Abstract
The role of N-linked glycosylation of the Newcastle disease virus (NDV) fusion (F) protein in viral replication and pathogenesis was examined by eliminating potential acceptor sites using a reverse genetics system for the moderately pathogenic strain Beaudette C (BC). The NDV-BC F protein contains six potential acceptor sites for N-linked glycosylation at residues 85, 191, 366, 447, 471, and 541 (sites Ng1 to Ng6, respectively). The sites at Ng2 and Ng5 are present in heptad repeat (HR) domains HR1 and HR2, respectively, and thus might affect fusion. Each N-glycosylation site was eliminated individually by replacing asparagine (N) with glutamine (Q), and a double mutant (Ng2 + 5) involving the two HR domains was also made. Each mutant was successfully recovered by reverse genetics except for the one involving Ng6, which is present in the cytoplasmic domain. All of the F proteins expressed by the recovered mutant viruses were efficiently cleaved and transported to the infected-cell surface. None of the individual mutations affected viral fusogenicity, but the double mutation at Ng2 and Ng5 in HR1 and HR2 increased fusogenicity >12-fold. The single mutations at sites Ng1, Ng2, and Ng5 resulted in modestly reduced multicycle growth in vitro. These three single mutations were also the most attenuating in eggs and 1-day-old chicks and were associated with decreased replication and spread in 2-week-old chickens. In contrast, the combination of the mutations at Ng2 and Ng5 yielded a virus that, compared to the BC parent, replicated >100-fold more efficiently in vitro, was more virulent in eggs and chicks, replicated more efficiently in chickens with enhanced tropism for the brain and gut, and elicited stronger humoral cell responses. These results illustrate the effects of N-glycosylation of the F protein on NDV pathobiology and suggest that the N-glycans in HR1 and HR2 coordinately downregulate viral fusion and virulence.
INTRODUCTION
Newcastle disease virus (NDV) is a major avian pathogen affecting many species of birds, and it causes severe economic losses to the poultry industry worldwide (2). NDV isolates cause a broad spectrum of disease ranging from fatal to asymptomatic infection. NDV strains are grouped as highly virulent (velogenic), moderately virulent (mesogenic), and minimally virulent (lentogenic) based on pathogenicity in chickens (2). NDV is a member of the genus Avulavirus in the family Paramyxoviridae (39). The genome of NDV is a single-stranded, nonsegmented, negative-sense RNA of 15,186 nucleotides (nt) (10, 22, 34, 38). The genomic RNA contains six genes that encode at least seven proteins (7, 47). NDV initiates infection after attachment to susceptible cells and a subsequent membrane fusion process directed by two virion glycoproteins associated with the envelope, the hemagglutinin (HA)-neuraminidase (HN) protein and the fusion (F) protein (23). The HN protein mediates attachment by binding to the sialic acid receptor, has neuraminidase activity, and plays a role in fusion promotion, whereas the F protein is responsible for membrane fusion and penetration through the host cell membrane (24). The NDV F protein does not require the acidic pH of endosomes for the activation of fusion process; because of this acidic pH independence, infected cells fuse with adjacent cells to form syncytia, a process very similar to virus-cell fusion (4). Although the trigger mechanism for F-mediated membrane fusion is still unknown, it is postulated that interaction between the HN and F proteins stimulates conformational changes in the F protein that drive mergers of viral and host cell membranes (26).
The NDV F protein is a trimeric type I integral membrane protein that is synthesized as an inactive precursor F0 (66 kDa) that is posttranslationally cleaved by host cell proteases into two disulfide-linked subunits, N-terminal F2 (12.5 kDa) and C-terminal F1 (55 kDa) (34). A stretch of hydrophobic amino acids at the N terminus of the F1 subunit form a fusion peptide (FP) that interacts with the host cell membrane, thereby initiating the fusion process. The NDV F protein has two heptad repeat (HR) motifs in the F1 subunit; HR1 is adjacent to the fusion peptide, and HR2 is adjacent to the transmembrane (TM) domain. Crystal structure analysis of fusion proteins of different paramyxoviruses revealed that these heptad repeats assemble to form conserved six-helix bundles and that this assembly is tightly coupled to membrane fusion (4, 8, 31, 43, 48–51). Subsequent structural, biochemical, and functional studies of fusion protein of paramyxoviruses have led to the hypothesis that, prior to interaction of F protein with the host cell, the F protein is believed to fold in a prefusion, metastable conformation, which is then activated to undergo a large conformational rearrangement needed to accomplish membrane fusion (23, 25, 26). However, the mechanistic details of the extensive conformational rearrangements of the fusion protein are still not clear.
The F glycoprotein of NDV undergoes N-linked glycosylation in the rough endoplasmic reticulum of host cells, in which N-glycan chains are attached covalently to asparagine residues at the consensus sequence motif Asn-X-Ser/Thr (4, 6, 9, 11) (where “X” can be any amino acid except proline). N-glycans of viral envelope glycoproteins are involved in many functions, such as promoting efficient expression, transport, folding, and binding to cell surface receptors and facilitating fusion and infectivity (1, 3, 6, 9, 12, 14, 37). On the other hand, N-linked glycans also act in shielding the virus against antibody neutralization as has previously been reported to occur in HIV and hepatitis B and influenza viruses (19, 44, 46).
The F glycoprotein of NDV contains six potential N-linked glycosylation acceptor sites at residues 85, 191, 366, 447, 471, and 541 that are conserved in all strains (10, 36). A previous study has predicted that four of these sites present at residues 85, 191, 366, and 471 are functionally active (33). Two of these residues at positions 191 and 471 are present within the heptad repeats HR1 and HR2, suggesting that N-glycosylation at these sites might play an important role in the fusion promotion. The previous study demonstrated the role of N-linked glycosylation of NDV F protein in biological activity and protein stability using a plasmid transfection system (33). However, the contribution of NDV F protein N-linked glycosylation to virus replication, pathogenesis, and virulence in the natural host is unknown.
In the present study, a reverse genetics system was used to generate a panel of recombinant viruses with mutations in the N-glycosylation sites of the NDV F protein. These mutations eliminated each of the six N-glycosylation sites individually (Ng1, Ng2, Ng3, Ng4, Ng5, and Ng6) and in combination (Ng2 and Ng5). These mutant viruses allowed us to determine the usage of each N-glycosylation site and study the role of each N-glycan in the functional activity of the F protein and its effect on viral replication, pathogenesis, virulence, and immunogenicity in chickens. We demonstrate that, with deglycosylation of each N-glycan site, the NDV F protein remains completely functional. However, deletion of N-glycosylation sites in viruses modulates the viral pathogenesis to various extents.
MATERIALS AND METHODS
Cells and viruses.
A chicken embryo fibroblast cell line (DF1) and a human epidermoid carcinoma cell line (HEp-2) were grown in Dulbecco's minimal essential medium (DMEM) with 10% fetal bovine serum (FBS) and maintained in DMEM with 5% FBS. African green monkey kidney Vero cells were grown in Eagle's minimal essential medium (EMEM) containing 10% FBS and maintained in EMEM with 5% FBS. The modified vaccinia virus strain Ankara (MVA) expressing T7 RNA polymerase was kindly provided by Bernard Moss (NIH, Bethesda, MD) and propagated in primary chicken embryo fibroblast cells in DMEM with 2% FBS. The moderately pathogenic (mesogenic) NDV strain Beaudette C (BC) and its recombinant derivatives were grown in 9-day-old embryonated specific-pathogen-free (SPF) chicken eggs in an enhanced biosafety level 3 (BSL3) containment facility certified by the USDA following the guidelines of the IACUC, University of Maryland. After 2 days, the allantoic fluid was harvested and the virus was plaque purified using our standard procedure (21).
Construction of plasmids and recovery of mutant viruses.
