The repair protein trefoil factor 2 promotes Th2 responses to helminth infection and allergens in part by inducing IL-33.
Abstract
The molecular mechanisms that drive mucosal T helper type 2 (TH2) responses against parasitic helminths and allergens remain unclear. In this study, we demonstrate in mice that TFF2 (trefoil factor 2), an epithelial cell–derived repair molecule, is needed for the control of lung injury caused by the hookworm parasite Nippostrongylus brasiliensis and for type 2 immunity after infection. TFF2 is also necessary for the rapid production of IL-33, a TH2-promoting cytokine, by lung epithelia, alveolar macrophages, and inflammatory dendritic cells in infected mice. TFF2 also increases the severity of allergic lung disease caused by house dust mite antigens or IL-13. Moreover, TFF2 messenger RNA expression is significantly increased in nasal mucosal brushings during asthma exacerbations in children. These experiments extend the biological functions of TFF2 from tissue repair to the initiation and maintenance of mucosal TH2 responses.
Type 2 inflammatory responses (T helper type 2 [TH2] cells, IL-4, 5,13, IgE, eosinophils, basophils, mast cells, alternatively activated macrophages, and goblet cell metaplasia) are generated in over 3 billion people worldwide that suffer from allergic disease or harbor parasitic helminth infections (Baena-Cagnani, 2001; Braman, 2006; Nair et al., 2006; Brooker, 2010; Brooker et al., 2010). Although there has been much progress in the understanding of mechanisms responsible for allergen-driven airway hyperreactivity (AHR) and the expulsion of gastrointestinal (GI) nematodes, the initiation of these responses remains poorly understood (Paul and Zhu, 2010). Current hypotheses have focused on mucosal epithelia as an important source of cytokines that drive type 2 responses (Fallon et al., 2006; Neill et al., 2010; Paul and Zhu, 2010). However, few, if any, studies have uncovered the molecular mechanisms that link mucosal injury with the preferential induction of TH2 responses.
IL-33 (IL-1-F11) is a unique IL-1 family cytokine produced from damaged epithelia that utilizes NF-κB and MAPK activation to promote type 2 inflammation through the IL-1 receptor–related protein ST2 (Ali et al., 2007; Humphreys et al., 2008; Kurowska-Stolarska et al., 2008, 2009; Rankin et al., 2010). Epithelia and myeloid lineage cells at the mucosal interface may release IL-33 as an alarmin for the rapid induction of IL-13–driven immunity (Préfontaine et al., 2010). However, the mechanisms that regulate IL-33 release and whether IL-33 functions as a cytokine or nuclear factor remain unclear (Carriere et al., 2007; Ohno et al., 2009). Although epithelial cell death by necrosis may serve as one mechanism for IL-33 release, recent evidence shows that viral infection can result in IL-33 production from alveolar macrophages (Chang et al., 2011). Furthermore, IL-33 administration to mice infected with the GI nematode Trichuris muris promotes worm expulsion (Humphreys et al., 2008), but the endogenous mechanisms that regulate IL-33 production during worm infection are currently unknown.
Trefoil factor family peptides (TFF1–3) are protease-resistant mediators that serve critical roles in mucosal barrier function and repair (Podolsky, 1997; Paulsen et al., 2008). These proteins are constitutively released within the mucus gel layer that covers ocular, urinary, respiratory, and GI surfaces (Taupin and Podolsky, 2003). Furthermore, the trefoil motif, which resembles a three-leaf clover, is highly conserved among TFF proteins from frogs to humans (Taupin and Podolsky, 2003). TFFs are produced from epithelia, fibroblasts, and tissue macrophages within hours of injury to promote epithelial cell restitution through mechanisms that may require CXCR4, the putative TFF2 receptor (Dubeykovskaya et al., 2009). As such, TFF2 promotes organ regeneration and healing in several injury models (Farrellet al., 2002; Poulsen et al., 2005; Fox et al., 2007; Kurt-Jones et al., 2007). TFF2 expression is up-regulated during tissue injury associated with allergic lung inflammation in mice through STAT-6–dependent and –independent mechanisms (Nikolaidis et al., 2003, 2006) However, its absence did not affect lung inflammation or mucus metaplasia (Nikolaidis et al., 2006). Thus, its biological importance in the context of type 2 immunopathologies is not well understood.
This study investigated whether TFF2 served any role in the development of allergic lung disease or after infection with the hookworm Nippostrongylus brasiliensis. Our results indicate that TFF2 (a) promotes type 2 lung immunopathology induced by allergen or IL-13, (b) controls the extent of lung injury caused by migratory infectious stage larvae (L3), and (c) modulates early TH2 development. This mechanism involves rapid, coordinated IL-33 production from lung epithelia, alveolar macrophages, and inflammatory DCs. IL-33 induction requires the putative TFF2 receptor, CXCR4, but occurs independently of the TLR adaptor molecule MyD88. Collectively, these experiments demonstrate an important role for TFF2 in the regulation of IL-33 release at mucosal surfaces and the development of type 2 immune responses.
RESULTS
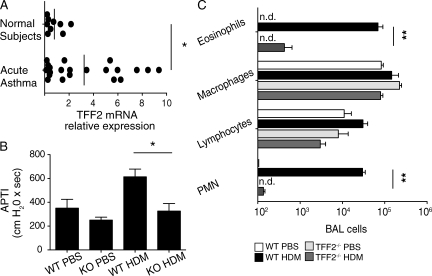
TFF2 expression is a central feature of asthma in humans and mice
TFF2 expression is induced within airway epithelial cells of mice challenged with allergen or type 2 cytokines (Nikolaidis et al., 2003; Follettie et al., 2006). To determine whether increased TFF2 expression was a feature of human asthma, we obtained nasal mucosa biopsies from pediatric patients experiencing asthma exacerbations and compared their TFF2 messenger RNA (mRNA) levels to nonasthmatic control subjects. TFF2 was significantly elevated in asthma patients over controls (Fig. 1 A), which prompted us to evaluate the biological role of TFF2 in the pathogenesis of murine asthma driven by house dust mite (HDM) antigens or IL-13 administration. Exposure of TFF2−/− mice to HDM antigens caused significantly less AHR (Fig. 1 B) and reduced the numbers of eosinophils and neutrophils recruited into the bronchoalveolar lavage (BAL), as compared with HDM-sensitized WT mice (Fig. 1 C). There were no differences between naive WT and TFF2−/− mice in the numbers of eosinophil or neutrophil precursors within the BM (not depicted). This may suggest that TFF2−/− mice have the normal potential to produce granulocytes but show impaired allergic airway inflammation in response to HDM antigens.
Figure 1.
Clinical asthma is marked by increased TFF2 expression, and TFF2−/− mice are resistant to HDM-induced murine asthma. (A) Quantification of TFF2 mRNA transcripts from nasal mucosal brushings of normal subjects (n = 9) or patients experiencing acute asthma exacerbation (n = 23). Each dot represents an individual patient. Vertical bars indicate the mean. (B) Airway pressure time index (APTI) of WT and TFF2−/− mice after immunization with 1× PBS or HDM antigen extract. Means ± SE of eight mice/group are shown. (C) Quantification of inflammatory cells recovered from the BAL fluid of WT and TFF2−/− mice after intratracheal administration of HDMs or saline. Means ± SE of four mice/group are shown. Data are representative of two to three independent experiments (*, P < 0.05; **, P < 0.01). n.d., not detected.
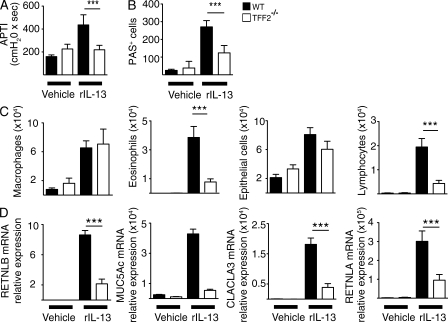
We also investigated whether the TFF2 deficiency modulated the development of type 2 allergic lung disease in an IL-13–driven model of murine asthma (Wills-Karp et al., 1998). rIL-13–treated WT C57BL/6 mice developed robust AHR, goblet cell metaplasia, and eosinophilic airway inflammation; however, these responses were significantly attenuated in TFF2−/− mice (Fig. 2, A–C). Moreover, IL-13–treated TFF2−/− mice showed impaired induction of lung mRNA transcripts for the goblet cell–specific genes MUC5AC, CLCA3, and RETNLB (Fig. 2 D), as well as the alternatively activated macrophage marker RETNLA (Fig. 2 D). Collectively, these findings suggest that TFF2 deficiency protects mice against experimental asthma induced by allergen or IL-13 and that increased TFF2 expression in asthma patients is associated with disease exacerbation.
Figure 2.
TFF2 is required for IL-13–driven allergic airway inflammation and airway hyperresponsiveness. (A) Airway pressure time index (APTI) of WT and TFF2−/− mice was measured 8 d after administration of rIL-13 (5 µg/mouse) or vehicle (1× PBS). Data represent mean ± SE of eight mice/group. (B) Quantification of PAS-positive cells within airway epithelium at day 8 after injection of rIL-13 or PBS. Data represent mean ± SE of eight mice/group. (C) Numbers of epithelia, macrophages, eosinophils, and lymphocytes in BAL fluid at day 8 after injection of rIL-13 or PBS. Data represent mean ± SE of eight mice/group. (D) Quantification of mRNA transcripts encoding RETNLB, MUC5AC, CLCA3, and RETNLA in the lung at day 8 after injection of rIL-13 or PBS. Data represent mean ± SE of four to six mice/group. Data are representative of four independent experiments (***, P < 0.001).
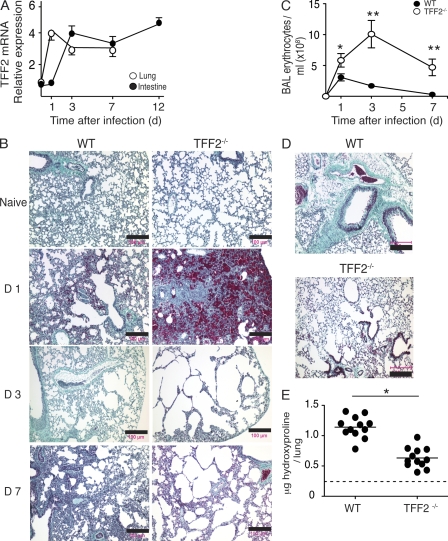
TFF2 regulates hookworm-mediated lung injury
TFF2 production can be rapidly induced, within minutes of mucosal injury (Taupin et al., 1999), as well as during allergen-induced inflammation (Taupin et al., 1999; Nikolaidis et al., 2003). We investigated whether TFF2 regulated tissue repair and/or TH2-dependent host immunity against the parasitic helminth N. brasiliensis. In this model, migratory L3 enter the lung tissues between 0 and 2 d after infection and cause hemorrhagic tissue injury that resolves over several weeks after infection (Marsland et al., 2008). Subsequently, by day 3 after infection, >90% of worms have exited the lung and enter the small intestine (Herbert et al., 2009). As shown in Fig. 3 A, TFF2 mRNA levels increased over threefold within the lung at day 1 and within the jejunum at day 3 after infection of WT C57BL/6 mice with 500 N. brasiliensis L3. This expression pattern for TFF2 was consistent with the kinetics of parasite migration through the host and suggested a potential role for this molecule in each mucosal compartment.
Figure 3.
