding. Virology. 2008;373:189–201. doi: 10.1016/j.virol.2007.11.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gupta M., Goldsmith C.S., Metcalfe M.G., Spiropoulou C.F., Rollin P.E. Reduced virus replication, proinflammatory cytokine production, and delayed macrophage cell death in human PBMCs infected with the newly discovered Bundibugyo ebolavirus relative to Zaire ebolavirus. Virology. 2010;402:203–208. doi: 10.1016/j.virol.2010.03.024. [DOI] [PubMed] [Google Scholar]
- Gupta M., Mahanty S., Ahmed R., Rollin P.E. Monocyte-derived human macrophages and peripheral blood mononuclear cells infected with ebola virus secrete MIP-1alpha and TNF-alpha and inhibit poly-IC-induced IFN-alpha in vitro. Virology. 2001;284:20–25. doi: 10.1006/viro.2001.0836. [DOI] [PubMed] [Google Scholar]
- Habjan M., Andersson I., Klingstrom J., Schumann M., Martin A., Zimmermann P., Wagner V., Pichlmair A., Schneider U., Muhlberger E., Mirazimi A., Weber F. Processing of genome 5′ termini as a strategy of negative-strand RNA viruses to avoid RIG-I-dependent interferon induction. PLoS ONE. 2008;3:e2032. doi: 10.1371/journal.pone.0002032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harcourt B.H., Sanchez A., Offermann M.K. Ebola virus inhibits induction of genes by double-stranded RNA in endothelial cells. Virology. 1998;252:179–188. doi: 10.1006/viro.1998.9446. [DOI] [PubMed] [Google Scholar]
- Harcourt B.H., Sanchez A., Offermann M.K. Ebola virus selectively inhibits responses to interferons, but not to interleukin-1beta, in endothelial cells. Journal of Virology. 1999;73:3491–3496. doi: 10.1128/jvi.73.4.3491-3496.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hartman A.L., Bird B.H., Towner J.S., Antoniadou Z.A., Zaki S.R., Nichol S.T. Inhibition of IRF-3 activation by VP35 is critical for the high level of virulence of ebola virus. Journal of Virology. 2008;82:2699–2704. doi: 10.1128/JVI.02344-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hartman A.L., Dover J.E., Towner J.S., Nichol S.T. Reverse genetic generation of recombinant Zaire Ebola viruses containing disrupted IRF-3 inhibitory domains results in attenuated virus growth in vitro and higher levels of IRF-3 activation without inhibiting viral transcription or replication. Journal of Virology. 2006;80:6430–6440. doi: 10.1128/JVI.00044-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hartman A.L., Ling L., Nichol S.T., Hibberd M.L. Whole-genome expression profiling reveals that inhibition of host innate immune response pathways by Ebola virus can be reversed by a single amino acid change in the VP35 protein. Journal of Virology. 2008;82:5348–5358. doi: 10.1128/JVI.00215-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- He G., He B., Racey P.A., Cui J. Positive selection of the bat interferon alpha gene family. Biochemical Genetics. 2010;48:840–846. doi: 10.1007/s10528-010-9365-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hensley L.E., Stevens E.L., Yan S.B., Geisbert J.B., Macias W.L., Larsen T., Daddario-DiCaprio K.M., Cassell G.H., Jahrling P.B., Geisbert T.W. Recombinant human activated protein C for the postexposure treatment of Ebola hemorrhagic fever. Journal of Infectious Diseases. 2007;196(Suppl 2):S390–399. doi: 10.1086/520598. [DOI] [PubMed] [Google Scholar]
- Hensley L.E., Young H.A., Jahrling P.B., Geisbert T.W. Proinflammatory response during Ebola virus infection of primate models: possible involvement of the tumor necrosis factor receptor superfamily. Immunology letters. 2002;80:169–179. doi: 10.1016/s0165-2478(01)00327-3. [DOI] [PubMed] [Google Scholar]
- Hervas-Stubbs S., Perez-Gracia J.L., Rouzaut A., Sanmamed M.F., Le Bon A., Melero I. Direct effects of type I interferons on cells of the immune system. Clin Cancer Res. 2011;17:2619–2627. doi: 10.1158/1078-0432.CCR-10-1114. [DOI] [PubMed] [Google Scholar]
- Hood C.L., Abraham J., Boyington J.C., Leung K., Kwong P.D., Nabel G.J. Biochemical and structural characterization of cathepsin L-processed Ebola virus glycoprotein: implications for viral entry and immunogenicity. Journal of Virology. 2010;84:2972–2982. doi: 10.1128/JVI.02151-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hume D.A. Differentiation and heterogeneity in the mononuclear phagocyte system. Mucosal Immunology. 2008;1:432–441. doi: 10.1038/mi.2008.36. [DOI] [PubMed] [Google Scholar]