The construction of plasmid pNDVfl carrying the full-length antigenome cDNA of NDV strain BC has been described previously (21). In the present study, a unique PacI site was created in the downstream untranslated region (UTR) of the M gene. To introduce mutations into the F gene of pNDVfl, a PacI-MluI fragment containing the F gene was amplified using each N-glycosylation mutant and forward and reverse primers with the desired mutations (Table 1). Two PCR products were generated, one by using a PacI forward primer and N-glycan site-specific mutated reverse primer and the second by using an N-glycan-specific mutated forward primer and MluI reverse primer. The PacI-MluI fragment containing the desired N-glycosylation mutation was amplified by overlapping PCR. The PCR product was cloned into pCR 2.1-TOPO vector (Invitrogen). The inserts bearing the N-glycan mutation were released by digestion with PacI and MluI and then cloned into the full-length cDNA of strain BC. A panel of N-glycosylation F mutants was generated as shown in Fig. 1. A double F mutant, Ng2 + 5, was also created by eliminating N-glycosylation sites 2 and 5. This was done by subjecting the Ng2 mutant to a second round of mutagenesis to remove Ng5. All mutant F cDNAs were sequenced in their entirety to confirm the presence of the desired mutations. Transfection and recovery of recombinant NDV mutants were performed by using a reverse genetics technique described previously (21).
Table 1.
Primers used in this study
| Primer | Nucleotide sequencea |
|---|---|
| Ng1 Forward | 5′ATGCATACCAGAGGACATTGACCACTTTGCTCACCCC3′ |
| Ng1 Reverse | 5′AATGTCCTCTGGTATGCATCCAAGGGGGCTTTCGCAC3′ |
| Ng2 Forward | 5′ACCAATTTCAGAAAACAGCTCAGGAATTAGGCTGCATCAG3′ |
| Ng2 Reverse | 5′AGCTGTTTTCTGAAATTGGTCATTAACAAACTGCTG3′ |
| Ng3 Forward | 5′GGCCAGACATCGGCCTGTATGTACTCAAAGACCG3′ |
| Ng3 Reverse | 5′CAGGCCGATGTCTGGCCGCTCAAGCAGGAATAAATACC3′ |
| Ng4 Forward | 5′CAGAAGCAGATCTCAATACAAGATTCTC3′ |
| Ng4 Reverse | 5′TATTGAGATCTGCTTCTGATAAGTTGCATCG3′ |
| Ng5 Forward | 5′GAATGTCCAGAACTCGATCAGTAATGCTTTGAATAAGTTAG3′ |
| Ng5 Reverse | 5′GAGTTCTGGACATTCCCAAGCTCAGTTG 3′ |
| Ng6 Forward | 5′ATTATGGCTTGGGCAGAATACCCTAGATC3′ |
| Ng6 Reverse | 5′CTAGGGTATTCTGCCCAAGCCATAATAAGGTC3′ |
| Ng7 Forward | 5′ATTATGGCTTGGGAATAATACCCTAGATC3′ |
| Ng7 Reverse | 5′CTAGGGTATTATTCCCAAGCCATAATAAGGTC3′ |
Bolded and underlined characters indicate mutations.
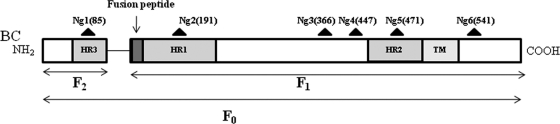
Fig 1.
Linear diagram of the NDV F protein. ▴, potential N-glycosylation sites Ng1 to Ng6, with the amino acid positions of the Asn residues indicated in parentheses. Dark gray boxes, heptad repeats; light gray box, transmembrane (TM) domain.
RT-PCR and sequence analysis.
The recovered F mutant viruses were subjected to five passages in 9-day-old SPF chicken embryos. From each passage, total RNAs were isolated from mutant NDV-infected allantoic fluid of 9-day-old SPF chicken embryos by the use of TRIzol reagent (Invitrogen). Reverse transcription-PCR (RT-PCR) was performed using a Thermoscript RT-PCR kit (Invitrogen) with primers PacIF (5′-4442CTAATCTGTCTTGATTAATTAAAGTTAGTTTACCTGTC4479-3′; positive sense) and MluIR (5′-6306TCATCTACAACGCGTAGTTTTTTCTAAAC6278-3′; negative sense) to amplify the F gene. The amplified cDNA fragments were then sequenced using a BigDye Terminator version 3.1 cycle sequencing kit (Applied Biosystems Inc.) and an ABI 3130xl Genetic Analyzer to confirm the presence of the introduced mutations in the recovered viruses. The HN gene from each recovered virus was also sequenced with available primers from our laboratory.
Production of anti-NDV F antisera.
Three synthetic peptides were custom synthesized (Invitrogen): a C-terminal tail (30 residues), corresponding to amino acids 524 to 553 of the cytoplasmic tail of the F protein; peptide A (10 residues), corresponding to amino acids 27 to 36; and peptide B (10 residues), corresponding to amino acids 67 to 76. One rabbit was injected subcutaneously with 1 mg of keyhole limpet hemocyanin (KLH)-conjugated C-terminal tail peptide, and another rabbit was injected with 0.5 mg each of KLH-conjugated peptide A and peptide B in Freund's complete adjuvant to raise anti-Fcyt and anti-FNterm antiserum, respectively. After 2 weeks, a booster immunization was given with 0.5 mg of peptide in Freund's incomplete adjuvant, andthe hyperimmune sera were collected 2 weeks later. Western blot analysis was performed using NDV-infected cell lysates to confirm the specificity of the two antisera to NDV F protein (data not shown).
Western blot analysis and PNGase F digestion.
Vero cells were infected with each mutant virus at a multiplicity of infection (MOI) of 1.0 and incubated for 1 h at 37°C. Cells were washed with phosphate-buffered saline (PBS) and overlaid with 2% DMEM. After 36 h postinfection (p.i.), the cells were washed with PBS and divided into two aliquots. From one aliquot, proteins were extracted using cell lysis buffer (Clontech), and the second aliquot was treated with denaturing buffer (New England BioLabs). Equal amount of cell lysates from the first aliquot were diluted in Laemmli sample buffer (Bio-Rad Laboratories) in the presence of reducing agent and loaded onto 10% polyacrylamide gels. Equal amounts of cell lysates from the second aliquot were digested with PNGaseF (New England BioLabs). Briefly, infected cell extracts were denatured at 100°C for 10 min. The reaction mixture was put on ice for 5 min, and PNGaseF (2 U), 10× reaction buffer, and 10% NP-40 supplied by the manufacturer were added to equal amounts of cell lysates from each recombinant virus in 40 μl of reaction buffer and incubated overnight at 37°C. The digestion was stopped by boiling, and samples were diluted in Laemmli sample buffer in the presence of reducing agent and loaded onto 10% polyacrylamide gels along with equal amounts of undigested cell lysates. After electrophoresis, the gels were equilibrated in transfer buffer and transferred onto a nitrocellulose membrane. The membrane was blocked with blocking solution (5% skim milk–PBS) for 2 h at room temperature and incubated with primary antibody anti-Fcyt (1:100 dilution) overnight at 4°C. Membranes were washed three times in washing solution (0.05% Tween 20–PBS) and then incubated in secondary antibody, and anti-rabbit IgG antibodies were diluted (1:5,000) in dilution buffer for 1 h at room temperature. Membranes were washed extensively, and bound antibody was detected using an ECL Western blotting detection reagent system (Amersham).
Cell surface expression of the F proteins of N-glycosylation mutant viruses.
Cell surface expression of the F proteins of N-glycosylation mutant viruses was quantitatively determined by flow cytometry. Briefly, DF1 cells were infected with each recombinant virus at an MOI of 0.1. After 24 h, the cells were detached with PBS containing 5 mM EDTA and centrifuged at 500 × g for 5 min at 4°C. Cells were then incubated with the anti-FNterm antiserum (1:10 dilution) for 30 min at 4°C. Subsequently, cells were washed with PBS and incubated for 30 min on ice with 1:500-diluted Alexa Fluor 488-conjugated goat anti-rabbit immunoglobulin G antibodies. Cells were analyzed by using a FACSria II apparatus and Flowjo software (Becton Dickinson Biosciences).
Fusion assay and syncytium formation of N-glycosylation mutant viruses.
The ability of each N-glycosylation mutant virus to form syncytia was determined according to a procedure described by Kohn (20). Briefly, Vero cells in 6-well plates were infected with each virus at an MOI of 0.1. Cells were maintained in 5% MEM at 37°C and 5% CO2. At 36 h p.i., the medium was removed and the cells were washed with PBS, fixed with methanol for 20 min at room temperature, and stained with hematoxylin-eosin. The fusion index of each mutant virus was calculated by observing 10 fields per well in duplicate. The fusion index is the ratio of the total number of nuclei to the number of cells in which these nuclei are present (i.e., the mean number of nuclei per cell).
