Abstract
The nosological status of schizoaffective disorders remains controversial. Twin studies are potentially valuable for investigating relationships between schizoaffective-mania, schizoaffective-depression and other psychotic syndromes, but no such study has yet been reported. We ascertained 224 probandwise twin pairs (106 monozygotic, 118 same-sex dizygotic), where probands had psychotic or manic symptoms, from the Maudsley Twin Register in London (1948–1993). We investigated Research Diagnostic Criteria schizoaffective-mania, schizoaffective-depression, schizophrenia, mania and depressive psychosis primarily using a non-hierarchical classification, and additionally using hierarchical and data-derived classifications, and a classification featuring broad schizophrenic and manic syndromes without separate schizoaffective syndromes. We investigated inter-rater reliability and co-occurrence of syndromes within twin probands and twin pairs. The schizoaffective syndromes showed only moderate inter-rater reliability. There was general significant co-occurrence between syndromes within twin probands and monozygotic pairs, and a trend for schizoaffective-mania and mania to have the greatest co-occurrence. Schizoaffective syndromes in monozygotic probands were associated with relatively high risk of a psychotic syndrome occurring in their co-twins. The classification of broad schizophrenic and manic syndromes without separate schizoaffective syndromes showed improved inter-rater reliability, but high genetic and environmental correlations between the two broad syndromes. The results are consistent with regarding schizoaffective-mania as due to co-occurring elevated liability to schizophrenia, mania and depression; and schizoaffective-depression as due to co-occurring elevated liability to schizophrenia and depression, but with less elevation of liability to mania. If in due course schizoaffective syndromes show satisfactory inter-rater reliability and some specific etiological factors they could alternatively be regarded as partly independent disorders.
Keywords: schizoaffective disorder, schizophrenia, bipolar disorder, depressive psychosis, genetics
INTRODUCTION
The status of schizoaffective disorder, or disorders, is a matter of ongoing nosological controversy. Debate continues over whether they are best regarded as subtypes of schizophrenia or psychotic mood disorders; as mixtures of cases, some of whom have schizophrenia and others psychotic mood disorders; as lying between these disorders on a single liability continuum; as due to the co-occurrence of elevated liabilities to these disorders; or as partly independent disorders in their own right [Brockington and Meltzer, 1983; Kendell, 1988; Bertelsen and Gottesman, 1995; Kendler et al., 1995; Cheniaux et al., 2008; Craddock et al., 2009]. Criticisms include poor inter-rater reliability [Hiller et al., 1993; Maj et al., 2000] and instability of diagnosis over time [Schwartz et al., 2000; Laursen et al., 2005]. There are ongoing calls for the term schizoaffective disorder to be abandoned [Lake and Hurwitz, 2007; Malhi et al., 2008]. On the other hand, the manic/bipolar subtype of Research Diagnostic Criteria (RDC) schizoaffective disorder [Spitzer et al., 1978] may be particularly useful in genetic association studies [Hamshere et al., 2009; Craddock et al., 2010; Breuer et al., 2011].
The most common division of schizoaffective disorder is into manic/bipolar and depressive subtypes. In family studies, relatives of probands with both subtypes have elevated risks of schizophrenia [Kendler et al., 1986; Maier et al., 1993], the same schizoaffective subtype [Maier et al., 1993], and in most [Rice et al., 1987; Maier et al., 1993; Kendler et al., 1995] but not all studies [Kendler et al., 1986] unipolar depression. The manic/bipolar subtype is associated with a relatively high familial risk of mania/bipolar disorder in some studies [Rice et al., 1987; Maier et al., 1993], while other studies have also found the depressive subtype to be associated with elevated familial risk of mania/bipolar disorder [Kendler et al., 1986, 1995; Gershon et al., 1988]. Although the definitions of schizoaffective disorders differ notably between diagnostic classifications, the one study to employ both RDC and DSM-III-R criteria [Maier et al., 1992, 1993] found a similar pattern of familial risks with both.
These family studies assigned single main-lifetime diagnoses using a diagnostic hierarchy with schizophrenia at the top. An alternative is the non-hierarchical lifetime-ever approach where individuals can have more than one diagnosis during their lifetime, which allows investigation of within-person co-occurrence of syndromes in addition to co-occurrence in relatives. We previously used this approach in the Maudsley twin series for investigation of schizoaffective disorder in general in relation to schizophrenia and mania [Cardno et al., 2002], as did Lichtenstein et al. [2009] in a large family/adoption study of schizophrenia and mania/bipolar disorder.
Non-hierarchical lifetime-ever RDC schizoaffective-mania and schizoaffective-depression both have heritabilities of around 80% in the Maudsley twin series [Cardno et al., 1999]. Twin studies are also potentially valuable for investigating the relationships between schizoaffective-mania, schizoaffective-depression and other psychotic syndromes but, to our knowledge, no such twin study has yet been reported.
In the current study we investigated RDC schizoaffective-mania, schizoaffective-depression, and other syndromes (schizophrenia, mania and depressive psychosis) in the Maudsley twin series [Cardno et al., 1999]. In keeping with our previous investigation of general schizoaffective disorder [Cardno et al., 2002], our primary analysis was based on a non-hierarchical lifetime-ever classification. Additionally, in order to gain further perspectives on relationships between syndromes, we investigated a lifetime-only classification, where only one of the syndromes occurred; a hierarchical main-lifetime classification; a data-derived classification based on latent class analysis; and a classification featuring broad schizophrenic and manic syndromes without separate schizoaffective syndromes. We evaluated these approaches in terms of inter-rater reliability and co-occurrence of syndromes within twin probands (for the non-hierarchical lifetime-ever classification) and within twin pairs (for all classifications).
MATERIALS AND METHODS
Participants
This sample has been described in detail [Cardno et al., 1999]. Briefly, probands were ascertained from the Maudsley Twin Register in London as patients of multiple birth who had attended any facility of the Maudsley and Bethlem Royal Hospitals between 1948 and 1993, had a same-sex co-twin surviving to 15 years of age, and had suffered psychotic symptomatology or an episode of RDC mania or hypomania at some time in their lives. Probands were excluded if they had dementia or if psychotic symptoms occurred only during acute organic states. The twin register was set up prior to the establishment of Local Research Ethics Committees and the Declaration of Helsinki, but was based on consistent research ethics principles.
Zygosity determination was carried out blind to research diagnoses and was based on all available information, including analysis of genetic markers in 42% of pairs. Agreement between zygosity determination by genetic markers and physical resemblance information was 95%.
The sample comprised 224 proband wise pairs (120 male and 104 female) from which 28 probands (12.5%) were doubly ascertained. 197 pairs (87.9%) were White. The sample included the 114 twins investigated by Gottesman and Shields [1972]; 107 of these twins were followed up for an additional 25 years or until death. The mean age of co-twins at last follow-up was 46.5 years (SD=15.4). There was no substantial ascertainment bias for zygosity (106 MZ and 118 same-sex DZ pairs), but the sample probably contained more severe cases than if we had ascertained via a population-based sample [Cardno et al., 1999]. Of note, 96% of probands with lifetime-ever RDC mania had delusions or hallucinations at some time in their lives [Cardno et al., 2002].
