Abstract
The anterior cruciate ligament (ACL) is an important structure in maintaining the normal biomechanics of the knee and is the most commonly injured knee ligament. However, the oblique course of the ACL within the intercondylar fossa limits the visualization and assessment of the pathology of the ligament. This pictorial essay provides a comprehensive and illustrative review of the anatomy and biomechanics as well as updated information on different modalities of radiological investigation of ACL, particularly magnetic resonance imaging.
Keywords: Magnetic resonance, Knee, Anterior cruciate ligament, Tear
ANATOMY
The anterior cruciate ligament (ACL) runs in an oblique course from the tibia to the lateral femoral condyle. It is an intra-articular extrasynovial ligament composed of fibres running from the anterior intercondylar region of the proximal tibia to the medial aspect of the lateral femoral condyle within the intercondylar groove. The fibres of the ACL are arranged into two bundles known as the anteromedial and posterolateral bundle according to their tibial insertion[1]. The anteromedial bundle inserts at a more medial and superior aspect of the lateral femoral condyle while the posterolateral bundle inserts at a more lateral and distal aspect of the lateral femoral condyle. Occasionally there is an additional intermediate bundle in between these two bundles[2,3]. The whole ACL measures approximately 38 mm in length and 11 mm in width[4]. The anteromedial bundle is 36.9 ± 2.9 mm in length, while the posterolateral bundle is 20.5 ± 2.5 mm in length. Both bundles are similar in size, with an average width of 5.0 ± 0.7 mm and 5.3 ± 0.7 mm in the mid-substance[5].
INJURY MECHANISMS
The ACL resists anterior tibial translation during extension and provides rotational stability[6-8]. The anteromedial bundle is taut when the knee is flexed and the posterolateral bundle is taut when the knee is extended[3]. The anteromedial bundle is longest in flexion and may be the primary component that resists anterior displacement of the tibia in flexion. The posterolateral bundle seems primarily to resist anterior tibial translation in extension and also contributes to rotatory stability of the knee joint[8] being employed in the “screw home” phenomenon i.e. during terminal extension of the knee, the tibia externally rotates relative to the femur serving to “lock” the knee in extension. The anteromedial and posterolateral bundles stabilize the knee joint in response to anterior tibial loads and combined rotatory loads in a synergistic way[9].
ACL tears may be partial or complete. Partial tears can range from a minor tear involving just a few fibres to a high grade near-complete tear involving almost all of the ACL fibres. A partial tear can involve both or only a single bundle to varying degree. Sometimes plastic deformity of the ACL without fibre discontinuity can occur causing ACL insufficiency[10].
The mechanism of the ACL injury includes internal rotation of the tibia relative to the femur. This commonly occurs during falls while skiing, as well as in contact sports such as football. With valgus stress, the medial femorotibial joint compartment is distracted producing medial collateral injury and medial meniscal injury (O’Donoghue’s triad). Another mechanism of ACL injury is hyperextension such as occurs during jumping or high kick maneuvers and will lead to contra-coup bone contusion on the anterior tibia and femoral condyle. ACL tears resulting from hyperextension frequently occur without concomitant collateral ligament or meniscal injury[11]. The third mechanism is external rotation of the tibia relative to the femur with varus stress leading to impaction and bone oedema medially and distraction laterally resulting in avulsion of the lateral tibial rim (Segond fracture) and tear of the lateral collateral ligament.
The majority of the ACL injuries can be diagnosed by history and clinical examination. The anterior drawer test, Lachman test and pivot shift test are the most commonly applied clinical tests to diagnose ACL tear though they do rely both on the experience of the clinician and the degree of patient cooperation. In chronic ACL insufficiency, the pivot shift test has reported high sensitivities for detecting the ACL injury ranging from 84% to 98.4%. The test’s specificity has been shown to vary more widely, with reported values from as low as 35% in the alert patient to as high as 98.4% in the anesthetized patient[12]. Anterior drawer and Lachman tests have similar sensitivity but lower specificity. However, in acute injury, if the patient is in pain or swelling, the examination may be limited and the sensitivity and specificity of the clinical tests are limited[12]. Association injury such as meniscal tear or chondral injury may also limit a full clinical examination. As a result, magnetic resonance imaging (MRI) is helpful in the assessment of suspected ACL injury.
Most ACL tears (approximately 80%) are complete, occurring around the middle one-third of the ACL (90%) or less frequently close to the femoral (7%) or tibial (3%) attachments. Less frequently (approximately 20%), ACL tears are incomplete with partial disruption of the ACL fibres[13]. Partial tears may involve only one or both bundles to a varying degree though the anteromedial band does tend to be the more commonly affected. Imaging, and in particular MRI, is very helpful in the assessment of suspected ACL injury.
Radiography
Radiographs have limited value in the diagnosis of acute ACL injury. Findings are indirect and limited to bone abnormalities. On radiography, there are several indirect signs that could raise suspicion of underlying ACL injury. Avulsion fracture of ACL at the tibial insertion or femoral origin can be found on radiographs but is better defined by computed tomography (CT)[14,15] (Figure 1A and B). Avulsion fracture of lateral tibial rim (Segond fracture) (Figure 2) is commonly associated with an ACL tear[16-18] and is classically due to avulsion fracture of the iliotibial band though the term has also been applied when there is avulsion of the fibular collateral ligament or biceps femoris tendon[15,17-19].
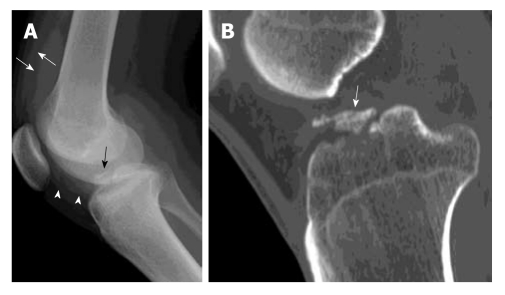
Figure 1.
Avulsion fracture of tibial spine. A 20-year-old man suffered knee injury during a football match. A: Lateral radiograph of the knee shows a displaced avulsion fracture of the anterior cruciate ligament (black arrow) at the anterior intercondylar eminence of tibia. The fracture fragment is completely elevated from the native bone. Increased soft tissue opacity in the suprapatellar pouch (white arrows) and infrapatellar pouch (white arrowheads) is in keeping with haemarthrosis; B: Reformatted sagittal computed tomography image of the same patient through the mid tibial plateau shows a displaced avulsion fracture of the tibial intercondylar eminence (white arrow).
Figure 2.
Segond fracture. A 30-year-old man suffered knee injury during a basketball match. A: Frontal radiograph of the right knee shows an avulsion fracture fragment at the lateral tibial rim (black arrow) compatible with Segond fracture. This fracture is frequently associated with a torn anterior cruciate ligament which also happened in this patient (not shown); B: A coronal T2-weighted fat suppression magnetic resonance image of the same patient. Corresponding site reveals a minimally displaced Segond fracture (white arrow) which may be easily missed in this patient with no significant bone bruise or oedema.
Osteochondral impaction fracture may very occasionally be seen in the condylopatellar sulcus of the lateral femoral condyle (lateral femoral notch sign) (Figure 3A). A sulcus deeper than 1.5 mm is a fairly specific though very insensitive indirect radiographic sign of a torn ACL[20] (Figure 3B). Haemarthrosis is very common in ACL tears and is seen as increased opacity in the suprapatellar pouch or even with fat fluid level (lipohemarthrosis) if associated with bone fracture (Figure 1A).