Hookworm infection induces the expression of TFF2, which limits hemorrhagic lung injury but promotes fibrosis and airway hyperresponsiveness. (A) Time course evaluation of TFF2 mRNA transcript levels in lung and jejunum of N. brasiliensis–infected WT C57BL/6 mice. Means ± SE of five to six mice/group are shown. (B) Masson’s Trichrome staining for collagen (green) on paraffin-embedded lung tissues of naive mice or after infection with 500 N. brasiliensis larvae at the indicated time points. Erythrocytes stain crimson red. Representative images are shown. (C) Numbers of erythrocytes in the BAL fluid of WT versus TFF2−/− mice infected with 500 N. brasiliensis larvae at the indicated time points. Means ± SE of five to six mice/group are shown. Data are representative of two to three independent experiments (*, P < 0.05; **, P < 0.01). (D) Masson’s Trichrome staining for collagen (green) on paraffin-embedded lung tissues of WT and TFF2−/− mice on day 28 after infection with 500 N. brasiliensis larvae. Representative images are shown. (E) Hydroxyproline content of lung tissue at day 28 after infection. Each point represents an individual lobe of lung. The dotted line indicates the level of hydroxyproline in naive WT mouse lung (*, P < 0.05). Horizontal bars indicate the mean. Data are representative of two independent experiments. Bars, 100 µm.
To investigate whether TFF2 served a critical function within hookworm-infected lungs, we compared lung histology between infected WT and TFF2−/− strains. Although naive TFF2−/− lung tissue showed moderately enlarged alveolar space at baseline, infected TFF2−/− animals developed excessive lung hemorrhage at day 1 and enlarged distal airspaces from alveolar wall destruction at days 3 and 7 after infection (Fig. 3 B). In contrast, WT mice developed focal hemorrhagic lesions around migrating parasites at day 1 after inoculation, followed by a progressive closure of the damaged areas of lung tissue at days 3 and 7 after inoculation (Fig. 3 B). To quantitatively measure lung injury, the numbers of erythrocytes within the BAL fluid were counted from cohorts of WT and TFF2−/− mice between days 0 and 7 after infection (Meyer et al., 1998). Fig. 3 C shows that from as early as day 1 after infection, TFF2−/− lung tissues had significantly greater numbers of erythrocytes than the WT strain and remained elevated over the course of observation. This was consistent with the histological evidence of excessive lung hemorrhage in the absence of TFF2.
TFF2 was also necessary for chronic lung repair after N. brasiliensis infection–induced injury. At day 28 after infection, when parasites were no longer present (not depicted), TFF2−/− mice had much less collagen deposition within their lungs, as determined by histological staining (Fig. 3 D) and measurement of hydroxyproline (essential component of collagen; Fig. 3 E). TFF2−/− mice did show less destruction of alveolar walls during the chronic repair phase (day 28), as compared with the acute injury phase (day 3), which implies redundancy between TFF2 and many other wound-healing mechanisms (Barron and Wynn, 2011; Brancato and Albina, 2011). Thus, N. brasiliensis infection–induced TFF2 production within the lung promotes both tissue repair and fibrosis.
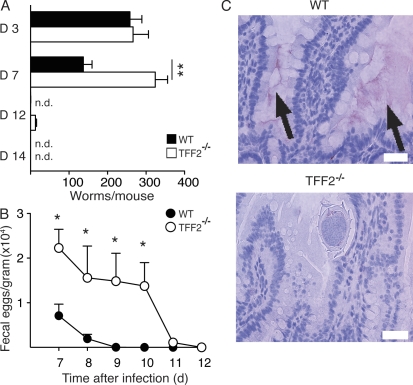
TFF2 promotes worm expulsion from the GI tract
TFF2 was also rapidly induced within the GI tract after the entry of worms into the intestinal lumen. We did not find any gross histological evidence of gut injury caused by N. brasiliensis in either WT or TFF2−/− mice (not depicted). Therefore, we investigated whether TFF2 promoted the clearance of lumen-dwelling worms from infected mice. As shown in Fig. 4 A, the numbers of parasites that initially migrated from the lung to the intestine on day 3 were not different between WT and TFF2−/− strains. However, worm expulsion, which is an IL-4– and IL-13–dependent process (Finkelman et al., 2004), was significantly impaired in TFF2−/− mice at days 7 and 12, in comparison with the WT strain (Fig. 4 A). Similarly, TFF2−/− mice harbored significantly more worm eggs in their stool, as compared with WT controls between days 7 and 10 after infection (Fig. 4 B). TFF2 was secreted into the gut lumen of infected WT mice at day 7 after infection, which correlated with the onset of worm expulsion, whereas the lack of TFF2 was associated with increased worm burden (Fig. 4 C). Thus, immunity against N. brasiliensis adult worms in the intestine is accompanied by increased TFF2 production. In the absence of TFF2, more worm eggs are passed into the environment and parasites reside within their hosts for longer periods of time.
Figure 4.
TFF2 promotes spontaneous expulsion and termination of egg production during N. brasiliensis infection. (A) N. brasiliensis intestinal worm numbers recovered from WT versus TFF2−/− mice at the indicated time points after a primary infection. Means ± SE of 8–10 mice/group are shown. n.d., not detected. (B) N. brasiliensis fecal egg numbers in WT versus TFF2−/− mice after a primary infection. Means ± SE of 8–10 mice/group are shown. (C) Immunostaining for Tff2 protein (magenta precipitate indicated by arrows) in paraffin-embedded sections of jejunum from N. brasiliensis–infected WT (top) or TFF2−/− (bottom) mice at day 7 after infection. Bars, 70 µm. Data are representative of four independent experiments (*, P < 0.05; **, P < 0.01).
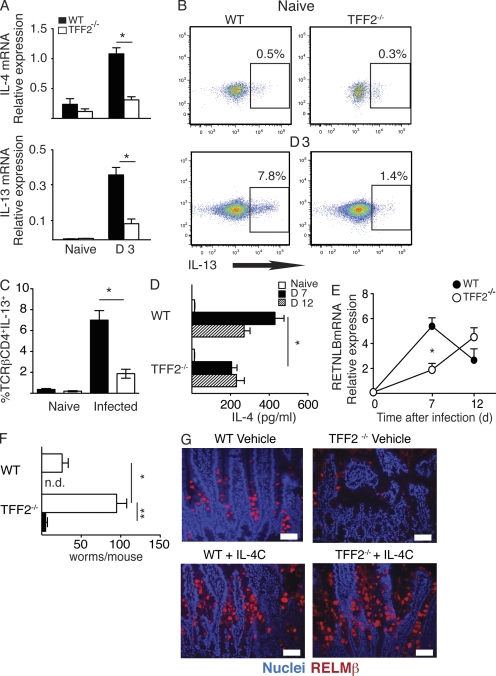
TFF2 promotes an early TH2 response during N. brasiliensis infection
IL-4 and IL-13 are both necessary and sufficient for host protection against most GI nematodes (Finkelman et al., 2004) and most allergic lung immunopathologies (Wills-Karp et al., 1998). Given that TFF2−/− mice had significant defects in both worm clearance and allergic lung pathology, we postulated that TFF2 might promote type 2 cytokine production. Consistent with this hypothesis, TFF2−/− mice displayed defects in both the early (lung) and late (intestinal) stages of N. brasiliensis infection. In the early phase, TFF2−/− mice expressed fewer IL-4 and IL-13 lung mRNA transcripts than WT mice at day 3 after inoculation (Fig. 5 A). Intracellular IL-13 staining of TCR-β+CD4+ cells within the lung draining LNs (Fig. 5 B and Fig. S1) revealed that at day 3 after infection, TFF2−/− mice produced three- to fourfold less IL-13 than infected WT animals (Fig. 5, B and C), yet there were no obvious differences in T cell recruitment to the LN between these strains.
Figure 5.
Early defect TH2 expansion and RELM-β expression in TFF2−/− mice is responsible for delayed immunity against N. brasiliensis infection. (A) IL4 and IL13 mRNA transcripts in naive WT and TFF2−/− mice or 3 d after N. brasiliensis infection. Means ± SE of five to six mice/group are shown. (B) Representative dot plot showing IL-13–positive CD4+ lymphocytes within the LN of naive WT and TFF2−/− mice or 3 d after N. brasiliensis infection. Four individual mice/group were analyzed for infected samples, whereas naive LNs were pooled from two to three mice. (C) Mean percentage (±SE) of IL-13–positive CD4+ lymphocytes from the experiment described in B. (D) Serum IL-4 abundance, as determined by in vivo cytokine capture assay at 0, 7, and 12 d after infection. Means ± SE of five to six mice/group are shown. (E) Intestinal RELM-β mRNA transcript levels at 0, 7, and 12 d after infection. Means ± SE of five to six mice/group are shown. (F) N. brasiliensis intestinal worms recovered from intestinal lumen on day 8 from WT versus TFF2−/− mice that were injected with vehicle or rIL-4/anti–IL-4 complexes (IL-4C) at days 0 and 4. Means ± SE of five to six mice/group are shown. n.d., not detected. (G) Immunofluorescence staining for RELM-β within the jejunum of mice from the experiment described in F. Cell nuclei stained with DAPI. Bars, 50 µm. Data are representative of three to four independent experiments (*, P < 0.05; **, P < 0.01).
During the later stages of N. brasiliensis infection, TFF2−/− mice secreted less IL-4 than WT animals at day 7 after infection (Fig. 5 D). Also, compared with WT controls, TFF2−/− mice had significantly fewer intestinal mRNA transcripts for RELM-β (Resistin-like molecule β), an IL-4/IL-13–dependent goblet cell–derived cytokine which is both necessary and sufficient for the normal expulsion of N. brasiliensis adult worms from the GI tract (Fig. 5 E; Herbert et al., 2009). However, these defects were transient, as TFF2−/− mice produced IL-4 and expressed RELM-β transcripts at levels equivalent to infected WT mice by day 12 after infection (Fig. 5 E), which was closely associated with the ability of TFF2−/− mice to eventually clear worm infection by day 14 after infection.
Based on these observations, we hypothesized that the delay in IL-4 secretion, RELM-β production, and worm clearance in TFF2−/− mice resulted from a proximal defect in type 2 cytokine production. To directly test this possibility, we administered rIL-4 to mice in the form of IL-4/anti–IL-4 mAb complexes (IL-4C; Finkelman et al., 1993) to infected WT or TFF2−/− mice on days 0 and 4 followed by quantitation of adult worm numbers at day 8 after infection. As predicted, IL-4C administration to TFF2−/− mice dramatically increased RELM-β production (Fig. 5 F) and successfully cleared intestinal worms (Fig. 5 G). Collectively, these data indicate that the delayed immunity against N. brasiliensis in TFF2−/− animals results from an early defect in type 2 cytokine production.