Participant Assessments
Diagnoses were based on RDC criteria [Spitzer et al., 1978] using all available clinical information, including one or more research interviews (Gottesman and Shields’ [1972] cued-questions recorded interview and/or the Schedule for Affective Disorders and Schizophrenia – Lifetime Version (SADS-L) [Spitzer and Endicott, 1978]) in 72.8% of probands and 59.4% of co-twins, and information from case records, informants and primary care doctors. Further clinical variables, including age at onset and illness course, were rated using the Operational Criteria Checklist (OPCRIT) [McGuffin et al., 1991]. Ratings for individual members from each pair were made by separate clinical raters in all cases where there was any suggestion of concordance for psychotic or manic symptoms.
Classification of Syndromes
Non-hierarchical lifetime-ever classification
For the primary analysis, twins were rated according to whether they had ever fulfilled the criteria for RDC schizoaffective disorder manic and depressed types (which we refer to as schizoaffective-mania and schizoaffective-depression), schizophrenia, mania and depressive psychosis. If a twin had more than one syndrome during their lifetime, each syndrome was rated as present.
Additionally, we investigated the following classifications:
Lifetime-only classification
The same syndromes were used, but a syndrome was rated as present if it was the only one of the five syndromes to occur during an individual’s lifetime.
Hierarchical main-lifetime classification
Main-lifetime syndromes were assigned using a diagnostic hierarchy as in previous family studies of schizoaffective disorders [Kendler et al., 1986, 1995; Rice et al., 1987; Gershon et al., 1988; Maier et al., 1992, 1993]. The order of syndromes (from top to bottom) was schizophrenia, schizoaffective-mania, schizoaffective-depression, mania/bipolar disorder, and depressive psychosis. If a twin had more than one syndrome during their lifetime, the highest syndrome in the hierarchy was taken as the main-lifetime syndrome.
Data-derived classification
We entered the five lifetime-ever syndromes as categorical binary variables (present/absent) into a latent class analysis in the 219 individual twins who had at least one of these syndromes. The analysis was performed using Latent GOLD model-based clustering [Statistical Innovations Inc., 2005], which produces classes based on co-occurrence of syndromes, and gives both a probabilistic assignment and a modal (most likely) assignment of individuals to classes. The optimal number of classes was determined by minimising the Bayesian Information Criterion (BIC).
Then, as an aid to interpretation, and to simplify the classification process, we performed a classification and regression tree (CART) analysis to yield a decision aid. This is an iterative approach that aimed to find the optimal set of classification rules for assigning individuals to their modal class from the latent class analysis. The classification rules were based on combinations of the presence or absence of the psychotic syndromes and allowed the generation of new categorical syndromes. This analysis was performed with R Library ‘rpart’ software [Therneau and Atkinson, 2010]. We used the entropy option with the default complexity parameter setting to select the set of classification rules.
Classification without schizoaffective syndromes
We investigated a classification approach which involved combining syndromes so there were no distinct schizoaffective syndromes. We defined two broad syndromes based on symptom groups: a broad schizophrenic syndrome comprising lifetime-ever schizophrenia, schizoaffective-mania, or schizoaffective-depression (i.e., any syndrome that included characteristic schizophrenic symptoms); and a broad manic syndrome, comprising mania or schizoaffective-mania (i.e., any syndrome that included a manic syndrome). A broad depressive syndrome could also be envisaged but, in order to be properly evaluated, should probably include probands with non-psychotic depressive syndromes, which was beyond the scope of the current study. Individual twins could have one, both or neither of the broad lifetime-ever syndromes (schizophrenic and manic).
Frequency of occurrence, demographics and illness history variables for each syndrome are shown in Supplementary Table 1.
Statistical Analysis
Inter-rater reliability
Inter-rater reliability of syndromes was based on assessment of 30 cases and expressed as the mean kappa coefficient (κ) between pairs of raters [Cardno et al., 1999]. The reliabilities for non-hierarchical lifetime-ever syndromes have been reported by Cardno et al. [1999]; none of the other reliabilities have been previously reported.
Concordances, correlations and modeling
We calculated the proband wise concordance for syndrome co-occurrence a) within individual twin probands (for non-hierarchical lifetime-ever syndromes) and b) within MZ and DZ pairs (for all syndromes). Because the significance of concordances varies according to the lifetime risk of the syndrome, we also calculated tetrachoric correlations using Mx statistical modeling software [Neale et al., 2003]. These are based on a liability-threshold model [Neale and Cardon, 1992; Rijsdijk and Sham, 2002] and take into account the lifetime morbid risk of the syndrome in the general population. Population risks were estimated by extrapolation from local case register data for schizophrenia, and the relative frequencies of syndromes within the sample, as we have done previously [Cardno et al., 1999]. Correlations with confidence intervals that did not include zero were interpreted as being statistically significant at P<0.05, two-tailed. No adjustment for multiple testing was made as the work was exploratory and the analyses were unlikely to be statistically independent of each other.
If two syndromes share any kind of risk factor (genetic or environmental) the tetrachoric correlations within probands are expected to be statistically significant, and similar in MZ and DZ probands unless zygosity-specific factors are operating. If the syndromes share familial risk factors in common, significant within-pair correlations are also expected, and if there are shared genetic risk factors the within-pair correlations are expected to be greater in MZ than DZ pairs [Kendler et al., 1992].
Additionally, for each syndrome, we investigated concordance for a general category of any RDC psychotic syndrome in co-twins (presence of any of the five syndromes or RDC unspecified functional psychosis), because of evidence that schizoaffective disorders may be associated with relatively high levels of total psychotic and affective illness in relatives [Kendler et al., 1995].
In the classification without separate schizoaffective syndromes, both broad schizophrenia and broad mania were relatively frequent in the sample, so we applied biometrical modeling in Mx to estimate heritability, and genetic and environmental correlations between the two syndromes, using the same methods as in previous analyses of this sample [Cardno et al., 1999, 2002]. We employed general ACE models that include additive genetic (a2), common environmental (c2) and individual-specific (non-shared) environmental (e2) effects.
RESULTS
Non-Hierarchical Lifetime-Ever Classification
Using Landis and Koch’s [1977] criteria as a guide, schizoaffective-mania and schizoaffective-depression had only moderate inter-rater reliability (mean κ=0.58 and 0.46, respectively), while schizophrenia, mania and depressive psychosis had substantial reliability (mean κ=0.64–0.68: Cardno et al., [1999] and Supplementary Table 1).