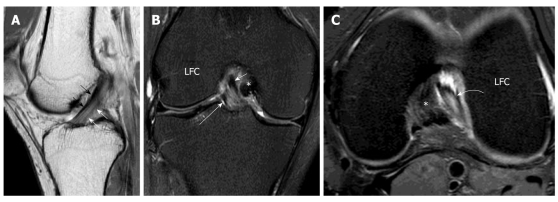
Figure 3.
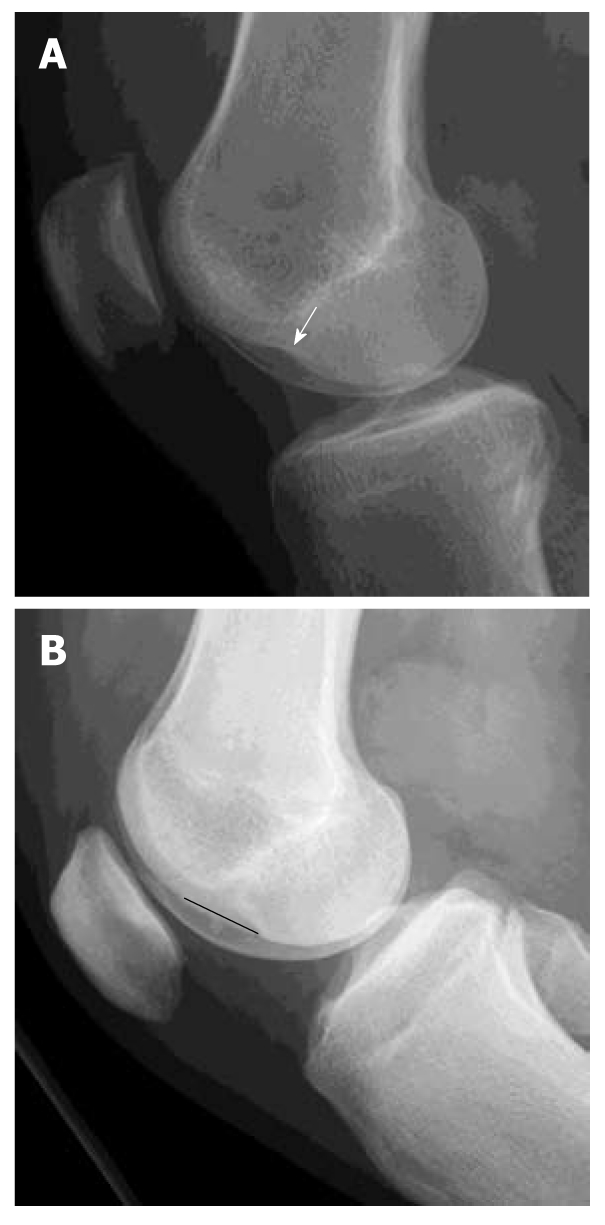
Osteochondral injury lateral femoral condyle. Lateral radiographs of two patients with complete anterior cruciate ligament (ACL) tear. A: Deep notch sign is abnormal deepening of the condylofemoral sulcus larger than 1.5 mm (white arrow); B: Long notch sign is abnormal lengthening of the condylofemoral sulcus (black straight line). These two signs are suggestive of osteochondral fracture of the lateral femoral condyle and highly associated with ACL tear though these are not very common findings.
Computed tomography
Although the ACL can be visualized on CT, its visibility is impaired in the presence of haemarthrosis and most patients with ACL injury are evaluated by MRI since this is also best for detecting concomitant menisceal, ligamentous or chondral injuries. If ACL avulsion injury is seen by radiography, CT is helpful in determining the size, and comminution of the avulsion bone fragment (Figure 1B) with three-dimensional CT allowing better fracture depiction. CT arthrography can be performed and has a comparable accuracy to MRI in the detection of both cruciate injury as well as menisceal injury[21].
Magnetic resonance imaging
MR sequences applied for optimal visualization of the ACL are 2D fast spin echo sequences either with or without fat suppression. Different planes are used for anatomical correlation. In most centres, the sequences used to visualize ACL include Turbo spin echo (TSE) sagittal intermediate weighted sequence either with fat suppression and non-fat suppression, TSE coronal T2 weighted fat suppression sequence and TSE axial intermediate weighted with fat-suppression sequence. In our centre, the standard knee protocol comprises the following three sequences (Figure 4A-C): (1) Coronal T2 weighted fat suppressed sequence; (2) TSE sagittal intermediate weighted sequence; and (3) TSE axial intermediate weighted with fat-suppression sequence.
Figure 4.
Normal anterior cruciate ligament. Volunteer, 24-year-old man with no history of injury and clinical instability. Sagittal intermediate-weighted magnetic resonance (MR) of the knee. A: Demonstrates a normal anterior cruciate ligament (ACL) which is characterized by a taut, continuous, low signal intensity fibres extending from the tibial plateau anteriorly to the medial aspect of the lateral femoral condyle. The more anterior portion of ACL is the anteromedial (AM) bundle (black arrows) while the more posterior portion is posterolateral (PL) bundle (white arrows). They cannot be well delineated from each other on this sagittal image. The PL bundle shows higher signal intensity than AM bundle. Coronal T2-weighted fat suppression MR knee image; B: The mid and distal ACL in the intercondylar fossa. The fibres are running superiorly and laterally within the intercondylar fossa from tibial attachment to the lateral femoral condyle (LFC). The more medial portion is the AM bundle (white short arrow) while the lateral portion is the PL bundle (white long arrow). Axial intermediate-weighted fat suppression MR image; C: Normal mid substance of ACL (curved white arrow). The ACL is elliptical in appearance because it is running obliquely to the scan plane. The two bundles cannot be differentiated from each other. *: Posterior cruciate ligament.
Additional sequences comprise oblique views, flexion views, T1-weighted sequences and small FOV or small coil images when necessary. T1-weighted sequences are useful for suspected fracture or characterizing loose bodies within the knee as any osseous fragments may contain a central marrow component. Small field of view sequences with the small coil placed directly over the area of interest are helpful at delineating peripheral pathology around the knee[22]. Oblique views are helpful in determining the presence, severity and location of ACL tears and will be discussed later.
MR images of the knees in flexion can provide more space around the ACL within the intercondylar area, helping to decrease volume-averaging artifact and thereby allowing better visualization of the femoral end of the ligament[23,24]. Recently 3D fast spin echo imaging with or without suppression has been shown to have the same diagnostic accuracy as 2D sequences. This can decrease volume averaging artifacts and shorten overall MR examination time[25].
The normal ACL should have a taut, low to intermediate signal intensity with continuous fibres in all planes and sequences. It courses parallel or steeper than the intercondylar line. The PL bundle usually has higher signal intensity than the AM bundle.
MRI is highly accurate at diagnosing ACL tears with accuracy, sensitivity and specificity of more than 90%[26-28].
Diagnosis of ACL tear on MR images is usually based on direct signs[26,28,29].
The primary sign of ACL tear is fibre discontinuity (Figure 5A). The oblique sagittal plane is the most helpful in diagnosis supported by coronal and axial imaging. The empty notch sign on coronal imaging is a frequent finding in complete ACL tear[30]. In acute or subacute injury, thickening and oedema of the ACL is found characterized by increased signal intensity on T2 or intermediate-weighted sequences (Figure 5B). In chronic case the fibres can be completely absorbed (Figure 5C) or the residual ACL stump can become adherent to the synovial envelope covering the posterior cruciate ligament[31]. As the orientation of the ACL makes visualization of the entire ACL in one plane difficult, some authors advocate use of oblique planes either parallel or perpendicular to the ACL to increase ligament and tear conspicuity. Oblique coronal and sagittal views parallel to the ACL have been advocated and found to be effective in improving visualization of the ACL[32-34] (Figure 6A and B). We have initiated oblique axial imaging of the ACL and found it to very useful in allowing much clearer delineation of the two ACL bundles, and determining the presence, the location of the normal individual bundle anatomy[34] and possibly individual bundle involvement of partial tears (Figure 7A and B). A clear potential benefit of imaging in an oblique axial plane is that it allows the ACL to be visualized on 11-15 contiguous images rather than on 2-3 contiguous images as with oblique sagittal or coronal imaging.
