Abstract
Ultrasonography has advantages over other imaging modalities in terms of availability and comfort, safety, and diagnostic potential. Operating costs are low compared with both computed tomography (CT) and magnetic resonance imaging (MRI). The portable equipment is accessible at locations distant from medical centers. Importantly, ultrasonography is performed while patients lie in a comfortable position, without pain or claustrophobia.
Keywords: Ultrasound, Orthopedic surgery, Safety, No radiation, Soft tissue
INTRODUCTION
Ultrasonography is a totally safe noninvasive imaging technique. In contrast to computed tomography (CT) and X-rays, it does not emit ionizing radiation. Unlike magnetic resonance imaging (MRI), it is safe for all patients, including those with cardiac pacemakers and metal implants, without any contraindications.
With its outstanding diagnostic benefits, notably high resolution and capability of real time assessment[1,2], orthopedic ultrasound is often referred to as the “orthopedic surgeon’s stethoscope”. Its high resolution enables detection of tendon tears, tiny calcifications, and foreign bodies. Calcification in soft tissue and destructive and reparative hypertrophic changes on bone surfaces are more readily apparent, and at an earlier stage, than with plain X-rays, CT or MRI. Ultrasonography thus enhances early detection of pathologies.
The real time capability of musculoskeletal sonography enables dynamic assessment of joint and tendon movements and stability[3], and detection of fracture union and reunion, structural abnormalities, infection, ligamentous injury[4], nerve compression and mechanical impingement between orthopedic hardware and soft tissue structures. Beyond diagnostics, real time capability is useful for guiding therapeutic interventions, such as cyst aspiration. The fact that ultrasound examinations may be easily repeated as often as necessary, makes this modality useful for monitoring treatment.
Due to its flexibility and precision in the selection of the point of examination and in the field of vision, musculoskeletal ultrasonography has spatial, as well as temporal benefits. The possibility of placing the sonographic probe at the point of maximal tenderness increases the likelihood of detecting abnormalities, and ensures clinical relevance of the examination. Sonography affords comparisons of targeted findings with those of the contralateral side, and also enables under “vision” biopsy or joint aspiration.
Of the many indications for musculoskeletal ultrasonography, the evaluation of soft tissue pathology is particularly common[5]. In addition, ultrasonography is useful for the detection of fluid collection, and for visualization of cartilage and bone surfaces. Color or power Doppler provides important physiological information, including that relating to the vascular system. The capability of ultrasonography in delineating structures according to their echo textures results in excellent pictorial representation. This imaging principle is based on physical changes in composition, as compared to imaging with MRI, which is based on changes in chemical composition.
This article reviews the contribution of sonography to the evaluation of the musculoskeletal system.
NECK REGION
Ultrasonography is preferable to radiography for the early detection of calcification in soft tissue in the neck region. In the investigation of suspected soft tissue tumors, such as in acute swelling of sterno-cleido mastoideus, and in cases of congenital muscular torticollis, ultrasound can often distinguish between a true tumor mass and a hematoma or muscle rupture[6].
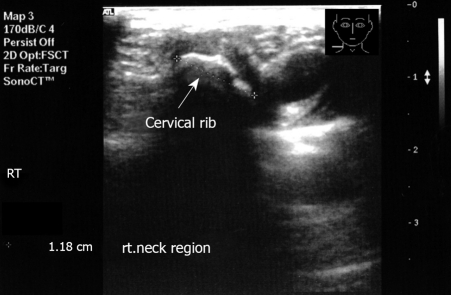
The appearance of an echogenic structure with acoustic shadowing in the region of tenderness may indicate a cervical rib[7] (Figures 1 and 2). Fracture of the clavicle in the newborn[8] and congenital pseudoarthrosis of the clavicle can also be diagnosed with ultrasound[9].
Figure 1.
Transverse imaging of the right neck region. Note the echogenic structure with acoustic shadow.
Figure 2.
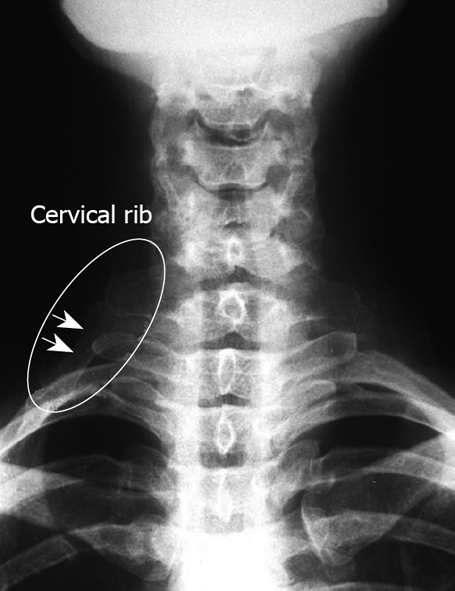
X-ray corresponding to Figure 1. Note the cervical rib.
SHOULDER
At our medical center, the shoulder is one of the bodily areas for which musculoskeletal sonography is most requested[10]. Age-related degenerative changes and overuse syndrome with degenerative tears leads many patients to seek medical treatment for painful shoulder.
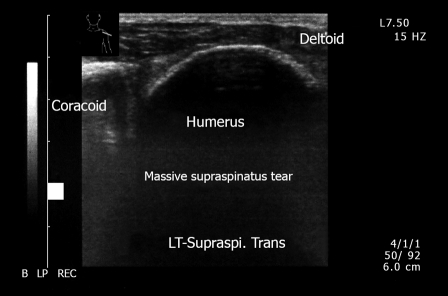
Suspicion of rotator cuff pathology is the most important indication for shoulder sonography. Musculoskeletal ultrasound enables early detection of changes in tendons, in bursae-rotator cuff and in cartilage, thus leading to adequate treatment. Tears can be seen, located, and measured[11-13] (Figures 3, 4 and 5). Their full anatomical extent can be assessed. Calcification is more visible with ultrasound than with MRI (Figure 6) and the capability of precise location enables assessment of treatment. Sonographic palpation and comparison with the other shoulder is easily performed.
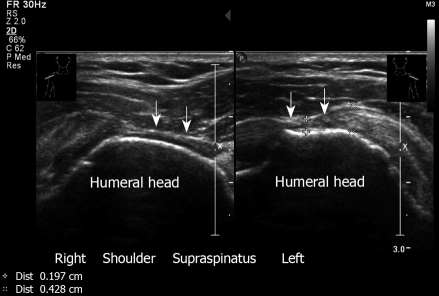
Figure 3.
Partial thickness tear of supraspinatus. Right and left shoulder. Note the narrowing of the tendon. Transverse sonogram. A 70-year old male who presents with bilateral shoulder pain and has a painful arc at clinical examination.
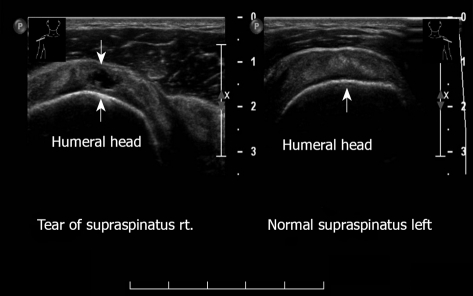
Figure 4.
Transverse sonogram, supraspinatus right and left shoulder. Anechoic defect. Partial thickness tear, right. Left: Normal supraspinatus.
Figure 5.
Massive full-thickness tear of supraspinatus. Left shoulder. Non visualization of tendon. This 81-year old female has severe shoulder pain that increases at night.
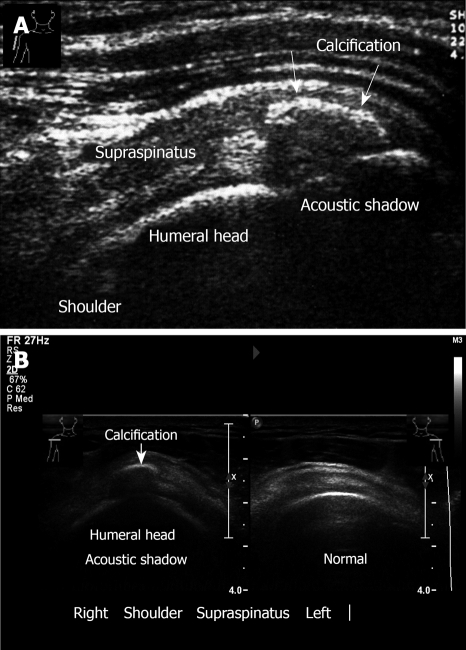
Figure 6.
