Abstract
Highly pathogenic avian influenza (HPAI) viruses of the H5 and H7 subtypes typically possess multiple basic amino acids around the cleavage site (MBS) of their hemagglutinin (HA) protein, a recognized virulence motif in poultry. To determine the importance of the H5 HA MBS as a virulence factor in mammals, recombinant wild-type HPAI A/Vietnam/1203/2004 (H5N1) viruses that possessed (H5N1) or lacked (ΔH5N1) the H5 HA MBS were generated and evaluated for their virulence in BALB/c mice, ferrets, and African green monkeys (AGMs) (Chlorocebus aethiops). The presence of the H5 HA MBS was associated with lethality, significantly higher virus titers in the respiratory tract, virus dissemination to extrapulmonary organs, lymphopenia, significantly elevated levels of proinflammatory cytokines and chemokines, and inflammation in the lungs of mice and ferrets. In AGMs, neither H5N1 nor ΔH5N1 virus was lethal and neither caused clinical symptoms. The H5 HA MBS was associated with mild enhancement of replication and delayed virus clearance. Thus, the contribution of H5 HA MBS to the virulence of the HPAI H5N1 virus varies among mammalian hosts and is most significant in mice and ferrets and less remarkable in nonhuman primates.
INTRODUCTION
The sporadic transmission of highly pathogenic avian influenza (HPAI) H5N1 viruses from domestic poultry to humans in many parts of the world highlights the threat that these viruses pose to public health from their potential to cause another pandemic. More than 500 laboratory-confirmed HPAI H5N1 infections have been recorded since 2003 in 15 countries, with a case-fatality rate of nearly 60% (54). Most of these infections can be traced to direct exposure to diseased poultry; human-to-human transmission of the H5N1 virus remains limited to small family clusters (20, 50). To date, the gene compositions of the H5N1 viruses isolated from infected humans have remained wholly avian in origin and are poorly transmitted among individuals, in contrast to the efficient transmission displayed by the swine-origin influenza A H1N1 pandemic virus that has infected millions worldwide. As the HPAI H5N1 viruses are now endemic in many bird species in Asia (9), there are concerns that these viruses may become easily transmissible among individuals through genetic reassortment with a human influenza virus or through adaptation in an intermediate host. Understanding the basis of the virulence of HPAI H5N1 viruses in humans therefore remains a priority.
Although several virus genes and gene products contribute to the pathogenicity of HPAI H5N1 viruses (8, 10, 15, 19), the cleavability of the hemagglutinin (HA) protein and the distribution of HA-activating proteases in the host are recognized as major virulence factors (6, 17, 40). The HA0 precursor protein undergoes posttranslational cleavage into two subunits, HA1 and HA2, to facilitate the fusion of the viral and cellular membranes (25, 27, 53). The amino acid sequence upstream of the HA cleavage site as well as the presence or absence of a vicinal carbohydrate side chain is believed to regulate HA cleavability (23, 24). Most of the low-pathogenicity influenza A viruses contain a single arginine residue at the HA cleavage site. These HAs are cleaved by extracellular trypsin-like serine proteases secreted by nonciliated cells of the respiratory epithelium in humans and gastrointestinal tract of birds, resulting in local infections (32). Some HPAI viruses of the H5 and H7 subtypes, on the other hand, contain multiple basic amino acids around the cleavage site (MBS) of the HA molecule (5) that can act as a recognition motif for subtilisin-like proteases that recognize polybasic motifs (39). The ubiquitous distribution of intracellular proteases such as furin (41) and PC6 (18) contributes to the propensity of HPAI viruses with the MBS motif to disseminate and replicate in extrapulmonary organs of birds, thereby expanding the range of tissues that they can infect. While the role of MBS as a virulence motif in poultry is well established, the influence of MBS on the virulence of HPAI viruses in mammals remains unknown and is the focus of this study.