Concordances and tetrachoric correlations are shown in Table I (within MZ and DZ probands) and Table II (in MZ pairs). (DZ pairs were less informative because of the smaller overall number of concordant pairs, but the results are given in Supplementary Table 2). There was a general pattern of significant co-occurrence between syndromes, shown by correlations with confidence intervals above zero. For all syndrome combinations this occurred in at least two of the three analyses (in MZ probands, DZ probands and MZ pairs) and for most syndrome combinations all three correlations were significant. All syndrome combinations showed significant co-occurrence in MZ pairs, consistent with some overlap in familial influences on all pairs of syndromes. The most consistent trend was for the correlations between schizoaffective-mania and mania to be relatively high. Although the confidence intervals for these correlations overlapped with those of other syndrome combinations, they were the highest-ranking cross-syndrome correlations in MZ probands and MZ pairs, and second highest in DZ probands (the marginally highest-ranking correlation being between depressive psychosis and mania).
TABLE I.
Co-occurrence of RDC Non-Hierarchical Lifetime-Ever Syndromes within Monozygotic (MZ) and Dizygotic (DZ) Probandsa
| Proband syndrome (number of probands) | Co-occurring syndrome number of probands with co-occurrence (%);tetrachoric correlation (95%CI)b | ||||
|---|---|---|---|---|---|
| Schizophrenia | Schizoaffective-mania | Schizoaffective-depression | Mania | Depressive psychosis | |
| MZ | |||||
| Schizophrenia (49) | - | 6 (12.2) 0.77 (0.55 to 1.00) |
1 (2.0) 0.36 (−0.05 to 0.68) |
5 (10.2) 0.61 (0.38 to 0.79) |
3 (6.1) 0.51 (0.24 to 0.74) |
| Schizoaffective-mania (13) | 6 (46.2) 0.73 (0.54 to 0.86) |
- | 2 (15.4) 0.66 (0.34 to 0.87) |
7 (53.8) 0.87 (0.71 to 0.95) |
0 (0.0) |
| Schizoaffective-depression (12) | 1 (8.3) 0.34 (−0.06 to 0.64) |
2 (16.7) 0.68 (0.35 to 0.88) |
- | 1 (8.3) 0.46 (0.04 to 0.74) |
2 (16.7) 0.62 (0.29 to 0.83) |
| Mania (22) | 5 (22.7) 0.59 (0.38 to 0.76) |
7 (31.8) 0.89 (0.72 to 1.00) |
1 (4.5) 0.46 (0.04 to 0.76) |
- | 2 (9.1) 0.53 (0.21 to 0.77) |
| Depressive psychosis (20) | 3 (15.0) 0.49 (0.22 to 0.69) |
0 (0.0) | 2 (10.0) 0.61 (0.28 to 0.84) |
2 (10.0) 0.52 (0.21 to 0.75) |
- |
| DZ | |||||
| Schizophrenia (57) | - | 3 (5.3) 0.56 (0.28 to 0.79) |
3 (5.3) 0.56 (0.28 to 0.79) |
5 (8.8) 0.57 (0.35 to 0.76) |
3 (5.3) 0.48 (0.21 to 0.70) |
| Schizoaffective-mania (10) | 3 (30.0) 0.62 (0.34 to 0.81) |
- | 1 (10.0) 0.57 (0.13 to 0.85) |
5 (50.0) 0.85 (0.66 to 0.95) |
3 (30.0) 0.75 (0.48 to 0.91) |
| Schizoaffective-depression (13) | 3 (23.1) 0.56 (0.29 to 0.75) |
1 (7.7) 0.52 (0.09 to 0.81) |
- | 2 (15.4) 0.58 (0.26 to 0.80) |
1 (7.7) 0.46 (0.04 to 0.75) |
| Mania (27) | 5 (18.5) 0.54 (0.33 to 0.71) |
5 (18.5) 0.76 (0.55 to 0.91) |
2 (7.4) 0.56 (0.24 to 0.79) |
- | 9 (33.3) 0.83 (0.68 to 0.93) |
| Depressive psychosis (20) | 3 (15.0) 0.49 (0.22 to 0.69) |
3 (15.0) 0.70 (0.42 to 0.89) |
1 (5.0) 0.47 (0.05 to 0.77) |
9 (45.0) 0.87 (0.73 to 0.95) |
- |
An individual twin may have more than one lifetime-ever syndrome.
Tetrachoric correlations were not calculated where there was no co-occurrence. Frequency of co-occurrence and correlations for schizophrenia with mania from Cardno et al. [2002].
TABLE II.
Co-occurrence of RDC Non-Hierarchical Lifetime-Ever Syndromes in Monozygotic (MZ) Twin Pairsa
| Proband syndrome (number of proband wise pairs) | Co-twin syndrome number of concordant pairs (%);tetrachoric correlation (95%CI)b | |||||
|---|---|---|---|---|---|---|
| Schizophrenia | Schizoaffective-mania | Schizoaffective-depression | Mania | Depressive psychosis | Any psychotic syndromec | |
| Schizophrenia (49) | 20 (40.8) 0.83 (0.72 to 0.91) |
2 (4.1) 0.50 (0.17 to 0.77) |
2 (4.1) 0.50 (0.17 to 0.77) |
4 (8.2) 0.55 (0.31 to 0.76) |
2 (4.1) 0.42 (0.11 to 0.68) |
28 (57.1) |
| Schizoaffective-mania (13) | 3 (23.1) 0.56 (0.29 to 0.75) |
4 (30.8) 0.82 (0.59 to 0.94) |
2 (15.4) 0.66 (0.34 to 0.87) |
5 (38.5) 0.79 (0.59 to 0.91) |
2(15.4) 0.60 (0.28 to 0.82) |
9 (69.2) |
| Schizoaffective-depression (12) | 3 (25.0) 0.58 (0.31 to 0.77) |
1 (8.3) 0.54 (0.10 to 0.82) |
5 (41.7) 0.88 (0.69 to 0.97) |
1 (8.3) 0.46 (0.04 to 0.74) |
4 (33.3) 0.77 (0.54 to 0.91) |
9 (75.0) |
| Mania (22) | 3 (13.6) 0.47 (0.21 to 0.68) |
5 (22.7) 0.81 (0.59 to 0.95) |
3 (13.6) 0.69 (0.41 to 0.89) |
8 (36.4) 0.83 (0.66 to 0.93) |
3 (13.6) 0.62 (0.35 to 0.82) |
14 (63.6) |
| Depressive psychosis (20) | 2 (10.0) 0.40 (0.10 to 0.63) |
1 (5.0) 0.47 (0.05 to 0.77) |
1 (5.0) 0.47 (0.05 to 0.77) |
2 (10.0) 0.52 (0.21 to 0.75) |
2 (10.0) 0.54 (0.22 to 0.77) |
10 (50.0) |
An individual twin may have more than one lifetime-ever syndrome.
Tetrachoric correlations were not calculated where there was no co-occurrence, nor for the category of any psychotic syndrome. Concordances and correlations for the same syndrome (e.g., probands with schizophrenia and co-twins with schizophrenia) from Cardno et al. [1999], and concordances for schizophrenia with mania from Cardno et al. [2002].
Any of the five syndromes or RDC unspecified functional psychosis.
Correlations between schizoaffective-mania and schizoaffective-depression were not higher than correlations with other syndromes. Apart from the trend towards relatively high correlations between schizoaffective-mania and mania, there was no clearly consistent clustering of higher correlations between schizoaffective syndromes and schizophrenia versus affective syndromes – rather, there were notable inter-correlations between all syndromes.