Ultrasound examination of calcification. A: Calcific tendinitis. Calcification in the supraspinatus tendon, longitudinal view. Note: Acoustic shadow behind the calcification. A 29-year old woman presents with a short history (3 d) of incapacitating shoulder pain and with severe restriction in the range of shoulder movement; B: Transverse sonogram. Calcification of supraspinatus, right. Left normal sonogram.
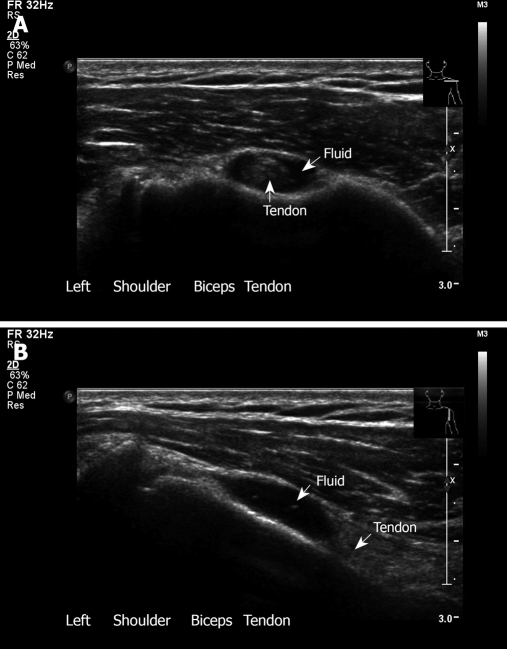
The presence of fluid around the biceps tendon or subdeltoid bursa may indicate a bursitis infection or tear (Figure 7). Lesions associated with rotator cuff disease, such as long biceps tenosynovitis and sub-acromial deltoid bursitis, can be visualized by ultrasound.
Figure 7.
Ultrasound examination of biceps tendon. A: Bicipital tendinitis. Transverse sonogram. The tendon is surrounded by fluid. This 33-year old woman presents with pain and local tenderness in the area of the bicipital groove; B: Longitudinal view with fluid around the biceps.
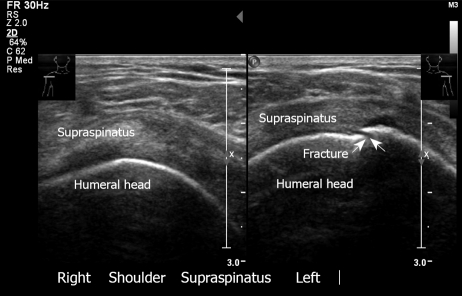
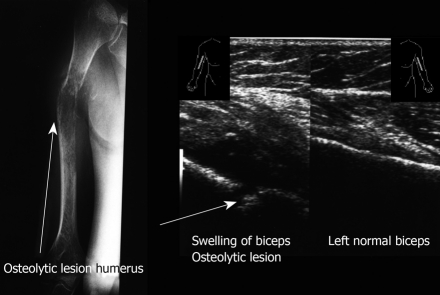
Ultrasound can detect fractures in the head and shaft of the humerus, especially the greater tuberosity (Figure 8). Greater tuberosity fractures are characterized by sonography as cortical discontinuity, and may appear as a cortical gap or step-off (double line)[14]. They should be included in the differential diagnosis of every shoulder sonography examination, even in the absence of a clear history of trauma. Osteolytic lesions of the proximal humerus can also be detected in ultrasound (Figure 9).
Figure 8.
Fracture of greater tuberosity, left. Note the discontinuity of the bone. The right shoulder has normal appearance. Transverse sonogram.
Figure 9.
Longitudinal sonogram. Swelling of soft tissue with severe irregularity of the cortex right humerus. Left biceps normal. X-ray of the right arm demonstrates the osteolytic lesion of the right humerus. A 75-year old man presents with swelling of the right humerus, limitation of movement, night pain and weight loss.
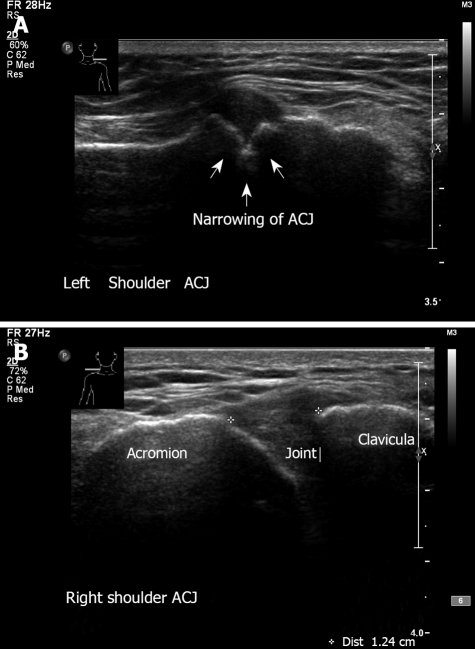
Since conventional radiography does not adequately diagnose symptoms of shoulder pain, a sonographic examination is recommended as part of the early diagnostic protocol[15,16]. Ultrasound is useful in detecting pathologies in the acromioclavicular joint, such as acromioclavicular joint arthritis and dislocation (Figure 10)[17], as well as septic arthritis of the sternoclavicular[18] and acromioclavicular joints[19].
Figure 10.
Ultrasound examination of acromioclavicular joint. A: Left shoulder - A-C arthritis. Note the irregularity and narrowing of the acromioclavicular joint. Erosive changes at the articular surface of the joint. A 65-year old man with a long history of pain and tenderness related to the acromioclavicular joint; B: Normal right acromioclavicular joint with open joint space.
The effectiveness of sonography has been demonstrated for the evaluation and diagnosis of Hill-Sachs lesions, which frequently follow anterior gleno-humeral dislocation of the shoulder[20]. Moreover, ultrasound can be used to assess sonographic images in hemiplegic shoulders of stroke patients[21].
Dynamic sonography enables direct visualization of the relationships between the acromion, humeral head, and intervening soft tissues during active shoulder motion, and can provide information on the potential intrinsic and extrinsic causes of shoulder impingement syndrome[22]. In cases of frozen shoulder, abnormal gliding and rotational movement are apparent, with the entire soft tissue moving as a single unit (deltoid, rotator cuff. and humeral head). The capability of ultrasound in detecting a full thickness tear is impressive. Drakeford et al[23] reported sensitivity of 92% and specificity of 95%. Ultrasound can also be used to detect tears of pectoral muscle (Figure 11).
Figure 11.
Longitudinal sonogram. Demonstrates a large pectoralis tear left. A 23-year old soldier felt a pop when he was lifting a wounded friend.
ARM-ELBOW
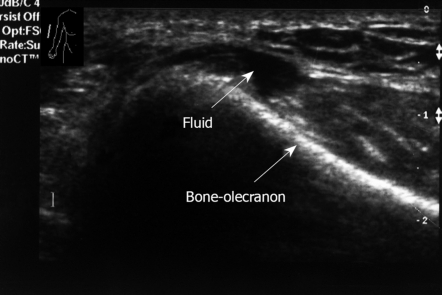
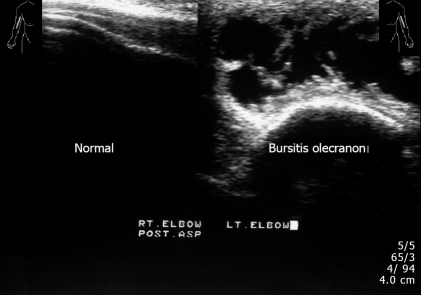
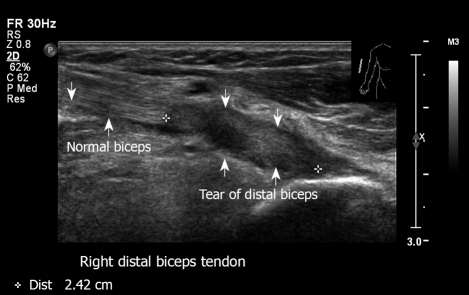
Ultrasound is useful for examining proximal muscles acting on the shoulder and elbow. Muscle compartments are divided into flexor and extensor groups. Ultrasound can detect common tendon injuries, such as “tennis” and “golfer” elbow, in which swelling, thickening, and accumulation of fluid is apparent[24,25]. Musculoskeletal ultrasound is an effective imaging technique for the diagnosis of olecranon bursitis, especially its early manifestation. Sensitive detection of small fluid collection is possible (Figure 12), as well as differentiation between soft tissue and bone lesion, and between septic and non septic elbow. Ultrasound examination allows detection of effusions, synovial proliferation, calcification, loose bodies, rheumatoid nodules, gout tophi, and septic processes (Figure 13)[26,27], as well as distal biceps tendon lesions (Figure 14).
Figure 12.