In addition to the local expression of the proteases that activate the HA, tissue tropism also plays a major role in the pathogenesis and host-range restriction displayed by influenza A viruses. Because human and avian influenza viruses differ in their binding preference to terminal sialic acids (SA) on host cells, the type and distribution of these residues on cells of the respiratory and gastrointestinal tracts are associated with the susceptibility of different hosts to influenza A virus infection (45). van Riel and colleagues (2007) reported that human influenza viruses attach to cells in the human trachea, bronchi, and type I pneumocytes in the alveoli while H5 avian influenza viruses preferentially target cells in the bronchioles, type II pneumocytes, and alveolar macrophages in the alveoli (51). The authors speculated that the pattern of virus attachment to the cells of the human respiratory tract may contribute to differences in the severity and localization of disease induced by human and avian influenza viruses. However, receptor binding preference is still insufficient to predict the severity of disease outcome induced by H5N1 viruses, as both low-pathogenicity and HPAI H5N1 viruses target the same types of cells (51). Intriguingly, H5N1 viruses could infect and productively replicate in human nasopharyngeal and oropharyngeal tissues ex vivo despite the absence of detectable α2,3-SA receptors on these cells (30). These findings suggest that alternative, as-yet-unidentified receptors may mediate virus entry into the cells of the human upper respiratory tract and that H5N1 disease severity is not totally dependent on the predicted tropism of the virus for tissues of the lower respiratory tract (30).
Data from clinical observations and limited autopsies conducted on fatal cases of human H5N1 infection suggest that extensive virus replication, systemic spread, and the induction of an intense inflammatory response may all contribute to the pathogenesis of H5N1 influenza (11). The intense inflammatory response has been implicated in the development of acute respiratory distress syndrome (3) which in turn is the leading cause of death among patients infected with the H5N1 virus. Gaining a better understanding of the virulence determinants of HPAI H5N1 viruses in mammalian models would provide significant insights on developing effective intervention and therapeutic strategies that could improve the clinical management of the disease in humans. In this study, we examined the role of the MBS in the H5 HA of the HPAI A/Vietnam/1203/2004 (H5N1) virus on its virulence in BALB/c mice, ferrets, and African green monkeys (AGMs; Chlorocebus aethiops).
MATERIALS AND METHODS
Recombinant viruses.
The removal of the MBS from the H5 HA gene of the H5N1 wild-type (wt) virus, as well as the rescue of recombinant H5N1 and ΔH5N1 viruses by reverse genetics, was previously described (43). Briefly, a coculture of Madin-Darby canine kidney (MDCK) cells and 293T cells was transfected with the plasmids that carry the eight gene segments of the desired influenza virus by lipofection. Virus stocks were cloned and amplified in specific-pathogen-free eggs, and the sequences of all gene segments were verified to be identical to the plasmids used in the transfection by reverse transcription-PCR (RT-PCR). All experiments involving the recombinant H5N1 wt viruses, including animal studies, were conducted using enhanced containment procedures in biosafety level 3 (BSL3) facilities approved for use by the U.S. Department of Agriculture and the Centers for Disease Control and Prevention. All animal studies were approved by the National Institutes of Health Animal Care and Use Committee.
Virus replication in vitro.
Confluent monolayer cultures of MDCK cells in 6-well plates were infected with either the H5N1 or the ΔH5N1 virus at a multiplicity of infection of 0.001 in triplicate. Culture supernatants were collected at 12-h intervals up to 72 h and stored frozen at −80°C prior to virus titration on MDCK cells.
Virus replication and pathogenicity studies in mice.
To determine the ability of the viruses to replicate in different organs of mice, groups of 6- to 8-week-old female BALB/c mice (Taconic, Germantown, NY) were lightly anesthetized and infected intranasally (i.n.) with 125 50% tissue culture infectious doses (TCID50) of either the H5N1 (equivalent to 50× 50% mouse lethal dose [MLD50]) or ΔH5N1 virus in 50 μl. Four mice from each group were sacrificed on days 2, 4, 6, and 8 postinfection (p.i.). However, organs were collected only on days 2, 4, and 6 p.i. from mice that were infected with the H5N1 virus since all remaining animals succumbed to infection by day 7 p.i. Virus titers in nasal turbinates, lungs, spleen, and brain were determined in MDCK cells and expressed as TCID50/g of tissue as previously described (44).
The concentration of cytokines and chemokines induced by either the H5N1 or ΔH5N1 virus was measured in clarified lung tissue homogenates by suspension array technology using the Bio-Plex Pro mouse cytokine 23-plex assay kit system (Bio-Rad, Hercules, CA) according to the manufacturer's instructions.