- Ito H., Watanabe S., Sanchez A., Whitt M.A., Kawaoka Y. Mutational analysis of the putative fusion domain of Ebola virus glycoprotein. Journal of virology. 1999;73:8907–8912. doi: 10.1128/jvi.73.10.8907-8912.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Janeway C.A., Jr., Medzhitov R. Innate immune recognition. Annual Review of Immunology. 2002;20:197–216. doi: 10.1146/annurev.immunol.20.083001.084359. [DOI] [PubMed] [Google Scholar]
- Jasenosky L.D., Neumann G., Lukashevich I., Kawaoka Y. Ebola virus VP40-induced particle formation and association with the lipid bilayer. Journal of virology. 2001;75:5205–5214. doi: 10.1128/JVI.75.11.5205-5214.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jin H., Yan Z., Prabhakar B.S., Feng Z., Ma Y., Verpooten D., Ganesh B., He B. The VP35 Protein of Ebola Virus Impairs Dendritic Cell Maturation Induced by Virus and Lipopolysaccharide. Journal of General Virology. 2009 doi: 10.1099/vir.0.017343-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson W.D., Jr., Mei B., Cohn Z.A. The separation, long-term cultivation, and maturation of the human monocyte. Journal of Experimental Medicine. 1977;146:1613–1626. doi: 10.1084/jem.146.6.1613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaletsky R.L., Simmons G., Bates P. Proteolysis of the Ebola virus glycoproteins enhances virus binding and infectivity. Journal of Virology. 2007;81:13378–13384. doi: 10.1128/JVI.01170-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kash J.C., Muhlberger E., Carter V., Grosch M., Perwitasari O., Proll S.C., Thomas M.J., Weber F., Klenk H.D., Katze M.G. Global suppression of the host antiviral response by Ebola- and Marburgviruses: increased antagonism of the type I interferon response is associated with enhanced virulence. Journal of Virology. 2006;80:3009–3020. doi: 10.1128/JVI.80.6.3009-3020.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kepler T.B., Sample C., Hudak K., Roach J., Haines A., Walsh A., Ramsburg E.A. Chiropteran types I and II interferon genes inferred from genome sequencing traces by a statistical gene-family assembler. BMC Genomics. 2010;11:444. doi: 10.1186/1471-2164-11-444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kimberlin C.R., Bornholdt Z.A., Li S., Woods V.L., Jr., MacRae I.J., Saphire E.O. Ebolavirus VP35 uses a bimodal strategy to bind dsRNA for innate immune suppression. Proc Natl Acad Sci U S A. 2010;107:314–319. doi: 10.1073/pnas.0910547107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kobayashi N., Karisola P., Pena-Cruz V., Dorfman D.M., Jinushi M., Umetsu S.E., Butte M.J., Nagumo H., Chernova I., Zhu B., Sharpe A.H., Ito S., Dranoff G., Kaplan G.G., Casasnovas J.M., Umetsu D.T., Dekruyff R.H., Freeman G.J. TIM-1 and TIM-4 glycoproteins bind phosphatidylserine and mediate uptake of apoptotic cells. Immunity. 2007;27:927–940. doi: 10.1016/j.immuni.2007.11.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kondratowicz A.S., Lennemann N.J., Sinn P.L., Davey R.A., Hunt C.L., Moller-Tank S., Meyerholz D.K., Rennert P., Mullins R.F., Brindley M., Sandersfeld L.M., Quinn K., Weller M., McCray P.B., Jr., Chiorini J., Maury W. T-cell immunoglobulin and mucin domain 1 (TIM-1) is a receptor for Zaire Ebolavirus and Lake Victoria Marburgvirus. Proc Natl Acad Sci U S A. 2011;108:8426–8431. doi: 10.1073/pnas.1019030108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kortepeter M.G., Bausch D.G., Bray M. Basic clinical and laboratory features of filoviral hemorrhagic fever. Journal of Infectious Diseases. 2011;204(Suppl 3):S810–816. doi: 10.1093/infdis/jir299. [DOI] [PubMed] [Google Scholar]
- Kuchroo V.K., Dardalhon V., Xiao S., Anderson A.C. New roles for TIM family members in immune regulation. Nature Reviews Immunology. 2008;8:577–580. doi: 10.1038/nri2366. [DOI] [PubMed] [Google Scholar]