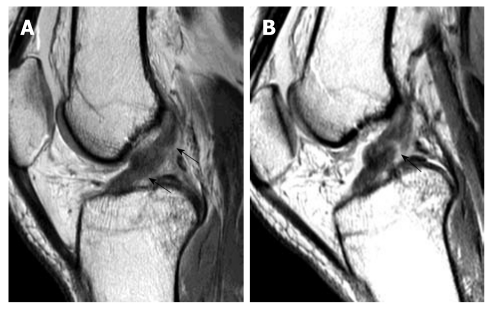
Figure 5.
Primary signs of anterior cruciate ligament tear. Sagittal intermediate-weighted images of three different patients showing different patterns of anterior cruciate ligament (ACL) tear. A: Typical appearance of ACL tear at the mid-substance with fibres discontinuity of ACL (arrowheads). Residual stumps on femoral (asterisk) and tibial sides (white arrow) are lax, thickened and increased in signal intensity; B: Chronic ACL tear with absence of normal ACL fibres compatible with complete resorption of fibres. PCL (Curved black arrow); C: Acute high grade intrasubstance tear as characterized by thickening and oedematous change of ACL fibres which show increased signal intensity (white arrows). The fibres are still in continuity suggestive of partial ACL tear.
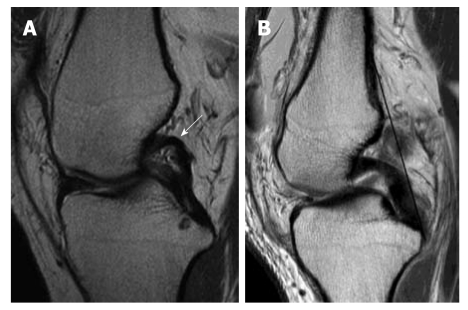
Figure 6.
High resolution imaging normal anterior cruciate ligament in oblique coronal and oblique sagittal planes. Volunteer of a 31-year-old man with no history of injury and clinical instability. Note that the AM bundle (white long arrow) and PL bundle (white short arrow) can be well depicted on the oblique coronal image at the tibial attachment but not at the femoral attachment and not by the oblique sagittal image.
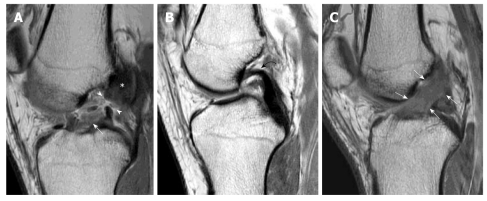
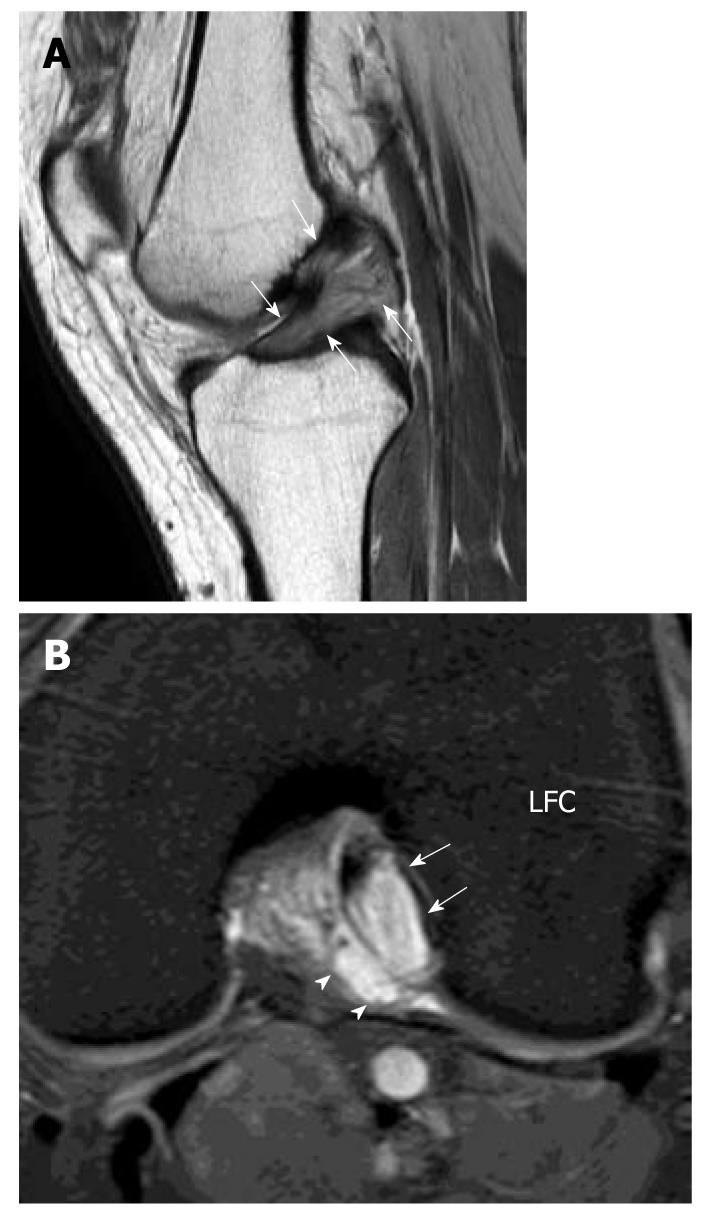
Figure 7.