Among the 12 MZ probands with schizoaffective-depression, two were bipolar (i.e., also had schizoaffective-mania or mania) and 10 were unipolar. The significant co-occurrence between MZ probands with schizoaffective-depression and co-twins with schizoaffective-mania, and also co-twins with mania (Table II), was due to a unipolar proband who had a co-twin with both schizoaffective-mania and mania.
There was a trend for the highest risks of any psychotic syndrome to be in co-twins of MZ probands with schizoaffective-mania (69.2%) and schizoaffective-depression (75.0%) (Table II).
Lifetime-Only Classification
The most notable finding here was that schizoaffective-mania rarely occurred in the absence of another syndrome (it occurred alone in only two probands - one MZ, one DZ). Compared with the number of probands with lifetime-ever schizoaffective-mania (n=23), this was an 11.5 times reduction, while for the other syndromes there was only a 1.2 to 2.3 times reduction (Supplementary Table 1). This finding suggests relatively high diagnostic instability to and/or from schizoaffective-mania. The small number of probands with lifetime-only schizoaffective-mania (and schizoaffective-depression), meant that substantive conclusions could not be derived from the patterns of within-pair co-occurrence (Supplementary Tables 3 and 4).
Hierarchical Main-Lifetime Classification
The number of probands with schizoaffective syndromes was smaller than in the primary non-hierarchical lifetime-ever classification (schizoaffective-mania: hierarchical n=14, non-hierarchical n=23; schizoaffective-depression: hierarchical n=19, non-hierarchical n=25) because it only included probands with schizoaffective syndromes who had not also had an episode of schizophrenia (probands with episodes of both a schizoaffective syndrome and schizophrenia were diagnosed as having schizophrenia in the hierarchical classification).
Inter-rater reliability remained only moderate for schizoaffective-mania and schizoaffective-depression (mean κ=0.43 and 0.42, respectively) and substantial for the other syndromes (mean κ=0.64–0.78: Supplementary Table 1).
Co-occurrence within MZ pairs is shown in Table III. (DZ pairs were again less informative (Supplementary Table 5)). As with the non-hierarchical classification, schizoaffective-mania showed significant co-occurrence with all other syndromes, and relatively high concordance for any psychotic syndrome (in this case 100%). There was zero concordance for schizoaffective-mania itself, possibly because of the smaller number of probands in the hierarchical classification. Schizoaffective-depression showed significant co-occurrence with the non-manic syndromes (schizophrenia, schizoaffective-depression and depressive psychosis), but not the manic syndromes (schizoaffective-mania and mania/bipolar disorder), although this trend in favour of a unipolar-bipolar distinction for schizoaffective syndromes is tempered by the sample size limitations. Schizoaffective-depression also showed relatively high concordance for any psychotic syndrome (66.7%).
TABLE III.
Co-occurrence of RDC Hierarchical Main-Lifetime Syndromes in Monozygotic (MZ) Twin Pairsa
| Proband syndrome (numbser of proband wise pairs) | Co-twin syndrome number of concordant pairs (%);tetrachoric correlation (95%CI)b | |||||
|---|---|---|---|---|---|---|
| Schizophrenia | Schizoaffective-mania | Schizoaffective-depression | Mania/bipolar disorder | Depressive psychosis | Any psychotic syndromec | |
| Schizophrenia (49) | 20 (40.8) 0.83 (0.72 to 0.91) |
2 (4.1) 0.59 (0.24 to 0.89) |
2 (4.1) 0.56 (0.21 to 0.84) |
0 (0.0) | 1 (2.0) 0.38 (−0.04 to 0.71) |
28 (57.1) |
| Schizoaffective-mania (7) | 3 (42.9) 0.68 (0.41 to 0.85) |
0 (0.0) | 1 (14.3) 0.65 (0.20 to 0.90) |
1 (14.3) 0.61 (0.17 to 0.87) |
1 (14.3) 0.63 (0.18 to 0.88) |
7 (100.0) |
| Schizoaffective-depression (9) | 3 (33.3) 0.63 (0.36 to 0.81) |
0 (0.0) | 1 (11.1) 0.61 (0.17 to 0.88) |
0 (0.0) | 1 (11.1) 0.59 (0.15 to 0.86) |
6 (66.7) |
| Mania/bipolar disorder (12) | 0 (0.0) | 0 (0.0) | 1 (8.3) 0.58 (0.14 to 0.86) |
3 (25.0) 0.77 (0.50 to 0.92) |
1 (8.3) 0.55 (0.12 to 0.84) |
7 (58.3) |
| Depressive psychosis (13) | 1 (7.7) 0.32 (−0.06 to 0.61) |
0 (0.0) | 0 (0.0) | 1 (7.7) 0.51 (0.09 to 0.79) |
2 (15.4) 0.67 (0.35 to 0.87) |
6 (46.2) |
Diagnostic hierarchy of syndromes in the order presented from schizophrenia (top) to depressive psychosis (bottom).
Tetrachoric correlations were not calculated where there was no co-occurrence, nor for the category of any psychotic syndrome.
Any of the five syndromes or RDC unspecified functional psychosis.
Data-Derived Classification
In the latent class analysis, a four-class model fitted best with a clear Bayesian Information Criterion (BIC) minimum (BIC values were: for 2 classes, 1107.52; 3 classes, 1095.55; 4 classes, 1089.56; 5 classes, 1107.10). The rules derived from the classification tree approach for assigning twins to classes were as follows: class 1 – presence of schizophrenia and absence of depressive psychosis; class 2 – presence of mania or schizoaffective mania and absence of the other syndromes; class 3 – presence of depressive psychosis; and class 4 – presence of schizoaffective-depression and absence of schizophrenia and depressive psychosis. Thus, the two schizoaffective syndromes characterised different classes (classes 2 and 4), while mania and schizoaffective-mania characterised the same class (class 2). Concordances and correlations for the data-derived syndromes are shown in Supplementary Table 6.
Classification without Schizoaffective Syndromes
Inter-rater reliability for both the lifetime-ever broad schizophrenic and broad manic syndrome was substantial (0.71 and 0.77, respectively), as was reliability for the broad mixed schizophrenic-manic syndrome (co-occurring broad schizophrenia and broad mania: 0.63) (Supplementary Table 1)). The two broad syndromes had virtually indistinguishable profiles of gender, age at onset and illness course (Supplementary Table 1).
Broad schizophrenia and broad mania showed a high degree of co-occurrence and high genetic and individual-specific environmental correlations (0.83 and 0.72, respectively), consistent with a high level of etiological overlap. Details of concordances, correlations and model-fitting are shown in Supplementary Tables 7 and 8 and accompanying notes.