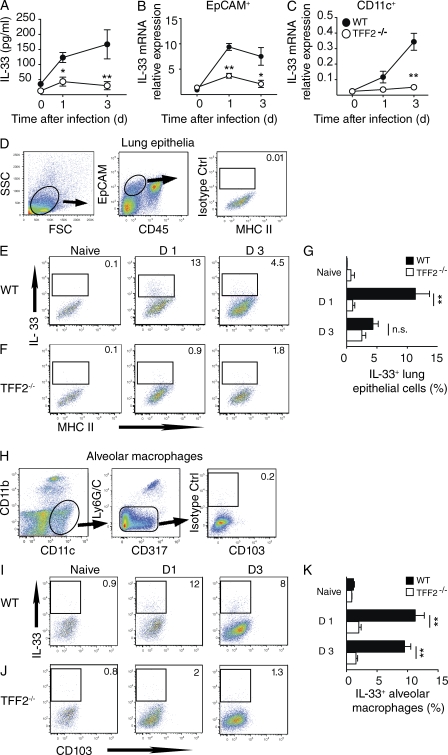
TFF2 is required for hookworm-induced IL-33 production within lung epithelia and alveolar macrophages
Given that early IL-4 and IL-13 production was significantly impaired in worm-infected TFF2−/− mice, the underlying mechanisms were further investigated. Although there are multiple epithelial cell–derived cytokines that can promote type 2 immunity (Ito et al., 2005; Schmitz et al., 2005; Saenz et al., 2010), we focused on IL-33 (IL-1-F11), an IL-1 family cytokine which has been reported to elicit TH2-associated inflammation after its release from damaged epithelial cells (Schmitz et al., 2005; Carriere et al., 2007; Kurowska-Stolarska et al., 2009). Strikingly, N. brasiliensis–infected WT mice produced highly elevated IL-33 levels within the BAL fluid at both days 1 and 3 after infection (Fig. 6 A). In contrast, TFF2−/− mice produced very low amounts of IL-33 at these time points (Fig. 6 A).
Figure 6.
TFF2 is necessary for N. brasiliensis–induced IL-33 production from lung epithelial cells and alveolar macrophages. (A) Levels of IL-33 within the BAL fluid of WT and TFF2−/− mice after N. brasiliensis infection. Means ± SE of four to five mice/group are shown. (B and C) IL33 mRNA levels within EpCAM+ (B) or CD11c+ cells (C; 106 total cells) sorted from the lungs of naive or N. brasiliensis–infected WT and TFF2−/− mice with magnetic beads. Means ± SE of four individual mice/group are shown. (D) Gating strategy for the identification of lung epithelia from whole lung tissue as FSCHiSSCMed, EpCAM+, CD45−, and MHC class II− cells. Representative data from a WT mouse at day 3 after infection stained intracellularly with a PE-labeled isotype control IgG. (E and F) Representative dot plots showing intracellular IL-33 staining within WT or TFF2−/− lung epithelia at the indicated times after N. brasiliensis infection. Numbers indicate the percentage of positive cells. (G) Quantification of the experiment described in E and F that shows the mean ± SE of four individual mice/group. (H) Gating strategy for the identification of alveolar macrophages from whole lung tissue as CD11b−, CD11c+, LyCG/C−, CD317+/−, and CD103−. (I and J) Representative dot plots showing intracellular IL-33 staining within WT or TFF2−/− alveolar macrophages at the indicated times after N. brasiliensis infection. Numbers indicate the percentage of positive cells. (K) Quantification of the experiment described in I and J that shows the mean ± SE of four individual mice/group. Data are representative of two to four independent experiments for each genotype analyzed per time point (*, P < 0.05; **, P < 0.01).
To identify the potential cellular sources of IL-33, our initial experiments focused on lung epithelia and macrophage/DC lineage cells within whole lung digests. We used mAb specific for either epithelial cell adhesion molecule (EpCAM), which is expressed broadly on epithelial cells, or CD11c, which is highly expressed on alveolar macrophages/DCs (van Rijt et al., 2005; Trzpis et al., 2007). Once isolated by magnetic bead sorting, IL-33 mRNA transcript levels were determined from 106 cells of each population. Surprisingly, IL-33 expression was induced in both lung epithelia (Fig. 6 B) and macrophages/DCs (Fig. 6 C) from N. brasiliensis–infected WT mice at days 1 and 3 after infection. However, parasitized TFF2−/− mice only slightly increased their IL-33 mRNA levels in these cell populations (Fig. 6, B and C). Similar differences in IL-33 levels between strains were detected by immunofluorescence staining (not depicted).
To specifically determine whether lung epithelia or alveolar macrophages produced IL-33 at the protein level, we evaluated these populations by flow cytometry. Our gating strategy defined lung epithelia as EpCAM+, CD45−, and MHC class II−, to exclude the large population of EpCAM+ cells that coexpressed CD45+ (common leukocyte antigen; Fig. 6 D). In WT mice, N. brasiliensis infection caused a 10-fold increase of IL-33+ lung epithelia at day 1 after infection but only a fourfold increase by day 3 (Fig. 6 E). In contrast, TFF2−/− lung epithelia showed moderate differences after infection that were not significant (Fig. 6, F and G). This demonstrates that TFF2 is necessary for the rapid, but transient induction of IL-33 within lung epithelia after N. brasiliensis infection.
Given that TFF2 regulated IL-33 from lung epithelia, we investigated whether it was also important for IL-33 production from alveolar macrophages. Our gating strategy defined alveolar macrophages as CD11b−, CD11c+, CD317+/−, Ly6G/C−, and CD103− (Fig. 6 H; Lambrecht and Hammad, 2009). Results shown in Fig. 6 I demonstrate that WT macrophages also up-regulated IL-33 production at both days 1 and 3 after infection. In contrast, these IL-33+ alveolar macrophages were significantly less abundant within TFF2−/− lung tissues at both time points (Fig. 6, J and K). Overall, this indicates that TFF2 promotes IL-33 mRNA and protein expression in lung epithelia and alveolar macrophages within the first 3 d after hookworm infection.
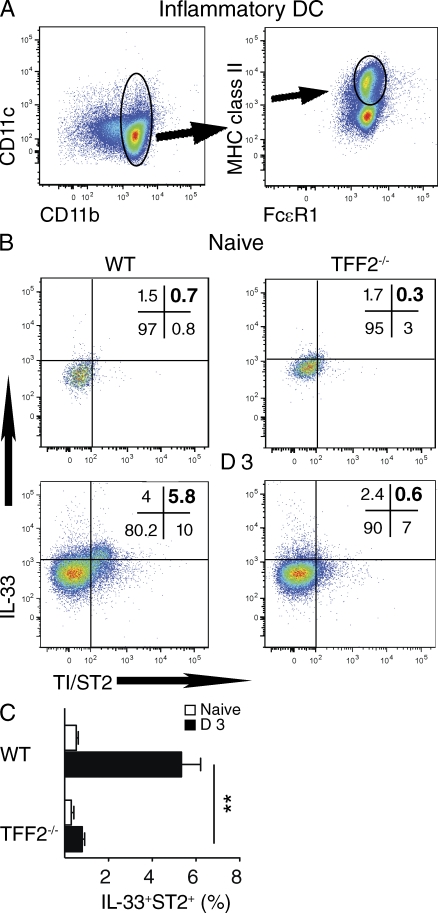
TFF2 deficiency impairs IL-33 production from inflammatory DCs, and IL-33 is necessary for host immunity against N. brasiliensis
Inflammatory DCs have been shown as critical drivers for the in vivo differentiation of TH2 cells (Hammad et al., 2010; Phythian-Adams et al., 2010). Therefore, it was important to determine whether TFF2 also regulated IL-33 production in this important cell population. Inflammatory DCs within mediastinal LNs (MLNs) were defined as CD11b+CD11c+MHC class II+ and FcεRI+ (Fig. 7 A; Hammad et al., 2010). Inflammatory DCs that coexpressed ST2 and IL-33 increased fivefold in percentage by day 3 after infection within WT mice, but this population was distinctly IL-33neg within TFF2−/− MLNs (Fig. 7, B and C). We did not detect these differences in naive mice (Fig. 7 B) or at day 1 after infection (not depicted).
Figure 7.
TFF2 is required for inflammatory DCs to express IL-33 within the lung draining LNs after N. brasiliensis infection. (A) Gating strategy for the identification of inflammatory DCs as CD11b+, CD11c+, FcεR1+, and MHC class II+ within the MLNs. (B) Plots are gated on inflammatory DCs in MLNs of naive WT and TFF2−/− mice or day 3 after infection with N. brasiliensis. Numbers indicate the percentage in each quadrant. (C) Percentage of IL-33+, TI/ST2+ inflammatory DCs from the experiment described in B. TI/ST2 (also known as IL-1RL1) is a critical subunit of the murine IL-33 receptor. Means ± SE of four mice/group are shown. Data are representative of three independent experiments (** P < 0.01).
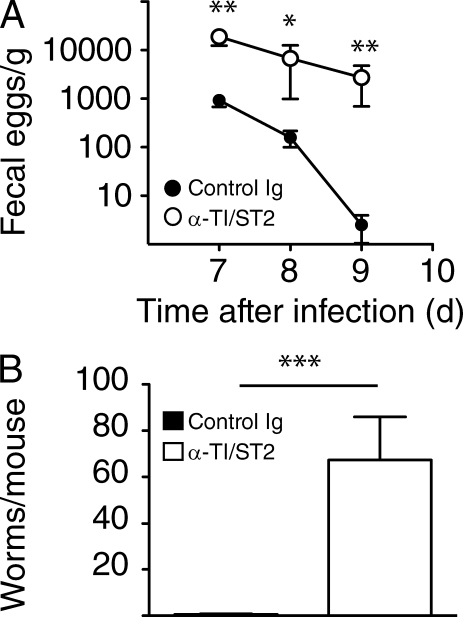
Although ST2+IL-33+ inflammatory DCs were a relatively small population within the MLNs of N. brasiliensis–infected WT mice, intact ST2 signaling in the host served a critical role for the development of host immunity. Data shown in Fig. 8 indicate that treatment of WT C57BL/6 mice with two 750-µg doses of neutralizing anti-ST2 mAb significantly increased both parasite egg production (Fig. 8 A) and the numbers of adult hookworms recovered from the intestine at day 9 after infection (Fig. 8 B). Thus, TFF2 promotes IL-33 production from inflammatory DCs during the early stages of hookworm infection, and neutralization of ST2 (IL-33 receptor) impairs the normal expulsion of N. brasiliensis adult worms from infected hosts.
Figure 8.
ST2 is necessary for host immunity against N. brasiliensis. (A) N. brasiliensis fecal egg numbers in WT C57BL/6 mice after treatment with anti-T1/ST2 mAb or isotype control on days 0 and 4. Means ± SE of six mice/group are shown. (B) N. brasiliensis intestinal worm numbers at day 9 after infection from the experiment described in A. Means ± SE of six mice/group are shown. Data are representative of two independent experiments (*, P < 0.05; **, P < 0.01; and ***, P < 0.001).
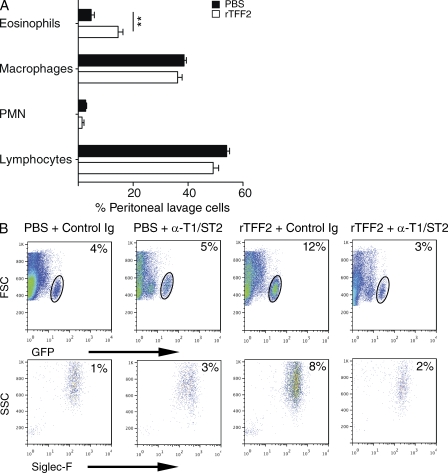
Given this novel role for TFF2 in the rapid production of IL-33 from a variety of cellular sources, we sought to determine whether the administration of rTFF2 was alone sufficient to induce a type 2 response. As eosinophils are a hallmark of type 2 inflammation and are constitutively fluorescent within IL-4 reporter mice (4Get; Voehringer et al., 2006), we inoculated naive 4Get animals i.p. with 4 µg rTFF2 over 4 d and evaluated whether these cells were recruited to the peritoneal cavity on day 5. rTFF2 administration selectively increased the percentage of eosinophils as compared with PBS treatment but did not increase the percentage of macrophages, PMNs, or lymphocytes (Fig. 9 A). rTFF2 administration did not increase the percentage of mast cells or basophils (not depicted). Importantly, ST2 was required for this effect because the increase of peritoneal eosinophils (FSCMedSScHiSiglec-F+, GFP+) was abrogated by the treatment of mice with anti-ST2 mAb during rTFF2 administration (Fig. 9 B). This is consistent with evidence that rIL-33 administration to naive mice results in the rapid and selective recruitment of eosinophils (Schmitz et al., 2005). Collectively, these data show that increased levels of TFF2 are sufficient to rapidly induce eosinophil recruitment through a mechanism that is dependent on the IL-33 receptor ST2.