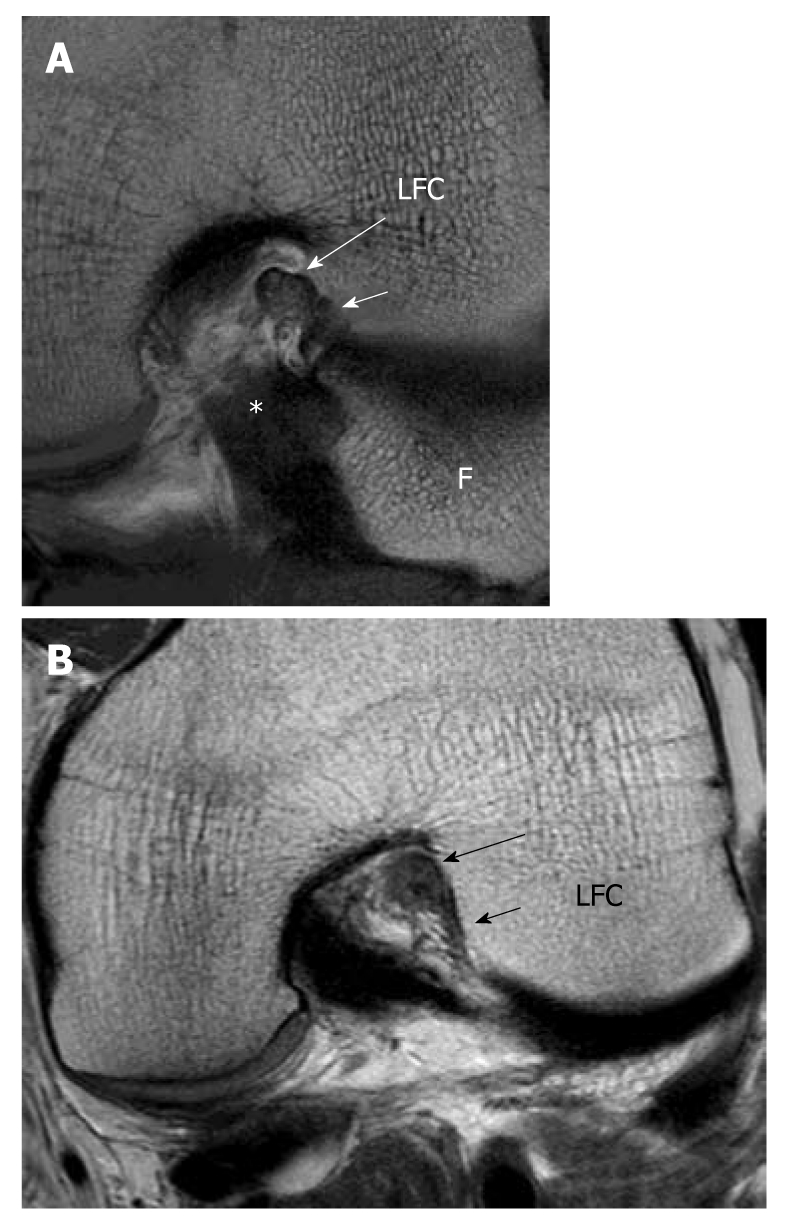
High resolution imaging anterior cruciate ligament in oblique axial plane. A: Oblique axial image can clearly delineate the two bundles and assess each bundle separately; AM bundle (long white arrow) PL bundle (short white arrow). B: Partial tear of the anterior cruciate ligament. Oblique axial image at the femoral side shows thickening and hyperintense signal intensity of the AM bundle (black long arrow) while fibres are absent in the region of the PL bundle (black short arrow). Features are compatible with high grade partial AM bundle tear and complete PL tear which were confirmed in arthroscopy. LFC: Lateral femoral condyle; *: Posterior cruciate ligament; F: Fibular head.
Partial tears of the ACL are more difficult to diagnose than complete ACL tears. Partial tears are characterized by increased signal intensity and fiber laxity with increased concavity (or bowing) of the ACL (Figure 8). Continuous fibres are evident which suggest the tear is not complete. The sensitivity (40% to 75%) and specificity (51% to 89%) of MRI in the diagnosis of partial tears is poor[35,36] though this poor performance may be improved by the higher resolution afforded by 3T imaging. A recent study employing 3T MRI reported a sensitivity of 77% and specificity of 97% in detecting partial tears of the ACL[37]. If more than 50% of the ACL fibres are torn this would be considered a high grade tear, a medium grade tear is 10%-50% of fibres torn, while a low grade tear is less than 10% of fibres torn. The Holy Grail, with respect to imaging of partial ACL tears, would be to have sufficient resolution to determine whether there was a low, medium or high grade tear in each particular ACL bundle.
Figure 8.

Partial tear of the anterior cruciate ligament. Sagittal intermediate-weighted image of partial anterior cruciate ligament (ACL) tear. The ACL appears lax, concave in appearance (white arrow) and increased in signal intensity. However, the fibres are still in continuity suggestive of partial ACL tear.
Potential pitfalls of MR in defining ACL tears are partial volume artifact and reparative fibrosis following an ACL injury bridging the residual ACL stump and adjacent structures, such as femoral notch, the posterior cruciate ligament (PCL) or the synovial envelope covering the PCL. This will help retain a near normal alignment of the ACL and may lead to an ACL appearing to be intact in the previous complete or partial tear. It is conceivable however that such a re-attached ACL may still remain functionally sound and this possibility should be consistently reported. Flexion imaging is particularly helpful in this situation as even 20 degrees of flexion helps change the orientation of central structures in the knee joint to such a degree that the ACL stump can be seen to be adherent to the PCL (Figure 9).
Figure 9.
Magnetic resonance knee in partial flexion. Volunteer, 31-year-old man with no history of injury and clinical instability. Sagittal intermediate-weighted magnetic resonance image in full extension. A: And 30 degree of knee flexion; B: Demonstrates the usefulness of knee flexion. When the knee is extended, sagittal image shows features suspicious of an anterior cruciate ligament (ACL) tear. When the knee is flexed, a gap (black arrow) is clearly present confirming the presence of an ACL tear.
Bone bruising is very common in ACL tears. McCauley et al[27] suggested that the presence of bone bruising in the posterior aspect of the tibial plateau and posterior displacement of the posterior horn of the lateral meniscus are highly specific for a torn ACL. However, some authors found that secondary signs such as bone bruising do not help significantly in the diagnosis of ACL tears[37-39].
A bone bruise is commonly caused by internal rotation in valgus stress injury, where there is impaction of the posterior aspect of the tibial plateau against the mid or anterior portion of the femoral condyle[40] (Figure 10). This abnormal medullary signal intensity is attributed to subcortical microfracture, oedema, or haemorrhage[28,40]. In the case of anteromedial mechanism of injury or direct compression injuries, the bone bruise pattern is different, such as kissing bone oedema lesions or involving the posteromedial tibial plateau.
Figure 10.

Bone bruises. A 26-year-old man suffered knee injury. Sagittal T2-weighted fat suppression magnetic resonance knee image shows that there are bone rises (asterisks) present in the mid-lateral femoral condyle and posterolateral tibial plateau which indicate that the mechanism of injury is internal rotation of the tibia in valgus stress injury. This pattern of bone bruise has a high association of anterior cruciate ligament complete tear which is present in this patient (not shown).
Bone bruising is a result of impaction at the time of injury. Particularly in young patients who most likely have more elasticity of their ACL fibres, it is distraction and impaction, particularly of the more central rather than posterior aspects of the condyles, that can occur even in the absence of an ACL tear. We would consider bone bruising to be a strong but not absolute indicator of ACL tear.
The deep lateral femoral notch sign, although uncommon, is quite specific for ACL tear and is due to impaction injury of the lateral femoral condyle onto the tibia[41] (Figure 11). A notch depth of over 2 mm is diagnostic of ACL tear. Segond fracture is due to avulsion fracture of the iliotibial band, fibular collateral ligament and biceps femoris tendon and can be seen on MRI examination (Figure 3B). Bosch-Bock bump relates to a bone excrescence located 2-5 mm below the lateral articular margin of the tibia. This bump indicates a chronic tear of the ACL.
Figure 11.
Patellar buckling sign and lateral femoral notch sign. A 37-year-old man who suffered knee injury. Osteochondral injury and patellar buckling sign. Sagittal intermediate-weighted magnetic resonance image demonstrates a deep depression of the middle portion of the lateral femoral condyle (curved white arrow). Normal condylopatellar sulcus should be smaller than 1.5 mm. Notch depth between 1 and 2 mm is suggestive and over 2 mm is diagnostic of anterior cruciate ligament tear. Buckling of proximal patellar tendon (white arrow) also indicates the underlying anterior cruciate ligament tear.
Since the function of the ACL is to prevent anterior tibial translation in extension, ACL tear should increase the degree of anterior tibial translation during knee extension giving rise to “anterior tibial translocation”[41-43] (Figure 12). It is usually apparent on sagittal MR images at the mid-lateral femoral condyle. If there is ≥ 5 mm anterior translocator of the tibia relative to the femur, this would be indicative of ACL tear (sensitivity 86%, specificity 99%)[44] while an anterior tibial translation > 7 mm is fully diagnostic of ACL tear.
Figure 12.