DISCUSSION
Inter-Rater Reliability
In the primary non-hierarchical lifetime-ever classification, and in all other classifications in this study where RDC schizoaffective-mania or schizoaffective-depression were treated as individual syndromes, the inter-rater reliability was only moderate. Inter-rater reliability for general schizoaffective disorder has been reported to be even lower [Maj et al., 2000] and, even where high, has been associated with difficult diagnostic decisions [Kendler et al., 1995]. The issue is not specific to one diagnostic system [Hiller et al., 1993; Jäger et al., 2011]. In the current study, reliability notably improved and became substantial when schizoaffective syndromes were combined with other syndromes in the broad mixed schizophrenic-manic phenotype (co-occurring broad schizophrenia and broad mania). This phenotype is similar to the broad ‘middle psychosis’ discussed by Craddock et al. [2009].
In future studies of schizoaffective disorders it will be important to assess and report inter-rater reliability. If there are problems, one option would be to consider using broader combined syndromes, if appropriate. The situation may be helped if the proposed changes aimed at improving inter-rater reliability of, e.g., DSM-5 schizoaffective disorders [American Psychiatric Association, 2011], are successful.
Schizoaffective Disorder or Disorders?
Non-hierarchical lifetime-ever schizoaffective-mania and schizoaffective-depression did not co-occur with each other more than with other syndromes. They also characterised different classes in the data-derived classification. The results of family studies are conflicting, some supporting the distinction between schizoaffective-mania and schizoaffective-depression [Rice et al., 1987; Maier et al., 1993] and some not [Kendler et al., 1986, 1995], so it would be valuable, wherever possible, to consider schizoaffective-mania and schizoaffective-depression separately in order to gain further evidence on this issue.
Conceptual Models
Schizoaffective-mania
Conceptual models of schizoaffective-mania in relation to schizophrenia and mania/bipolar disorder are outlined in Table IV, focusing on expected patterns of co-occurrence in twin pairs. Against model 1 (subtype of schizophrenia), co-twins of probands with schizoaffective-mania had a notably different pattern of co-occurrence from co-twins of probands with schizophrenia with both non-hierarchical and hierachical approaches (Tables II and III, respectively: comparing the first two rows of correlations). Consistent with model 2 (subtype of mania/bipolar disorder), with the non-hierarchical approach, co-twins of probands with schizoaffective-mania had a similar pattern of co-occurrence to co-twins of probands with mania (Table II: comparing correlations in rows two and four). However, against model 2, with the hierarchical approach co-twins of probands with schizoaffective-mania had notably higher co-occurrence of schizophrenia than co-twins of probands with mania/bipolar disorder (correlations of 0.68 versus 0: Table III). Against model 3 (mixture of cases of schizophrenia and mania/bipolar disorder), co-twins of probands with schizoaffective-mania had a notably higher risk of any psychotic syndrome than co-twins of probands with either schizophrenia or mania/bipolar disorder (Tables II and III), rather than an intermediate risk, as would be expected.
TABLE IV.
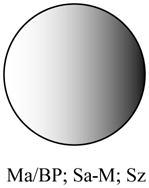
Conceptual Models of Schizoaffective-Mania (Sa-M) in Relation to Schizophrenia (Sz) and Mania/Bipolar Disorder (Ma/BP) with Expected Patterns of Co-occurrence in Twin Pairs
| Modela | Diagrammatic representation | Expected pattern of co-occurrence in twin pairs |
|---|---|---|
| 1. Subtype of schizophrenia |
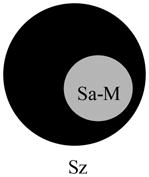
|
Twin probands with Sa-M and twin probands with Sz → relatively similar pattern of co-occurrence in co-twins |
| 2. Subtype of mania/bipolar disorder |
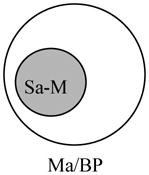
|
Twin probands with Sa-M and twin probands with Ma/BP → relatively similar pattern of co-occurrence in co-twins |
| 3. Mixture of cases of schizophrenia and mania/bipolar disorder |

|
Twin probands with Sa-M → pattern of co-occurrence intermediate between Sz and Ma/BP in co-twins |
| 4. Single liability continuum |
|
Twin probands with Sa-M → both Sz and Ma/BP elevated in co-twins Etiological influences on Sa-M, Sz and Ma/BP entirely overlap (quantitative differences in loading of etiological influences contribute to differences between syndromes) |
| 5. Co-occurring elevated liability to schizophrenia and mania/bipolar disorder |

|
Twin probands with Sa-M → both Sz and Ma/BP elevated in co-twins All etiological influences on Sa-M are also etiological influences on Sz and Ma/BP |
| 6. Partly independent disorder |
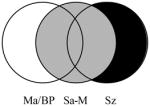
|
Twin probands with Sa-M → both Sz and Ma/BP elevated in co-twins Some etiological influences on Sa-M are not shared with either Sz or Ma/BP |
Diagrams for models 4–6 adapted from Craddock et al. [2009]. In variants of model 6 some segments of the central gray circle may not be present, e.g., if there are no etiological factors that influence Sa-M and Ma/BP, but not Sz.
The general pattern of results showed schizoaffective-mania to have a notable familial association with both schizophrenia and mania/bipolar disorder, which is consistent with models 4 through 6 where schizoaffective-mania has an intermediate position between schizophrenia and mania/bipolar disorder. Against model 4 (single liability continuum), there is evidence from this and other samples that schizophrenia and mania/bipolar disorder only partly share etiological factors in common [Cardno et al., 2002; Mortensen et al., 2003, 2010; Murray et al., 2004; International Schizophrenia Consortium, 2009; Lichtenstein et al., 2009; Van Snellenberg and de Candia, 2009; Gottesman et al., 2010]. Model 5 (co-occurring elevated liability to schizophrenia and mania/bipolar disorder) and model 6 (partly independent disorder) cannot be formally distinguished on the basis of the current study results. The key issue is whether there are notable etiological influences on schizoaffective-mania that are not shared with schizophrenia or mania/bipolar disorder. For general schizoaffective disorder, we were able to investigate this using multivariate biometrical modeling [Cardno et al., 2002], but the lack of concordant DZ pairs with schizoaffective-mania, precludes this analysis in the current study.
A further approach is to consider measured risk factors. In this respect it will be interesting to see whether, for example, the evidence of a relatively specific association with genetic markers in GABAA receptor genes [Craddock et al., 2010; Breuer et al., 2011] is fully confirmed. However, in order for schizoaffective-mania to be satisfactorily regarded as a partly independent disorder it will also be important to improve its inter-rater reliability, as discussed above.
To sum up, the results of this study are consistent with regarding schizoaffective-mania as due to co-occurring elevated liability to schizophrenia and mania/bipolar disorder. There is supportive evidence from family studies, which show an elevated risk of both schizophrenia and mania/bipolar disorder in relatives [Kendler et al., 1986; Maier et al., 1993]. Schizoaffective-mania is also likely to be associated with elevated liability to depression. Only psychotic depression was included in the current study, but there is an association between schizoaffective-mania and elevated familial risk of unipolar depression in most [Rice et al., 1987; Maier et al., 1993; Kendler et al., 1995], although not all [Kendler et al., 1986], family studies.