- Kuhn J.H., Becker S., Ebihara H., Geisbert T.W., Johnson K.M., Kawaoka Y., Lipkin W.I., Negredo A.I., Netesov S.V., Nichol S.T., Palacios G., Peters C.J., Tenorio A., Volchkov V.E., Jahrling P.B. Proposal for a revised taxonomy of the family Filoviridae: classification, names of taxa and viruses, and virus abbreviations. Archives of Virology. 2010;155:2083–2103. doi: 10.1007/s00705-010-0814-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kuhn J.H., Radoshitzky S.R., Guth A.C., Warfield K.L., Li W., Vincent M.J., Towner J.S., Nichol S.T., Bavari S., Choe H., Aman M.J., Farzan M. Conserved receptor-binding domains of Lake Victoria marburgvirus and Zaire ebolavirus bind a common receptor. Journal of Biological Chemistry. 2006;281:15951–15958. doi: 10.1074/jbc.M601796200. [DOI] [PubMed] [Google Scholar]
- Lee J.E., Saphire E.O. Ebolavirus glycoprotein structure and mechanism of entry. Future Virol. 2009;4:621–635. doi: 10.2217/fvl.09.56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leung D.W., Ginder N.D., Fulton D.B., Nix J., Basler C.F., Honzatko R.B., Amarasinghe G.K. Structure of the Ebola VP35 interferon inhibitory domain. Proc Natl Acad Sci U S A. 2009;106:411–416. doi: 10.1073/pnas.0807854106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leung D.W., Prins K.C., Borek D.M., Farahbakhsh M., Tufariello J.M., Ramanan P., Nix J.C., Helgeson L.A., Otwinowski Z., Honzatko R.B., Basler C.F., Amarasinghe G.K. Structural basis for dsRNA recognition and interferon antagonism by Ebola VP35. Nature Structural & Molecular Biology. 2010;17:165–172. doi: 10.1038/nsmb.1765. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leung L., Martinez O., Reynard O., Volchkov V., Basler C. Ebola Virus Failure to Stimulate Plasmacytoid Dendritic Cell Interferon Responses Correlates With Impaired Cellular Entry. Journal of Infectious Diseases. 2011;204(Suppl 3):S973–S977. doi: 10.1093/infdis/jir331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leung L.W., Park M.S., Martinez O., Valmas C., Lopez C.B., Basler C.F. Ebolavirus VP35 suppresses IFN production from conventional but not plasmacytoid dendritic cells. Immunology and Cell Biology. 2011;89:792–802. doi: 10.1038/icb.2010.169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Levi M., Ten Cate H. Disseminated intravascular coagulation. New England Journal of Medicine. 1999;341:586–592. doi: 10.1056/NEJM199908193410807. [DOI] [PubMed] [Google Scholar]
- Lin G., Simmons G., Pohlmann S., Baribaud F., Ni H., Leslie G.J., Haggarty B.S., Bates P., Weissman D., Hoxie J.A., Doms R.W. Differential N-linked glycosylation of human immunodeficiency virus and Ebola virus envelope glycoproteins modulates interactions with DC-SIGN and DC-SIGNR. Journal of Virology. 2003;77:1337–1346. doi: 10.1128/JVI.77.2.1337-1346.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lopez C.B., Yount J.S., Moran T.M. Toll-like receptor-independent triggering of dendritic cell maturation by viruses. Journal of Virology. 2006;80:3128–3134. doi: 10.1128/JVI.80.7.3128-3134.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MacDonald K.P., Munster D.J., Clark G.J., Dzionek A., Schmitz J., Hart D.N. Characterization of human blood dendritic cell subsets. Blood. 2002;100:4512–4520. doi: 10.1182/blood-2001-11-0097. [DOI] [PubMed] [Google Scholar]
- Mahanty S., Hutchinson K., Agarwal S., McRae M., Rollin P.E., Pulendran B. Cutting edge: impairment of dendritic cells and adaptive immunity by Ebola and Lassa viruses. Journal of Immunology. 2003;170:2797–2801. doi: 10.4049/jimmunol.170.6.2797. [DOI] [PubMed] [Google Scholar]
- Martinez O., Johnson J., Manicassamy B., Rong L., Olinger G.G., Hensley L.E., Basler C.F. Zaire Ebola virus entry into human dendritic cells is insensitive to cathepsin L inhibition. Cellular Microbiology. 2010;12:148–157. doi: 10.1111/j.1462-5822.2009.01385.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martinez O., Valmas C., Basler C.F. Ebola virus-like particle-induced activation of NF-kappaB and Erk signaling in human dendritic cells requires the glycoprotein mucin domain. Virology. 2007;364:342–354. doi: 10.1016/j.virol.2007.03.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marzi A., Moller P., Hanna S.L., Harrer T., Eisemann J., Steinkasserer A., Becker S., Baribaud F., Pohlmann S. Analysis of the Interaction of Ebola Virus Glycoprotein with DC-SIGN (Dendritic Cell–Specific Intercellular Adhesion Molecule 3–Grabbing Nonintegrin) and Its Homologue DC-SIGNR. The Journal of Infectious Diseases. 2007;196:S237–S246. doi: 10.1086/520607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mateo M., Carbonnelle C., Reynard O., Kolesnikova L., Nemirov K., Page A., Volchkova V.A., Volchkov V.E. VP24 is a molecular determinant of Ebola virus virulence in guinea pigs. Journal of Infectious Diseases. 2011;204(Suppl 3):S1011–1020. doi: 10.1093/infdis/jir338. [DOI] [PubMed] [Google Scholar]