Growth characteristics of N-glycosylation mutant viruses.
The growth kinetics of N-glycosylation mutant viruses were evaluated by multiple-step growth assays. DF1 cells in duplicate wells of six-well plates were infected with each virus at an MOI of 0.01. After 1 h of adsorption, the cells were washed with PBS and overlaid with DMEM containing 2% FBS at 37°C. Supernatant was collected and replaced with an equal volume of fresh medium at 8-h intervals until 64 h p.i. The titer of virus in the sample was quantified by a plaque assay on DF1 cells. All plaque assays were performed in six-well plates. Briefly, monolayers of DF1 cells were infected with 0.2 ml of 10-fold-diluted fresh virus-infected allantoic fluid. After 1 h of adsorption, cells were covered with DMEM containing 2% FBS and 0.8% methylcellulose and then incubated at 37°C. Six days later, the cells were fixed with methanol and stained with crystal violet. The syncytium formation in DF1 cells was determined in duplicate wells of six-well plates infected with each virus at an MOI of 0.01. Cells were maintained in 5% DMEM at 37°C and 5% CO2. At 24 h p.i., the medium was removed and the cells were washed with PBS, fixed with methanol for 20 min at room temperature, and stained with hematoxylin-eosin.
Pathogenicity studies.
The pathogenicity of the N-glycosylation mutant viruses was determined by a mean death time (MDT) test in 9-day-old embryonated chicken eggs and the intracerebral pathogenicity index (ICPI) test in 1-day-old chicks (2) and in 2-week-old chickens. All studies were conducted under biosafety level (BSL3)-enhanced (E) conditions at the University of Maryland.
Briefly, for the MDT test, a series of 10-fold (10−6 to 10−10) dilutions of fresh infective allantoic fluid was made with sterile phosphate-buffered saline, and 0.1 ml of each diluent was inoculated into the allantoic cavity of five 9-day-old SPF embryonated chicken eggs and incubated at 37°C. Each egg was examined three times daily for 7 days, and times of embryo death were recorded. The minimum lethal dose is defined as the highest virus dilution that causes all embryos inoculated with that dilution to die. The MDT is the mean time in hours required for the minimum lethal dose to kill all inoculated embryos.
For the ICPI test, 0.05 ml (1:10 dilution) of fresh infective allantoic fluid of each virus was inoculated into groups of 10 1-day-old SPF chicks via the intracerebral route. The inoculation was done using a 27-gauge needle attached to a 1-ml stepper syringe dispenser that was set to dispense 0.05 ml of solution per inoculation. The birds were inoculated by inserting the needle up to the hub into the right or left rear quadrant of the cranium. The birds were observed for clinical symptoms and mortality once every 8 h for a period of 8 days. At each observation, the birds were scored as follows: 0, healthy; 1, sick; or 2, dead. The ICPI is the mean score per bird per observation over the 8-day period.
The pathogenicity of the F mutant viruses was further evaluated in 2-week-old chickens by a natural route of infection. Briefly, 2-week-old SPF chickens in groups of 10 were inoculated with 106 PFU (50 μl in each naris and eye) of each virus per chicken via the occulonasal route. The birds were observed daily for clinical signs of disease until 14 days p.i. In order to determine the replication efficiency of the mutant viruses, additional 2-week-old chickens in groups of 5 were inoculated with 106 PFU of the parental virus and each mutant virus per chicken via the occulonasal route. At 3 day p.i., 3 birds from each group were sacrificed and organs (brain, nasal turbinate, lungs, and gut) were collected. The virus titers in these organs in DF1 cells were determined by a plaque assay. The extra 2 birds in each group were present to accommodate possible losses due to infection, which occurred in the recombinant Ng2 + 5 (rNg2 + 5) group.
Measurement of humoral responses of N-glycosylation mutant viruses by ELISA.
Four-week-old chickens in groups of 5 were inoculated with 106 PFU of wild-type and N-glycosylation mutant viruses per bird via the occulonasal route. Serum samples were collected on the 3rd, 7th, and 14th days p.i. Commercial NDV enzyme-linked immunosorbent assay (ELISA) kits (Synbiotics Corporation, San Diego, CA) were used to detect antibodies against the NDV antigens. The assay was designed to measure NDV antibody bound to NDV whole-antigen-coated plates. Serum samples were diluted 1:100 in dilution buffer (Synbiotics Corporation), added to the plates, and incubated for 1 h at room temperature. The plates were washed three times with plate-washing solution (Synbiotics Corporation) and incubated for 1 h with an isotype-specific secondary antibody, namely, horseradish peroxidase (HRP)-conjugated goat anti-chicken IgG. The plates were washed three times and developed with ABTS [2,2′-azinobis(3-ethylbenzothiazoline-6-sulfonic acid)-diammonium salt] peroxidase substrate solution (Synbiotics Corporation), development was stopped by the addition of peroxidase stop solution, and analysis was performed at 405 nm using an ELx800 ELISA plate reader (BioTek, Winooski, VT).
RESULTS
Generation of recombinant NDVs containing mutations that eliminate potential N-glycosylation acceptor sites in the F protein.
We investigated the role of N-linked glycosylation of the NDV F protein in viral biological activities and viral pathogenesis using a previously described reverse genetics system for the mesogenic strain Beaudette C (BC) (21). The NDV F protein has six potential acceptor N-glycosylation sites, as indicated in Fig. 1. The wild-type recombinant BC parent (rBC) containing an introduced, unique MluI site (positions 6292 to 6297) in the intergenic region between the F and HN genes had previously been created, and for the present study this parent was further modified to contain a unique PacI site (positions 4456 to 4463) in the downstream untranslated region of the M gene. Thus, mutations could readily be introduced into the PacI-MluI fragment bearing the F gene. Each of the six potential N-linked glycosylation sites at amino acid sequence positions 85, 191, 366, 447, 471, and 541 (Ng1 to Ng6, respectively) in the F protein was mutated by overlapping PCR to change asparagine, the first amino acid residue of the conserved sequence NXS/T, to glutamine. Glutamine was chosen because it is structurally similar to asparagine, differing by only a single methylene group. To make each mutation, the first and third positions (underlined) of the respective aspargine codon (AAT or AAC, depending on the particular site) were replaced to create a codon for glutamine (CAG). Thus, each mutant would require two nucleotide changes in order to revert to any codon specifying asparagine, thereby reducing the likelihood of direct reversion during virus replication. A double N-glycosylation mutant was also created for Ng2 (position 191) and Ng5 (position 471) to examine the effect of combined loss of the two N-linked glycosylation sites in HR1 and HR2. The single-site mutants were designated Ng1, Ng2, Ng3, Ng4, Ng5, and Ng6, and the one double mutant was designated Ng2 + 5. The sequence of each mutant F gene was confirmed in the final cDNA clones. Recombinant viruses were recovered as described previously (21). We were unable to recover a viable virus from the Ng6 cDNA in several attempts. To investigate this further, we changed the glutamine to asparagine in the Ng6 clone by using primers Ng7 forward and Ng7 reverse and found that infectious virus (Ng7 clone) could readily be recovered. This indicated that the inability to recover rNg6 virus was specific to that mutation, implying that it is severely debilitating or lethal. The presence of the introduced mutations in the mutant viruses was confirmed by RT-PCR and subsequent DNA sequence analysis of the F gene of each virus (data not shown). The HN gene of each mutant virus was also sequenced, and no adventitious mutations were detected in either the F or the HN gene. To determine the genetic stability of each F gene mutation, the recovered viruses were plaque purified and subjected to five passages in 9-day-old embryonated chicken eggs. Sequence analysis of the F and HN genes of the mutant viruses at each passage level showed that the introduced mutations were unaltered and that no adventitious or compensatory mutations had been introduced (data not shown).
Determination of the N-glycosylation site usage in the NDV F protein.