Longitudinal sonogram, right elbow. Small amount of fluid posterior aspect. No erosive changes in the bone.
Figure 13.
Longitudinal view, left elbow. Swelling and fluid of soft tissue. Reactive elbow joint effusion, corresponding to bursitis. Right elbow normal appearance. This 60-year old man had pain and swelling over the dorsal aspect of the left elbow, olecranon bursitis.
Figure 14.
Right distal biceps tendon tear in the area of insertion. Proximal biceps look normal. This 62-year old man felt a severe sudden sharp pain in the distal humerus region after lifting a heavy suitcase.
HAND
Ultrasound examination of the flexor and extensor tendons and ligaments of the finger may reveal such pathologies as tendinopathy, tenosynovitis, ruptures, and neoplasia (Figure 15 ). Cystic or solid swelling palpable tumors and occult ganglion can be observed[28-30]. Foreign bodies often remain undetected in penetrating wounds and lacerations, pathologies frequently treated in the emergency room. Sonography is useful in the localization and removal of soft tissue foreign bodies[31,32], and in the detection of greenstick fractures of the distal radius and ulna[33].
Figure 15.
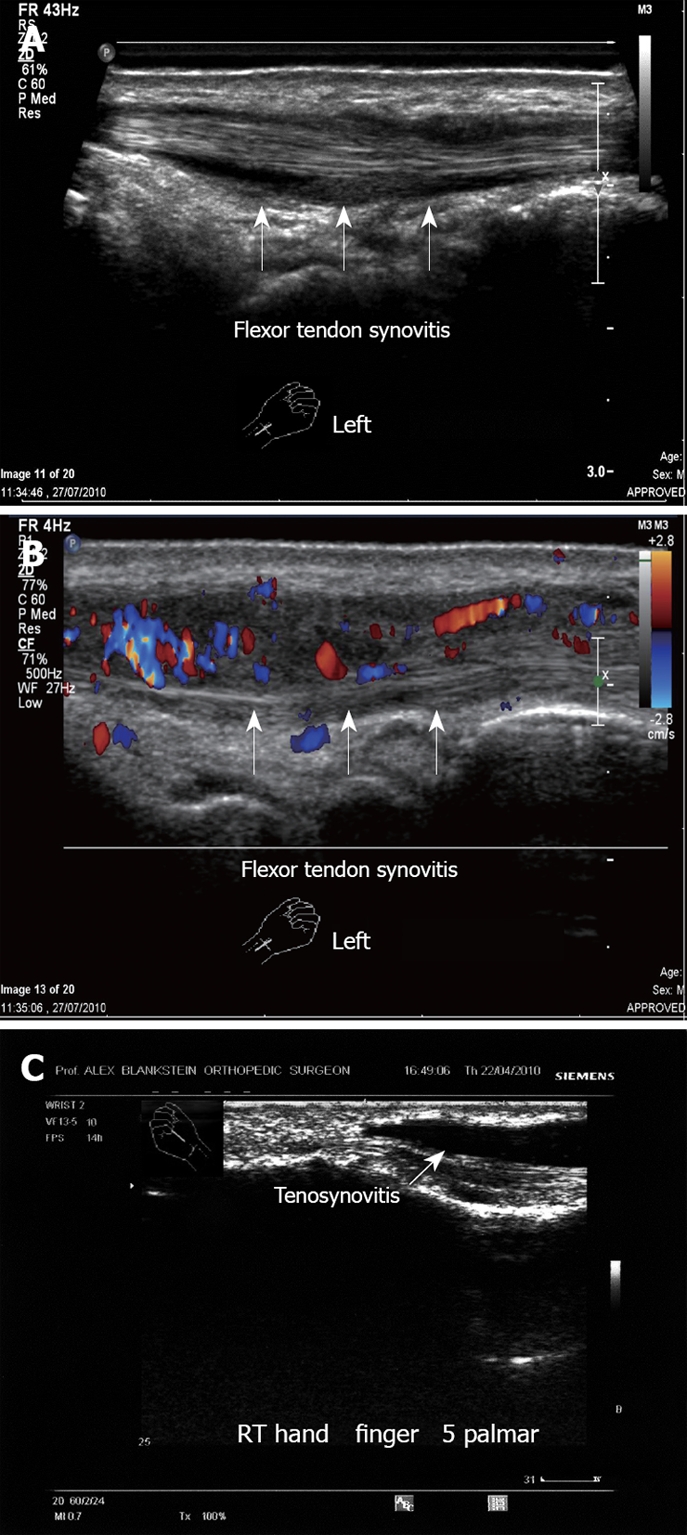
Ultrasound examination of flexor tendons synovitis. A: Left hand flexor tendon synovitis. Note the fluid around the tendon. No tear is demonstrated; B: Left hand flexor tendon synovitis. Note the hyper-vascularity with the vascular inflammation signs; C: Flexor tendon synovitis, right hand mid-phalanx. Note the large amount of clear fluid around the tendon. This 55-year old woman presented with acute pain in the palmar aspect of the hand with irregular synovial thickening, increased fluid and hypervascularity.
The sonographic examination of a patient with suspected traumatic Mallet finger is important for the differentiation between traumatic Mallet finger and flexion deformity due to rheumatoid arthritis or osteoarthritis[34].
WRIST
Ultrasound can be helpful in differentiating synovial and teno-synovial pathology, and in examining pathological and morphostructural changes of the median nerve in carpal tunnel syndrome.
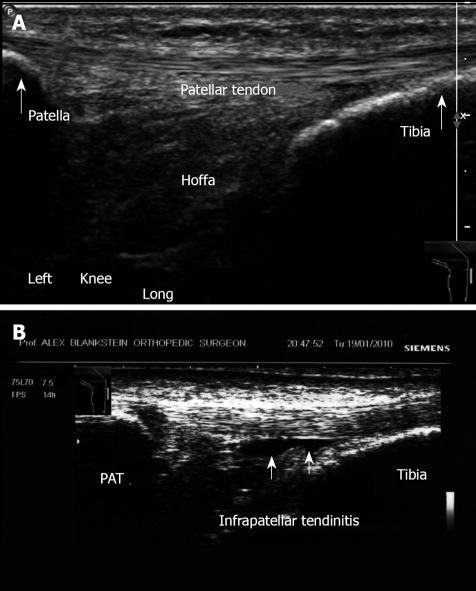
KNEE
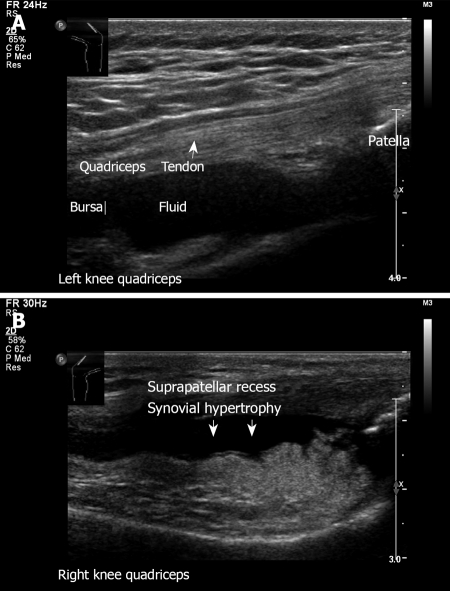
While, clinical examination of the knee joint is relatively easy, very small effusions and synovitic proliferations may be missed. Ultrasound can detect these, as well as fluid in the knee and in the area of the tendons (Figure 16). Further, ultrasound is useful for assessing ligaments, and for diagnosing pathologies relating to anterior knee pain[35-37].
Figure 16.
Ultrasound examination of knee quadriceps. A: Left knee longitudinal view. Transducer on the anterior aspect of the knee. Note the fluid in the suprapatellar recess. Normal quadriceps tendon with its insertion to the patella; B: Similar transducer position demonstrating synovial hypertrophy. A 68-year old woman with rheumatoid arthritis presented with pain and swelling of the right anterior knee.