If, in the future, schizoaffective-mania shows satisfactory inter-rater reliability and some specific etiological factors, it could alternatively be regarded as a partly independent disorder.
Schizoaffective-depression
Non-hierarchical lifetime-ever schizoaffective-depression showed significant familial co-occurrence with all other syndromes (Table II). The pattern of co-occurrence in co-twins was notably different from co-twins of probands with schizophrenia or depressive psychosis, which goes against schizoaffective-depression being regarded as a subtype of schizophrenia or depressive psychosis. Also, the relatively high risk of any psychotic syndrome in co-twins goes against it being regarded as a mixture of cases, some of whom have schizophrenia and others depressive psychosis.
Against the single liability model, it is unlikely that schizophrenia and depressive psychosis completely share etiological factors. For example, co-occurrence within probands and twin pairs in the current study was only moderate (Tables I-III). Regarding the partly independent disorder model, there are currently no confirmed etiological influences on schizoaffective-depression that are not shared with schizophrenia or depressive psychosis.
The results are consistent with regarding schizoaffective-depression as a marker of co-occurring elevated liability to schizophrenia, depression and mania, but with the level of liability to mania being lower than for schizoaffective-mania in the current study. Family studies support an elevated liability to schizophrenia [Maj et al., 1991; Maier et al., 1993; Kendler et al., 1995]; most [Rice et al., 1987; Maier et al., 1993; Kendler et al., 1995] but not all [Kendler et al., 1986] support an elevated liability to depression; and the results are mixed regarding mania, with some showing an association [Kendler et al., 1986, 1995; Gershon et al., 1988] and some not [Rice et al., 1987; Maier et al., 1993]. As with schizoaffective-mania, if, in the future, schizoaffective-depression shows satisfactory reliability and some specific etiological factors, it could alternatively be regarded as a partly independent disorder.
Data-derived classification
This analysis was mainly useful for providing evidence, from an alternative perspective, for the relatively close relationship between schizoaffective-mania and mania, and the lack of a particularly close relationship between the two schizoaffective syndromes. It is not clear whether any of the data-derived syndromes will become useful phenotypes in their own right.
Classification without schizoaffective syndromes
This analysis resulted in notably improved inter-rater reliability compared with the separate schizoaffective syndromes, but the broad syndromes had high overlap of genetic and environmental influences and indistinguishable profiles for gender, age at onset and illness course. Many studies of schizophrenia and bipolar disorder include schizoaffective disorders with both, and these spectrum phenotypes are likely to have considerable etiological overlap.
Limitations
To our knowledge, this is the largest systematically-ascertained twin sample to date covering the full range of psychoses and with detailed information on symptoms. However, even with an ascertainment period spanning 45 years, the sample size was limited, and in particular there were no DZ pairs concordant for schizoaffective-mania or schizoaffective-depression. This meant that within-pair analyses were mainly based on MZ pairs and multivariate biometrical modeling of schizoaffective and other syndromes was not feasible, although it was feasible for investigation of the broad schizophrenic and manic syndromes. It is likely that familial factors made an important contribution to the co-occurrence between syndromes, but the extent to which familial and non-familial factors produce similar or differing patterns of co-occurrence [Kendler et al., 2011] is not known.
Inter-rater reliability has been discussed above. Unreliability is likely to widen the confidence intervals around the correlations which estimate the degree of co-occurrence between syndromes [Hutcheon et al., 2010] and reduce the chances of finding statistically significant co-occurrence. It is therefore notable that the schizoaffective syndromes showed significant co-occurrence with the other syndromes despite their only moderate reliability, and it is expected that the estimates of co-occurrence would become more precise if reliability improved.
The results could have differed with longer follow-up, although large differences would not be expected as mean length of follow-up was 22 years (SD=12.5). Exploration of gender effects was limited by sample size and the fact that only same-sex pairs were included. However, risks in males and females were not significantly different in a family study of RDC schizoaffective manic and depressive subtypes [Rice et al., 1987].
The results could have differed if we had employed a diagnostic classification other than RDC. However, the one family study to employ both RDC and DSM-III-R criteria [Maier et al., 1992, 1993] found a similar pattern of familial risks with both systems. There is close correspondence between the DSM-IV and the RDC mainly-schizophrenic forms of schizoaffective disorder [Peralta and Cuesta, 2008]. In the current sample, 5/25 (20%) of MZ probands with lifetime-ever schizoaffective syndromes had predominantly psychotic symptoms, and none of their co-twins had schizophrenia (Supplementary Table 9), which does not support this sub-syndrome as having an especially close relationship with schizophrenia, albeit with small numbers.
To our knowledge, this is the first report of inter-rater reliability and degree of co-occurrence for this range of schizoaffective and other syndrome definitions, so it will be valuable to independently replicate the results presented here. The optimal conceptualization of schizoaffective syndromes will depend in part on the particular research or clinical purpose. Hence, it will also be valuable to incorporate associations with other relevant variables [Laursen et al., 2007; Cheniaux et al., 2008; Malhi et al., 2008; Craddock et al., 2009], other schizoaffective subtypes [e.g., Maj, 1989; Marneros, 2003], subforms of schizophrenia, and a broader range of manic and depressive syndromes including non-psychotic forms and the degree of mood-incongruent psychotic symptoms [Craddock et al., 2004; Peralta and Cuesta, 2008].
Supplementary Material
Acknowledgments
Part of this work was carried out while Dr Cardno was a Medical Research Council (UK) Clinical Training Fellow. The National Institute of Mental Health (MH44359) and the Stanley Medical Research Institute provided grant support that enabled collection of the clinical data. We are indebted to the twins, their families and clinical staff. We gratefully acknowledge the late Dr Eliot Slater for establishing the Maudsley Twin Register and J. Shields, J. Marshall, B. Coid, A. Macdonald, T. Ribchester, N. Davies, P. Venturi, L. Jones, S. Lewis, A. Farmer, A. Reveley, P. Sham and C. Allan for their work on the Maudsley twin psychosis series.