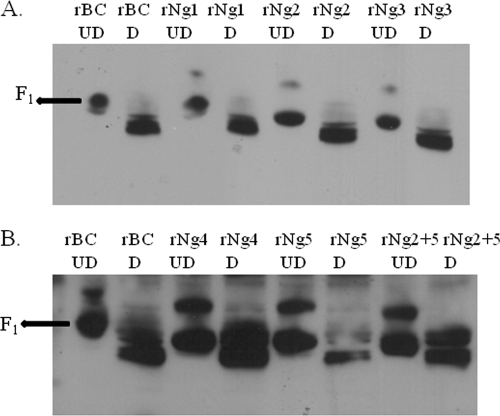
We examined the F proteins encoded by the N-glycosylation mutants to determine which of the potential N-linked glycosylation sites in the NDV-BC F protein were utilized. Vero cells were infected with wild-type rBC and the N-glycosylation mutant viruses. The infected cell lysates were divided into two aliquots: one aliquot was left untreated, and the other was treated with PNGaseF, which cleaves high mannose and complex oligosaccharides from N-linked glycoproteins (Fig. 2). The relative electrophoretic mobilities of the F proteins were examined by Western blot analysis in the presence of reducing agent by using rabbit antiserum raised against a synthetic peptide representing the NDV F cytoplasmic tail (anti-Fcyt antiserum). The sizes of the F0 and F1 proteins of wild-type rBC are 66 and 55 kDa, respectively. Our results showed that the F0 protein was efficiently cleaved in the wild-type and all mutant viruses. In undigested cell lysates, mutation of single N-glycosylation sites resulted in faster electrophoretic migration of mutant F1 protein compared to the wild-type F1 protein except for rNg1, suggesting that each mutation resulted in the loss of an N-linked glycan (Fig. 2). In the case of rNg1, the N-glycan site at residue 85 is present in the F2 subunit; hence, we observed a migration pattern of rNg1 F1 protein similar to that seen with rBC. In the double mutant, rNg2 + 5, the mobility shift of the F0 and F1 proteins was greater compared to that of F proteins of the single-site mutants, suggesting that N-glycans had been removed from both site 191 and site 471 (Fig. 2B). The F proteins of the smutants, after treatment with PNGaseF, comigrated with those of the wild-type virus, supporting the interpretation that sites Ng1 to Ng5 are used in the NDV F protein for N-glycosylation and that replacement of asparagine with glutamine at the respective sites prevented N-glycosylation.
Fig 2.
Analysis of the F proteins of the N-glycosylation mutants by Western blotting and PNGaseF digestion. Vero cells were infected with wild-type rBC and N-glycosylation mutant viruses at an MOI of 1, and total proteins were collected after 36 h p.i. Samples were resolved on 10% polyacrylamide gels in the presence of reducing agent. Samples from rBC, rNg1, rNg2, and rNg3 (A) and rBC, rNg4, rNg5, and rNg2 + 5 (B) were digested overnight with PNGaseF or kept as untreated controls, separated by 10% polyacrylamide gels in the presence of reducing agent, and blotted onto nitrocellulose membranes. Western blot analysis was performed using a rabbit antiserum raised against a synthetic peptide designed from the F protein cytoplasmic tail. D, digested; UD, undigested.
Cell surface expression of F proteins encoded by the N-glycosylation mutant viruses.
Cell surface expression of the F proteins of the N-glycosylation mutant viruses was quantified by flow cytometry. DF1 cells were infected with each of the mutant viruses, and at 24 h p.i., the cells were detached, treated with rabbit antiserum raised against a mixture of two synthetic peptides designed from the N-terminal region of the F protein (anti-FNterm antiserum), treated with Alexa Fluor-conjugated goat anti-rabbit antibodies, and analyzed by flow cytometry (Table 2). The results showed that the percentages of cells expressing the different mutant F proteins were similar to that of the wild-type rBC virus. The mean fluorescence intensities of rNg3, rNg4, and rNg2 + 5 ranged from 15% to 25% above that of the wild-type rBC, while cells infected with rNg1 and rNg2 had decreased mean fluorescence intensities of 5% and 7% lower than that of wild-type rBC. These results suggested that all the N-glycosylation mutant F proteins retained their ability to be transported efficiently to the cell surface.
Table 2.
Cell surface expression of the F proteins of the N-glycosylation mutant virusesa
| Virus | % of positive cells ± SD | Relative mean fluorescence intensity |
|---|---|---|
| rBC | 99 ± 2.4 | 1.00 |
| rNg1 | 98 ± 3.8 | 0.95 |
| rNg2 | 99 ± 4.2 | 0.93 |
| rNg3 | 96 ± 3.1 | 1.15 |
| rNg4 | 97 ± 2.2 | 1.20 |
| rNg5 | 99 ± 1.8 | 1.00 |
| rNg2 + 5 | 99 ± 3.0 | 1.25 |
| None (mock-infected cells) | 0.01 |
Cell surface expression of the F protein was determined by flow cytometry. DF1 cells were infected with each mutant virus at an MOI of 0.1. Surface expression of the F proteins was assessed by flow cytometry at 24 h p.i. with a cocktail of anti-FNterm antibody followed by anti-rabbit Alexa Fluor 488-conjugated antibodies. Surface immunofluorescence was quantitated by fluorescence-activated cell sorter (FACS) analysis. Uninfected DF1 cells were used as negative controls. Values shown represent averages of the results from three independent experiments. SD, standard deviation (P <0.05).
Fusion activity of N-glycosylation mutant viruses.
To determine the role of each N-glycan in the fusion activity of F protein, Vero cells were infected with the mutant viruses and, at 36 h p.i., the cells were fixed and stained with hematoxylin-eosin and examined microscopically to quantify the percentage of nuclei involved in syncytia as the fusion index. The fusion indices of the rNg1, rNg2, rNg3, rNg4, and rNg5 viruses were similar to that of the wild-type rBC virus (Fig. 3). Interestingly, the rNg2 + 5 double-mutant virus exhibited a dramatically increased (>12-fold higher) fusion index compared to the parental rBC virus (Fig. 3). Thus, the individual elimination of N-linked glycosylation sites (including Ng2 and Ng5 in HR1 and HR2) did not significantly change the fusion activity of NDV F protein, but the dual loss of the sites in HR1 and HR2 in rNg2 + 5 resulted in a dramatic increase in fusion activity.
Fig 3.
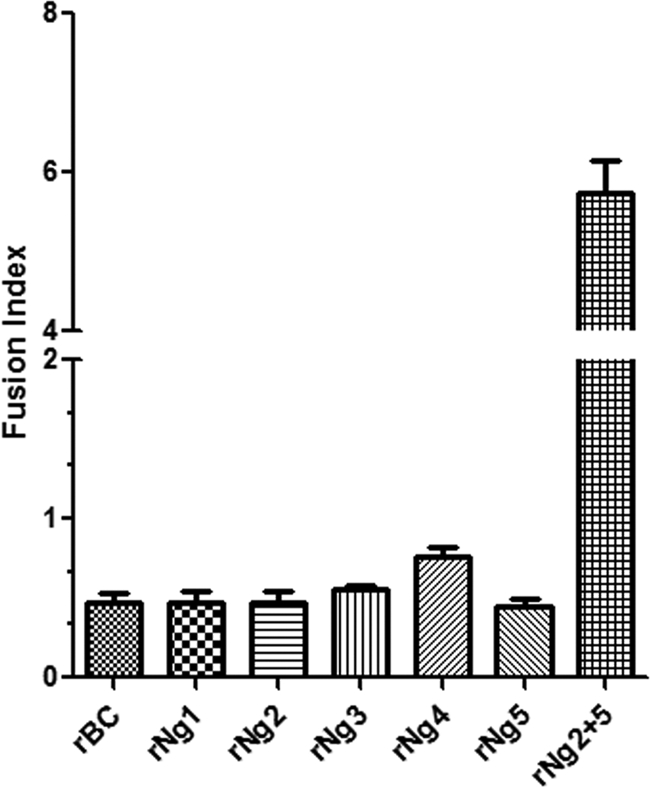
Comparison of the fusogenicities of wild-type rBC and the N-glycosylation mutant viruses. Vero cells were infected with the indicated viruses at an MOI of 0.1, fixed at 36 h p.i., and stained with hematoxylin-eosin. The fusion index was calculated as the ratio of the total number of nuclei in multinuclear cells to the total number of nuclei in the field. Data represent the means of the results from three independent experiments.