Uncovered posterior horn lateral meniscus and anterior tibial translation. A 32-year-old man who suffered knee injury. Sagittal intermediate-weighted magnetic resonance image of complete anterior cruciate ligament tear patient. The anterior displacement of the tibial translation is measured as the distance between two lines parallel to the picture frame (white lines). At the mid-sagittal plane of lateral femoral condyle, a line is drawn through the most posterior corner of the lateral tibial plateau, and the second line is tangent to the most posterior aspect of the lateral femoral condyle. Anterior tibial translation between 5 and 7 mm is suggestive and over 7 mm is diagnostic of anterior cruciate ligament tear. Note that the lateral meniscus also intersects the tangent to posterior margin of tibia and represents the uncovered posterior horn of lateral meniscus.
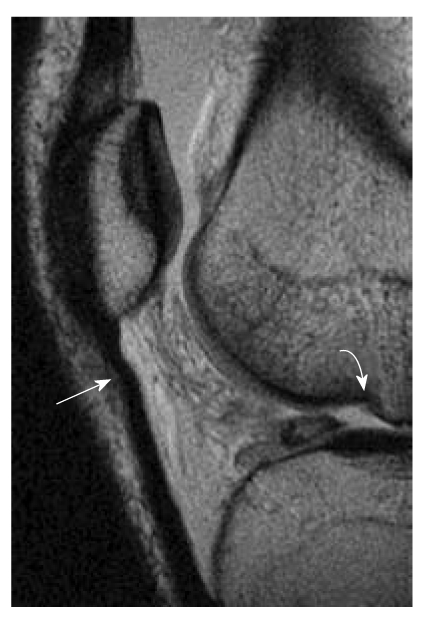
Femorotibial translation and rotation gives rise to a host of other signs which are all moderately suggestive of ACL injury such as buckling of the patellar tendon (Figure 11), buckling of the posterior cruciate ligament[45] (Figure 13), a posterior PCL line[41], uncovered posterior horn of the medial or lateral meniscus[30] (Figure 12) or visibility of the whole posterior cruciate ligament or lateral collateral ligament in one coronal image (Figure 14).
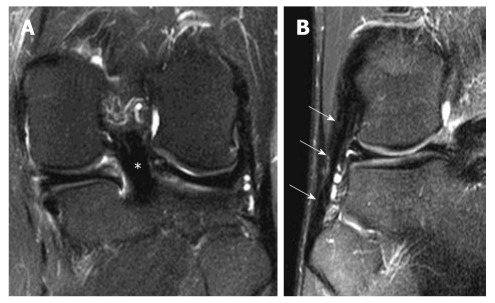
Figure 13.
Posterior cruciate ligament buckling and Posterior cruciate ligament line sign. Sagittal intermediate-weighted magnetic resonance knee image of a completely torn anterior cruciate ligament. A: Posterior cruciate ligament (PCL) buckling sign. The PCL is considered to be hyperbuckled if any portion of its posterosuperior border is concave (white arrow); B: The PCL line sign. A line tangential to the posterior margin of the PCL is drawn (black line) and if this tangent does not intersect the posterior cortex of the femur within 5cm of its distal end, the PCL line is considered to be positive.
Figure 14.
Coronal whole posterior cruciate ligament and lateral collateral ligament sign. Coronal T2-weighted fat suppression magnetic resonance knee images of two different patients with complete anterior cruciate ligament tear show that A: The entire posterior cruciate ligament (*); B: Entire lateral collateral ligament (white arrows) can be seen in a single coronal image.
Shearing fat pad injury is also associated with ACL tear[29] and results in fracture of the infrapatellar fat pad (Figure 15).
Figure 15.

Shearing of fat pad. Sagittal T2-weighted fat suppression magnetic resonance image shows a fracture of Hoffa’s fat pad that has isolated a segment of fat (white arrows).
ASSOCIATED INJURIES
Meniscal injury
Meniscal tear is commonly associated with ACL tear (65%-70%)[46]. Peripheral vertical tear in the posterior horn of lateral meniscus (“posterolateral corner tear”) is highly associated with acute ACL tear[47,48] and easily overlooked[49] (Figure 16). Chronic ACL insufficiency or tear increases the incidence of peripheral vertical tear at the posterior horn of medial meniscus most likely related to chronic femorotibial instability[50]. Peripheral posterior horn tears accounted for more than half of meniscal tears seen in patients with acute or chronic ACL injuries[51]. Together with medial collateral ligament tear and ACL tear, these form the classical O’Donoghue’s triad (Figure 17).
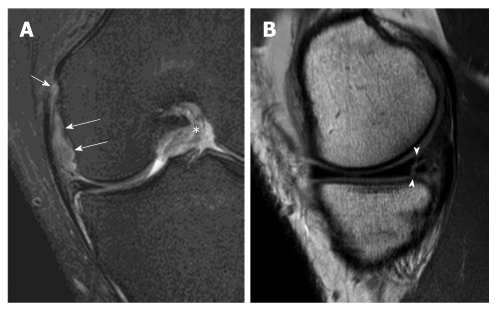
Figure 16.

Peripheral vertical tear in a patient with complete anterior cruciate ligament tear. Sagittal intermediate-weighted magnetic resonance image demonstrates a peripheral vertical tear (white arrows) extending of the posterior horn of lateral meniscus. This kind of peripheral vertical tear can be easily missed and is frequently associated with anterior cruciate ligament tear.
Figure 17.
O’ Donoghue’s triad. Magnetic resonance images of a patient with complete anterior cruciate ligament (ACL) tear showing O’ Donoghue’s triad. A: Coronal T2-weighted fat suppression magnetic resonance (MR) image demonstrates complete tear of the meniscofemoral ligament (white long arrows) and femoral attachment of the medial collateral ligament (white short arrow). Note that the ACL in the intercondylar fossa has a substantial tear (asterisk); B: Sagittal intermediate-weighted MR image shows an associated vertical and horizontal (complex) peripheral tear at the posterior horn of medial meniscus (arrowheads). These injuries constitute the classical “O Donoghue’s triad”.
Posterolateral corner injury
Posterolateral corner injury needs to be addressed because of its contribution to tridimensional instability of the knee (sagittal, frontal and rotational instability). Some of the studies suggest that ACL reconstruction without repair of the posterolateral corner injury increases the likelihood of instability and ACL re-tear[52]. Posterolateral corner injury includes the fibular collateral ligament, the popliteus muscle and tendon, the popliteofibular ligament, the lateral and posterolateral capsule and the biceps femoris tendon (Figure 18). The average length of fibular collateral ligament is 66 mm (59-74 mm) and the average thickness at the mid portion measures 3.4 mm (3-4 mm)[53]. The mean total length of the popliteus tendon was 42.0 mm[54]. The thickness of the popliteomeniscal ligament is variable. Peduto et al[55] found that in ten cadaveric knees, half of anteroinferior popliteomeniscal fascicle was ≥ 2 mm, the other half was smaller than 2 mm.
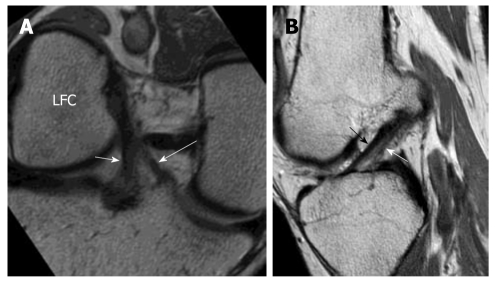
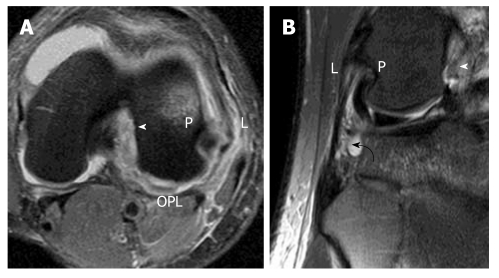
Figure 18.