References
- American Psychiatric Association. DSM-5 development. [Accessed October 3, 2011];2011 ( http://www.dsm5.org/ProposedRevisions/Pages/proposedrevision.aspx?rid=144#)
- Bertelsen A, Gottesman II. Schizoaffective psychoses: Genetical clues to classification. Am J Med Genet Part B. 1995;60:7–11. doi: 10.1002/ajmg.1320600103. [DOI] [PubMed] [Google Scholar]
- Breuer R, Hamshere ML, Strohmaier J, Mattheisen M, Degenhardt F, Meier S, Paul T, O’Donovan MC, Mühleisen TW, Schulze TG, Nöthen MM, Cichon S, Craddock N, Rietschel M. Independent evidence for the selective influence of GABAA receptors on one component of the bipolar disorder phenotype. Mol Psychiatry. 2011;16:587–589. doi: 10.1038/mp.2010.67. [DOI] [PubMed] [Google Scholar]
- Brockington IF, Meltzer HY. The nosology of schizoaffective psychosis. Psychiatr Dev. 1983;1:317–338. [PubMed] [Google Scholar]
- Cardno AG, Marshall EJ, Coid B, Macdonald AM, Ribchester TR, Davies NJ, Venturi P, Jones LA, Lewis SW, Sham PC, Gottesman II, Farmer AE, McGuffin P, Reveley AM, Murray RM. Heritability estimates for psychotic disorders: The Maudsley twin psychosis series. Arch Gen Psychiatry. 1999;56:162–168. doi: 10.1001/archpsyc.56.2.162. [DOI] [PubMed] [Google Scholar]
- Cardno AG, Rijsdijk FV, Sham PC, Murray RM, McGuffin P. A twin study of genetic relationships between psychotic symptoms. Am J Psychiatry. 2002;159:539–545. doi: 10.1176/appi.ajp.159.4.539. [DOI] [PubMed] [Google Scholar]
- Cheniaux E, Landeira-Fernandez J, Lessa Telles L, Lessa JL, Dias A, Duncan T, Versiani M. Does schizoaffective disorder really exist? A systematic review of the studies that compared schizoaffective disorder with schizophrenia or mood disorders. J Affect Disord. 2008;106:209–217. doi: 10.1016/j.jad.2007.07.009. [DOI] [PubMed] [Google Scholar]
- Craddock N, Jones I, Kirov G, Jones L. The Bipolar Affective Disorder Dimension Scale (BADDS) - a dimensional scale for rating lifetime psychopathology in bipolar spectrum disorders. BMC Psychiatry. 2004;4:19. doi: 10.1186/1471-244X-4-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Craddock N, Jones L, Jones IR, Kirov G, Green EK, Grozeva D, Moskvina V, Nikolov I, Hamshere ML, Vukcevic D, Caesar S, Gordon-Smith K, Fraser C, Russell E, Norton N, Breen G, St Clair D, Collier DA, Young AH, Ferrier IN, Farmer A, McGuffin P, Holmans PA, Donnelly P, Owen MJ, O’Donovan MC Wellcome Trust Case Control Consortium (WTCCC) Strong genetic evidence for a selective influence of GABAA receptors on a component of the bipolar disorder phenotype. Mol Psychiatry. 2010;15:146–153. doi: 10.1038/mp.2008.66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Craddock N, O’Donovan MC, Owen MJ. Psychosis genetics: Modeling the relationship between schizophrenia, bipolar disorder, and mixed (or “schizoaffective”) psychoses. Schizophr Bull. 2009;35:482–490. doi: 10.1093/schbul/sbp020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gershon ES, DeLisi LE, Hamovit J, Nurnberger JI, Jr, Maxwell ME, Schreiber J, Dauphinais D, Dingman CW, II, Guroff JJ. A controlled family study of chronic psychoses: Schizophrenia and schizoaffective disorder. Arch Gen Psychiatry. 1988;45:328–336. doi: 10.1001/archpsyc.1988.01800280038006. [DOI] [PubMed] [Google Scholar]
- Gottesman II, Laursen TM, Bertelsen A, Mortensen PB. Severe mental disorders in offspring with 2 psychiatrically ill parents. Arch Gen Psychiatry. 2010;67:252–257. doi: 10.1001/archgenpsychiatry.2010.1. [DOI] [PubMed] [Google Scholar]
- Gottesman II, Shields J. Schizophrenia and genetics: A twin vantage point. New York: Academic Press; 1972. [Google Scholar]
- Hamshere ML, Green EK, Jones IR, Jones L, Moskvina V, Kirov G, Grozeva D, Nikolov I, Vukcevic D, Caesar S, Gordon-Smith K, Fraser C, Russell E, Breen G, St Clair D, Collier DA, Young AH, Ferrier IN, Farmer A, McGuffin P, Holmans PA, Owen MJ, O’Donovan MC, Craddock N Wellcome Trust Case Control Consortium. Genetic utility of broadly defined bipolar schizoaffective disorder as a diagnostic concept. Br J Psychiatry. 2009;195:23–29. doi: 10.1192/bjp.bp.108.061424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hiller W, Dichtl G, Hecht H, Hundt W, von Zerssen D. An empirical comparison of diagnoses and reliabilities in ICD-10 and DSM-III-R. Eur Arch Psychiatry Clin Neurosci. 1993;242:209–217. doi: 10.1007/BF02189965. [DOI] [PubMed] [Google Scholar]
- Hutcheon JA, Chiolero A, Hanley JA. Random measurement error and regression dilution bias. BMJ. 2010;340:1402–1406. doi: 10.1136/bmj.c2289. [DOI] [PubMed] [Google Scholar]
- International Schizophrenia Consortium. Common polygenic variation contributes to risk of schizophrenia and bipolar disorder. Nature. 2009;460:748–752. doi: 10.1038/nature08185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jäger M, Haack S, Becker T, Frasch K. Schizoaffective disorder - an ongoing challenge for psychiatric nosology. Eur Psychiatry. 2011;26:159–165. doi: 10.1016/j.eurpsy.2010.03.010. [DOI] [PubMed] [Google Scholar]
- Kendell RE. Other functional psychoses. In: Kendell RE, Zeally AK, editors. Companion to psychiatric studies. 4. Edinburgh: Churchill Livingstone; 1988. pp. 362–373. [Google Scholar]
- Kendler KS, Aggen SH, Knudsen GP, Røysamb E, Neale MC, Reichborn-Kjennerud T. The structure of genetic and environmental risk factors for syndromal and subsyndromal common DSM-IV axis I and all axis II disorders. Am J Psychiatry. 2011;168:29–39. doi: 10.1176/appi.ajp.2010.10030340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kendler KS, Gruenberg AM, Tsuang MT. A DSM-III family study of the nonschizophrenic psychotic disorders. Am J Psychiatry. 1986;143:1098–1105. doi: 10.1176/ajp.143.9.1098. [DOI] [PubMed] [Google Scholar]
- Kendler KS, McGuire M, Gruenberg AM, Walsh D. Examining the validity of DSM-III-R schizoaffective disorder and its putative subtypes in the Roscommon family study. Am J Psychiatry. 1995;152:755–764. doi: 10.1176/ajp.152.5.755. [DOI] [PubMed] [Google Scholar]
- Kendler KS, Neale MC, Kessler RC, Heath AC, Eaves LJ. Major depression and generalized anxiety disorder: Same genes, (partly) different environments? Arch Gen Psychiatry. 1992;49:716–722. doi: 10.1001/archpsyc.1992.01820090044008. [DOI] [PubMed] [Google Scholar]