- Mateo M., Reid S.P., Leung L.W., Basler C.F., Volchkov V.E. Ebolavirus VP24 binding to karyopherins is required for inhibition of interferon signaling. Journal of Virology. 2010;84:1169–1175. doi: 10.1128/JVI.01372-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Medzhitov R., Preston-Hurlburt P., Janeway C.A., Jr. A human homologue of the Drosophila Toll protein signals activation of adaptive immunity. Nature. 1997;388:394–397. doi: 10.1038/41131. [DOI] [PubMed] [Google Scholar]
- Morris D.L., Singer K., Lumeng C.N. Adipose tissue macrophages: phenotypic plasticity and diversity in lean and obese states. Curr Opin Clin Nutr Metab Care. 2011;14:341–346. doi: 10.1097/MCO.0b013e328347970b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mortellaro A., Wong S.C., Fric J., Ricciardi-Castagnoli P. The need to identify myeloid dendritic cell progenitors in human blood. Trends in immunology. 2010;31:18–23. doi: 10.1016/j.it.2009.09.010. [DOI] [PubMed] [Google Scholar]
- Mulherkar N., Raaben M., de la Torre J.C., Whelan S.P., Chandran K. The Ebola virus glycoprotein mediates entry via a non-classical dynamin-dependent macropinocytic pathway. Virology. 2011;419:72–83. doi: 10.1016/j.virol.2011.08.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nanbo A., Imai M., Watanabe S., Noda T., Takahashi K., Neumann G., Halfmann P., Kawaoka Y. Ebolavirus is internalized into host cells via macropinocytosis in a viral glycoprotein-dependent manner. PLoS Pathogens. 2010;6 doi: 10.1371/journal.ppat.1001121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Negredo A., Palacios G., Vazquez-Moron S., Gonzalez F., Dopazo H., Molero F., Juste J., Quetglas J., Savji N., de la Cruz Martinez M., Herrera J.E., Pizarro M., Hutchison S.K., Echevarria J.E., Lipkin W.I., Tenorio A. Discovery of an ebolavirus-like filovirus in europe. PLoS Pathogens. 2011;7:e1002304. doi: 10.1371/journal.ppat.1002304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Neumann G., Feldmann H., Watanabe S., Lukashevich I., Kawaoka Y. Reverse genetics demonstrates that proteolytic processing of the Ebola virus glycoprotein is not essential for replication in cell culture. Journal of virology. 2002;76:406–410. doi: 10.1128/JVI.76.1.406-410.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Neumann G., Geisbert T.W., Ebihara H., Geisbert J.B., Daddario-DiCaprio K.M., Feldmann H., Kawaoka Y. Proteolytic processing of the Ebola virus glycoprotein is not critical for Ebola virus replication in nonhuman primates. Journal of Virology. 2007;81:2995–2998. doi: 10.1128/JVI.02486-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Noda T., Sagara H., Suzuki E., Takada A., Kida H., Kawaoka Y. Ebola virus VP40 drives the formation of virus-like filamentous particles along with GP. Journal of virology. 2002;76:4855–4865. doi: 10.1128/JVI.76.10.4855-4865.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Okumura A., Pitha P.M., Yoshimura A., Harty R.N. Interaction between Ebola virus glycoprotein and host toll-like receptor 4 leads to induction of proinflammatory cytokines and SOCS1. Journal of Virology. 2010;84:27–33. doi: 10.1128/JVI.01462-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Omatsu T., Bak E.J., Ishii Y., Kyuwa S., Tohya Y., Akashi H., Yoshikawa Y. Induction and sequencing of Rousette bat interferon alpha and beta genes. Veterinary Immunology and Immunopathology. 2008;124:169–176. doi: 10.1016/j.vetimm.2008.03.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Piccioli D., Tavarini S., Borgogni E., Steri V., Nuti S., Sammicheli C., Bardelli M., Montagna D., Locatelli F., Wack A. Functional specialization of human circulating CD16 and CD1c myeloid dendritic-cell subsets. Blood. 2007;109:5371–5379. doi: 10.1182/blood-2006-08-038422. [DOI] [PubMed] [Google Scholar]