Posterolateral corner injury. A 25-year-old man suffered knee injury during a football match. A: Axial intermediate-weighted; B: Coronal T2-weighted fat suppression images of a patient with acute complete anterior cruciate ligament tear (white arrowhead). Oedema with thickening of the lateral collateral ligament and partial disruption of the fibres are present at the femoral origin (L). The posterior capsule and the oblique popliteal ligament (OPL) also show thickening and oedematous change. There is mild sprain of the femoral insertion of the popliteus tendon (P). The popliteofibular ligament is severely swollen and oedematous suggestive of high grade partial tear (curved black arrow).
In general, these normally low-signal-intensity structures are defined as injured or sprained when there is thickening and intermediate signal intensity within the structure on fat-suppressed fast spin-echo T2-weighted images and as torn when the structure is discontinuous with a visible gap[52]. Some researchers support the use of a coronal oblique plane of imaging to improve visualization of some of the finer, obliquely oriented structures of the posterolateral corner, including the popliteofibular, arcuate, and fabellofibular ligaments[56], although this has not become routine.
Ganglion cyst and mucoid degeneration of the ACL
Cystic degeneration of the ACL has been has been attributed to mucinous degeneration of connective tissue[57,58] or considered as intrasubstance ACL tear. On MR imaging, cystic degeneration can manifest as well-defined ganglion cysts arising from the ACL which occur in about 1% of patients[59] (Figure 19) or increased signal intensity of the whole ACL, giving rise to an appearance similar to a stalk of celery[60] (Figure 20). This increase in signal intensity is due to deposition of amorphous mucoid matrix among the ACL fibres, Clinical symptoms include pain, swelling symptoms and mechanical locking. ACL ganglion cysts and mucoid degeneration identified on MRI are usually not discernible at arthroscopy[58]. Since the ACL is surrounded by a synovial envelope, masses can arise from this synovium similar to synovium elsewhere. These synovial masses include focal nodular synovitis, pigmented villonodular synovitis, or gouty tophi. Other much less common synovial type masses include synovial vascular malformations[61] and synovial chondromatosis[62].
Figure 19.
Celery stalk sign (mucoid degeneration). Sagittal intermediate-weighted magnetic resonance (MR) image. A: Enlargement of anterior cruciate ligament (ACL) (white arrows) with increased signal intensity compatible with mucoid degeneration. Low-signal-intensity fibres running parallel to the long axis of high signal ACL i.e. celery stalk sign; B: Axial intermediate-weighted fat suppression MR image shows cystic change within the ACL (white arrows) predominantly in the PL bundle. LFC: Lateral femoral condyle.
Figure 20.

Pericruciate ganglion cyst. Sagittal intermediate-weighted MR image shows a ganglion cyst (white arrows) arising from proximal posterior half of ligament.
CONCLUSION
The ACL ligament is a very important ligament structurally and because it is so frequently injured. Imaging, and in particular, MRI has allowed a much more accurate assessment of ACL injuries and other conditions affecting the ACL as well as associated injuries. However, work still needs to be done to improve the accuracy with which partial tears can be diagnosed and located.
Footnotes
Peer reviewers: Naiquan Nigel Zheng, Professor, Mechanical Engineering, University of North Carolina, 9201 University City Blvd, Charlotte, NC 28223, United States; John J Elias, PhD, Calhoun Research Laboratory, Akron General Medical Center, 400 Wabash Ave, Akron, OH 44307, United States; Eduardo Magalhães, PT, MD, Eduardo Magalhães Institute, Domingos de M oraes street, n° 2243, room 56, São Paulo 04035-000, Brazil
Supported by A grant from the Research Grants Council of the Hong Kong Special Administrative Region, China, Project No. SEG_CUHK02
S- Editor Lv S L- Editor Hughes D E- Editor Zheng XM
References
- 1.Yasuda K, van Eck CF, Hoshino Y, Fu FH, Tashman S. Anatomic single- and double-bundle anterior cruciate ligament reconstruction, part 1: basic science. Am J Sports Med. 2011;39:1789–1799. doi: 10.1177/0363546511402659. [DOI] [PubMed] [Google Scholar]
- 2.Norwood LA, Cross MJ. Anterior cruciate ligament: functional anatomy of its bundles in rotatory instabilities. Am J Sports Med. 1979;7:23–26. doi: 10.1177/036354657900700106. [DOI] [PubMed] [Google Scholar]
- 3.Amis AA, Dawkins GP. Functional anatomy of the anterior cruciate ligament. Fibre bundle actions related to ligament replacements and injuries. J Bone Joint Surg Br. 1991;73:260–267. doi: 10.1302/0301-620X.73B2.2005151. [DOI] [PubMed] [Google Scholar]
- 4.Girgis FG, Marshall JL, Monajem A. The cruciate ligaments of the knee joint. Anatomical, functional and experimental analysis. Clin Orthop Relat Res. 1975:216–231. doi: 10.1097/00003086-197501000-00033. [DOI] [PubMed] [Google Scholar]
- 5.Cohen SB, VanBeek C, Starman JS, Armfield D, Irrgang JJ, Fu FH. MRI measurement of the 2 bundles of the normal anterior cruciate ligament. Orthopedics. 2009;32:687. doi: 10.3928/01477447-20090728-35. [DOI] [PubMed] [Google Scholar]
- 6.Takai S, Woo SL, Livesay GA, Adams DJ, Fu FH. Determination of the in situ loads on the human anterior cruciate ligament. J Orthop Res. 1993;11:686–695. doi: 10.1002/jor.1100110511. [DOI] [PubMed] [Google Scholar]
- 7.Sakane M, Fox RJ, Woo SL, Livesay GA, Li G, Fu FH. In situ forces in the anterior cruciate ligament and its bundles in response to anterior tibial loads. J Orthop Res. 1997;15:285–293. doi: 10.1002/jor.1100150219. [DOI] [PubMed] [Google Scholar]
- 8.Gabriel MT, Wong EK, Woo SL, Yagi M, Debski RE. Distribution of in situ forces in the anterior cruciate ligament in response to rotatory loads. J Orthop Res. 2004;22:85–89. doi: 10.1016/S0736-0266(03)00133-5. [DOI] [PubMed] [Google Scholar]
- 9.Zantop T, Herbort M, Raschke MJ, Fu FH, Petersen W. The role of the anteromedial and posterolateral bundles of the anterior cruciate ligament in anterior tibial translation and internal rotation. Am J Sports Med. 2007;35:223–227. doi: 10.1177/0363546506294571. [DOI] [PubMed] [Google Scholar]