Growth characteristics of the N-glycosylation mutant viruses in cell culture.
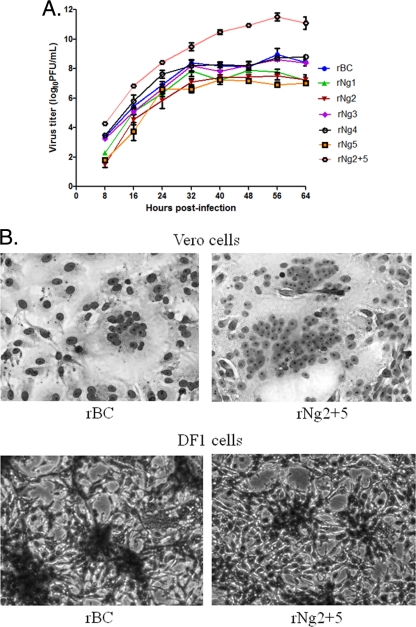
The in vitro replication characteristics of the wild-type and mutant viruses were compared in a multistep growth experiment in DF1 cells (Fig. 4A). Mutant viruses rNg1, rNg2, and rNg5 exhibited modestly delayed and reduced growth compared to the parental rBC virus: the yield of rNg1 was 0.5 log10 lower, whereas those of rNg2 and rNg5 were 1 log10 lower. In addition, syncytium formation by rNg1, rNg2, and rNg5 was evident by 36 h p.i. compared to 24 h p.i. for wild-type rBC in DF1 cells. For mutant viruses rNg3 and rNg4, there was no significant difference in growth kinetics or syncytium formation compared to wild-type rBC. Interestingly, the double-mutant virus rNg2 + 5 replicated faster and attained a much higher titer than the wild-type virus. Specifically, at 64 h p.i., the titer of mutant virus rNg2 + 5 was 2.5 log10 higher than that of the wild-type virus. Furthermore, the rNg2 + 5 virus initiated syncytium formation at 18 h p.i. compared to 24 h p.i. for the wild-type virus (Fig. 4B). These results demonstrated that the individual elimination of Ng1, Ng2, and Ng5 of the NDV F protein decreased the replication of the virus to various extents, whereas the combination of two of these sites, Ng2 and Ng5, in the double mutant rNg2 + 5 strongly increased virus replication.
Fig 4.
Growth kinetics of viruses in tissue culture. (A) Comparison of multicycle growth kinetics of wild-type rBC and the N-glycosylation mutant viruses in DF1chicken embryo fibroblast cells. Cells were infected with the indicated viruses at an MOI of 0.01, and cell culture medium supernatant aliquots were harvested and replaced at 8-h intervals until 64 h p.i. The virus titers in the aliquots were determined by plaque assays in DF1 cells. Values represent averages of the results from three independent experiments. (B) Syncytium formation of rBC and rNg2 + 5 in Vero and DF1 cells. Vero and DF1 cells were infected in duplicate wells of six-well plates with each virus at an MOI of 0.01. Cells were maintained in 5% DMEM at 37°C and 5% CO2. At 24 h p.i., the medium was removed and the cells were washed with PBS, fixed with methanol for 20 min at room temperature, and stained with hematoxylin-eosin.
Pathogenicity of the N-glycosylation mutant viruses in chicken eggs and 1-day-old chicks.
The pathogenicity of the N-glycosylation mutant viruses and that of their wild-type rBC parent were evaluated by two standard pathogenicity assays, namely, the mean embryo death time (MDT) assay and the intracerebral pathogenicity index (ICPI) test. MDT values were determined in 9-day-old embryonated chicken eggs (Table 3). NDV strains are categorized into three pathotypes on the basis of their MDT values: velogenic (MDT less than 60 h), mesogenic (60 to 90 h), and lentogenic (greater than 90 h). The MDT values of rNg1 (76 h) and rNg2 (78 h) were increased compared to that of the wild-type rBC parent (59 h), indicating a modest reduction in virulence. The rNg3, rNg4, and rNg5 viruses had MDT values of 60 h, 56 h, and 68 h, respectively, which were marginally increased (i.e., attenuated) compared to wild-type rBC. In contrast, the MDT value of the rNg2 + 5 double mutant was 51 h, indicating an increase in virulence compared to wild-type rBC. We also evaluated the pathogenicity of the recombinant viruses in 1-day-old chicks by the ICPI test. Velogenic strains give values approaching 2.0, whereas lentogenic strains give values close to 0. The ICPI values of the parental rBC, rNg1, rNg2, rNg3, rNg4, rNg5, and rNg2 + 5 viruses were 1.52, 1.16, 1.12, 1.42, 1.48, 1.30, and 1.88, respectively (Table 3). Thus, the results of the ICPI test were consistent with the results of the MDT test: specifically, the rNg1 and rNg2 mutants were the most attenuated, followed by the rNg5 mutant, and the rNg3 and rNG4 mutants were the least attenuated compared to the wild-type rBC parent. In contrast, the rNg2 + 5 mutant was more virulent than rBC virus.
Table 3.
Pathogenicity of the N-glycosylation mutant viruses in embryonated eggs and chicks
| Virus | MDT (h)a | ICPI scoreb |
|---|---|---|
| rBC | 59 | 1.52 |
| rNg1 | 76 | 1.16 |
| rNg2 | 78 | 1.12 |
| rNg3 | 60 | 1.42 |
| rNg4 | 56 | 1.48 |
| rNg5 | 68 | 1.30 |
| rNg2 + 5 | 51 | 1.88 |
Mean embryo death time (MDT) values represent the mean time required for the minimum lethal dose of virus to kill all of the inoculated embryos. Pathotype MDT definitions: virulent strains, <60 h; intermediately virulent strains, 60 to 90 h; avirulent strains, >90 h.
Intracerebral pathogenicity index (ICPI) scores were calculated as follows: ICPI = [(total number of sick chicks × 1) + (total number of dead chicks × 2)]/80 observations. ICPI values for velogenic strains approached the maximum score of 2.00, whereas lentogenic strains gave values close to 0. Values represent the means of the results from three independent experiments. P < 0.05.
Replication and virulence of the N-glycosylation mutant viruses in 2-week-old chickens.
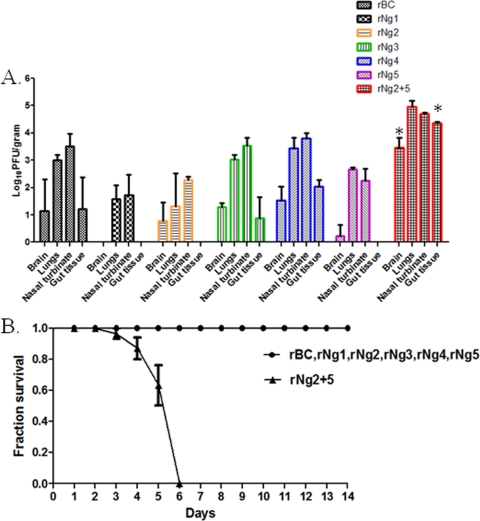
We examined the effect of mutations of the N-glycosylation sites of the F protein on replication and virulence in 2-week-old chickens. Chickens in groups of 5 were inoculated by the oculonasal route (mimicking natural infection) at a dose of 106 PFU per bird. Three chickens from each group were euthanized on the 3rd day p.i., and tissue samples of the brain, lung, nasal turbinates, and gut were collected. All of the birds appeared to be healthy on the 3rd day p.i. except in the case of birds infected with the rNg2 + 5 virus, where two birds were found dead and one paralyzed on the 3rd day p.i. (tissues were taken only from the 3 living birds). Virus titers in tissue samples were measured by a plaque assay using DF1 cells (Fig. 5A). Differences in the presence or absence of virus and in the virus titers in the different organs were observed between wild-type rBC and the N-glycosylation mutant viruses. The rNg1 mutant virus was not detected in the brain and gut, and its titers in the lung and nasal turbinate tissue were reduced by ∼50% compared to those of wild-type rBC. The rNg2 mutant virus was not detected in gut tissue, and there were 43%, 64%, and 67% reductions in titers in the lung, nasal turbinates, and brain compared to those seen with wild-type rBC virus. The rNg3 virus replicated at titers in the brain, lungs, and nasal turbinates similar to those seen with the wild-type virus, whereas replication of the rNg5 virus was somewhat reduced and that mutant was not detected in gut tissue. The rNg4 virus replicated to 7% (nasal turbinates), 14% (lungs), and 33% (brain) to 62% (gut) higher titers compared to wild-type rBC. The double mutant rNg2 + 5 virus replicated to significant higher titers in all of the sampled organs compared to the rBC parent, specifically, ∼3 logs higher titer in the gut and brain and 65% and 33% greater in the lungs and nasal turbinates, respectively. These results are consistent with the results of the MDT and ICPI tests, showing that, compared to wild-type rBC, rNg1 and rNg2 were the most attenuated, followed by rNg5, whereas rNg2 + 5 exhibited increased replication. We also examined the effects of the N-glycosylation mutations on morbidity and mortality. Two-week-old chickens in groups of 10 were inoculated with each mutant virus via the oculonasal route with 106 PFU of virus per bird and were observed for 14 days for clinical signs (Fig. 5B). The birds inoculated with wild-type rBC showed clinical signs of depression, watery greenish diarrhea, and drooping wings by the 9th day p.i. The groups of birds infected with the single-site N-glycosylation mutant viruses remained healthy throughout the observation period. In contrast, birds inoculated with the double-mutant rNg2 + 5 virus first exhibited signs of sickness and paralysis at 2 day p.i., and deaths were observed beginning at day 3 p.i. By the 6th day p.i., all 10 birds inoculated with the double-mutant rNg2 + 5 virus had died (Fig. 5B).