- Prins K.C., Cardenas W.B., Basler C.F. Ebola virus protein VP35 impairs the function of interferon regulatory factor-activating kinases IKKepsilon and TBK-1. Journal of Virology. 2009;83:3069–3077. doi: 10.1128/JVI.01875-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prins K.C., Delpeut S., Leung D.W., Reynard O., Volchkova V.A., Reid S.P., Ramanan P., Cardenas W.B., Amarasinghe G.K., Volchkov V.E., Basler C.F. Mutations abrogating VP35 interaction with double-stranded RNA render Ebola virus avirulent in guinea pigs. Journal of Virology. 2010;84:3004–3015. doi: 10.1128/JVI.02459-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Randolph G.J., Jakubzick C., Qu C. Antigen presentation by monocytes and monocyte-derived cells. Current Opinion in Immunology. 2008;20:52–60. doi: 10.1016/j.coi.2007.10.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ray R.B., Basu A., Steele R., Beyene A., McHowat J., Meyer K., Ghosh A.K., Ray R. Ebola virus glycoprotein-mediated anoikis of primary human cardiac microvascular endothelial cells. Virology. 2004;321:181–188. doi: 10.1016/j.virol.2003.12.014. [DOI] [PubMed] [Google Scholar]
- Reid S.P., Leung L.W., Hartman A.L., Martinez O., Shaw M.L., Carbonnelle C., Volchkov V.E., Nichol S.T., Basler C.F. Ebola virus VP24 binds karyopherin alpha1 and blocks STAT1 nuclear accumulation. Journal of Virology. 2006;80:5156–5167. doi: 10.1128/JVI.02349-05. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reid S.P., Valmas C., Martinez O., Sanchez F.M., Basler C.F. Ebola virus VP24 proteins inhibit the interaction of NPI-1 subfamily karyopherin alpha proteins with activated STAT1. Journal of Virology. 2007;81:13469–13477. doi: 10.1128/JVI.01097-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reizis B., Bunin A., Ghosh H.S., Lewis K.L., Sisirak V. Plasmacytoid dendritic cells: recent progress and open questions. Annual Review of Immunology. 2011;29:163–183. doi: 10.1146/annurev-immunol-031210-101345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reynard O., Borowiak M., Volchkova V.A., Delpeut S., Mateo M., Volchkov V.E. Ebolavirus glycoprotein GP masks both its own epitopes and the presence of cellular surface proteins. Journal of Virology. 2009;83:9596–9601. doi: 10.1128/JVI.00784-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Robinson M.J., Sancho D., Slack E.C., LeibundGut-Landmann S., Reis e Sousa C. Myeloid C-type lectins in innate immunity. Nature immunology. 2006;7:1258–1265. doi: 10.1038/ni1417. [DOI] [PubMed] [Google Scholar]
- Rodriguez-Manzanet R., DeKruyff R., Kuchroo V.K., Umetsu D.T. The costimulatory role of TIM molecules. Immunological Reviews. 2009;229:259–270. doi: 10.1111/j.1600-065X.2009.00772.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ruf W. Emerging roles of tissue factor in viral hemorrhagic fever. Trends in immunology. 2004;25:461–464. doi: 10.1016/j.it.2004.07.002. [DOI] [PubMed] [Google Scholar]
- Ryabchikova E.I., Kolesnikova L.V., Luchko S.V. An analysis of features of pathogenesis in two animal models of Ebola virus infection. The Journal of Infectious Diseases. 1999;179:S199–S202. doi: 10.1086/514293. [DOI] [PubMed] [Google Scholar]
- Saeed M.F., Kolokoltsov A.A., Albrecht T., Davey R.A. Cellular entry of Ebola virus involves uptake by a macropinocytosis-like mechanism and subsequent trafficking through early and late endosomes. PLoS Pathogens. 2010;6 doi: 10.1371/journal.ppat.1001110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sanchez A., Lukwiya M., Bausch D., Mahanty S., Sanchez A.J., Wagoner K.D., Rollin P.E. Analysis of human peripheral blood samples from fatal and nonfatal cases of Ebola (Sudan) hemorrhagic fever: cellular responses, virus load, and nitric oxide levels. Journal of Virology. 2004;78:10370–10377. doi: 10.1128/JVI.78.19.10370-10377.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sanchez A.G., Thomas W., Feldmann, Heinz . Lippincott Williams and Wilkins; Filoviridae: 2007. Marburg and Ebola Viruses. [Google Scholar]
- Schnittler H.J., Feldmann H. Marburg and Ebola hemorrhagic fevers: does the primary course of infection depend on the accessibility of organ-specific macrophages? Clinical Infectious Diseases. 1998;27:404–406. doi: 10.1086/517704. [DOI] [PubMed] [Google Scholar]