To assess the impact of the H5 HA MBS on the population of circulating white blood cells (WBC) in mice, groups of 3 mice were infected i.n. with 125 TCID50 of either the H5N1 or ΔH5N1 virus. An additional group of animals served as mock-infected controls and received 50 μl of L15 medium. Whole-blood samples were collected daily from the tail of mice until day 5 p.i. Differential WBC counts were determined by preparing thin blood smears, staining the slides with the Hema-3 system stain (Fisher Scientific), and calculating the percentage of each WBC type per 100 WBCs counted under an oil-immersion objective.
To evaluate the pathology induced by the H5N1 viruses in the lungs, sections were prepared from formalin-fixed, paraffin-embedded tissues and then stained with hematoxylin and eosin. The sections were analyzed for pathological changes by a pathologist who was unaware of the inoculum administered to each mouse.
Virus replication in ferrets.
Groups of nine 6-month-old male ferrets (Triple F Farms, Pennsylvania) were infected i.n. with 107 TCID50 of the biological (b) or reverse-genetics-derived (r) H5N1 or ΔH5N1 virus. Three animals from each group were euthanized on days 3 and 6 p.i., and virus titers were determined in the nasal turbinates, lungs, and brain as previously described. A section of the right lung was examined for histopathologic changes. The remaining 3 ferrets in each group were followed for clinical observations, including weight and temperature monitoring, for 14 days (44).
Measurement of ferret cytokine mRNAs by real-time PCR.
Whole-blood samples from ferrets infected with bH5N1, rH5N1, and ΔH5N1 virus were collected in PaxGene blood RNA tubes (Qiagen, Gaithersburg, MD) before infection (day 0) and on day 3 p.i. The blood samples were processed, and total RNA was isolated according to the manufacturer's instructions. Total RNA from nasal washes from the same ferrets was isolated using the QIAmp viral RNA minikit (Qiagen, Gaithersburg, MD). RNA quantities for each sample were determined using a Nanodrop 2000C spectrophotometer (Thermo Scientific), and the concentrations were normalized by dilution in nuclease-free water. RNA samples were reverse transcribed using a QuantiTect reverse transcription kit (Qiagen) in 20-μl reaction volumes containing 200 ng total RNA. A single aliquot of each cDNA sample was preamplified with PCR primers corresponding to alpha interferon (IFN-α), MX-1, interleukin-2 (IL-2), IFN-β, IL-6, IL-4, IFN-γ, IL-8, tumor necrosis factor alpha (TNF-α), OAS-1, MIG-1, IL-10, ISG-15, IL-5, IL-12, RIG-1, CXCL10, IL-1β, RANTES, and the glyceraldehyde-3-phosphate dehydrogenase (GAPDH) housekeeping gene in a 10-μl reaction volume using a TaqMan PreAmp Master Mix kit (Applied Biosystems) according to the manufacturer's protocol. Following preamplification, the samples were diluted 1:5 (vol/vol) in Tris-EDTA (TE) buffer, pH 8.0.
Custom-designed primers and TaqMan 6-carboxyfluorescein (FAM)–6-carboxytetramethylrhodamine (TAMRA) probes for each gene were supplied by Applied Biosystems, and 20× assay mixes were prepared containing 18 μM primers and 5 μM probe (final concentration of 900 nM [each] primer and 250 nM [each] probe). Fluidigm BioMark 48-by-48 arrays were prepared according to the manufacturer's instructions. Briefly, 20× assay mixes were diluted 1:1 (vol/vol) with DA assay loading reagent (Fluidigm, South San Francisco, CA) and 5 μl was added to duplicate assay inlets of the array. Five microliters of each sample reaction mix was prepared by mixing 2× TaqMan Universal Mastermix (Applied Biosystems), DA sample loading reagent, and 2.25 μl of sample cDNA. The sample mixes were loaded in duplicate per the manufacturer's recommendations, resulting in 4 quantitative PCR (qPCR) mixtures for each sample. After loading, PCR was performed under the following reaction conditions: 50°C for 2 min and 95°C for 10 min, followed by 40 cycles of 95°C for 15 s and 60°C for 1 min. Data were processed using an automatic detector threshold setting, linear baseline correction, and a quality threshold setting of 0.65 using the Fluidigm real-time PCR analysis software. The mean for the four replicate threshold cycle (CT) values of each ferret gene was determined and normalized relative to the mean CT value of the GAPDH housekeeping gene. Fold changes were calculated over baseline CT values represented by preinfection samples.