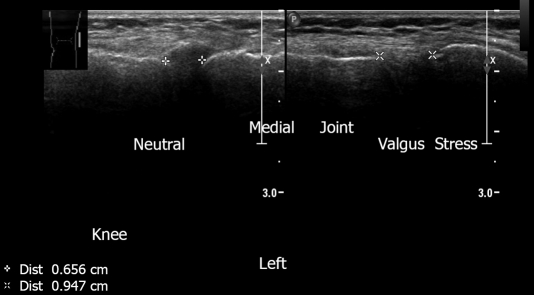
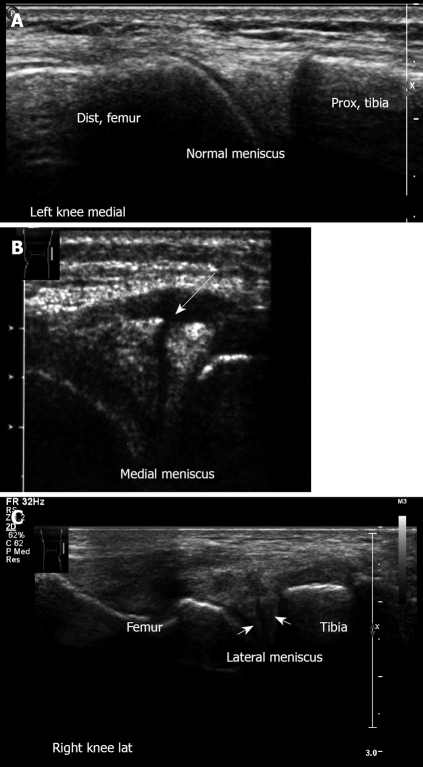
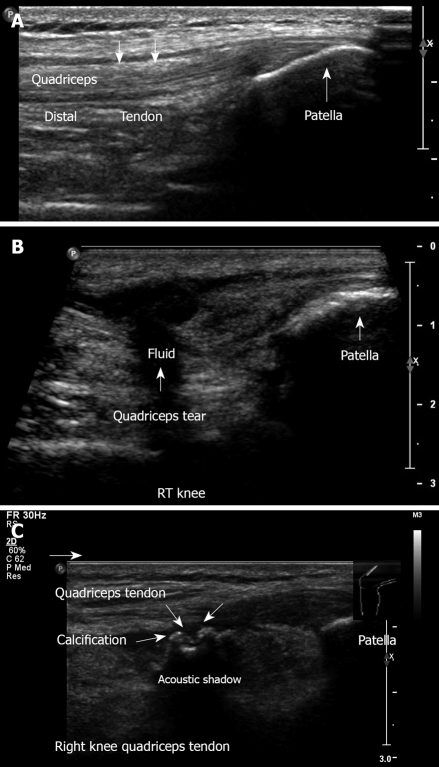
Dynamic sonographic examination, with stress tests (Figure 17), can demonstrate instability and meniscal pathology (Figure 18)[38]. Synovial cysts, medial collateral ligaments, lateral collateral ligaments and tears of tendon can be assessed. Ultrasound is also used in diagnosis of patellar and quadriceps tears (Figure 19 ).
Figure 17.
Left knee medial aspect. Ultrasound demonstrates medial collateral ligament. Joint space is normal. Neutral position. Joint space measures 0.656 cm. The same area under valgus stress, demonstrating joint space of 0.947 cm, pointing to medial collateral ligament insufficiency, clinically manifested by mild knee instability.
Figure 18.
Ultrasound examination of meniscus. A: Left knee medial aspect, longitudinal sonogram. Medial meniscus anterior horn. Note the triangle-shaped hyperechoic structure of the normal medial meniscus; B: Medial meniscus lesion. Note the cleft and irregularity of the torn meniscus. This young football player suffered an acute twisting injury. Clinically he had pain with mild swelling on the medial aspect, there was a joint effusion with medial line tenderness. Mac-Murray and Apley tests were positive over the medial meniscus; Right knee lateral meniscus lesion. Note the irregularity of the torn lateral meniscus.
Figure 19.
Ultrasound examination of patellar and quadriceps tears. A: Longitudinal ultrasound image obtained in the midline, demonstrating the anterior knee, quadriceps tendon with its insertion to the patella, suprapatellar recess, and the patella. No effusion is visible; B: Longitudinal view. Complete quadriceps tendon tear. This 62-year old physician suffered direct trauma to his right knee when falling down stairs; C: Quadriceps tendinitis with calcification of the right knee. This 50-year old man had a contusion with hematoma of the quadriceps muscle one year ago.
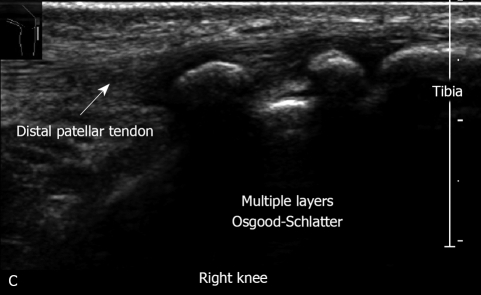
Sonographic examination of the knee has been proposed as a simple and reliable method for diagnosis of Osgood-Schlatter (Figure 20) disease[39] and patella bipartite[40].
Figure 20.
Right knee Osgood-Schlatter disease. Note the severe irregularity of tibial tuberosity. This 14-year old football player has severe pain and swelling of the tibial tuberosity,
In medial collateral ligament (MCL) injury, the combination of sonographic findings with those from a real time sonography valgus stress test can support the clinical diagnosis of an MCL stretch or tear, and pinpoint the exact location of the isolated MCL injury, thus facilitating proper treatment[41].
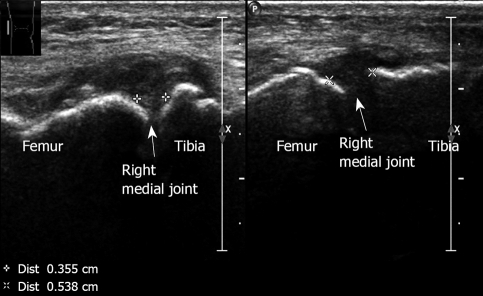
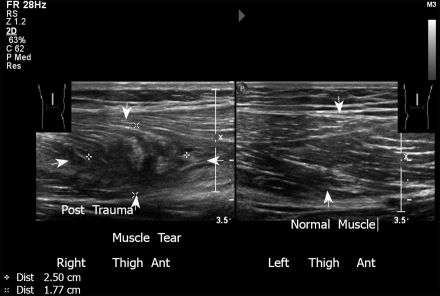
Ultrasound can suggest an early diagnosis of osteoarthritis (Figure 21) by demonstrating joint effusion, synovial thickening, bony changes, patello femoral changes, articular cartilage changes, peripheral tears and lesions of the tendon, and meniscal pathologies, such as meniscal cysts, and Baker cyst[42]. Pathologies can be detected by ultrasound at a stage in which plain radiographs still appear normal. Muscle and ligament pathology (Figures 22, 23 and 24), and tumors of the tibial tuberosity can be diagnosed[43], as well as fractures of the patella (Figure 25)[44].
Figure 21.
Osteoarthritis medial aspect, right knee. Medial joint space narrowing with osteophyte formation and thickening of the medial collateral ligament, measured 0.355 cm. Lateral joint with normal appearance measured 0.538 cm. A 75-year old woman with typical findings of osteoarthritic changes.
Figure 22.
Longitudinal sonogram of the thigh. A young basketball player presented with pain over the anterior aspect of the distal right femur. Note the irregularity with partial tear of the muscle. Left thigh: Normal appearance.
Figure 23.
Ultrasound examination of patellar tendon. A: Longitudinal view. Anterior aspect. Ultrasound image shows the patellar tendon from its origin in the patella into the tibial tuberosity left knee; B: Infrapatellar tendinitis. Note fluid accumulation deep to the patellar tendon.
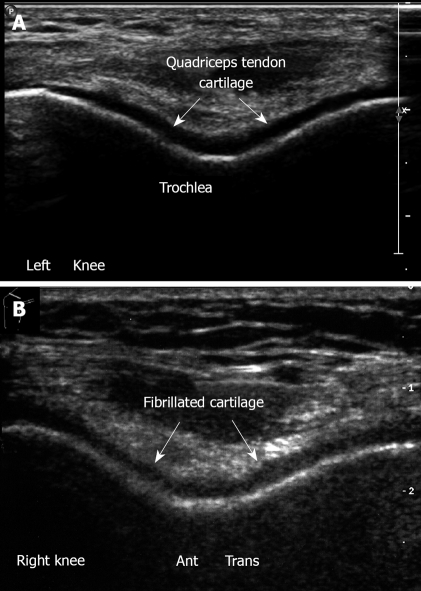
Figure 24.
Ultrasound examination of knee cartilage. A: Left knee. Flexion position. Anterior transverse view. Note trochlear cartilage of femur. The hyaline cartilage is a hypoechoic homogenous structure with sharp margins, overlying the bright hyperechoic line of subchondral bone; B: Cartilage lesion. Anterior transverse right knee in flexion, irregularity and narrowing of the hyaline cartilage which is roughened and fibrillated.