- Schnittler H.J., Feldmann H. Viral hemorrhagic fever – a vascular disease? Thrombosis and Haemostasis. 2003;89:967–972. [PubMed] [Google Scholar]
- Schornberg K., Matsuyama S., Kabsch K., Delos S., Bouton A., White J. Role of endosomal cathepsins in entry mediated by the Ebola virus glycoprotein. Journal of Virology. 2006;80:4174–4178. doi: 10.1128/JVI.80.8.4174-4178.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shabman R.S., Gulcicek E.E., Stone K.L., Basler C.F. The Ebola virus VP24 protein prevents hnRNP C1/C2 binding to karyopherin α1 and partially alters its nuclear import. J Infect Dis. 2011;204(Supply 3):S904–S910. doi: 10.1093/infdis/jir323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shabo I., Svanvik J. Expression of macrophage antigens by tumor cells. Advances in experimental medicine and biology. 2011;714:141–150. doi: 10.1007/978-94-007-0782-5_7. [DOI] [PubMed] [Google Scholar]
- Shimojima M., Takada A., Ebihara H., Neumann G., Fujioka K., Irimura T., Jones S., Feldmann H., Kawaoka Y. Tyro3 family-mediated cell entry of Ebola and Marburg viruses. Journal of Virology. 2006;80:10109–10116. doi: 10.1128/JVI.01157-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Simmons G., Reeves J.D., Grogan C.C., Vandenberghe L.H., Baribaud F., Whitbeck J.C., Burke E., Buchmeier M.J., Soilleux E.J., Riley J.L., Doms R.W., Bates P., Pohlmann S. DC-SIGN and DC-SIGNR bind ebola glycoproteins and enhance infection of macrophages and endothelial cells. Virology. 2003;305:115–123. doi: 10.1006/viro.2002.1730. [DOI] [PubMed] [Google Scholar]
- Simmons G., Wool-Lewis R.J., Baribaud F., Netter R.C., Bates P. Ebola virus glycoproteins induce global surface protein down-modulation and loss of cell adherence. Journal of Virology. 2002;76:2518–2528. doi: 10.1128/jvi.76.5.2518-2528.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Steinman R.M. Decisions About Dendritic Cells: Past, Present, and Future. Annual Review of Immunology. 2011 doi: 10.1146/annurev-immunol-100311-102839. [DOI] [PubMed] [Google Scholar]
- Steinman R.M., Idoyaga J. Features of the dendritic cell lineage. Immunological Reviews. 2010;234:5–17. doi: 10.1111/j.0105-2896.2009.00888.x. [DOI] [PubMed] [Google Scholar]
- Steinman R.M., Idoyaga J. Features of the dendritic cell lineage. Immunological Reviews. 2010;234:5–17. doi: 10.1111/j.0105-2896.2009.00888.x. [DOI] [PubMed] [Google Scholar]
- Stroher U., West E., Bugany H., Klenk H.D., Schnittler H.J., Feldmann H. Infection and activation of monocytes by Marburg and Ebola viruses. Journal of Virology. 2001;75:11025–11033. doi: 10.1128/JVI.75.22.11025-11033.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sullivan N.J., Peterson M., Yang Z.Y., Kong W.P., Duckers H., Nabel E., Nabel G.J. Ebola virus glycoprotein toxicity is mediated by a dynamin-dependent protein-trafficking pathway. Journal of Virology. 2005;79:547–553. doi: 10.1128/JVI.79.1.547-553.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Swanepoel R., Smit S.B., Rollin P.E., Formenty P., Leman P.A., Kemp A., Burt F.J., Grobbelaar A.A., Croft J., Bausch D.G., Zeller H., Leirs H., Braack L.E., Libande M.L., Zaki S., Nichol S.T., Ksiazek T.G., Paweska J.T. Studies of reservoir hosts for Marburg virus. Emerging Infectious Diseases. 2007;13:1847–1851. doi: 10.3201/eid1312.071115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Swenson D.L., Warfield K.L., Kuehl K., Larsen T., Hevey M.C., Schmaljohn A., Bavari S., Aman M.J. Generation of Marburg virus-like particles by co-expression of glycoprotein and matrix protein. FEMS Immunology and Medical Microbiology. 2004;40:27–31. doi: 10.1016/S0928-8244(03)00273-6. [DOI] [PubMed] [Google Scholar]
- Takada A., Fujioka K., Tsuiji M., Morikawa A., Higashi N., Ebihara H., Kobasa D., Feldmann H., Irimura T., Kawaoka Y. Human Macrophage C-Type Lectin Specific for Galactose and N-Acetylgalactosamine Promotes Filovirus Entry. Journal of Virology. 2004;78:2943–2947. doi: 10.1128/JVI.78.6.2943-2947.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Takada A., Watanabe S., Ito H., Okazaki K., Kida H., Kawaoka Y. Downregulation of [beta]1 Integrins by Ebola Virus Glycoprotein: Implication for Virus Entry. Virology. 2000;278:20–26. doi: 10.1006/viro.2000.0601. [DOI] [PubMed] [Google Scholar]