Figure 9.
Administration of rTFF2 to naive mice induces eosinophilia through an IL-33–dependent mechanism. (A) Naive IL-4 fluorescent reporter mice (4Get) were administered four daily i.p. injections of 1 µg rTFF2 or PBS and analyzed on day 5, and the percentage of inflammatory leukocytes from cytospin preparations of peritoneal lavage fluid were determined by Giemsa staining. Means ± SE of four mice per group are shown (**, P < 0.01). (B) Flow cytometry dot plots showing the gating strategy used to identify GFP+Siglec-F+ cells within the peritoneal cavity after the same treatments as described in A, but combined with the administration of anti-ST2 mAb or isotype-matched control Ig on days 0, 2, and 4. The percentage of total cells within the gated population is shown in the top right corner of each plot. The bottom plots are gated on cells shown within the corresponding top plot gates. Data represent mean ± SE of four mice/group. Data are representative of two to three independent experiments.
TFF2 drives antigen-specific TH2 differentiation through IL-33
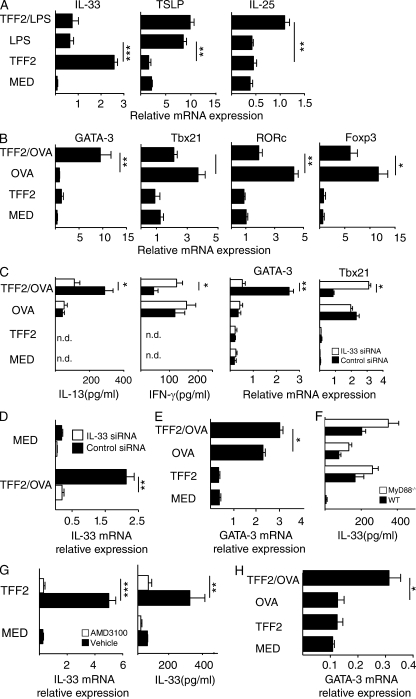
Although our data indicated that TFF2 was required for IL-33 production, it remained unclear whether TFF2 could directly stimulate IL-33 release. As macrophages are known to produce more IL-33 than DCs (Ohno et al., 2009), we generated WT BM-derived macrophages (BMDMs) and treated these cells with rTFF2 and/or bacterial LPS followed by quantitation of mRNA transcripts for the canonical TH2-promoting cytokines, IL-33, IL-25, and thymic stromal lymphopoietin (TSLP). Surprisingly, TFF2 itself was a selective stimulus for IL-33, whereas TFF2 alone did not induce expression of IL-25 or TSLP (Fig. 10 A). As expected, LPS alone induced a moderate increase of IL-33, but co-administration of TFF2 and LPS actually reduced IL-33 levels compared with TFF2 alone (Fig. 10 A). In contrast, co-administration of TFF2 and LPS stimulated a significant increase of IL-25, which suggested a possible synergistic mechanism regarding the production of this type 2–promoting cytokine (Fig. 10 A).
Figure 10.
TFF2-treated antigen-presenting cells selectively drive TH2 differentiation through an IL-33–dependent mechanism. (A) BMDMs from WT mice were evaluated for mRNA expression levels of IL33, IL25, and TSLP after exposure to media (MED), 100 ng/ml LPS, 40 ng/ml rhTFF2 (TFF2), or LPS and TFF2 for 48 h. Mean ± SE of quadruplicate wells is shown. (B) Quantification of mRNA transcripts for GATA3, TBX21, RORC, and FOXP3 in co-cultures of OTII CD4+ T cells and BMDMs that were left untreated (MED), treated with 40 ng/ml rhTFF2, pulsed with 50 µg/ml OVA, or pretreated with rTFF2 and pulsed with 50 µg/ml OVA (TFF2 + OVA). Cells were analyzed at 96 h. Data show mean ± SE of triplicate wells. (C) BMDMs were transfected with siRNA specific for IL-33 (IL-33 siRNA) or scrambled control (control) 48 h before the co-culture experiment described in B. IL-13 and IFN-γ protein levels were determined by ELISA, and mRNA levels of GATA3 and TBX21 were determined by quantitative RT-PCR. Mean ± SE of triplicate wells is shown. (D) BMDMs transfected with scrambled control or IL-33 siRNA were tested for IL-33 induction 96 h after treatment with OVA and 40 ng/ml rTFF2. Mean ± SE of triplicate wells is shown. (E) GM-CSF differentiated BMDCs from naive WT C57BL/6 mice were stimulated as in B. Error bars indicate SE. (F) IL-33 protein levels in supernatants of WT versus MyD88−/− BMDMs that were subjected to the co-culture conditions described in B. The experiment was performed two times. Data show mean ± SE of triplicate wells. (G) Il33 mRNA expression and IL-33 protein levels from WT BMDMs that were exposed to 1 µg/ml AMD3100 (CXCR4 antagonist) 24 h before exposure to stimulation with 40 ng/ml TFF2 or media for 48 h. Data show mean ± SE of triplicate wells. (H) GATA3 expression levels from co-cultures of WT naive CD4+ OTII cells and TI/ST2−/− BMDMs that were treated with 40 ng/ml rTFF2 or left untreated before pulse with OVA (endotoxin <0.2 ng/ml free) and co-cultured with OTII cells for 96 h. Data show mean ± SE from triplicate wells. Data are representative of two to four independent experiments (*, P < 0.05; **, P < 0.01; and ***, P < 0.001).
To directly test whether TFF2-induced IL-33 production alone was sufficient to drive TH2 cell differentiation from naive T cell precursors, rTFF2-exposed BMDMs were used to stimulate naive OVA-specific CD4+ T cells (OTII). T cell lineage commitment was determined by mRNA quantification for levels of the following transcription factors: TBET/TBX21 (TH1), GATA3 (TH2), RORC (TH17), and FOXP3 (Treg). Within 96 h of co-culture, rTFF2-treated, OVA-pulsed BMDMs increased GATA3 expression nearly 10-fold, whereas co-cultures containing naive OTII cells with mock-treated, OVA-pulsed BMDMs did not up-regulate GATA3 (Fig. 10 B). Interestingly, rTFF2 treatment moderately suppressed TBET, RORC, and FOXP3 expression compared with mock-treated, OVA-pulsed BMDMs (Fig. 10 B). Targeted knockdown of IL-33 in BMDMs blocked TFF2-driven GATA3 expression and IL-13 production but increased TBET expression and IFN-γ production (Fig. 10, C and D). Moreover, rTFF2-treatment of OVA-pulsed BM-derived DCs (BMDCs) also caused a significant up-regulation of GATA3 expression within the OVA-specific OTII cells (Fig. 10 E). Overall, these findings demonstrated that TFF2 functioned as a specific stimulus for IL-33 production, which, at least in this in vitro co-culture system, functioned to selectively drive antigen-specific TH2 differentiation from naive T cell precursors.
TFF2-induced IL-33 production requires CXCR4 but not ST2 or MyD88
To investigate the mechanisms required for TFF2-mediated IL-33 production, we initially focused on MyD88, the critical adaptor molecule for most Toll-like receptor and IL-1 cytokine signaling pathways (Takeuchi and Akira, 2002). Contrary to expectation, TFF2-treated BMDMs from MyD88−/− mice resulted in slightly greater levels of GATA3 than induced by WT BMDMs; however, this was not significant (Fig. 10 F). Next, we asked whether TFF2 induced IL-33 release from macrophages through mechanisms that required the putative TFF2 receptor CXCR4 (Dubeykovskaya et al., 2009). Treatment of WT BMDMs with the CXCR4 antagonist AMD3100 completely blocked TFF2-mediated IL-33 mRNA expression and protein release (Fig. 10 G). Collectively, these data indicate that TFF2 functions through CXCR4, not MyD88, for the induction of IL-33 production by BMDMs.
Lastly, to determine whether BMDMs required autocrine IL-33 signaling to promote TH2 differentiation, we generated BMDMs from ST2−/− mice. Data show that TFF2-treated, OVA-pulsed BMDMs from ST2−/− mice induced significantly more GATA3 expression within OVA-specific OTII cells as compared with nontreated ST2−/− BMDMs (Fig. 10 H). Thus, TFF2-mediated effects on macrophages did not require MyD88 or autocrine IL-33 signaling but were dependent on CXCR4, the putative TFF2 receptor.
DISCUSSION
The molecular and cellular mechanisms that initiate type 2 immunity remain topics of considerable debate and controversy. Although mechanistically unclear, most of the evidence suggests that epithelial cells make important contributions toward TH2 differentiation (Artis and Grencis, 2008; Paul and Zhu, 2010). Herein, we demonstrate that the epithelial-derived repair molecule TFF2 promotes the release of IL-33, an established regulator of type 2 inflammation. In mice, this mechanism is critical for allergic lung immunopathologies and the development of host immunity against hookworms. Moreover, we demonstrate that pediatric asthma is associated with an increase of mucosal TFF2 expression.
As type 2 cytokines have previously been shown to induce TFF2 expression in the mouse lung (Nikolaidis et al., 2003; Follettie et al., 2006), we investigated its functional role in both the HDM- and IL-13–induced models of allergic asthma. HDM-induced TH2 responses may result from the injurious effects of protease-containing allergens upon airway epithelia. Indeed, HDM antigens are a major cause of clinical asthma and TH2-driven allergic inflammation in humans (Karp, 2010). Similar to HDM antigens, rIL-13 administration in WT mice normally drives mucus hypersecretion, eosinophil recruitment, and AHR (Wills-Karp et al., 1998). TFF2−/− mice were significantly protected against most of the allergic features induced by either HDMs or IL-13. This suggests that TFF2 may function as an effector molecule of type 2 immunity during murine asthma, which may partially explain how IL-13 causes airway epithelia to promote AHR, goblet cell activation, and mucus hypersecretion (Kuperman et al., 2002). Consistent with this hypothesis, TFF2 is known to increase mucus viscosity, which is a contributing factor to airflow obstruction during asthma pathogenesis (Thim et al., 2002; Agrawal et al., 2007). In addition, we show that children experiencing acute asthma exacerbations expressed high levels of TFF2 mRNA in the nasal mucosa. Collectively, these results suggest that TFF2 release, perhaps in response to epithelial injury caused by allergens, serves an important role in the subsequent expression of type 2 cytokine–mediated immune responses in the allergic airway mucosa.