Fig 5.
Virus replication in the indicated organs (A) and percent survival (B) of 2-week-old chickens inoculated with wild-type rBC and the N-glycosylation mutant viruses. (A) Two-week-old chickens in groups of 5 were inoculated with 106 PFU of virus per bird by the oculonasal route, mimicking natural infection. Three chickens per group were sacrificed 3 days p.i., and samples of the brain, lungs, trachea, and gut were collected (more birds were inoculated than were sacrificed to allow for attrition). Virus titers were determined by plaque assays in DF1 cells. Values represent averages of the results from three independent plaque assay experiments. (B) Two-week-old chickens in groups of 10 were inoculated with 106 PFU of virus per bird and observed for 10 days for signs of disease and for mortality. Note that all of the birds survived in the rBC, rNg1, rNg2, rNg3, rNg4, and rNg5 groups. Significant differences are indicated by an asterisk (P < 0.05).
Host immune responses following N-glycosylation mutant virus infection.
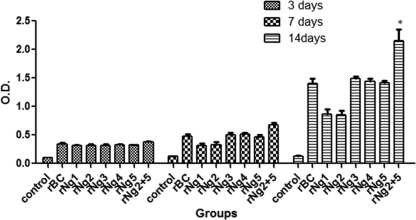
N-glycosylation of viral proteins can influence immunogenicity. In order to examine the effect of loss of N-linked glycans from the F protein on the immune response to NDV, 4-week-old chickens in groups of 5 were inoculated via the occulonasal route with 106 PFU of wild-type and mutant viruses per bird. Sera were collected on days 3, 7, and 14 p.i., and antibody levels were measured by an NDV-specific ELISA. As shown in Fig. 6, there were no significant differences in the total NDV-specific serum antibody responses elicited by wild-type rBC virus versus the mutant viruses on the 3rd p.i. On the 7th day p.i., chickens inoculated with the rNg2 + 5 virus exhibited slightly higher antibody titers than the other groups, and on the 14th day p.i. there was a significantly higher mean antibody titer in the rNg2 + 5 group compared to the other groups, including the wild-type rBC group. This correlates with our earlier findings indicating that increased replication of mutant virus rNg2 + 5 resulted in enhanced antibody production.
Fig 6.
NDV-specific serum antibody responses in chickens infected with wild-type rBC and the N-glycosylation mutants. Four-week-old chickens in groups of 5 were inoculated with 106 PFU of virus per bird via the occulonasal route. Sera were collected on days 3, 7, and 14 p.i. and analyzed by an NDV-specific ELISA. Data represent mean absorbance values ± standard deviations. *, the mean value for the rNg2 + 5 group was taken for 3 animals because 2 birds died by day 14 and were not included in the analysis. P values were <0.0001.
DISCUSSION
N-glycosylation has been shown to have a key role in viral glycoprotein folding, proteolytic processing, and function and also has been shown to influence viral infectivity and tropism and the immune response (1, 12, 14, 30, 33, 35, 37). In the present study, we examined the role of N-glycosylation of the NDV-BC F glycoprotein in the context of infectious virus by using reverse genetics to construct mutants that were then analyzed in cell culture and, importantly, in the natural chicken host by the use of standard pathogenicity tests in eggs and 1-day-old chicks, as well as by inoculation of 2-week-old and 4-week-old chickens by the oculonasal route to mimic natural infection. Analysis of N-glycosylation site usage in NDV-BC F proteins showed that five of the six potential N-glycosylation acceptor sites are utilized, one in the F2 subunit and four in the F1 subunit. Previously, it was reported that the sixth N-glycosylation site of NDV strain AV, which corresponds to site 541 (Ng6) in NDV-BC and is located in the cytoplasmic domain in both strains, was not utilized as an acceptor site for N-linked glycosylation (33). In the present study, we were unable to recover virus bearing the N541Q mutation, and the deleterious effect of this mutation was confirmed by the ability to rescue virus in which the assignment had been restored to that of wild-type virus. Taken together, these data suggest that this site probably does not normally contain a sugar side chain, which would be consistent with its location in the cytoplasmic domain, but that the assignment of N at position 541 is important for some function(s) of the cytoplasmic tail that is essential for virus replication. It was of particular interest that both previous and present studies indicated that sites Ng2 and Ng5 are utilized for N-glycosylation, since these sites are located in HR1 and HR2, respectively, and thus have the potential to affect fusion.
One of the important functions of N-glycans in glycoproteins is to facilitate protein processing and folding (13). Our results showed that deletion of single or multiple N-glycans in the F glycoprotein in the context of whole virus had little effect on cell surface expression of the F protein. The results from the present study are similar to the findings reported previously for the respiratory syncytial virus F protein, where deletion of multiple N-glycans did not affect F protein transportation to the cell surface (9, 52). These results suggest that no single N-glycan (nor Ng2 and Ng5 together) was essential for NDV-BC F protein transport to the cell surface. In addition, none of the mutations significantly affected the efficiency of F protein cleavage. Biophysical and crystallographic studies of several paramyxovirus F proteins have revealed that the F protein is present in the virus particle in a metastable state that, upon viral contact with the target cell, undergoes a conformational shift to insert the fusion peptide present at the N terminus of the F1 subunit into the target membrane. The F protein then makes the transition to a postfusion structure driven by association of HR1 with HR2, which brings the transmembrane domain and fusion peptide into close proximity, resulting in the merger of viral and host cell membranes. Thus, one of the important phases of the fusion process is the formation of a coiled coil triple strand by the HRs, which is a common structural feature of the paramyxovirus, orthomyxovirus, and retrovirus fusion proteins (16, 23, 32). The presence of N-glycan side chains in HR1 and HR2 thus might influence the conformational changes involved in the fusion process. Our fusion index assay of single N-glycan mutants showed that there were no major differences in fusion activity compared to wild-type rBC. Interestingly, in the present study, while the individual removal of the N-linked site from HR1 or HR2 had little effect on fusion, the removal of both sites in rNg2 + 5 mutant virus resulted in a hyperfusogenic phenotype. This result has some similarity to those of a previous study with Nipah virus in which the removal of multiple glycans from the Nipah virus F protein resulted in a hyperfusogenic phenotype (1). It was suggested that the presence of N-glycans on the Nipah virus F protein decreases the rate of six-helix bundle formation, resulting in slower fusion kinetics. Similarly, for NDV, it may be that the presence of the N-linked glycans in HR1 and HR2 delays or otherwise reduces association between HR1 and HR2, resulting in reduced fusion. The more interesting finding was that, while the single mutations at sites Ng2 and Ng5 were somewhat inhibitory to growth individually in vitro, in combination they resulted in faster growth and a dramatic 2.5 log10 increase in viral titer. This presumably was primarily due to the increase in fusion, which may have increased the efficiency and rate of infection as well as cell-to-cell spread by fusion. Evaluation of the pathogenicity of the N-glycan mutants in vivo provided results consistent with the in vitro growth study. The rNg1 and rNg2 mutants (and, to a lesser extent, the rNg5 mutant) were the most attenuated based on the standard MDT and ICPI tests. Similarly, in 2-week-old chickens, the rNg1, rNg2, and rNg5 mutants were the most attenuated based on tissue tropism and the magnitude of virus replication. Interestingly, while the effects of the Ng2 and Ng5 mutations were modestly attenuating on their own, when added together they resulted in a virus that replicated to substantially higher titers in every sampled tissue, was more virulent in the MDT and ICPI assays, and converted NDV-BC from a nonlethal virus into one that killed all of the inoculated 2-week-old chickens within 6 days. A similar observation was reported earlier for neurovirulent influenza virus strain A/WSN/33 in mice (28, 45) and H5N2 influenza virus in chickens (18): in both cases, loss of carbohydrate from the HA gene increased the virulence of the virus. In the case of influenza virus, a suggested mechanism for this increased virulence was that the loss of carbohydrate resulted in improved accessibility of the receptor-binding site to cellular receptors. In the case of NDV, in which the attachment function is on the HN protein, the situation is probably different. Instead, this effect probably reflects the increased fusogenic nature of the F protein, which likely increases the efficiency and rate of infection in the various tissues.