- Towner J.S., Amman B.R., Sealy T.K., Carroll S.A., Comer J.A., Kemp A., Swanepoel R., Paddock C.D., Balinandi S., Khristova M.L., Formenty P.B., Albarino C.G., Miller D.M., Reed Z.D., Kayiwa J.T., Mills J.N., Cannon D.L., Greer P.W., Byaruhanga E., Farnon E.C., Atimnedi P., Okware S., Katongole-Mbidde E., Downing R., Tappero J.W., Zaki S.R., Ksiazek T.G., Nichol S.T., Rollin P.E. Isolation of genetically diverse Marburg viruses from Egyptian fruit bats. PLoS Pathogens. 2009;5:e1000536. doi: 10.1371/journal.ppat.1000536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Towner J.S., Pourrut X., Albarino C.G., Nkogue C.N., Bird B.H., Grard G., Ksiazek T.G., Gonzalez J.P., Nichol S.T., Leroy E.M. Marburg virus infection detected in a common African bat. PLoS ONE. 2007;2:e764. doi: 10.1371/journal.pone.0000764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Valmas C., Basler C.F. Marburg virus VP40 antagonizes interferon signaling in a species-specific manner. Journal of Virology. 2011;85:4309–4317. doi: 10.1128/JVI.02575-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Valmas C., Grosch M.N., Schumann M., Olejnik J., Martinez O., Best S.M., Krahling V., Basler C.F., Muhlberger E. Marburg virus evades interferon responses by a mechanism distinct from ebola virus. PLoS Pathogens. 2010;6:e1000721. doi: 10.1371/journal.ppat.1000721. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vestweber D. Regulation of endothelial cell contacts during leukocyte extravasation. Current Opinion in Cell Biology. 2002;14:587–593. doi: 10.1016/s0955-0674(02)00372-1. [DOI] [PubMed] [Google Scholar]
- Volchkov V.E., Feldmann H., Volchkova V.A., Klenk H.D. Processing of the Ebola virus glycoprotein by the proprotein convertase furin. Proc Natl Acad Sci U S A. 1998;95:5762–5767. doi: 10.1073/pnas.95.10.5762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wahl-Jensen V., Kurz S., Feldmann F., Buehler L.K., Kindrachuk J., DeFilippis V., da Silva Correia J., Fruh K., Kuhn J.H., Burton D.R., Feldmann H. Ebola virion attachment and entry into human macrophages profoundly effects early cellular gene expression. PLoS Negl Trop Dis. 2011;5:e1359. doi: 10.1371/journal.pntd.0001359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wahl-Jensen V., Kurz S.K., Hazelton P.R., Schnittler H.J., Stroher U., Burton D.R., Feldmann H. Role of Ebola virus secreted glycoproteins and virus-like particles in activation of human macrophages. Journal of Virology. 2005;79:2413–2419. doi: 10.1128/JVI.79.4.2413-2419.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wahl-Jensen V.M., Afanasieva T.A., Seebach J., Stroher U., Feldmann H., Schnittler H.J. Effects of Ebola virus glycoproteins on endothelial cell activation and barrier function. Journal of Virology. 2005;79:10442–10450. doi: 10.1128/JVI.79.16.10442-10450.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Warfield K.L., Aman M.J. Advances in virus-like particle vaccines for filoviruses. Journal of Infectious Diseases. 2011;204(Suppl 3):S1053–1059. doi: 10.1093/infdis/jir346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Warfield K.L., Bosio C.M., Welcher B.C., Deal E.M., Mohamadzadeh M., Schmaljohn A., Aman M.J., Bavari S. Ebola virus-like particles protect from lethal Ebola virus infection. Proc Natl Acad Sci U S A. 2003;100:15889–15894. doi: 10.1073/pnas.2237038100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Warfield K.L., Posten N.A., Swenson D.L., Olinger G.G., Esposito D., Gillette W.K., Hopkins R.F., Costantino J., Panchal R.G., Hartley J.L., Aman M.J., Bavari S. Filovirus-like particles produced in insect cells: immunogenicity and protection in rodents. Journal of Infectious Diseases. 2007;196(Suppl 2):S421–429. doi: 10.1086/520612. [DOI] [PubMed] [Google Scholar]