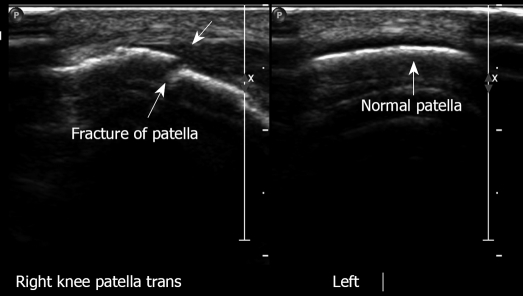
Figure 25.
Longitudinal view, right patella with fracture. Left patella normal.
LEG-FOOT
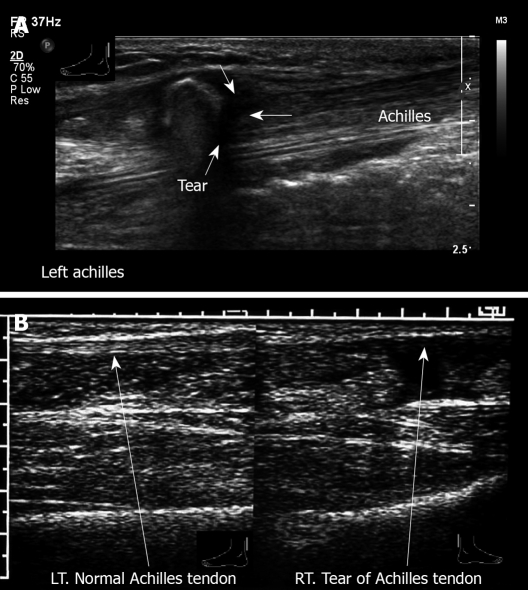
Ultrasound can provide a dynamic assessment of muscle tear, or of an intermittent muscle hernia or tendon subluxation. As with other soft tissue lesions, ultrasonography is useful for the evaluation of underlying pathologies in patients presenting with achillodynia and ankle pain. The Achilles tendon is the tendon most commonly evaluated in the leg and may be associated with a wide range of pathologies, including tendonosis, tears, calcification, and inflammations (Figure 26)[45,46]. Haglund deformity may be related to Achilles tendon pathology. The dynamic nature of the ultrasound examination enables tendon movement and visualization from the origin to the insertion of a tendon, as is needed in the evaluation of the Achilles tendon. Diseases of the Achilles tendon include a broad spectrum of pathologies ranging from paratendonitis to complete tendon ruptures. Tendonitis appears as fusiform swelling with hypoechogenicity and, tears and gaps can be measured. Ultrasound examination can detect shrapnel lesions, and contribute to the planning of surgical correction of ruptures in the Achilles tendon[47].
Figure 26.
Ultrasound examination of achilles tendon. A: Longitudinal view, left ankle posterior aspect. Complete tear of Achilles tendon with retraction. A 54-year old man felt a sudden sharp pain in the left Achilles tendon while running. Physical examination revealed absence of plantar flexion and a positive Thompson test; B: Longitudinal view. Right: tear of Achilles tendon. Left: Normal Achilles tendon.
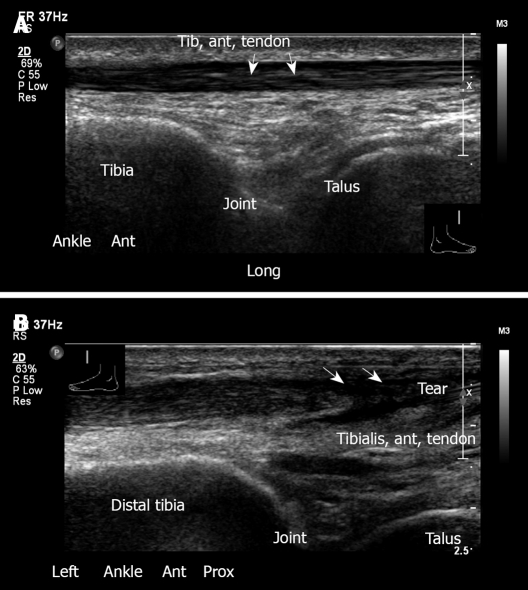
Ultrasound is also useful for diagnosing such pathologies of the ankle as tendon and ligament ruptures, and inflammation of the tendon sheath (Figure 27)[48-51]. Ankle sprain can demonstrate partial or complete tears. The most common torn ankle ligament is the anterior talofibular. Ligaments may appear hypoechoic with fluid, or discontinuous. Similarly, ultrasound allows the appearance of the calcaneo fibular and deltoid ligaments to be seen.
Figure 27.
Ultrasound examination of tibialis anterior tendon. A: Anterior longitudinal view, ankle. Tibiotalar joint with normal appearance of tibialis anterior tendon; B: Left ankle, longitudinal view. Tear of tibialis anterior tendon. This 68-year old male suffered from pain in the anterior aspect of the left ankle after much walking. No trauma had occurred.
The sonographic appearance of rough fragmentation with saw-teeth appearance is a specific sign which has demonstrated effectiveness in the evaluation of Sever’s disease[52].
Sonography can be effective in evaluating cases of tibial stress fractures[53]. Routine ultrasound examination includes the anterior tibial, posterior tibial, peroneal and Achilles tendon and the tibiotalar joint is evaluated for effusion or loose bodies.
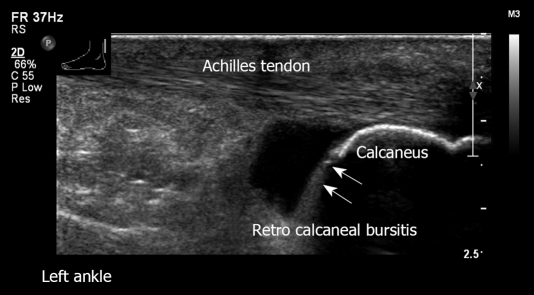
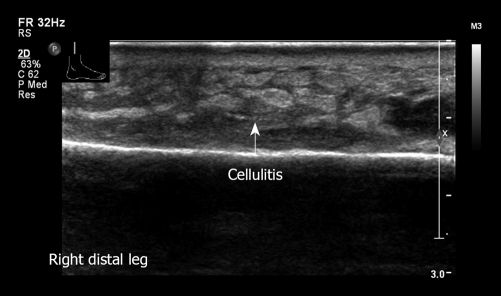
Tendinitis is visualized in ultrasound as hypoechogenicity of the tendon with increased interfibrillar distance. Retro-calcaneal bursitis and cellulitis can be seen (Figures 28 and 29). Partial tears indicate intrasubstance defects extending toward one surface of the tendon. Tendon discontinuity may indicate the proximal and distal stumps of the tendon. Insertion tendinopathy is seen as a hypoechoic enlargement of the tendon with fluid in the area inserted in the bone. Ultrasound is helpful in evaluating any syndesmosis, as is needed in post traumatic anterior ankle pain and in detecting foreign bodies in the ankle (Figure 30).
Figure 28.
Left ankle retro-calcaneal bursitis. Longitudinal view. Normal Achilles tendon. Note the large amount of fluid in the retro-calcaneal bursa.
Figure 29.
Longitudinal view, distal right leg. Swelling of soft tissue with fluid. Note increased echogenicity and thickening of the subcutaneous fat in the inflamed region.
Figure 30.