- 10.Larson RL. Prosthetic replacement of knee ligaments: Overview. In: Feagin JA, editor. The crucial ligaments: Diagnosis and treatment of ligamentous injuries about the knee. New York: Churchill Livingstone; 1988. pp. 495–501. [Google Scholar]
- 11.Weber WN, Neumann CH, Barakos JA, Petersen SA, Steinbach LS, Genant HK. Lateral tibial rim (Segond) fractures: MR imaging characteristics. Radiology. 1991;180:731–734. doi: 10.1148/radiology.180.3.1871286. [DOI] [PubMed] [Google Scholar]
- 12.Lubowitz JH, Bernardini BJ, Reid JB. Current concepts review: comprehensive physical examination for instability of the knee. Am J Sports Med. 2008;36:577–594. doi: 10.1177/0363546507312641. [DOI] [PubMed] [Google Scholar]
- 13.Vahey TN, Broome DR, Kayes KJ, Shelbourne KD. Acute and chronic tears of the anterior cruciate ligament: differential features at MR imaging. Radiology. 1991;181:251–253. doi: 10.1148/radiology.181.1.1887042. [DOI] [PubMed] [Google Scholar]
- 14.Griffith JF, Antonio GE, Tong CW, Ming CK. Cruciate ligament avulsion fractures. Arthroscopy. 2004;20:803–812. doi: 10.1016/j.arthro.2004.06.007. [DOI] [PubMed] [Google Scholar]
- 15.Bales CP, Guettler JH, Moorman CT. Anterior cruciate ligament injuries in children with open physes: evolving strategies of treatment. Am J Sports Med. 2004;32:1978–1985. doi: 10.1177/0363546504271209. [DOI] [PubMed] [Google Scholar]
- 16.Goldman AB, Pavlov H, Rubenstein D. The Segond fracture of the proximal tibia: a small avulsion that reflects major ligamentous damage. AJR Am J Roentgenol. 1988;151:1163–1167. doi: 10.2214/ajr.151.6.1163. [DOI] [PubMed] [Google Scholar]
- 17.Stallenberg B, Gevenois PA, Sintzoff SA, Matos C, Andrianne Y, Struyven J. Fracture of the posterior aspect of the lateral tibial plateau: radiographic sign of anterior cruciate ligament tear. Radiology. 1993;187:821–825. doi: 10.1148/radiology.187.3.8497638. [DOI] [PubMed] [Google Scholar]
- 18.Chan KK, Resnick D, Goodwin D, Seeger LL. Posteromedial tibial plateau injury including avulsion fracture of the semimembranous tendon insertion site: ancillary sign of anterior cruciate ligament tear at MR imaging. Radiology. 1999;211:754–758. doi: 10.1148/radiology.211.3.r99jn16754. [DOI] [PubMed] [Google Scholar]
- 19.Donald L, Resnick MD, Heung Sik Kang MD, Michael L. Knee. 2th ed. Philadelphia: Saunders; 2007. Internal Derangements of Joints. p. 1823. [Google Scholar]
- 20.Pao DG. The lateral femoral notch sign. Radiology. 2001;219:800–801. doi: 10.1148/radiology.219.3.r01jn12800. [DOI] [PubMed] [Google Scholar]
- 21.Vande Berg BC, Lecouvet FE, Poilvache P, Dubuc JE, Maldague B, Malghem J. Anterior cruciate ligament tears and associated meniscal lesions: assessment at dual-detector spiral CT arthrography. Radiology. 2002;223:403–409. doi: 10.1148/radiol.2232011024. [DOI] [PubMed] [Google Scholar]
- 22.Antonio GE, Griffith JF, Yeung DK. Small-field-of-view MRI of the knee and ankle. AJR Am J Roentgenol. 2004;183:24–28. doi: 10.2214/ajr.183.1.1830024. [DOI] [PubMed] [Google Scholar]
- 23.Pereira ER, Ryu KN, Ahn JM, Kayser F, Bielecki D, Resnick D. Evaluation of the anterior cruciate ligament of the knee: comparison between partial flexion true sagittal and extension sagittal oblique positions during MR imaging. Clin Radiol. 1998;53:574–578. doi: 10.1016/s0009-9260(98)80148-7. [DOI] [PubMed] [Google Scholar]
- 24.Niitsu M, Ikeda K, Fukubayashi T, Anno I, Itai Y. Knee extension and flexion: MR delineation of normal and torn anterior cruciate ligaments. J Comput Assist Tomogr. 1996;20:322–327. doi: 10.1097/00004728-199603000-00030. [DOI] [PubMed] [Google Scholar]
- 25.Gene Saragnese. 3D imaging of the knee takes a step forward. Field strength. 2010;42:16–19. [Google Scholar]
- 26.Lee JK, Yao L, Phelps CT, Wirth CR, Czajka J, Lozman J. Anterior cruciate ligament tears: MR imaging compared with arthroscopy and clinical tests. Radiology. 1988;166:861–864. doi: 10.1148/radiology.166.3.3340785. [DOI] [PubMed] [Google Scholar]
- 27.McCauley TR, Moses M, Kier R, Lynch JK, Barton JW, Jokl P. MR diagnosis of tears of anterior cruciate ligament of the knee: importance of ancillary findings. AJR Am J Roentgenol. 1994;162:115–119. doi: 10.2214/ajr.162.1.8273648. [DOI] [PubMed] [Google Scholar]
- 28.Mink JH, Levy T, Crues JV. Tears of the anterior cruciate ligament and menisci of the knee: MR imaging evaluation. Radiology. 1988;167:769–774. doi: 10.1148/radiology.167.3.3363138. [DOI] [PubMed] [Google Scholar]
- 29.Robertson PL, Schweitzer ME, Bartolozzi AR, Ugoni A. Anterior cruciate ligament tears: evaluation of multiple signs with MR imaging. Radiology. 1994;193:829–834. doi: 10.1148/radiology.193.3.7972833. [DOI] [PubMed] [Google Scholar]
- 30.Tung GA, Davis LM, Wiggins ME, Fadale PD. Tears of the anterior cruciate ligament: primary and secondary signs at MR imaging. Radiology. 1993;188:661–667. doi: 10.1148/radiology.188.3.8351329. [DOI] [PubMed] [Google Scholar]
- 31.Lo IK, de Maat GH, Valk JW, Frank CB. The gross morphology of torn human anterior cruciate ligaments in unstable knees. Arthroscopy. 1999;15:301–306. doi: 10.1016/s0749-8063(99)70039-3. [DOI] [PubMed] [Google Scholar]
- 32.Duc SR, Zanetti M, Kramer J, Käch KP, Zollikofer CL, Wentz KU. Magnetic resonance imaging of anterior cruciate ligament tears: evaluation of standard orthogonal and tailored paracoronal images. Acta Radiol. 2005;46:729–733. doi: 10.1080/02841850500215907. [DOI] [PubMed] [Google Scholar]
- 33.Hong SH, Choi JY, Lee GK, Choi JA, Chung HW, Kang HS. Grading of anterior cruciate ligament injury. Diagnostic efficacy of oblique coronal magnetic resonance imaging of the knee. J Comput Assist Tomogr. 2003;27:814–819. doi: 10.1097/00004728-200309000-00022. [DOI] [PubMed] [Google Scholar]
- 34.Ng AW, Griffith JF, Law KY, Ting JW, Tipoe GL, Ahuja AT, Chan KM. Oblique axial MR imaging of the normal anterior cruciate ligament bundles. Skeletal Radiol. 2011 doi: 10.1007/s00256-011-1208-1. [DOI] [PubMed] [Google Scholar]
- 35.Umans H, Wimpfheimer O, Haramati N, Applbaum YH, Adler M, Bosco J. Diagnosis of partial tears of the anterior cruciate ligament of the knee: value of MR imaging. AJR Am J Roentgenol. 1995;165:893–897. doi: 10.2214/ajr.165.4.7676988. [DOI] [PubMed] [Google Scholar]