- Watanabe S., Takada A., Watanabe T., Ito H., Kida H., Kawaoka Y. Functional Importance of the Coiled-Coil of the Ebola Virus Glycoprotein. Journal of Virology. 2000;74:10194–10201. doi: 10.1128/jvi.74.21.10194-10201.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Watanabe S., Watanabe T., Noda T., Takada A., Feldmann H., Jasenosky L.D., Kawaoka Y. Production of Novel Ebola Virus-Like Particles from cDNAs: an Alternative to Ebola Virus Generation by Reverse Genetics. Journal of Virology. 2004;78:999–1005. doi: 10.1128/JVI.78.2.999-1005.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wauquier N., Becquart P., Padilla C., Baize S., Leroy E.M. Human fatal zaire ebola virus infection is associated with an aberrant innate immunity and with massive lymphocyte apoptosis. PLoS Negl Trop Dis. 2010;4 doi: 10.1371/journal.pntd.0000837. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weissenhorn W., Carfi A., Lee K.H., Skehel J.J., Wiley D.C. Crystal structure of the Ebola virus membrane fusion subunit, GP2, from the envelope glycoprotein ectodomain. Molecular Cell. 1998;2:605–616. doi: 10.1016/s1097-2765(00)80159-8. [DOI] [PubMed] [Google Scholar]
- Wong A.C., Sandesara R.G., Mulherkar N., Whelan S.P., Chandran K. A forward genetic strategy reveals destabilizing mutations in the Ebolavirus glycoprotein that alter its protease dependence during cell entry. Journal of Virology. 2010;84:163–175. doi: 10.1128/JVI.01832-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wool-Lewis R.J., Bates P. Endoproteolytic processing of the ebola virus envelope glycoprotein: cleavage is not required for function. Journal of Virology. 1999;73:1419–1426. doi: 10.1128/jvi.73.2.1419-1426.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wyers M., Formenty P., Cherel Y., Guigand L., Fernandez B., Boesch C., Le Guenno B. Histopathological and Immunohistochemical Studies of Lesions Associated with Ebola Virus in a Naturally Infected Chimpanzee. The Journal of Infectious Diseases. 1999;179:S54–S59. doi: 10.1086/514300. [DOI] [PubMed] [Google Scholar]
- Xiao S., Zhu B., Jin H., Zhu C., Umetsu D.T., DeKruyff R.H., Kuchroo V.K. Tim-1 stimulation of dendritic cells regulates the balance between effector and regulatory T cells. European Journal of Immunology. 2011;41:1539–1549. doi: 10.1002/eji.201040993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang Z., Delgado R., Xu L., Todd R.F., Nabel E.G., Sanchez A., Nabel G.J. Distinct cellular interactions of secreted and transmembrane Ebola virus glycoproteins. Science. 1998;279:1034–1037. doi: 10.1126/science.279.5353.1034. [DOI] [PubMed] [Google Scholar]
- Yang Z.Y., Duckers H.J., Sullivan N.J., Sanchez A., Nabel E.G., Nabel G.J. Identification of the Ebola virus glycoprotein as the main viral determinant of vascular cell cytotoxicity and injury. Nature Medicine. 2000;6:886–889. doi: 10.1038/78645. [DOI] [PubMed] [Google Scholar]
- Ye L., Lin J., Sun Y., Bennouna S., Lo M., Wu Q., Bu Z., Pulendran B., Compans R.W., Yang C. Ebola virus-like particles produced in insect cells exhibit dendritic cell stimulating activity and induce neutralizing antibodies. Virology. 2006 doi: 10.1016/j.virol.2006.03.021. [DOI] [PubMed] [Google Scholar]
- Yonezawa A., Cavrois M., Greene W.C. Studies of Ebola Virus Glycoprotein-Mediated Entry and Fusion by Using Pseudotyped Human Immunodeficiency Virus Type 1 Virions: Involvement of Cytoskeletal Proteins and Enhancement by Tumor Necrosis Factor Alpha. Journal of Virology. 2005;79:918–926. doi: 10.1128/JVI.79.2.918-926.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zaki S.R., Shieh W.J., Greer P.W., Goldsmith C.S., Ferebee T., Katshitshi J., Tshioko F.K., Bwaka M.A., Swanepoel R., Calain P., Khan A.S., Lloyd E., Rollin P.E., Ksiazek T.G., Peters C.J. A novel immunohistochemical assay for the detection of Ebola virus in skin: implications for diagnosis, spread, and surveillance of Ebola hemorrhagic fever. Commission de Lutte contre les Epidemies a Kikwit. Journal of Infectious Diseases. 1999;179(Suppl 1):S36–47. doi: 10.1086/514319. [DOI] [PubMed] [Google Scholar]
- Zampieri C.A., Fortin J.F., Nolan G.P., Nabel G.J. The ERK mitogen-activated protein kinase pathway contributes to Ebola virus glycoprotein-induced cytotoxicity. Journal of Virology. 2007;81:1230–1240. doi: 10.1128/JVI.01586-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zuckerman S.H., Ackerman S.K., Douglas S.D. Long-term human peripheral blood monocyte cultures: establishment, metabolism and morphology of primary human monocyte-macrophage cell cultures. Immunology. 1979;38:401–411. [PMC free article] [PubMed] [Google Scholar]