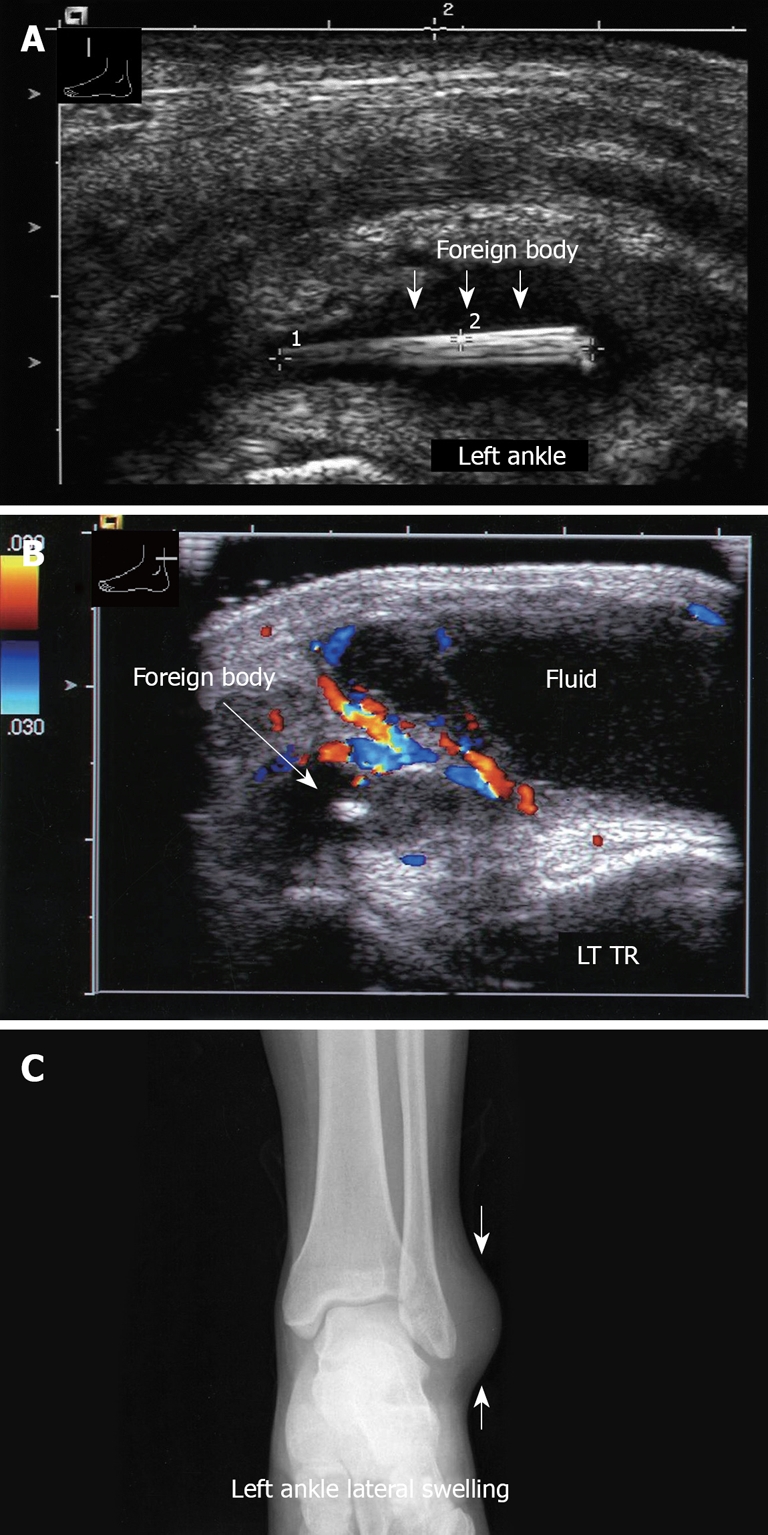
Ultrasound examination of left ankle. A: Longitudinal sonogram, left ankle, demonstrates a wooden foreign body; B: Transverse view, left ankle. Note the hypervascularity in the inflamed area; C: Corresponding X-ray of left ankle. Note the swelling on the lateral aspect. No foreign body is visible.
Ultrasound is useful in the assessment of foot lesions such as plantar fasciitis, plantar fascial tears, fibromatosis, morton neuroma, Jones fractures, and fractures of sesamoids and the 5th metatarsal bone[54].
HIP PATHOLOGY IN CHILDREN
Only rarely can a small effusion of the hip joint be detected by clinical examination. Thus, ultrasound, with its effectiveness in detecting effusion and synovitis, is generally used in the early assessment of hip pathology[55]. Detection of an effusion allows direct aspiration to decrease the pressure and to evaluate the fluid for possible septic arthritis[56]. Prompt aspiration in suspected cases of septic arthritis obviates the need for lengthy workups, and guides further treatment[57]. Further, ultrasound can be used to visualize fragmentation of the femoral head in “Perthes disease”[58], and to detect a slipped capital femoral epiphysis[59].
DEVELOPMENTAL DYSPLASIA OF THE HIP (DDH)
Clinical assessment of the newborn hip is routinely performed in the first days of life. Static and dynamic scanning by ultrasound enhances the rate of early detection of hip abnormalities[60]. Ultrasound follow-up is part of the routine management of hip dysplasia.
BONE AND MUSCLES PATHOLOGY
Assessment of the echogenic surface of bone and the acoustic shadow behind it can reveal abnormalities. Although sonography is not generally the examination of choice for the diagnosis of bone pathology, it should not be ignored, since significant pathologies, including fractures, bone erosions and lytic lesions, are occasionally detected.
Ultrasound can be used to detect subperiosteal collections of fluid in early osteomyelitis, as well as fractures[61], osteophyte, and bone tumors with bone damage. It provides excellent anatomical detail of the cortical surface of superficial bone. In cases of exostosis, it may be used to measure the thickness of the cartilage cap. The use of ultrasound for the diagnosis of fractures is gaining more and more interest. When ultrasound evaluation is targeted and combined with an orthopedic examination of the pathological area, precise demonstration of cortical disruption, soft tissue damage, and hematoma are possible. Knowledge of bone anatomy is essential for complete ultrasound evaluation of the musculoskeletal system.
Muscle pathologies such as rupture, calcification, myositis ossificans, hemorrhage can be also assessed by ultrasound.
MUSCULOSKELETAL ULTRASOUND IN RHEUMATOLOGY
During recent years, musculoskeletal ultrasound has become recognized as an effective imaging technique for the diagnosis and follow-up of patients with rheumatic diseases[62-67]. While most commonly used in the assessment of soft tissue disease or detection of fluid collection, ultrasound can also be used to visualize other structures, such as cartilage and bone surfaces[62,68,69].
CONCLUSION
Ultrasound is an invaluable diagnostic technique in orthopedic practice. Technological developments in resolution quality have increased the diagnostic possibilities while improvements in picture quality have increased clinical applications.
Muscoskeletal sonography is safer and more informative than X-rays for evaluating soft tissues pathology. Compared with MRI, it is accessible to all patients, without contraindications, and provides real time dynamic assessment.
Musculoskeletal ultrasonography is indicated for evaluation of soft tissue damage, particularly in sports injuries. The most practical uses are the evaluation of tendon structures, dynamic examination in motion, and the assessment of articular structures and diseases. Bursal disease with synovitis can be easily detected. Ultrasound should be performed when investigating rotator cuff tears, inflammation, calcific tendinitis and impingement syndrome, frozen shoulder, tennis or golfer elbow, biceps muscle, and distal biceps tendon insertion. Other indications include carpal tunnel syndrome, cysts of the wrists, pathology of tendon of the hands, retained foreign bodies, joint effusion, diseases of the knee, meniscal cysts, Baker cyst, ligament and osteoarthritis changes, Osgood Schlatter, and patella bipartite. In the ankle, ultrasound can detect tibio talar effusion, pathology of tibialis anterior, posterior, peroneal tendons, Achilles tendon, plantar fasciitis, and Morton neuroma.
Musculoskeletal sonography should be performed by an experienced operator with extensive knowledge of anatomy. Investment in training is justified in light of the contribution of this technology to diagnostic and therapeutic orthopedics and its accessibility to patients due to safety, non- ionizing radiation, low operating costs, lack of contraindications, and availability in locations distant from medical centers.
Acknowledgments
I would like to particularly thank Professor Avraham Ganel, Head of Pediatric Orthopedics, Sheba Medical Center, for his great help in guiding us in the writing of this review article. Also, a very special thank to Lydia Diamant, ultrasound technician, for her help and assistance in coordinating the ultrasound figures.