Given the central role of TFF family proteins in epithelial cell restitution after mucosal injury (Taupin and Podolsky, 2003), we examined the effects of TFF2 deficiency on hookworm-induced lung pathology. Migration of N. brasiliensis L3 through lung tissue causes extensive hemorrhage during acute infection (Marsland et al., 2008). Pulmonary repair mechanisms subsequent to the exit of L3 from the lung result in progressive structural changes that resemble chronic obstructive pulmonary disorder and emphysema, in addition to the IL-13–dependent processes that drive increased AHR (Marsland et al., 2008). Our study demonstrates that N. brasiliensis infection causes a rapid up-regulation of lung TFF2 expression (24 h), which functionally limits the extent of tissue injury caused by migratory L3, as TFF2−/− mice show excessive hemorrhage and accelerated development of emphysematous changes. This is consistent with TFF2’s known role in accelerating tissue repair in several other systems (Farrell et al., 2002; Poulsen et al., 2005).
Although TFF2 may induce tissue repair directly, our data show that TFF2 was also a prerequisite for the initial production of type 2 cytokines in the lung, as TFF2−/− mice had impaired IL-4 and IL-13 responses at day 3 after inoculation compared with WT mice. This initial TH2 cell expansion at day 3 after infection was STAT-6 independent (unpublished data), as previously demonstrated by others (Jankovic et al., 2000; van Panhuys et al., 2008). Although TFF2 played an essential role in the early phase of type 2 immunity against hookworms, during later stages of the response, the TFF2 deficiency did not prevent the host from eventually producing sufficient levels of IL-4 to drive RELM-β–dependent worm expulsion (Herbert et al., 2009). Furthermore, an early administration of rIL-4 to N. brasiliensis–infected TFF2−/− mice rapidly increased RELM-β levels and facilitated more rapid worm clearance. This demonstrated that TFF2−/− mice had impaired immunity to N. brasiliensis infection because of an early defect in type 2 cytokines and that TFF2 functioned in a redundant manner with other TH2 effector molecules during the later stages of infection. This is not unexpected, as there are multiple redundant mechanisms that promote TH2 responses (Neill et al., 2010; Paul and Zhu, 2010). Consistent with this hypothesis, repeated immunization of TFF2−/− mice with chicken egg OVA over 3–4 wk resulted in only a moderate reduction of eosinophilic inflammation (Nikolaidis et al., 2006). Thus, TFF2 may primarily function to rapidly respond to injurious agents and provide early instruction toward TH2 development.
The epithelial-derived cytokines IL-25, IL-33, and TSLP are demonstrated regulators of type 2 immune responses (Fallon et al., 2006; Zaph et al., 2007; Humphreys et al., 2008). Thus, we postulated that TFF2 might induce type 2 immunity through inducing the production of one or more of these molecules. Surprisingly, TFF2 promoted IL-33 release from lung epithelia and alveolar macrophages within 24 h after infection. Even more striking was that TFF2 was required for IL-33 production within inflammatory DCs recruited to the lung draining LNs by day 3 after infection. Given the recent demonstration that inflammatory DCs are central initiators of type 2 immunity during allergic responses and worm infection (Hammad et al., 2010; Phythian-Adams et al., 2010), our data provide one potential mechanism underlying this capability. Our co-culture experiments demonstrated that rTFF2 was sufficient to confer TH2-promoting abilities upon BMDMs and BMDCs. However, it remains possible that TFF2 might also induce TSLP and/or IL-25 under certain conditions, something which is supported by our demonstration that BMDMs produced IL-25 when exposed to a combination of LPS and TFF2. Collectively, our demonstration that TFF2 regulates IL-33 production from both hematopoietic and nonhematopoietic cell lineages suggests that we have uncovered an important mechanism of mucosal immunoregulation.
IL-33 is a well-established regulator of allergic lung inflammation, anaphylactic shock, and colitis (Kurowska-Stolarska et al., 2008; Kearley et al., 2009; Pushparaj et al., 2009; Oboki et al., 2010; Rani et al., 2011). To date however, the biologically relevant signals for IL-33 release in the context of type 2 pathologies have been unclear. Our study provides the following insights: (a) TFF2 regulates IL-33 production, (b) hookworm infection results in IL-33 release into the lung tissue, and (c) pulmonary epithelia, alveolar macrophages, and inflammatory DCs are important sources of IL-33. Chang et al. (2011) recently demonstrated that influenza-infected rodents have IL-33+ alveolar macrophages and develop IL-13–driven AHR. These data are remarkably consistent with the central conclusions of our study, which are that infection-induced lung injury causes TFF2 release that promotes IL-33 from innate sources for the rapid development of type 2 immunity.
IL-33 has been shown to regulate the immunobiology of DCs (Rank et al., 2009), basophils (Pecaric-Petkovic et al., 2009), mast cells (Hsu et al., 2010), and T lymphocytes (Guo et al., 2009) and promote the development of alternatively activated macrophages (Kurowska-Stolarska et al., 2009; Zaiss et al., 2011). We found that ST2 expression on macrophages was not essential in order for TFF2 to instruct these cells to drive antigen-specific GATA3 expression within the CD4+ T cells, which implies that ST2 expression on T cells is sufficient for TH2 differentiation. Indeed, ST2 was necessary for host protection against N. brasiliensis. This finding is consistent with evidence that mice deficient in IL-1RL11 (subunit of IL-33 receptor) show increased susceptibility to N. brasiliensis infection and that rIL-33 administration promotes the expulsion of the whipworm T. muris (Humphreys et al., 2008; Neill et al., 2010).
Although our data also support the notion that IL-33/ST2 signaling promotes primary TH2 development (Townsend et al., 2000), there is controversy regarding whether ST2 signaling promotes TH2 responses (Hoshino et al., 1999). Thus, we cannot rule out the possibility that IL-33 only functions to expand naive TH2 precursors (Guo et al., 2009). However, our data are consistent with reports that ST2 deletion or blockade impairs type 2 responses in vivo (Löhning et al., 1998; Coyle et al., 1999; Townsend et al., 2000). Thus, we propose that a TFF2/IL-33 axis exists, which serves an important function in the development of TH2 responses and host immunity against hookworm infection.
Several lines of evidence suggest that TFF2 preferentially drives type 2 inflammation and antigen-specific TH2 differentiation through its ability to induce IL-33 production. First, rTFF2 could rapidly induce the selective recruitment of eosinophils in 4Get mice through a mechanism that was blocked by inhibition of ST2, the critical subunit of the IL-33 receptor. Second, TFF2 treatment of BMDMs or BMDCs co-cultured with OVA-specific CD4+ T cells (OTII) resulted in the specific induction of GATA-3, the TH2 lineage–specific transcription factor (Ouyang et al., 2000; Seki et al., 2004), as well as IL-13 production in culture supernatants. These cultures also contained IL-5 but no IL-10, IFN-γ, or IL-17A (unpublished data). Lastly, IL-33 production from BMDMs was necessary to promote T cell differentiation toward a TH2 phenotype and for the concomitant suppression of TH1 development. IL-33 most likely works directly on the T cells and not through autocrine effects on BMDMs, as ST2−/− macrophages also induced GATA3 expression after TFF2 treatment.
TFF2-mediated IL-33 production required the CXCR4 receptor, which is a chemokine receptor used by T cell tropic strains of the human immunodeficiency virus (Grivel and Margolis, 1999). The natural ligand for CXCR4 is SDF-1 (stromal cell–derived factor 1; Allen et al., 2004). Consistent with evidence that the TFF2 receptor is CXCR4, we demonstrate that AMD3100 (a specific antagonist of CXCR4) blocks TFF2-induced IL-33 production. This is in concordance with evidence that the CXCR4/SDF-1 axis is required for TH2-mediated allergic airway disease (Gonzalo et al., 2000) and that AMD3100 abolishes cockroach-induced murine asthma (Lukacs et al., 2002). Moreover, we have preliminary evidence that AMD3100 treatment also exacerbates N. brasiliensis–induced lung injury (unpublished data).
Our model predicts that TFF2 initiates a rapid, coordinated type 2 immune response in the lung after allergen exposure or worm infection–induced mucosal injury. We propose the following: (a) within hours of insult, TFF2 secretion drives epithelial cell restitution, which prevents excessive hemorrhage and also starts the tissue remodeling process; (b) within 24 h, TFF2 promotes IL-33 release from lung epithelia and alveolar macrophages, but although IL-33 production in epithelia is rapidly lost, IL-33 production in myeloid cells is sustained for several days; (c) within 3 d, TFF2 promotes IL-33 expression within ST2+ inflammatory DCs that migrate to draining LNs; (d) this results in the initial clonal burst of antigen-specific TH2 cells within the LN; and (e) once sufficient amounts of IL-4 and IL-13 are produced, these cytokines drive a myriad of effector functions within epithelia and macrophages (including TFF2 production) that promote worm expulsion and asthma pathogenesis (Kuperman et al., 2002; Herbert et al., 2009).
In the context of parasitic infections, the induction of type 2 immunity and tissue remodeling protects the host against organ damage and pathogen persistence. However, in the context of asthma, excess production of type 2 cytokines and tissue repair molecules is pathogenic. It is possible that the TFF2/IL-33 axis may have evolved under selective pressure from parasitic helminths for the initiation of IL-4– and IL-13–dependent host defense mechanisms, while simultaneously mediating the repair of damaged mucosa. This is consistent with the view that allergies and asthma represent maladaptive TH2 responses intended for worm parasites and suggests that TFF2 may be a possible target for therapeutic intervention in a broad array of allergic and parasitic human diseases.
MATERIALS AND METHODS
Mice, parasites, and asthma.
All experiments used male WT C57BL/6 or TFF2−/− mice (C57BL/6 × 129) that have been backcrossed to the C57BL/6 background for more than six generations (Farrell et al., 2002). Although pure WT C57BL/6 B6 mice were used as controls throughout the paper, all infection data were additionally confirmed with +/+ and +/− littermate controls. 4Get mice on a BALB/c background have been described previously (Mohrs et al., 2001). Worm burdens were assessed by opening mouse intestines longitudinally and incubating them in PBS at 37°C for 3 h in a modified Baermann apparatus in which tissues were placed in a sieve atop a 250-ml beaker. Parasites that collected at the bottom were counted. For fecal egg counts, feces were collected, weighed, and incubated in saturated NaCl solution, and eggs were counted using McMaster slides (Herbert et al., 2009). Allergic airway responses induced by HDMs or 5 µg rmIL-13 have been described previously (Wills-Karp et al., 1998) The Institutional Animal Care and Use Committee at the Cincinnati Children’s Hospital Medical Center (CCHMC) approved all protocols and procedures.
Subjects.
Nasal epithelial samples were obtained from healthy and asthmatic children at CCMHC and processed for RNA extraction and cDNA synthesis as previously described (Guajardo et al., 2005). Asthmatic children and their parents attending the hospital clinics and emergency department in the CCHMC were invited to participate in the study. Participants were included in exacerbation of asthma (asthma-E group, n = 23) or healthy nonatopic children (control group, n = 9), as previously described (Guajardo et al., 2005).
Assessment of airway responsiveness and BAL cellularity.