Virus replication in AGMs.
A total of 13 African green monkeys were used in the study which was conducted at Bioqual, Inc. (Rockville, MD). Two groups of 6 monkeys each were anesthetized and infected intratracheally and intranasally with 2 × 106 TCID50 of either the H5N1 or ΔH5N1 virus while one monkey was mock infected with L15 medium. Nasal and pharyngeal swabs, tracheal lavage samples, whole blood, and serum were collected from each monkey for virus titration, hematology, and cytokine analysis, respectively. The body weight and temperature of the monkeys were noted daily, and each animal was observed for clinical symptoms. The mock-infected animal was sacrificed together with two monkeys from each group on day 2 p.i., and from then on, 2 monkeys from each virus-infected group were sacrificed on days 4 and 7 p.i. Nasal turbinates, lungs, trachea, brain, liver, and spleen were sampled at necropsy for virus titration and pathological evaluation. Cytokine and chemokine measurements in AGM serum were conducted using the Bio-Plex Pro human cytokine 27-plex assay kit system (Bio-Rad, Hercules, CA) according to the manufacturer's instructions.
RESULTS
The influence of the H5 HA MBS on virus replication in vitro.
To determine the influence of the MBS of the H5 HA on replication of the H5N1 virus in vitro, cultures of MDCK cells supplemented with trypsin were infected with either the H5N1 virus or the H5N1 virus that lacks the MBS in its HA cleavage site (ΔH5N1) at a multiplicity of infection of 0.001. Virus titers were determined in culture supernatants collected at 12-hour intervals. The H5N1 virus consistently replicated to slightly higher titers than did the ΔH5N1 virus for the first 36 h, but the titers of the two viruses were comparable by 48 h p.i. (data not shown). Thus, the removal of the H5 HA MBS does not have a significant effect on the replication of the H5N1 virus in vitro.
Virus replication and pathogenicity in mice.
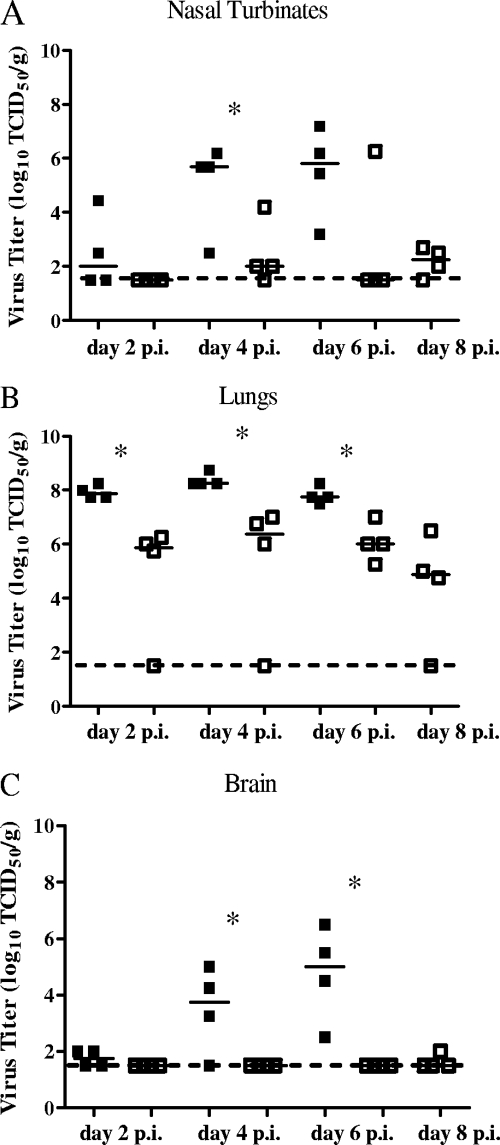
The H5 HA MBS was previously determined to be a virulence motif in mice—removal of the H5 HA MBS was sufficient to render the highly pathogenic H5N1 virus nonlethal to mice (15, 43). To evaluate whether the H5 HA MBS confers any replication advantage in vivo, groups of mice were infected with either the H5N1 or the ΔH5N1 virus and virus replication was determined in the respiratory and extrapulmonary organs at different time points postinfection. The ΔH5N1 virus replicated to about 100- to 1,000-fold-lower titers in the nasal turbinates and lungs of mice than did the H5N1 virus (Fig. 1A and B, respectively), suggesting that removal of the H5 HA MBS not only alleviates the lethality of the H5N1 virus (43) but is also associated with a significant reduction in the level of virus replication in the respiratory tract of mice. The H5 HA MBS was also associated with extrapulmonary virus dissemination in mice, as only the H5N1 virus replicated consistently in the brain (Fig. 1C). These results are consistent with our previous findings that in the context of the H5N1 wt virus genes, the MBS is a major virulence determinant in mice (43).