Footnotes
Peer reviewer: Michael T Hirschmann, MD, Department of Orthopaedic Surgery and Traumatology, Institution of Kantonsspital Bruderholz, Bruderholz, 4101, Switzerland
S- Editor Sun H L- Editor Hughes D E- Editor Lin YP
References
- 1.Jacobson JA. Musculoskeletal ultrasound and MRI: which do I choose? Semin Musculoskelet Radiol. 2005;9:135–149. doi: 10.1055/s-2005-872339. [DOI] [PubMed] [Google Scholar]
- 2.Nazarian LN. The top 10 reasons musculoskeletal sonography is an important complementary or alternative technique to MRI. AJR Am J Roentgenol. 2008;190:1621–1626. doi: 10.2214/AJR.07.3385. [DOI] [PubMed] [Google Scholar]
- 3.Khoury V, Cardinal E, Bureau NJ. Musculoskeletal sonography: a dynamic tool for usual and unusual disorders. AJR Am J Roentgenol. 2007;188:W63–W73. doi: 10.2214/AJR.06.0579. [DOI] [PubMed] [Google Scholar]
- 4.Garcia T, Hornof WJ, Insana MF. On the ultrasonic properties of tendon. Ultrasound Med Biol. 2003;29:1787–1797. doi: 10.1016/s0301-5629(03)01069-x. [DOI] [PubMed] [Google Scholar]
- 5.Blankstein A, Heyman Z, Salai M, Yitzchak Y, Chechick A. [Ultrasound in evaluation of soft tissue lesions of the musculoskeletal system] Harefuah. 1997;133:212–215. [PubMed] [Google Scholar]
- 6.Dudkiewicz I, Ganel A, Blankstein A. Congenital muscular torticollis in infants: ultrasound-assisted diagnosis and evaluation. J Pediatr Orthop. 2005;25:812–814. doi: 10.1097/01.bpo.0000184648.81109.75. [DOI] [PubMed] [Google Scholar]
- 7.Blankstein A, Ganel A, Diamant L, Chechick A. Cervical rib--preliminary data on diagnosis by ultrasound. Ultraschall Med. 2008;29:286–288. doi: 10.1055/s-2006-926824. [DOI] [PubMed] [Google Scholar]
- 8.Blankstein A, Ganel A, Salai M, Cohen I, Heim M, Diamant L, Chechick A. Fracture of the clavicle in the newborn - Detection and follow-up by sonography. Akt Traumatol. 2001;31:27–29. [Google Scholar]
- 9.Blankstein A, Dudkiewicz I, Givon U, Ganel A. Ultrasonographic imaging of congenital pseudoarthrosis of the clavicle. Akt Traumatol. 2004;34:234–236. [Google Scholar]
- 10.Blankstein A, Heyman Z, Yitzchak Y. [Ultrasound examination of the shoulder] Harefuah. 1995;128:441–444. [PubMed] [Google Scholar]
- 11.van Holsbeeck MT, Kolowich PA, Eyler WR, Craig JG, Shirazi KK, Habra GK, Vanderschueren GM, Bouffard JA. US depiction of partial-thickness tear of the rotator cuff. Radiology. 1995;197:443–446. doi: 10.1148/radiology.197.2.7480690. [DOI] [PubMed] [Google Scholar]
- 12.Farin PU, Jaroma H. Acute traumatic tears of the rotator cuff: value of sonography. Radiology. 1995;197:269–273. doi: 10.1148/radiology.197.1.7568835. [DOI] [PubMed] [Google Scholar]
- 13.Teefey SA, Hasan SA, Middleton WD, Patel M, Wright RW, Yamaguchi K. Ultrasonography of the rotator cuff. A comparison of ultrasonographic and arthroscopic findings in one hundred consecutive cases. J Bone Joint Surg Am. 2000;82:498–504. [PubMed] [Google Scholar]
- 14.Kleinbaum Y, Heyman Z, Ganel A, Mirovski Y, Blankstein A. Detection of greater tuberosity fractures by sonography. J Musculoskeletal Res. 2004;8:102–105. [Google Scholar]
- 15.Blankstein A, Mirovski Y, Givon U, Chechick A, Adunsky A, Ganel A. Ultrasonographic diagnosis in the evaluation of shoulder pain. J Musculoskeletal Res. 2004;8:195–200. [Google Scholar]
- 16.Middleton WD, Teefey SA, Yamaguchi K. Sonography of the Shoulder. Semin Musculoskelet Radiol. 1998;2:211–222. doi: 10.1055/s-2008-1080103. [DOI] [PubMed] [Google Scholar]
- 17.Blankstein A, Ganel A, Givon U, Dudkiewicz I, Perry M, Diamant L, Chechik A. Ultrasonography as a diagnostic modality in acromioclavicular joint pathologies. Isr Med Assoc J. 2005;7:28–30. [PubMed] [Google Scholar]
- 18.Blankstein A, Nerubay J, Lin E, Keren G, Friedman B, Horoszowski H. Septic arthritis of the sternoclavicular joint. Orthop Rev. 1986;15:440–442. [PubMed] [Google Scholar]
- 19.Blankstein A, Amsallem JL, Rubinstein E, Horoszowski H, Farin I. Septic arthritis of the acromioclavicular joint. Arch Orthop Trauma Surg. 1985;103:417–418. doi: 10.1007/BF00435451. [DOI] [PubMed] [Google Scholar]
- 20.Dudkiewicz I, Blankstein A. Ultrasonography: A highly efficient modalilty for diagnosis of Hill-Sachs lesions. Akt Traumatol. 2006;36:29–31. [Google Scholar]
- 21.Blankstein A, Ganel A, Dudkiewicz I, Givon U, Mirovski Y, Adunsky A. Ultrasonographic imaging in hemiplegic shoulders of stroke patients. Akt Traumatol. 2004;34:132–135. [Google Scholar]
- 22.Boehm TD, Kirschner S, Mueller T, Sauer U, Gohlke FE. Dynamic ultrasonography of rotator cuff muscles. J Clin Ultrasound. 2005;33:207–213. doi: 10.1002/jcu.20124. [DOI] [PubMed] [Google Scholar]
- 23.Drakeford MK, Quinn MJ, Simpson SL, Pettine KA. A comparative study of ultrasonography and arthrography in evaluation of the rotator cuff. Clin Orthop Relat Res. 1990:118–122. [PubMed] [Google Scholar]
- 24.van Holsbeeck MT. Sonography of the elbow, wrist and hand. In: van Holsbeeck MT, Introcaso JH, eds , editors. Musculoskeletal Ultrasound. St Louis: Mosby; 2001. pp. 517–571. [Google Scholar]
- 25.Martinoli C, Bianchi S, Giovagnorio F, Pugliese F. Ultrasound of the elbow. Skeletal Radiol. 2001;30:605–614. doi: 10.1007/s002560100410. [DOI] [PubMed] [Google Scholar]
- 26.Levin D, Nazarian LN, Miller TT, O'Kane PL, Feld RI, Parker L, McShane JM. Lateral epicondylitis of the elbow: US findings. Radiology. 2005;237:230–234. doi: 10.1148/radiol.2371040784. [DOI] [PubMed] [Google Scholar]
- 27.Blankstein A, Ganel A, Givon U, Mirovski Y, Chechick A. Ultrasonographic findings in patients with olecranon bursitis. Ultraschall Med. 2006;27:568–571. doi: 10.1055/s-2006-926569. [DOI] [PubMed] [Google Scholar]
- 28.Blankstein A, Chechick A, Adunski A, Givon U, Mirovski Y, Ganel A. Characteristics of soft tissue mass in the hand by ultrasonographic examination. J Musculoskeletal Res. 2005;9:45–51. [Google Scholar]
- 29.Cardinal E, Buckwalter KA, Braunstein EM, Mih AD. Occult dorsal carpal ganglion: comparison of US and MR imaging. Radiology. 1994;193:259–262. doi: 10.1148/radiology.193.1.8090903. [DOI] [PubMed] [Google Scholar]
- 30.Dias JJ, Dhukaram V, Kumar P. The natural history of untreated dorsal wrist ganglia and patient reported outcome 6 years after intervention. J Hand Surg Eur Vol. 2007;32:502–508. doi: 10.1016/J.JHSE.2007.05.007. [DOI] [PubMed] [Google Scholar]
- 31.Blankstein A, Cohen I, Heiman Z, Salai M, Diamant L, Heim M, Chechick A. Ultrasonography as a diagnostic modality and therapeutic adjuvant in the management of soft tissue foreign bodies in the lower extremities. Isr Med Assoc J. 2001;3:411–413. [PubMed] [Google Scholar]
- 32.Blankstein A, Cohen I, Heiman Z, Salai M, Heim M, Chechick A. Localization, detection and guided removal of soft tissue in the hands using sonography. Arch Orthop Trauma Surg. 2000;120:514–517. doi: 10.1007/s004020000173. [DOI] [PubMed] [Google Scholar]
- 33.Cohen E, Blankstein A, Rosenstock M, Atar D. Greenstick fractures of distal radius followed-up by ultrasound - A prospective study. Akt Traumatol. 2000;30:227–229. [Google Scholar]
- 34.Kleinbaum Y, Heyman Z, Ganel A, Blankstein A. Sonographic imaging of mallet finger. Ultraschall Med. 2005;26:223–226. doi: 10.1055/s-2005-858165. [DOI] [PubMed] [Google Scholar]