To evaluate airway responses, mice were anaesthetized, intubated, and respirated at a rate of 120 breaths per minute with a constant tidal volume (0.2 ml) and paralyzed with 25 mg/kg decamethonium bromide 24 h after the final HDM or IL-13 challenge. 50 µg/kg acetylcholine was injected into the inferior vena cava, and dynamic airway pressure (cm H2O × sec) was followed for 5 min. To collect BAL fluid, lungs were lavaged three times with a 1.0-ml aliquot of cold Hanks’ balanced salt solution (Invitrogen). Recovered lavage fluid (70–80%) was centrifuged (300 g for 10 min), and the cell pellet was resuspended in 1.0 ml of 10% FBS in PBS. Total cells were counted with a hemocytometer. Slides were prepared by cytocentrifugation (Cytospin 3; Shandon Instruments) and stained with Diff-Quik (Dade Behring). BAL cell differential counts were determined using morphological criteria under a light microscope (BX40; Olympus) with evaluation of ≥500 cells/slide.
Lung histopathology.
To assess airway inflammation and mucus cell content in the airway wall, lungs were excised and fixed in 10% formalin, washed in methanol, dehydrated and embedded in paraffin, and cut into 5-µm sections. Sections were mounted on slides and stained with hematoxylin and eosin and periodic acid Schiff (PAS). The left lung was removed and fixed in 10% neutral buffered formalin. Lungs were bisected and oriented cut side down in a paraffin block such that sections would reveal cross sections of consistent airways for comparison. Two, 5-µm sections, 30 µm apart, were PAS stained and examined for mucin production. Examination included assessment of the percentage of airways with PAS-positive cells (number of airways containing any PAS cells/number of total airways) as well as total number of goblet cells per section.
Microscopy/histology.
5-mm formalin-fixed, paraffin-embedded sections of lung or jejunum were prepared by the CCHMC Morphology core. A microscope (Eclipse E600; Nikon) fitted with a 40× objective oil-immersion lens (Plan Apochromat; Nikon) was used for image acquisition, and photos were captured with a SPOT Diagnostics RT slider digital color camera using a SPOT Diagnostics imaging system.
ELISA and real-time PCR.
RNA was DNase I treated and cDNA prepared using SuperScript II reverse transcription (Invitrogen). Real-time PCR was performed on a Gene Amp 7500 instrument (PE Biosystems) with the Syber Green detection reagent. Cycle threshold (CT) values for genes evaluated were determined and expressed using the 1/ΔΔct method (Table S1), as described previously (Herbert et al., 2010). Mouse cytokine ELISA kits specific for IL-13, IFN-γ, and IL-33 were obtained from eBioscience.
Isolation of lung tissue cells and BAL collection.
Lungs were perfused with 1× PBS and minced with scissors followed by digestion in serum-free RPMI containing 0.5 mg/ml Liberase CI (Roche) and 0.5 mg/ml DNase I (Sigma-Aldrich) RPMI for 30 min at 37°C with shaking. Samples were further disassociated by repeated passage through a 10-ml syringe fitted with an 18-g needle and finally passed through a 70-µm cell strainer to obtain a single cell suspension. For cytokine measurements, BAL fluid was collected using established protocols (Lewkowich et al., 2005) followed by concentration with Amicon Ultra centrifugal filter units with 3K cut-off (Millipore). Magnetic bead isolation of EpCAM- and CD11c-positive cells was performed according to the manufacturer’s protocol (Miltenyi Biotec)
Flow cytometric analyses.
Single cell suspensions of lung or MLN tissue were stained with one or more of the following fluorescently labeled mAbs: ST2L/IL-1R4 (clone 245707) and anti–IL-33 (R&D Systems), CD11c (clone N418), CD11b (clone M1/70), anti-CD326/EpCAM (clone G8.8), I-Ab (clone AF6-120.1), Ly6G/C (clone RB6-8C5), FcεRI (clone MAR-1), CD103 (clone 2E7), CD45 (clone 30-F11), CD317 (clone 120g8), and isotype control (MOPC-173; eBioscience). Before intracellular cytokine staining, cells were either stimulated with PMA/Ionomycin/Golgi-stop (BD) or 1 µg/ml anti-CD3/anti-CD28 mAb for 16 h, with Golgi-plug added the last 4 h before staining. Acquisition was performed with an LSRII flow cytometer (BD) or FACSCalibur (BD), and data were analyzed with FlowJo software (version 8.8; Tree Star). Rat anti–mouse ST2 (clone M955) and control IgG antibodies were provided by Amgen.
Generation of macrophages, DCs, and basophils.
BMDMs were grown in CMG media from an M-CSF transfected cell line, as described previously (Herbert et al., 2010). BMDCs were grown in media containing 20 ng/ml GM-CSF for 9 d. BM-derived basophils were generated from total BM cultured with 10 ng/ml IL-3 for 6 d.
OTII differentiation assay.
CD4+ cells were isolated from naive OVA-specific TCR transgenic mice (OTII) as previously described (Herbert et al., 2010). BMDMs were either left untreated or exposed to recombinant human TFF2 (endotoxin values <0.1 ng/ml [PeproTech]) for 16 h and then pulsed with 50 µg/well endotoxin-free chicken egg OVA for 8 h, washed several times, and co-cultured with purified naive OTII CD4+ cells at a ratio of 10:1 (CD4+/MΦ) for 72–96 h. IL-33 and scrambled control small interfering RNA (siRNA) BMDMs were electroporated with scrambled control or IL-33 siRNA (Thermo Fisher Scientific) using the Amaxa mouse macrophage Nucleofector kit according to manufacturer’s instruction (Lonza).
In vivo cytokine capture assays.
Relative amounts of in vivo IL-4 secretion were determined by the in vivo cytokine capture assay (Finkelman and Morris, 1999). Injected biotin-labeled anticytokine mAbs in this assay form complexes with the secreted cytokines they specifically bind that have a much longer in vivo half-life than free cytokines. Consequently, the complexes accumulate in vivo and can be measured by ELISA, using wells coated with mAbs that bind to an epitope on the cytokine that is not blocked by the injected mAb. Bound biotin-mAb/cytokine complexes are detected with horseradish peroxidase–streptavidin, followed by a luminogenic substrate. To measure IL-4 and IFN-γ secretion, mice were injected i.v. with 10 µg biotin-BVD4-1D11 (anti–IL-4 mAb), and serum was collected 6 h later and analyzed with microtiter plate wells coated with BVD6-24G2.3 (anti–IL-4). These antibodies were purified from ascites by ion-exchange chromatography as previously described (Herbert et al., 2008).
Long-acting IL-4 (IL-4C).
IL-4/anti–IL-4 mAb complexes (IL-4C) were prepared by mixing rmIL-4 with the rat IgG1 anti–IL-4 mAb, 11B11, at a 2:1 molar (1:5 weight) ratio. Mice were injected i.p. with IL-4C containing 5 µg IL-4 and 25 µg anti–mouse IL-4 (11B11). IL-4C slowly dissociated, releasing biologically active IL-4 for 3–5 d. Because IL-4C contain only one molecule of IgG mAb and 11B11 blocks IL-4R binding of IL-4, IL-4C do not activate complement, interact more strongly with Fc receptors than monomeric IgG of the same rat IgG2b isotype, or bind to IL-4R. IL-4C do not promote worm expulsion or cell differentiation in IL-4Rα–deficient mice (Herbert et al., 2009)
Statistical analysis.
Statistical significance was assessed by either the two-tailed Student’s t test (two groups) or analysis of variance for multiple groups with a post-hoc Tukey test to determine significance, all performed using Prism 4.0 software (GraphPad; *, P < 0.05; **, P < 0.01; and ***, P < 0.001).
Online supplemental material.
Fig. S1 shows the gating strategy for the identification of CD4+TCR-β+ T lymphocytes within the MLNs. Table S1 lists the primer sequences used for this study. Online supplemental material is available at http://www.jem.org/cgi/content/full/jem.20110079/DC1.
Acknowledgments
We thank Christopher Karp, Marat Khodoun, and Stephane Lajoie for critical discussions.
F.D. Finkelman is supported by a merit award from the US Department of Veterans Affairs, T.C. Wang is supported by National Institutes of Health (NIH) grant 5R01DK060758, G.K. Hershey is supported by grant U19AI70235, P.J. Bryce is supported by NIH grant R01AI076456, M. Wills-Karp is supported by NIH grants RO1 HL67736, RO1 AI1183315, U19A170235, and P50ES015903, IPL is supported by a Parker B. Francis Award, and D.R. Herbert is supported by grants R01AI095289 and RO1GM083204.
The authors have no conflicting financial interests.