- 36.Yao L, Gentili A, Petrus L, Lee JK. Partial ACL rupture: an MR diagnosis? Skeletal Radiol. 1995;24:247–251. doi: 10.1007/BF00198407. [DOI] [PubMed] [Google Scholar]
- 37.Van Dyck P, Vanhoenacker FM, Gielen JL, Dossche L, Van Gestel J, Wouters K, Parizel PM. Three tesla magnetic resonance imaging of the anterior cruciate ligament of the knee: can we differentiate complete from partial tears? Skeletal Radiol. 2011;40:701–707. doi: 10.1007/s00256-010-1044-8. [DOI] [PubMed] [Google Scholar]
- 38.Brandser EA, Riley MA, Berbaum KS, el-Khoury GY, Bennett DL. MR imaging of anterior cruciate ligament injury: independent value of primary and secondary signs. AJR Am J Roentgenol. 1996;167:121–126. doi: 10.2214/ajr.167.1.8659355. [DOI] [PubMed] [Google Scholar]
- 39.Gentili A, Seeger LL, Yao L, Do HM. Anterior cruciate ligament tear: indirect signs at MR imaging. Radiology. 1994;193:835–840. doi: 10.1148/radiology.193.3.7972834. [DOI] [PubMed] [Google Scholar]
- 40.Kaplan PA, Walker CW, Kilcoyne RF, Brown DE, Tusek D, Dussault RG. Occult fracture patterns of the knee associated with anterior cruciate ligament tears: assessment with MR imaging. Radiology. 1992;183:835–838. doi: 10.1148/radiology.183.3.1584943. [DOI] [PubMed] [Google Scholar]
- 41.Schweitzer ME, Cervilla V, Kursunoglu-Brahme S, Resnick D. The PCL line: an indirect sign of anterior cruciate ligament injury. Clin Imaging. 1992;16:43–48. doi: 10.1016/0899-7071(92)90090-v. [DOI] [PubMed] [Google Scholar]
- 42.Vahey TN, Hunt JE, Shelbourne KD. Anterior translocation of the tibia at MR imaging: a secondary sign of anterior cruciate ligament tear. Radiology. 1993;187:817–819. doi: 10.1148/radiology.187.3.8497637. [DOI] [PubMed] [Google Scholar]
- 43.Chiu SS. The anterior tibial translocation sign. Radiology. 2006;239:914–915. doi: 10.1148/radiol.2393040273. [DOI] [PubMed] [Google Scholar]
- 44.Chan WP, Peterfy C, Fritz RC, Genant HK. MR diagnosis of complete tears of the anterior cruciate ligament of the knee: importance of anterior subluxation of the tibia. AJR Am J Roentgenol. 1994;162:355–360. doi: 10.2214/ajr.162.2.8310927. [DOI] [PubMed] [Google Scholar]
- 45.Boeree NR, Ackroyd CE. Magnetic resonance imaging of anterior cruciate ligament rupture. A new diagnostic sign. J Bone Joint Surg Br. 1992;74:614–616. doi: 10.1302/0301-620X.74B4.1624525. [DOI] [PubMed] [Google Scholar]
- 46.Remer EM, Fitzgerald SW, Friedman H, Rogers LF, Hendrix RW, Schafer MF. Anterior cruciate ligament injury: MR imaging diagnosis and patterns of injury. Radiographics. 1992;12:901–915. doi: 10.1148/radiographics.12.5.1529133. [DOI] [PubMed] [Google Scholar]
- 47.Smith JP, Barrett GR. Medial and lateral meniscal tear patterns in anterior cruciate ligament-deficient knees. A prospective analysis of 575 tears. Am J Sports Med. 2001;29:415–419. doi: 10.1177/03635465010290040501. [DOI] [PubMed] [Google Scholar]
- 48.Vinson EN, Gage JA, Lacy JN. Association of peripheral vertical meniscal tears with anterior cruciate ligament tears. Skeletal Radiol. 2008;37:645–651. doi: 10.1007/s00256-008-0502-z. [DOI] [PubMed] [Google Scholar]
- 49.Laundre BJ, Collins MS, Bond JR, Dahm DL, Stuart MJ, Mandrekar JN. MRI accuracy for tears of the posterior horn of the lateral meniscus in patients with acute anterior cruciate ligament injury and the clinical relevance of missed tears. AJR Am J Roentgenol. 2009;193:515–523. doi: 10.2214/AJR.08.2146. [DOI] [PubMed] [Google Scholar]
- 50.Allen CR, Wong EK, Livesay GA, Sakane M, Fu FH, Woo SL. Importance of the medial meniscus in the anterior cruciate ligament-deficient knee. J Orthop Res. 2000;18:109–115. doi: 10.1002/jor.1100180116. [DOI] [PubMed] [Google Scholar]
- 51.Thompson WO, Fu FH. The meniscus in the cruciate-deficient knee. Clin Sports Med. 1993;12:771–796. [PubMed] [Google Scholar]
- 52.Vinson EN, Major NM, Helms CA. The posterolateral corner of the knee. AJR Am J Roentgenol. 2008;190:449–458. doi: 10.2214/AJR.07.2051. [DOI] [PubMed] [Google Scholar]
- 53.Meister BR, Michael SP, Moyer RA, Kelly JD, Schneck CD. Anatomy and kinematics of the lateral collateral ligament of the knee. Am J Sports Med. 2000;28:869–878. doi: 10.1177/03635465000280061601. [DOI] [PubMed] [Google Scholar]
- 54.Fineberg MS, Duquin TR, Axelrod JR. Arthroscopic visualization of the popliteus tendon. Arthroscopy. 2008;24:174–177. doi: 10.1016/j.arthro.2007.08.018. [DOI] [PubMed] [Google Scholar]
- 55.Peduto AJ, Nguyen A, Trudell DJ, Resnick DL. Popliteomeniscal fascicles: anatomic considerations using MR arthrography in cadavers. AJR Am J Roentgenol. 2008;190:442–448. doi: 10.2214/AJR.07.2643. [DOI] [PubMed] [Google Scholar]
- 56.Yu JS, Salonen DC, Hodler J, Haghighi P, Trudell D, Resnick D. Posterolateral aspect of the knee: improved MR imaging with a coronal oblique technique. Radiology. 1996;198:199–204. doi: 10.1148/radiology.198.1.8539378. [DOI] [PubMed] [Google Scholar]
- 57.Recht MP, Applegate G, Kaplan P, Dussault R, Schweitzer M, Dalinka MK, Resnick D. The MR appearance of cruciate ganglion cysts: a report of 16 cases. Skeletal Radiol. 1994;23:597–600. doi: 10.1007/BF02580380. [DOI] [PubMed] [Google Scholar]
- 58.McIntyre J, Moelleken S, Tirman P. Mucoid degeneration of the anterior cruciate ligament mistaken for ligamentous tears. Skeletal Radiol. 2001;30:312–315. doi: 10.1007/s002560100336. [DOI] [PubMed] [Google Scholar]
- 59.Bergin D, Morrison WB, Carrino JA, Nallamshetty SN, Bartolozzi AR. Anterior cruciate ligament ganglia and mucoid degeneration: coexistence and clinical correlation. AJR Am J Roentgenol. 2004;182:1283–1287. doi: 10.2214/ajr.182.5.1821283. [DOI] [PubMed] [Google Scholar]
- 60.Papadopoulou P. The celery stalk sign. Radiology. 2007;245:916–917. doi: 10.1148/radiol.2453050159. [DOI] [PubMed] [Google Scholar]
- 61.Tzurbakis M, Mouzopoulos G, Morakis E, Nikolaras G, Georgilas I. Intra-articular knee haemangioma originating from the anterior cruciate ligament: a case report. J Med Case Reports. 2008;2:254. doi: 10.1186/1752-1947-2-254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Majima T, Kamishima T, Susuda K. Synovial chondromatosis originating from the synovium of the anterior cruciate ligament: a case report. Sports Med Arthrosc Rehabil Ther Technol. 2009;1:6. doi: 10.1186/1758-2555-1-6. [DOI] [PMC free article] [PubMed] [Google Scholar]