The oligosaccharide chains on the glycoproteins of many viruses play an important role in altering immune responses. They may form a barrier that shields viruses from immune recognition (27, 29, 46). Conversely, deletion of some N-glycans in the glycoprotein of human immunodeficiency virus abrogated the in vivo priming of T cell recognition for a nearby epitope, indicating that carbohydrate side chains can also increase immunogenicity (41). Our study showed that the double-mutant rNg2 + 5 virus elicited the highest NDV-specific serum antibody response whereas the attenuated rNg1 and rNg2 viruses had the lowest antibody responses, as measured by ELISA. We did not extend the study beyond 14 days p.i. because of the morbidity and mortality of the chickens in the rNg2 + 5 group. It seems likely that the increased immune response was primarily due to the increased level of viral replication, which provided more antigenic stimulation. It is also possible that other factors were involved, such as greater exposure of epitopes due the loss of shielding glycans or improved antigen processing. This might be investigated in further work by comparing the immunogenicity of the rNg2 + 5 mutant to that of wild-type BC by the use of UV-inactivated virus, where differences in viral replication would not be a factor.
In summary, the present report demonstrates the impact of N-glycosylation of the F protein on NDV pathogenesis and virulence in chickens. The most striking finding was that, whereas the individual removal of site Ng2 or Ng5 in HR1 and HR2 was modestly attenuating, removal of both in combination resulted in a hyperfusogenic phenotype that was associated with increased replication in vitro and in vivo and converted a mesogenic strain into a velogenic strain. The simplest explanation is that the presence of N-glycans on both HR1 and HR2 normally impedes the conformational shifts in the F protein during the fusion process and thus in effect reduces the efficiency of fusion. The crystal structure of NDV F as published so far does not give a clear view of how the N-glycans have been decorated in the F protein. It is difficult to determine whether the N-glycan orientation affects the fusion process at all or whether N-glyans are responsible for any structural instability in the transition from the prefusion to the postfusion state, thus maintaining different energy states, or are interacting with some other host molecules. Previously, a hyperfusogenic phenotype was also observed with mutants of the F protein of parainfluenza virus 5 (previously called simian virus 5) in which the fusion peptide was modified by glycine-to-alanine substitutions, suggesting that the native glycine residues serve to reduce the efficiency of fusion (15). Wild-type Sendai virus also downregulates its fusion activity, in this case due to a difference in a transcription gene start signal that results in reduced F gene transcription and protein expression; correction of this difference results in a virus that replicates more efficiently and is more lethal (17). A number of other paramyxoviruses also downregulate F expression (5, 40, 42). The idea that paramyxoviruses contain structural elements that reduce the efficiency of fusion suggests that this is advantageous to the virus. The results of the present study, as well as those of the previous study performed with Sendai virus, indicate that a hyperfusogenic phenotype can be associated with increased virulence and rapid death. It may be that reducing the severity of disease and prolonging the survival of the infected host can increase the opportunity for viral spread.
ACKNOWLEDGMENTS
This research was supported by NIAID contract no. N01A060009 (85% support) and NIAID, NIH Intramural Research Program (15% support).
The views expressed herein do not necessarily reflect the official policies of the Department of Health and Human Services; neither does mention of trade names, commercial practices, or organizations imply endorsement by the U.S. government.
Footnotes
Published ahead of print 28 December 2011
REFERENCES
- 1. Aguilar HC, et al. 2006. N-glycans on Nipah virus fusion protein protect against neutralization but reduce membrane fusion and viral entry. J. Virol. 80:4878–4889 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Alexander DJ. 1997. Newcastle disease and other avian Paramyxoviridae infection, p 541–569 In Calnek BQ. (ed), Diseases of poultry, 10th ed Iowa State University Press, Ames, IA [Google Scholar]
- 3. Bagai S, Lamb RA. 1995. Individual roles of N-linked oligosaccharide chains in intracellular transport of the paramyxovirus SV5 fusion protein. Virology 209:250–256 [DOI] [PubMed] [Google Scholar]
- 4. Baker KA, Dutch RE, Lamb RA, Jardetzky TS. 1999. Structural basis for paramyxovirus-mediated membrane fusion. Mol. Cell 3:309–319 [DOI] [PubMed] [Google Scholar]
- 5. Bousse T, et al. 2002. The long noncoding region of the human parainfluenza virus type 1 f gene contributes to the read-through transcription at the m-f gene junction. J. Virol. 76:8244–8251 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Braakman I, van Anken E. 2000. Folding of viral envelope glycoproteins in the endoplasmic reticulum. Traffic 1:533–539 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Chambers P, Millar NS, Platt SG, Emmerson PT. 1986. Nucleotide sequence of the gene encoding the matrix protein of Newcastle disease virus. Nucleic Acids Res. 14:9051–9061 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Chen L, et al. 2001. The structure of the fusion glycoprotein of Newcastle disease virus suggests a novel paradigm for the molecular mechanism of membrane fusion. Structure 9:255–266 [DOI] [PubMed] [Google Scholar]
- 9. Collins PL, Mottet G. 1991. Post-translational processing and oligomerization of the fusion glycoprotein of human respiratory syncytial virus. J. Gen. Virol. 72(Pt. 12):3095–3101 [DOI] [PubMed] [Google Scholar]
- 10. de Leeuw O, Peeters B. 1999. Complete nucleotide sequence of Newcastle disease virus: evidence for the existence of a new genus within the subfamily Paramyxovirinae. J. Gen. Virol. 80(Pt. 1):131–136 [DOI] [PubMed] [Google Scholar]
- 11. Doms RW, Lamb RA, Rose JK, Helenius A. 1993. Folding and assembly of viral membrane proteins. Virology 193:545–562 [DOI] [PubMed] [Google Scholar]
- 12. Eichler R, Lenz O, Garten W, Strecker T. 2006. The role of single N-glycans in proteolytic processing and cell surface transport of the Lassa virus glycoprotein GP-C. Virol. J. 3:41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Ellgaard L, Molinari M, Helenius A. 1999. Setting the standards: quality control in the secretory pathway. Science 286:1882–1888 [DOI] [PubMed] [Google Scholar]
- 14. Goffard A, Dubuisson J. 2003. Glycosylation of hepatitis C virus envelope proteins. Biochimie 85:295–301 [DOI] [PubMed] [Google Scholar]
- 15. Horvath CM, Lamb RA. 1992. Studies on the fusion peptide of a paramyxovirus fusion glycoprotein: roles of conserved residues in cell fusion. J. Virol. 66:2443–2455 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Joshi SB, Dutch RE, Lamb RA. 1998. A core trimer of the paramyxovirus fusion protein: parallels to influenza virus hemagglutinin and HIV-1 gp41. Virology 248:20–34 [DOI] [PubMed] [Google Scholar]
- 17. Kato A, et al. 1999. Sendai virus gene start signals are not equivalent in reinitiation capacity: moderation at the fusion protein gene. J. Virol. 73:9237–9246 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Kawaoka Y, Naeve CW, Webster RG. 1984. Is virulence of H5N2 influenza viruses in chickens associated with loss of carbohydrate from the hemagglutinin? Virology 139:303–316 [DOI] [PubMed] [Google Scholar]