Fig 1.
H5 HA MBS and virus replication in mice. Groups of female BALB/c mice (n = 4/group) were infected with 125 TCID50 of either H5N1 (shaded symbols) or ΔH5N1 virus (open symbols) i.n., each symbol representing a discrete data point in each group. Nasal turbinates, lungs, and the brain were harvested on days 2, 4, 6, and 8 p.i. Horizontal bars represent the median virus titer, expressed as log10 TCID50/g of tissue. *, P < 0.05 by Mann-Whitney U test.
The H5 HA MBS and the cytokine response in the mouse lung.
Elevated levels of several proinflammatory cytokines and chemokines have been reported in mice following primary infection with HPAI H5N1 viruses (47, 49). As cytokine dysregulation has been suggested as one of the contributing factors for the extreme virulence of HPAI H5N1 viruses (11, 49), the cytokine and chemokine profiles elicited by the H5N1 and ΔH5N1 viruses in the lungs of mice infected with 125 TCID50 of either virus were evaluated using a multiplex cytokine bead array assay. The concentrations of the pleiotropic cytokine granulocyte colony-stimulating factor (G-CSF), as well as the proinflammatory cytokines IL-1α, IL-1β, and IL-12, were significantly higher in the lungs of mice infected with the H5N1 virus than in those infected with the ΔH5N1 virus, most notably on days 4 and 6 p.i. (Fig. 2). Concentrations of the cytokine IL-2, as well as those of TNF-α and IL-6, which were previously reported to be associated with HPAI H5N1 infection in mice (29, 49), were not detected in the lungs of mice infected with either virus, perhaps reflecting the use of different assay systems with differing sensitivities of detection for these cytokines. The concentrations of the chemokines monocyte chemoattractant protein 1 (MCP-1), MIP-1α, MIP-1β, RANTES, and KC (the murine equivalent of human IL-8) were also significantly higher in the H5N1 virus-infected group (Fig. 2). These chemokines are implicated in the recruitment of neutrophils and monocytes in the pulmonary tissues of mice that result in acute inflammation and severe lung pathology (31). The levels of the anti-inflammatory cytokine IL-10 were also elevated, likely the result of a negative feedback mechanism in response to the elevated levels of inflammatory cytokines in the local milieu.
Fig 2.
Cytokine and chemokine levels in the lungs of mice infected intranasally with the H5N1 or ΔH5N1 virus. Groups of female BALB/c mice (n = 4/group) were infected with 125 TCID50 of either H5N1 or ΔH5N1 virus i.n. Cytokines and chemokines were measured using a multiplex cytokine bead array assay kit on clarified lung homogenates from days 2, 4, 6, and 8 p.i. Cytokine concentrations are expressed as pg/ml. White bars represent mock-infected mice, gray bars represent ΔH5N1 virus-infected mice, and black bars represent H5N1 virus-infected mice. *, P < 0.05 by Mann-Whitney U test.