Footnotes
Abbreviations used:
- AHR
- airway hyperreactivity
- BAL
- bronchoalveolar lavage
- BMDC
- BM-derived DC
- BMDM
- BM-derived macrophage
- EpCAM
- epithelial cell adhesion molecule
- GI
- gastrointestinal
- HDM
- house dust mite
- MLN
- mediastinal LN
- mRNA
- messenger RNA
- PAS
- periodic acid Schiff
- siRNA
- small interfering RNA
- TSLP
- thymic stromal lymphopoietin
References
- Agrawal A., Mabalirajan U., Ram A., Ghosh B. 2007. Novel approaches for inhibition of mucus hypersecretion in asthma. Recent Pat. Inflamm. Allergy Drug Discov. 1:188–192 10.2174/187221307782418865 [DOI] [PubMed] [Google Scholar]
- Ali S., Huber M., Kollewe C., Bischoff S.C., Falk W., Martin M.U. 2007. IL-1 receptor accessory protein is essential for IL-33-induced activation of T lymphocytes and mast cells. Proc. Natl. Acad. Sci. USA. 104:18660–18665 10.1073/pnas.0705939104 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Allen C.D., Ansel K.M., Low C., Lesley R., Tamamura H., Fujii N., Cyster J.G. 2004. Germinal center dark and light zone organization is mediated by CXCR4 and CXCR5. Nat. Immunol. 5:943–952 10.1038/ni1100 [DOI] [PubMed] [Google Scholar]
- Artis D., Grencis R.K. 2008. The intestinal epithelium: sensors to effectors in nematode infection. Mucosal Immunol. 1:252–264 10.1038/mi.2008.21 [DOI] [PubMed] [Google Scholar]
- Baena-Cagnani C.E. 2001. The global burden of asthma and allergic diseases: the challenge for the new century. Curr. Allergy Asthma Rep. 1:297–298 10.1007/s11882-001-0037-z [DOI] [PubMed] [Google Scholar]
- Barron L., Wynn T.A. 2011. Fibrosis is regulated by Th2 and Th17 responses and by dynamic interactions between fibroblasts and macrophages. Am. J. Physiol. Gastrointest. Liver Physiol. 300:G723–G728 10.1152/ajpgi.00414.2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Braman S.S. 2006. The global burden of asthma. Chest. 130:4S–12S 10.1378/chest.130.1_suppl.4S [DOI] [PubMed] [Google Scholar]
- Brancato S.K., Albina J.E. 2011. Wound macrophages as key regulators of repair: origin, phenotype, and function. Am. J. Pathol. 178:19–25 10.1016/j.ajpath.2010.08.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brooker S. 2010. Estimating the global distribution and disease burden of intestinal nematode infections: adding up the numbers—a review. Int. J. Parasitol. 40:1137–1144 10.1016/j.ijpara.2010.04.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brooker S., Hotez P.J., Bundy D.A. 2010. The global atlas of helminth infection: mapping the way forward in neglected tropical disease control. PLoS Negl. Trop. Dis. 4:e779 10.1371/journal.pntd.0000779 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carriere V., Roussel L., Ortega N., Lacorre D.A., Americh L., Aguilar L., Bouche G., Girard J.P. 2007. IL-33, the IL-1-like cytokine ligand for ST2 receptor, is a chromatin-associated nuclear factor in vivo. Proc. Natl. Acad. Sci. USA. 104:282–287 10.1073/pnas.0606854104 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chang Y.J., Kim H.Y., Albacker L.A., Baumgarth N., McKenzie A.N., Smith D.E., Dekruyff R.H., Umetsu D.T. 2011. Innate lymphoid cells mediate influenza-induced airway hyper-reactivity independently of adaptive immunity. Nat. Immunol. 12:631–638 10.1038/ni.2045 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coyle A.J., Lloyd C., Tian J., Nguyen T., Erikkson C., Wang L., Ottoson P., Persson P., Delaney T., Lehar S., et al. 1999. Crucial role of the interleukin 1 receptor family member T1/ST2 in T helper cell type 2–mediated lung mucosal immune responses. J. Exp. Med. 190:895–902 10.1084/jem.190.7.895 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dubeykovskaya Z., Dubeykovskiy A., Solal-Cohen J., Wang T.C. 2009. Secreted trefoil factor 2 activates the CXCR4 receptor in epithelial and lymphocytic cancer cell lines. J. Biol. Chem. 284:3650–3662 10.1074/jbc.M804935200 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fallon P.G., Ballantyne S.J., Mangan N.E., Barlow J.L., Dasvarma A., Hewett D.R., McIlgorm A., Jolin H.E., McKenzie A.N. 2006. Identification of an interleukin (IL)-25–dependent cell population that provides IL-4, IL-5, and IL-13 at the onset of helminth expulsion. J. Exp. Med. 203:1105–1116 10.1084/jem.20051615 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Farrell J.J., Taupin D., Koh T.J., Chen D., Zhao C.M., Podolsky D.K., Wang T.C. 2002. TFF2/SP-deficient mice show decreased gastric proliferation, increased acid secretion, and increased susceptibility to NSAID injury. J. Clin. Invest. 109:193–204 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Finkelman F.D., Morris S.C. 1999. Development of an assay to measure in vivo cytokine production in the mouse. Int. Immunol. 11:1811–1818 10.1093/intimm/11.11.1811 [DOI] [PubMed] [Google Scholar]
- Finkelman F.D., Madden K.B., Morris S.C., Holmes J.M., Boiani N., Katona I.M., Maliszewski C.R. 1993. Anti-cytokine antibodies as carrier proteins. Prolongation of in vivo effects of exogenous cytokines by injection of cytokine-anti-cytokine antibody complexes. J. Immunol. 151:1235–1244 [PubMed] [Google Scholar]
- Finkelman F.D., Shea-Donohue T., Morris S.C., Gildea L., Strait R., Madden K.B., Schopf L., Urban J.F., Jr 2004. Interleukin-4- and interleukin-13-mediated host protection against intestinal nematode parasites. Immunol. Rev. 201:139–155 10.1111/j.0105-2896.2004.00192.x [DOI] [PubMed] [Google Scholar]
- Follettie M.T., Ellis D.K., Donaldson D.D., Hill A.A., Diesl V., DeClercq C., Sypek J.P., Dorner A.J., Wills-Karp M. 2006. Gene expression analysis in a murine model of allergic asthma reveals overlapping disease and therapy dependent pathways in the lung. Pharmacogenomics J. 6:141–152 10.1038/sj.tpj.6500357 [DOI] [PubMed] [Google Scholar]
- Fox J.G., Rogers A.B., Whary M.T., Ge Z., Ohtani M., Jones E.K., Wang T.C. 2007. Accelerated progression of gastritis to dysplasia in the pyloric antrum of TFF2−/− C57BL6 x Sv129 Helicobacter pylori-infected mice. Am. J. Pathol. 171:1520–1528 10.2353/ajpath.2007.070249 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gonzalo J.A., Lloyd C.M., Peled A., Delaney T., Coyle A.J., Gutierrez-Ramos J.C. 2000. Critical involvement of the chemotactic axis CXCR4/stromal cell-derived factor-1 alpha in the inflammatory component of allergic airway disease. J. Immunol. 165:499–508 [DOI] [PubMed] [Google Scholar]
- Grivel J.C., Margolis L.B. 1999. CCR5- and CXCR4-tropic HIV-1 are equally cytopathic for their T-cell targets in human lymphoid tissue. Nat. Med. 5:344–346 10.1038/6565 [DOI] [PubMed] [Google Scholar]
- Guajardo J.R., Schleifer K.W., Daines M.O., Ruddy R.M., Aronow B.J., Wills-Karp M., Hershey G.K. 2005. Altered gene expression profiles in nasal respiratory epithelium reflect stable versus acute childhood asthma. J. Allergy Clin. Immunol. 115:243–251 10.1016/j.jaci.2004.10.032 [DOI] [PubMed] [Google Scholar]
- Guo L., Wei G., Zhu J., Liao W., Leonard W.J., Zhao K., Paul W. 2009. IL-1 family members and STAT activators induce cytokine production by Th2, Th17, and Th1 cells. Proc. Natl. Acad. Sci. USA. 106:13463–13468 10.1073/pnas.0906988106 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hammad H., Plantinga M., Deswarte K., Pouliot P., Willart M.A., Kool M., Muskens F., Lambrecht B.N. 2010. Inflammatory dendritic cells—not basophils—are necessary and sufficient for induction of Th2 immunity to inhaled house dust mite allergen. J. Exp. Med. 207:2097–2111 10.1084/jem.20101563 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Herbert D.R., Orekov T., Perkins C., Finkelman F.D. 2008. IL-10 and TGF-β redundantly protect against severe liver injury and mortality during acute schistosomiasis. J. Immunol. 181:7214–7220 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Herbert D.R., Yang J.Q., Hogan S.P., Groschwitz K., Khodoun M., Munitz A., Orekov T., Perkins C., Wang Q., Brombacher F., et al. 2009. Intestinal epithelial cell secretion of RELM-β protects against gastrointestinal worm infection. J. Exp. Med. 206:2947–2957 10.1084/jem.20091268 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Herbert D.R., Orekov T., Roloson A., Ilies M., Perkins C., O’Brien W., Cederbaum S., Christianson D.W., Zimmermann N., Rothenberg M.E., Finkelman F.D. 2010. Arginase I suppresses IL-12/IL-23p40-driven intestinal inflammation during acute schistosomiasis. J. Immunol. 184:6438–6446 10.4049/jimmunol.0902009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoshino K., Kashiwamura S., Kuribayashi K., Kodama T., Tsujimura T., Nakanishi K., Matsuyama T., Takeda K., Akira S. 1999. The absence of interleukin 1 receptor-related T1/ST2 does not affect T helper cell type 2 development and its effector function. J. Exp. Med. 190:1541–1548 10.1084/jem.190.10.1541 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hsu C.L., Neilsen C.V., Bryce P.J. 2010. IL-33 is produced by mast cells and regulates IgE-dependent inflammation. PLoS ONE. 5:e11944 10.1371/journal.pone.0011944 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Humphreys N.E., Xu D., Hepworth M.R., Liew F.Y., Grencis R.K. 2008. IL-33, a potent inducer of adaptive immunity to intestinal nematodes. J. Immunol. 180:2443–2449 [DOI] [PubMed] [Google Scholar]
- Ito T., Wang Y.H., Duramad O., Hori T., Delespesse G.J., Watanabe N., Qin F.X., Yao Z., Cao W., Liu Y.J. 2005. TSLP-activated dendritic cells induce an inflammatory T helper type 2 cell response through OX40 ligand. J. Exp. Med. 202:1213–1223 10.1084/jem.20051135 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jankovic D., Kullberg M.C., Noben-Trauth N., Caspar P., Paul W.E., Sher A. 2000. Single cell analysis reveals that IL-4 receptor/Stat6 signaling is not required for the in vivo or in vitro development of CD4+ lymphocytes with a Th2 cytokine profile. J. Immunol. 164:3047–3055 [DOI] [PubMed] [Google Scholar]
- Karp C.L. 2010. Guilt by intimate association: what makes an allergen an allergen? J. Allergy Clin. Immunol. 125:955–960 10.1016/j.jaci.2010.03.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kearley J., Buckland K.F., Mathie S.A., Lloyd C.M. 2009. Resolution of allergic inflammation and airway hyperreactivity is dependent upon disruption of the T1/ST2-IL-33 pathway. Am. J. Respir. Crit. Care Med. 179:772–781 10.1164/rccm.200805-666OC [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kuperman D.A., Huang X., Koth L.L., Chang G.H., Dolganov G.M., Zhu Z., Elias J.A., Sheppard D., Erle D.J. 2002. Direct effects of interleukin-13 on epithelial cells cause airway hyperreactivity and mucus overproduction in asthma. Nat. Med. 8:885–889 [DOI] [PubMed] [Google Scholar]
- Kurowska-Stolarska M., Kewin P., Murphy G., Russo R.C., Stolarski B., Garcia C.C., Komai-Koma M., Pitman N., Li Y., Niedbala W., et al. 2008. IL-33 induces antigen-specific IL-5+ T cells and promotes allergic-induced airway inflammation independent of IL-4. J. Immunol. 181:4780–4790 (published erratum appears in J. Immunol. 2008. 181:8170) [DOI] [PubMed] [Google Scholar]
- Kurowska-Stolarska M., Stolarski B., Kewin P., Murphy G., Corrigan C.J., Ying S., Pitman N., Mirchandani A., Rana B., van Rooijen N., et al. 2009. IL-33 amplifies the polarization of alternatively activated macrophages that contribute to airway inflammation. J. Immunol. 183:6469–6477 10.4049/jimmunol.0901575 [DOI] [PubMed] [Google Scholar]