- 35.Friedman L, Finlay K, Popovich T, Chhem RK. Sonographic findings in patients with anterior knee pain. J Clin Ultrasound. 2003;31:85–97. doi: 10.1002/jcu.10140. [DOI] [PubMed] [Google Scholar]
- 36.Dudkiewicz I, Blankstein A. Ultrasonography: A highly efficient modalilty for anterior knee pain diagnosis. Akt Traumatol. 2006;36:180–182. [Google Scholar]
- 37.Blankstein A, Ganel A, Mirovsky Y, Chechick A, Dudkiewicz I. Early diagnosis of generalized knee pain and osteoarthritis by ultrasound. Akt Traumatol. 2006;36:175–179. [Google Scholar]
- 38.Azzoni R, Cabitza P. Is there a role for sonography in the diagnosis of tears of the knee menisci? J Clin Ultrasound. 2002;30:472–476. doi: 10.1002/jcu.10106. [DOI] [PubMed] [Google Scholar]
- 39.Blankstein A, Cohen I, Heim M, Diamant L, Salai M, Chechick A, Ganel A. Ultrasonography as a diagnostic modality in Osgood-Schlatter disease. A clinical study and review of the literature. Arch Orthop Trauma Surg. 2001;121:536–539. doi: 10.1007/s004020100285. [DOI] [PubMed] [Google Scholar]
- 40.Blankstein A, Cohen I, Salai M, Diamant L, Chechick A, Ganel A. Ultrasonography: an imaging modality enabling the diagnosis of bipartite patella. Knee Surg Sports Traumatol Arthrosc. 2001;9:221–224. doi: 10.1007/s001670100190. [DOI] [PubMed] [Google Scholar]
- 41.Kleinbaum Y, Blankstein A. Mild to moderate medial collateral ligament (MCL) injuries of the knee: sonographic findings and sonographic valgus stress test. J Musculoskeletal Res. 2008;11:9–14. [Google Scholar]
- 42.Ward EE, Jacobson JA, Fessell DP, Hayes CW, van Holsbeeck M. Sonographic detection of Baker's cysts: comparison with MR imaging. AJR Am J Roentgenol. 2001;176:373–380. doi: 10.2214/ajr.176.2.1760373. [DOI] [PubMed] [Google Scholar]
- 43.Bruck N, Sherr-Lurie N, Ganel A, Blankstein A. Tumours of the tibial tuberosity in children. Akt Traumatol. 2003;33:300–301. [Google Scholar]
- 44.Bianchi S, Zwass A, Abdelwahab IF, Banderali A. Diagnosis of tears of the quadriceps tendon of the knee: value of sonography. AJR Am J Roentgenol. 1994;162:1137–1140. doi: 10.2214/ajr.162.5.8165998. [DOI] [PubMed] [Google Scholar]
- 45.Blankstein A, Israeli A, Dudkiewicz I, Chechik A, Ganel A. Percutaneous Achilles tendon repair combined with real-time sonography. Isr Med Assoc J. 2007;9:83–85. [PubMed] [Google Scholar]
- 46.Blankstein A, Cohen I, Diamant L, Heim M, Dudkiewicz I, Israeli A, Ganel A, Chechick A. Achilles tendon pain and related pathologies: diagnosis by ultrasonography. Isr Med Assoc J. 2001;3:575–578. [PubMed] [Google Scholar]
- 47.Blansktein A, Heyman Z, Salai M, Yitzchak Y, Horoszowski H. Shrapnel lesion of the Achilles tendon: Diagnosis by ultrasonography. Eur J of Ultrasound. 1995;2:219–221. [Google Scholar]
- 48.Peetrons P, Creteur V, Bacq C. Sonography of ankle ligaments. J Clin Ultrasound. 2004;32:491–499. doi: 10.1002/jcu.20068. [DOI] [PubMed] [Google Scholar]
- 49.Bianchi S, Martinoli C, Gaignot C, De Gautard R, Meyer JM. Ultrasound of the ankle: anatomy of the tendons, bursae, and ligaments. Semin Musculoskelet Radiol. 2005;9:243–259. doi: 10.1055/s-2005-921943. [DOI] [PubMed] [Google Scholar]
- 50.Jacobson JA, Andresen R, Jaovisidha S, De Maeseneer M, Foldes K, Trudell DR, Resnick D. Detection of ankle effusions: comparison study in cadavers using radiography, sonography, and MR imaging. AJR Am J Roentgenol. 1998;170:1231–1238. doi: 10.2214/ajr.170.5.9574591. [DOI] [PubMed] [Google Scholar]
- 51.Khoury V, Guillin R, Dhanju J, Cardinal E. Ultrasound of ankle and foot: overuse and sports injuries. Semin Musculoskelet Radiol. 2007;11:149–161. doi: 10.1055/s-2007-1001880. [DOI] [PubMed] [Google Scholar]
- 52.Kleinbaum Y, Ganel A, Blankstein A. Ultrasonography as a diagnostic modality in Sever’s disease (calcaneal apophysitis) Akt Traumatol. 2006;36:294–297. [Google Scholar]
- 53.Farkash U, Naftal J, Deranze E, Blankstein A. Ultrasonography as a diagnostic modality of tibial stress fractures. J Musculoskelet Res. 2008;11:55–61. [Google Scholar]
- 54.Dudkiewicz I, Singh D, Blankstein A. Missed diagnosis fracture of the proximal fifth metatarsus – The role of ultrasound. Foot and Ankle Surg. 2005;11:161–166. [Google Scholar]
- 55.Novick GS. Sonography in pediatric hip disorders. Radiol Clin North Am. 1988;26:29–53. [PubMed] [Google Scholar]
- 56.Givon U, Liberman B, Schindler A, Blankstein A, Ganel A. Treatment of septic arthritis of the hip joint by repeated ultrasound-guided aspirations. J Pediatr Orthop. 2004;24:266–270. doi: 10.1097/00004694-200405000-00006. [DOI] [PubMed] [Google Scholar]
- 57.Bickerstaff DR, Neal LM, Booth AJ, Brennan PO, Bell MJ. Ultrasound examination of the irritable hip. J Bone Joint Surg Br. 1990;72:549–553. doi: 10.1302/0301-620X.72B4.2199451. [DOI] [PubMed] [Google Scholar]
- 58.Terjesen T. Ultrasonography in the primary evaluation of patients with Perthes disease. J Pediatr Orthop. 1993;13:437–443. doi: 10.1097/01241398-199307000-00004. [DOI] [PubMed] [Google Scholar]
- 59.Terjesen T. Ultrasonography for diagnosis of slipped capital femoral epiphysis. Comparison with radiography in 9 cases. Acta Orthop Scand. 1992;63:653–657. doi: 10.1080/17453679209169729. [DOI] [PubMed] [Google Scholar]
- 60.Rosendahl K, Markestad T, Lie RT, Sudmann E, Geitung JT. Cost-effectiveness of alternative screening strategies for developmental dysplasia of the hip. Arch Pediatr Adolesc Med. 1995;149:643–648. [PubMed] [Google Scholar]
- 61.Tomer K, Kleinbaum Y, Heyman Z, Dudkiewicz I, Blankstein A. Ultrasound diagnosis of fractures in adults. Akt Traumatol. 2006;36:171–174. [Google Scholar]
- 62.Backhaus M, Burmester GR, Gerber T, Grassi W, Machold KP, Swen WA, Wakefield RJ, Manger B. Guidelines for musculoskeletal ultrasound in rheumatology. Ann Rheum Dis. 2001;60:641–649. doi: 10.1136/ard.60.7.641. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Gibbon WW, Wakefield RJ. Ultrasound in inflammatory disease. Radiol Clin North Am. 1999;37:633–651. doi: 10.1016/s0033-8389(05)70120-2. [DOI] [PubMed] [Google Scholar]
- 64.Grassi W, Cervini C. Ultrasonography in rheumatology: an evolving technique. Ann Rheum Dis. 1998;57:268–271. doi: 10.1136/ard.57.5.268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Wakefield RJ, Gibbon WW, Emery P. The current status of ultrasonography in rheumatology. Rheumatology (Oxford) 1999;38:195–198. doi: 10.1093/rheumatology/38.3.195. [DOI] [PubMed] [Google Scholar]
- 66.Manger B, Kalden JR. Joint and connective tissue ultrasonography--a rheumatologic bedside procedure? A German experience. Arthritis Rheum. 1995;38:736–742. doi: 10.1002/art.1780380603. [DOI] [PubMed] [Google Scholar]
- 67.Manger B, Backhaus M. [Ultrasound diagnosis of rheumatic/inflammatory joint diseases] Z Arztl Fortbild Qualitatssich. 1997;91:341–345. [PubMed] [Google Scholar]
- 68.Grassi W, Tittarelli E, Pirani O, Avaltroni D, Cervini C. Ultrasound examination of metacarpophalangeal joints in rheumatoid arthritis. Scand J Rheumatol. 1993;22:243–247. doi: 10.3109/03009749309095131. [DOI] [PubMed] [Google Scholar]
- 69.Grassi W, Lamanna G, Farina A, Cervini C. Sonographic imaging of normal and osteoarthritic cartilage. Semin Arthritis Rheum. 1999;28:398–403. doi: 10.1016/s0049-0172(99)80005-5. [DOI] [PubMed] [Google Scholar]