- 19. Kniskern PJ, et al. 1994. Characterization and evaluation of a recombinant hepatitis B vaccine expressed in yeast defective for N-linked hyperglycosylation. Vaccine 12:1021–1025 [DOI] [PubMed] [Google Scholar]
- 20. Kohn A. 1965. Polykaryocytosis induced by Newcastle disease virus in monolayers of animal cells. Virology 26:228–245 [DOI] [PubMed] [Google Scholar]
- 21. Krishnamurthy S, Huang Z, Samal SK. 2000. Recovery of a virulent strain of newcastle disease virus from cloned cDNA: expression of a foreign gene results in growth retardation and attenuation. Virology 278:168–182 [DOI] [PubMed] [Google Scholar]
- 22. Krishnamurthy S, Samal SK. 1998. Nucleotide sequences of the trailer, nucleocapsid protein gene and intergenic regions of Newcastle disease virus strain Beaudette C and completion of the entire genome sequence. J. Gen. Virol. 79(Pt. 10):2419–2424 [DOI] [PubMed] [Google Scholar]
- 23. Lamb RA. 1993. Paramyxovirus fusion: a hypothesis for changes. Virology 197:1–11 [DOI] [PubMed] [Google Scholar]
- 24. Lamb RA, Parks GD. 2007. Paramyxoviridae: the viruses and their replication, p 1449–1496 In Knipe DM, et al. (ed), Fields virology, 5th ed, vol 1 Lippinicott Williams & Wilkins, Philadelphia, PA [Google Scholar]
- 25. Lamb RA, Jardetzky TS. 2007. Structural basis of viral invasion: lessons from paramyxovirus F. Curr. Opin. Struct. Biol. 17:427–436 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Lamb RA, Paterson RG, Jardetzky TS. 2006. Paramyxovirus membrane fusion: lessons from the F and HN atomic structures. Virology 344:30–37 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Lee J, Park JS, Moon JY, Kim KY, Moon HM. 2003. The influence of glycosylation on secretion, stability, and immunogenicity of recombinant HBV pre-S antigen synthesized in Saccharomyces cerevisiae. Biochem. Biophys. Res. Commun. 303:427–432 [DOI] [PubMed] [Google Scholar]
- 28. Li S, Schulman J, Itamura S, Palese P. 1993. Glycosylation of neuraminidase determines the neurovirulence of influenza A/WSN/33 virus. J. Virol. 67:6667–6673 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Li Y, et al. 2008. Removal of a single N-linked glycan in human immunodeficiency virus type 1 gp120 results in an enhanced ability to induce neutralizing antibody responses. J. Virol. 82:638–651 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Lin G, et al. 2003. Differential N-linked glycosylation of human immunodeficiency virus and Ebola virus envelope glycoproteins modulates interactions with DC-SIGN and DC-SIGNR. J. Virol. 77:1337–1346 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Luque LE, Russell CJ. 2007. Spring-loaded heptad repeat residues regulate the expression and activation of paramyxovirus fusion protein. J. Virol. 81:3130–3141 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Matthews JM, Young TF, Tucker SP, Mackay JP. 2000. The core of the respiratory syncytial virus fusion protein is a trimeric coiled coil. J. Virol. 74:5911–5920 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. McGinnes L, Sergel T, Reitter J, Morrison T. 2001. Carbohydrate modifications of the NDV fusion protein heptad repeat domains influence maturation and fusion activity. Virology 283:332–342 [DOI] [PubMed] [Google Scholar]
- 34. Nagai Y, Hamaguchi M, Toyoda T. 1989. Molecular biology of Newcastle disease virus. Prog. Vet. Microbiol. Immunol. 5:16–64 [PubMed] [Google Scholar]
- 35. Oostra M, de Haan CA, de Groot RJ, Rottier PJ. 2006. Glycosylation of the severe acute respiratory syndrome coronavirus triple-spanning membrane proteins 3a and M. J. Virol. 80:2326–2336 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Paldurai A, Kumar S, Nayak B, Samal SK. 2010. Complete genome sequence of highly virulent neurotropic Newcastle disease virus strain Texas GB. Virus Genes 41:67–72 [DOI] [PubMed] [Google Scholar]
- 37. Panda A, Elankumaran S, Krishnamurthy S, Huang Z, Samal SK. 2004. Loss of N-linked glycosylation from the hemagglutinin-neuraminidase protein alters virulence of Newcastle disease virus. J. Virol. 78:4965–4975 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Phillips RJ, Samson AC, Emmerson PT. 1998. Nucleotide sequence of the 5′ terminus of Newcastle disease virus and assembly of the complete genomic sequence: agreement with the “rule of six. ” Arch. Virol. 143:1993–2002 [DOI] [PubMed] [Google Scholar]
- 39. Lamb R, et al. 2005. The negative sense single stranded RNA viruses, p 607–738 In Fauquet CM, Mayo MA, Maniloff J, Desselberg U, Ball LA. (ed), Virus taxonomy. 8th Report of the International Committee on Taxonomy of Viruses. Elsevier Academic Press, San Diego, CA [Google Scholar]
- 40. Rassa JC, Parks GD. 1998. Molecular basis for naturally occurring elevated readthrough transcription across the M-F junction of the paramyxovirus SV5. Virology 247:274–286 [DOI] [PubMed] [Google Scholar]
- 41. Sjölander S, et al. 1996. N-linked glycans in the CD4-binding domain of human immunodeficiency virus type 1 envelope glycoprotein gp160 are essential for the in vivo priming of T cells recognizing an epitope located in their vicinity. Virology 215:124–133 [DOI] [PubMed] [Google Scholar]
- 42. Spriggs MK, Collins PL. 1986. Human parainfluenza virus type 3: messenger RNAs, polypeptide coding assignments, intergenic sequences, and genetic map. J. Virol. 59:646–654 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Swanson K, et al. 2010. Structure of the Newcastle disease virus F protein in the post-fusion conformation. Virology 402:372–379 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Vigerust DJ, et al. 2007. N-linked glycosylation attenuates H3N2 influenza viruses. J. Virol. 81:8593–8600 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Ward AC, de Koning-Ward TF. 1995. Changes in the hemagglutinin gene of the neurovirulent influenza virus strain A/NWS/33. Virus Genes 10:179–183 [DOI] [PubMed] [Google Scholar]
- 46. Wei X, et al. 2003. Antibody neutralization and escape by HIV-1. Nature 422:307–312 [DOI] [PubMed] [Google Scholar]
- 47. Wilde A, McQuain C, Morrison T. 1986. Identification of the sequence content of four polycistronic transcripts synthesized in Newcastle disease virus infected cells. Virus Res. 5:77–95 [DOI] [PubMed] [Google Scholar]
- 48. Yin HS, Wen X, Paterson RG, Lamb RA, Jardetzky TS. 2006. Structure of the parainfluenza virus 5 F protein in its metastable, prefusion conformation. Nature 439:38–44 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Yu M, et al. 2002. Six-helix bundle assembly and characterization of heptad repeat regions from the F protein of Newcastle disease virus. J. Gen. Virol. 83:623–629 [DOI] [PubMed] [Google Scholar]
- 50. Zhu J, et al. 2003. Crystallization and preliminary X-ray crystallographic analysis of the trimer core from measles virus fusion protein. Acta Crystallogr. D Biol. Crystallogr. 59:587–590 [DOI] [PubMed] [Google Scholar]
- 51. Zhu J, et al. 2003. Design and analysis of post-fusion 6-helix bundle of heptad repeat regions from Newcastle disease virus F protein. Protein Eng. 16:373–379 [DOI] [PubMed] [Google Scholar]
- 52. Zimmer G, Trotz I, Herrler G. 2001. N-glycans of F protein differentially affect fusion activity of human respiratory syncytial virus. J. Virol. 75:4744–4751 [DOI] [PMC free article] [PubMed] [Google Scholar]