- Kurt-Jones E.A., Cao L., Sandor F., Rogers A.B., Whary M.T., Nambiar P.R., Cerny A., Bowen G., Yan J., Takaishi S., et al. 2007. Trefoil family factor 2 is expressed in murine gastric and immune cells and controls both gastrointestinal inflammation and systemic immune responses. Infect. Immun. 75:471–480 10.1128/IAI.02039-05 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lambrecht B.N., Hammad H. 2009. Biology of lung dendritic cells at the origin of asthma. Immunity. 31:412–424 10.1016/j.immuni.2009.08.008 [DOI] [PubMed] [Google Scholar]
- Lewkowich I.P., Herman N.S., Schleifer K.W., Dance M.P., Chen B.L., Dienger K.M., Sproles A.A., Shah J.S., Köhl J., Belkaid Y., Wills-Karp M. 2005. CD4+CD25+ T cells protect against experimentally induced asthma and alter pulmonary dendritic cell phenotype and function. J. Exp. Med. 202:1549–1561 10.1084/jem.20051506 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Löhning M., Stroehmann A., Coyle A.J., Grogan J.L., Lin S., Gutierrez-Ramos J.C., Levinson D., Radbruch A., Kamradt T. 1998. T1/ST2 is preferentially expressed on murine Th2 cells, independent of interleukin 4, interleukin 5, and interleukin 10, and important for Th2 effector function. Proc. Natl. Acad. Sci. USA. 95:6930–6935 10.1073/pnas.95.12.6930 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lukacs N.W., Berlin A., Schols D., Skerlj R.T., Bridger G.J. 2002. AMD3100, a CxCR4 antagonist, attenuates allergic lung inflammation and airway hyperreactivity. Am. J. Pathol. 160:1353–1360 10.1016/S0002-9440(10)62562-X [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marsland B.J., Kurrer M., Reissmann R., Harris N.L., Kopf M. 2008. Nippostrongylus brasiliensis infection leads to the development of emphysema associated with the induction of alternatively activated macrophages. Eur. J. Immunol. 38:479–488 10.1002/eji.200737827 [DOI] [PubMed] [Google Scholar]
- Meyer T.S., Fedde M.R., Gaughan E.M., Langsetmo I., Erickson H.H. 1998. Quantification of exercise-induced pulmonary haemorrhage with bronchoalveolar lavage. Equine Vet. J. 30:284–288 10.1111/j.2042-3306.1998.tb04098.x [DOI] [PubMed] [Google Scholar]
- Mohrs M., Shinkai K., Mohrs K., Locksley R.M. 2001. Analysis of type 2 immunity in vivo with a bicistronic IL-4 reporter. Immunity. 15:303–311 10.1016/S1074-7613(01)00186-8 [DOI] [PubMed] [Google Scholar]
- Nair M.G., Guild K.J., Artis D. 2006. Novel effector molecules in type 2 inflammation: lessons drawn from helminth infection and allergy. J. Immunol. 177:1393–1399 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Neill D.R., Wong S.H., Bellosi A., Flynn R.J., Daly M., Langford T.K., Bucks C., Kane C.M., Fallon P.G., Pannell R., et al. 2010. Nuocytes represent a new innate effector leukocyte that mediates type-2 immunity. Nature. 464:1367–1370 10.1038/nature08900 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nikolaidis N.M., Zimmermann N., King N.E., Mishra A., Pope S.M., Finkelman F.D., Rothenberg M.E. 2003. Trefoil factor-2 is an allergen-induced gene regulated by Th2 cytokines and STAT6 in the lung. Am. J. Respir. Cell Mol. Biol. 29:458–464 10.1165/rcmb.2002-0309OC [DOI] [PubMed] [Google Scholar]
- Nikolaidis N.M., Wang T.C., Hogan S.P., Rothenberg M.E. 2006. Allergen induced TFF2 is expressed by mucus-producing airway epithelial cells but is not a major regulator of inflammatory responses in the murine lung. Exp. Lung Res. 32:483–497 10.1080/01902140601059547 [DOI] [PubMed] [Google Scholar]
- Oboki K., Ohno T., Kajiwara N., Arae K., Morita H., Ishii A., Nambu A., Abe T., Kiyonari H., Matsumoto K., et al. 2010. IL-33 is a crucial amplifier of innate rather than acquired immunity. Proc. Natl. Acad. Sci. USA. 107:18581–18586 10.1073/pnas.1003059107 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ohno T., Oboki K., Kajiwara N., Morii E., Aozasa K., Flavell R.A., Okumura K., Saito H., Nakae S. 2009. Caspase-1, caspase-8, and calpain are dispensable for IL-33 release by macrophages. J. Immunol. 183:7890–7897 10.4049/jimmunol.0802449 [DOI] [PubMed] [Google Scholar]
- Ouyang W., Löhning M., Gao Z., Assenmacher M., Ranganath S., Radbruch A., Murphy K.M. 2000. Stat6-independent GATA-3 autoactivation directs IL-4-independent Th2 development and commitment. Immunity. 12:27–37 10.1016/S1074-7613(00)80156-9 [DOI] [PubMed] [Google Scholar]
- Paul W.E., Zhu J. 2010. How are TH2-type immune responses initiated and amplified? Nat. Rev. Immunol. 10:225–235 10.1038/nri2735 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Paulsen F.P., Woon C.W., Varoga D., Jansen A., Garreis F., Jäger K., Amm M., Podolsky D.K., Steven P., Barker N.P., Sel S. 2008. Intestinal trefoil factor/TFF3 promotes re-epithelialization of corneal wounds. J. Biol. Chem. 283:13418–13427 10.1074/jbc.M800177200 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pecaric-Petkovic T., Didichenko S.A., Kaempfer S., Spiegl N., Dahinden C.A. 2009. Human basophils and eosinophils are the direct target leukocytes of the novel IL-1 family member IL-33. Blood. 113:1526–1534 10.1182/blood-2008-05-157818 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Phythian-Adams A.T., Cook P.C., Lundie R.J., Jones L.H., Smith K.A., Barr T.A., Hochweller K., Anderton S.M., Hämmerling G.J., Maizels R.M., MacDonald A.S. 2010. CD11c depletion severely disrupts Th2 induction and development in vivo. J. Exp. Med. 207:2089–2096 10.1084/jem.20100734 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Podolsky D.K. 1997. Healing the epithelium: solving the problem from two sides. J. Gastroenterol. 32:122–126 10.1007/BF01213309 [DOI] [PubMed] [Google Scholar]
- Poulsen S.S., Kissow H., Hare K., Hartmann B., Thim L. 2005. Luminal and parenteral TFF2 and TFF3 dimer and monomer in two models of experimental colitis in the rat. Regul. Pept. 126:163–171 10.1016/j.regpep.2004.09.007 [DOI] [PubMed] [Google Scholar]
- Préfontaine D., Nadigel J., Chouiali F., Audusseau S., Semlali A., Chakir J., Martin J.G., Hamid Q. 2010. Increased IL-33 expression by epithelial cells in bronchial asthma. J. Allergy Clin. Immunol. 125:752–754 10.1016/j.jaci.2009.12.935 [DOI] [PubMed] [Google Scholar]
- Pushparaj P.N., Tay H.K., H’ng S.C., Pitman N., Xu D., McKenzie A., Liew F.Y., Melendez A.J. 2009. The cytokine interleukin-33 mediates anaphylactic shock. Proc. Natl. Acad. Sci. USA. 106:9773–9778 10.1073/pnas.0901206106 [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- Rani R., Smulian A.G., Greaves D.R., Hogan S.P., Herbert D.R. 2011. TGF-β limits IL-33 production and promotes the resolution of colitis through regulation of macrophage function. Eur. J. Immunol. 41:2000–2009 10.1002/eji.201041135 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rank M.A., Kobayashi T., Kozaki H., Bartemes K.R., Squillace D.L., Kita H. 2009. IL-33-activated dendritic cells induce an atypical TH2-type response. J. Allergy Clin. Immunol. 123:1047–1054 10.1016/j.jaci.2009.02.026 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rankin A.L., Mumm J.B., Murphy E., Turner S., Yu N., McClanahan T.K., Bourne P.A., Pierce R.H., Kastelein R., Pflanz S. 2010. IL-33 induces IL-13-dependent cutaneous fibrosis. J. Immunol. 184:1526–1535 10.4049/jimmunol.0903306 [DOI] [PubMed] [Google Scholar]
- Saenz S.A., Siracusa M.C., Perrigoue J.G., Spencer S.P., Urban J.F., Jr, Tocker J.E., Budelsky A.L., Kleinschek M.A., Kastelein R.A., Kambayashi T., et al. 2010. IL25 elicits a multipotent progenitor cell population that promotes TH2 cytokine responses. Nature. 464:1362–1366 10.1038/nature08901 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schmitz J., Owyang A., Oldham E., Song Y., Murphy E., McClanahan T.K., Zurawski G., Moshrefi M., Qin J., Li X., et al. 2005. IL-33, an interleukin-1-like cytokine that signals via the IL-1 receptor-related protein ST2 and induces T helper type 2-associated cytokines. Immunity. 23:479–490 10.1016/j.immuni.2005.09.015 [DOI] [PubMed] [Google Scholar]
- Seki N., Miyazaki M., Suzuki W., Hayashi K., Arima K., Myburgh E., Izuhara K., Brombacher F., Kubo M. 2004. IL-4-induced GATA-3 expression is a time-restricted instruction switch for Th2 cell differentiation. J. Immunol. 172:6158–6166 [DOI] [PubMed] [Google Scholar]
- Takeuchi O., Akira S. 2002. MyD88 as a bottle neck in Toll/IL-1 signaling. Curr. Top. Microbiol. Immunol. 270:155–167 10.1007/978-3-642-59430-4_10 [DOI] [PubMed] [Google Scholar]
- Taupin D., Podolsky D.K. 2003. Trefoil factors: initiators of mucosal healing. Nat. Rev. Mol. Cell Biol. 4:721–732 10.1038/nrm1203 [DOI] [PubMed] [Google Scholar]
- Taupin D., Wu D.C., Jeon W.K., Devaney K., Wang T.C., Podolsky D.K. 1999. The trefoil gene family are coordinately expressed immediate-early genes: EGF receptor- and MAP kinase-dependent interregulation. J. Clin. Invest. 103:R31–R38 10.1172/JCI3304 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thim L., Madsen F., Poulsen S.S. 2002. Effect of trefoil factors on the viscoelastic properties of mucus gels. Eur. J. Clin. Invest. 32:519–527 10.1046/j.1365-2362.2002.01014.x [DOI] [PubMed] [Google Scholar]
- Townsend M.J., Fallon P.G., Matthews D.J., Jolin H.E., McKenzie A.N. 2000. T1/ST2-deficient mice demonstrate the importance of T1/ST2 in developing primary T helper cell type 2 responses. J. Exp. Med. 191:1069–1076 10.1084/jem.191.6.1069 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Trzpis M., McLaughlin P.M., de Leij L.M., Harmsen M.C. 2007. Epithelial cell adhesion molecule: more than a carcinoma marker and adhesion molecule. Am. J. Pathol. 171:386–395 10.2353/ajpath.2007.070152 [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Panhuys N., Tang S.C., Prout M., Camberis M., Scarlett D., Roberts J., Hu-Li J., Paul W.E., Le Gros G. 2008. In vivo studies fail to reveal a role for IL-4 or STAT6 signaling in Th2 lymphocyte differentiation. Proc. Natl. Acad. Sci. USA. 105:12423–12428 10.1073/pnas.0806372105 [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Rijt L.S., Jung S., Kleinjan A., Vos N., Willart M., Duez C., Hoogsteden H.C., Lambrecht B.N. 2005. In vivo depletion of lung CD11c+ dendritic cells during allergen challenge abrogates the characteristic features of asthma. J. Exp. Med. 201:981–991 10.1084/jem.20042311 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Voehringer D., Reese T.A., Huang X., Shinkai K., Locksley R.M. 2006. Type 2 immunity is controlled by IL-4/IL-13 expression in hematopoietic non-eosinophil cells of the innate immune system. J. Exp. Med. 203:1435–1446 10.1084/jem.20052448 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wills-Karp M., Luyimbazi J., Xu X., Schofield B., Neben T.Y., Karp C.L., Donaldson D.D. 1998. Interleukin-13: central mediator of allergic asthma. Science. 282:2258–2261 10.1126/science.282.5397.2258 [DOI] [PubMed] [Google Scholar]
- Zaiss M.M., Kurowska-Stolarska M., Böhm C., Gary R., Scholtysek C., Stolarski B., Reilly J., Kerr S., Millar N.L., Kamradt T., et al. 2011. IL-33 shifts the balance from osteoclast to alternatively activated macrophage differentiation and protects from TNF-alpha-mediated bone loss. J. Immunol. 186:6097–6105 10.4049/jimmunol.1003487 [DOI] [PubMed] [Google Scholar]
- Zaph C., Troy A.E., Taylor B.C., Berman-Booty L.D., Guild K.J., Du Y., Yost E.A., Gruber A.D., May M.J., Greten F.R., et al. 2007. Epithelial-cell-intrinsic IKK-β expression regulates intestinal immune homeostasis. Nature. 446:552–556 10.1038/nature05590 [DOI] [PubMed] [Google Scholar]