- Lake CR, Hurwitz N. Schizoaffective disorder merges schizophrenia and bipolar disorders as one disease - there is no schizoaffective disorder. Curr Opin Psychiatry. 2007;20:365–379. doi: 10.1097/YCO.0b013e3281a305ab. [DOI] [PubMed] [Google Scholar]
- Landis JR, Koch GC. The measurement of observer agreement for categorical data. Biometrics. 1977;33:1089–1091. [PubMed] [Google Scholar]
- Laursen TM, Labouriau R, Licht RW, Bertelsen A, Munk-Olsen T, Mortensen PB. Family history of psychiatric illness as a risk factor for schizoaffective disorder: A Danish register-based cohort study. Arch Gen Psychiatry. 2005;62:841–848. doi: 10.1001/archpsyc.62.8.841. [DOI] [PubMed] [Google Scholar]
- Laursen TM, Munk-Olsen T, Nordentoft M, Mortensen PB. A comparison of selected risk factors for unipolar depressive disorder, bipolar affective disorder, schizoaffective disorder, and schizophrenia from a Danish population-based cohort. J Clin Psychiatry. 2007;68:1673–1681. doi: 10.4088/jcp.v68n1106. [DOI] [PubMed] [Google Scholar]
- Lichtenstein P, Yip BH, Björk C, Pawitan Y, Cannon TD, Sullivan PF, Hultman CM. Common genetic determinants of schizophrenia and bipolar disorder in Swedish families: A population-based study. Lancet. 2009;373:234–239. doi: 10.1016/S0140-6736(09)60072-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maier W, Lichtermann D, Minges J, Hallmayer J, Heun R, Benkert O, Levinson DF. Continuity and discontinuity of affective disorders and schizophrenia: Results of a controlled family study. Arch Gen Psychiatry. 1993;50:871–883. doi: 10.1001/archpsyc.1993.01820230041004. [DOI] [PubMed] [Google Scholar]
- Maier W, Lichtermann D, Minges J, Heun R, Hallmayer J, Benkert O. Schizoaffective disorder and affective disorders with mood-incongruent psychotic features: Keep separate or combine? Evidence from a family study. Am J Psychiatry. 1992;149:1666–1673. doi: 10.1176/ajp.149.12.1666. [DOI] [PubMed] [Google Scholar]
- Maj M. A family study of two subgroups of schizoaffective patients. Br J Psychiatry. 1989;154:640–643. doi: 10.1192/bjp.154.5.640. [DOI] [PubMed] [Google Scholar]
- Maj M, Pirozzi R, Formicola AM, Bartoli L, Bucci P. Reliability and validity of the DSM-IV diagnostic category of schizoaffective disorder: Preliminary data. J Affect Disord. 2000;57:95–98. doi: 10.1016/s0165-0327(99)00059-2. [DOI] [PubMed] [Google Scholar]
- Maj M, Starace F, Pirozzi R. A family study of DSM-III-R schizoaffective disorder, depressive type, compared with schizophrenia and psychotic and nonpsychotic major depression. Am J Psychiatry. 1991;148:612–616. doi: 10.1176/ajp.148.5.612. [DOI] [PubMed] [Google Scholar]
- Malhi GS, Green M, Fagiolini A, Peselow ED, Kumari V. Schizoaffective disorder: Diagnostic issues and future recommendations. Bipolar Disord. 2008;10:215–230. doi: 10.1111/j.1399-5618.2007.00564.x. [DOI] [PubMed] [Google Scholar]
- Marneros A. The schizoaffective phenomenon: The state of the art. Acta Psychiatr Scand, Suppl. 2003;108 (Suppl 418):29–33. doi: 10.1034/j.1600-0447.108.s418.7.x. [DOI] [PubMed] [Google Scholar]
- McGuffin P, Farmer A, Harvey I. A polydiagnostic application of operational criteria in studies of psychotic illness: Development and reliability of the OPCRIT system. Arch Gen Psychiatry. 1991;48:764–770. doi: 10.1001/archpsyc.1991.01810320088015. [DOI] [PubMed] [Google Scholar]
- Mortensen PB, Pedersen CB, Melbye M, Mors O, Ewald H. Individual and familial risk factors for bipolar affective disorders in Denmark. Arch Gen Psychiatry. 2003;60:1209–1215. doi: 10.1001/archpsyc.60.12.1209. [DOI] [PubMed] [Google Scholar]
- Mortensen PB, Pedersen MG, Pedersen CB. Psychiatric family history and schizophrenia risk in Denmark: Which mental disorders are relevant? Psychol Med. 2010;40:201–210. doi: 10.1017/S0033291709990419. [DOI] [PubMed] [Google Scholar]
- Murray RM, Sham P, Van Os J, Zanelli J, Cannon M, McDonald C. A developmental model for similarities and dissimilarities between schizophrenia and bipolar disorder. Schizophr Res. 2004;71:405–416. doi: 10.1016/j.schres.2004.03.002. [DOI] [PubMed] [Google Scholar]
- Neale MC, Boker SM, Xie G, Maes HH. Mx: Statistical modelling. 6. Richmond, VA: VCU Box 900126, Department of Psychiatry; 2003. [Google Scholar]
- Neale MC, Cardon LR. Methodology for genetic studies of twins and families. Dordrecht, The Netherlands: Kluwer Academic Publishers; 1992. [Google Scholar]
- Peralta V, Cuesta MJ. Exploring the borders of the schizoaffective spectrum: A categorical and dimensional approach. J Affect Disord. 2008;108:71–86. doi: 10.1016/j.jad.2007.09.009. [DOI] [PubMed] [Google Scholar]
- Rice J, Reich T, Andreasen NC, Endicott J, Van Eerdewegh M, Fishman R, Hirschfeld RMA, Klerman GL. The familial transmission of bipolar illness. Arch Gen Psychiatry. 1987;44:441–447. doi: 10.1001/archpsyc.1987.01800170063009. [DOI] [PubMed] [Google Scholar]
- Rijsdijk FV, Sham PC. Analytic approaches to twin data using structural equation models. Brief Bioinform. 2002;3:119–133. doi: 10.1093/bib/3.2.119. [DOI] [PubMed] [Google Scholar]
- Schwartz JE, Fennig S, Tanenberg-Karant M, Carlson G, Craig T, Galambos N, Lavelle J, Bromet EJ. Congruence of diagnoses 2 years after a first-admission diagnosis of psychosis. Arch Gen Psychiatry. 2000;57:593–600. doi: 10.1001/archpsyc.57.6.593. [DOI] [PubMed] [Google Scholar]
- Spitzer RL, Endicott J. Schedule for affective disorders and schizophrenia: Lifetime version. New York: New York State Psychiatric Institute; 1978. [Google Scholar]
- Spitzer RL, Endicott J, Robins E. Research diagnostic criteria for a selected group of functional disorders. 3. New York: New York State Psychiatric Institute; 1978. [Google Scholar]
- Statistical Innovations Inc. Latent GOLD 4.0. Belmont, MA: Statistical Innovations Inc; 2005. [Google Scholar]
- Therneau TM, Atkinson B. rpart: Recursive partitioning. [Accessed October 3, 2011];R package version 3.1–46. 2010 Ported to R by Brian Ripley( http://CRAN.R-project.org/package=rpart)
- Van Snellenberg JX, de Candia T. Meta-analytic evidence for familial coaggregation of schizophrenia and bipolar disorder. Arch Gen Psychiatry. 2009;66:748–755. doi: 10.1001/archgenpsychiatry.2009.64. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