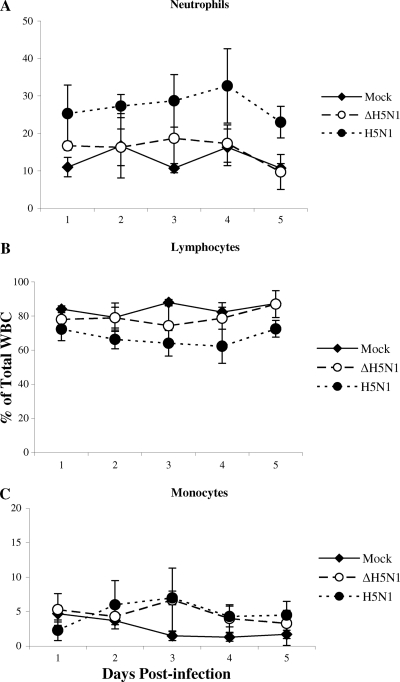
The H5 HA MBS is associated with lymphopenia in mice.
Tumpey et al. previously reported that an HPAI H5N1 infection caused lymphopenia in mice (49). To assess the impact of the H5 HA MBS on the leukocyte population in the peripheral blood, groups of mice were infected with either the H5N1 or ΔH5N1 virus while another group was mock infected with medium to serve as a control group. It is evident that mice infected with the H5N1 virus had a higher proportion of neutrophils (Fig. 3A) and monocytes (Fig. 3C) in the peripheral blood and a corresponding lower percentage of lymphocytes (Fig. 3B) than did mock-infected animals, as early as day 1 p.i. Animals infected with the ΔH5N1 virus exhibited a transient slight increase in the proportion of neutrophils (Fig. 3A) and a corresponding decrease in the proportion of lymphocytes (Fig. 3B) early in infection but displayed a WBC differential profile similar to that of the mock-infected group by day 4 p.i. Thus, the presence of the H5 HA MBS motif in the H5N1 virus resulted in an alteration of the leukocyte population in the peripheral blood of mice.
Fig 3.
The influence of the H5 HA MBS on leukocytes in the peripheral blood of mice. Groups of female BALB/c mice (n = 3/group) were infected i.n. with 125 TCID50 of either H5N1 or ΔH5N1 virus. WBC differential counts were performed on peripheral blood smears that were prepared daily from day 1 through day 5 p.i. The percentage of each WBC type was based on counting at least 100 WBCs under an oil-immersion objective.
The H5 HA MBS and mouse lung pathology.
Histopathological analysis of lung tissue sections from ΔH5N1-infected mice showed minimal to mild focal inflammation of the large airways by day 4 p.i. (Fig. 4A), progressing to moderate bronchial and bronchiolar inflammation with cuffing of airways by lymphocytes and neutrophils at day 6 (Fig. 4B). Inflammation was resolved and cleared by day 8 p.i. (data not shown). In contrast, there were significant multifocal to locally extensive inflammation and necrosis of the bronchial and bronchiolar epithelium, often accompanied by sloughing of the epithelium, in the lungs of H5N1-infected mice (Fig. 4D to F). Alveolar spaces contained pulmonary macrophages and neutrophils admixed with cellular debris. Thickening of the alveolar walls and various degrees of perivascular and peribronchiolar cuffing by lymphocytes, plasma cells, and neutrophils were also noted. Thus, removal of the H5 HA MBS resulted in a virus that caused mild inflammation, confined to the large airways in the lungs, that was less severe than the lung pathology caused by the H5N1 wt virus.
Fig 4.
Histopathological effects induced by the H5N1 virus in the lungs of mice. Formalin-fixed, paraffin-embedded lung tissue sections from ΔH5N1 virus (A and B)-, mock (C)-, or H5N1 virus (D, E, and F)-infected mice were stained with hematoxylin and eosin. Representative sections from tissues harvested on days 4 (A, C, and D) and 6 (B, E, and F) p.i. are shown. Lungs from H5N1 virus-infected mice had acute neutrophilic infiltrates and necrosis of the bronchial and bronchiolar epithelium (D and E) with considerable sloughing and attenuation of the bronchial lining epithelium, highlighted and magnified in panel F. Marked infiltration of the alveolar spaces with neutrophils was also apparent (E), with multifocal thickening and/or obliteration of alveolar walls. Lungs from ΔH5N1-infected mice were minimally affected at day 4 (A) and demonstrated mild to moderate neutrophilic infiltrate of the bronchial epithelium and variable peribronchiolar cuffing at day 6 (B).
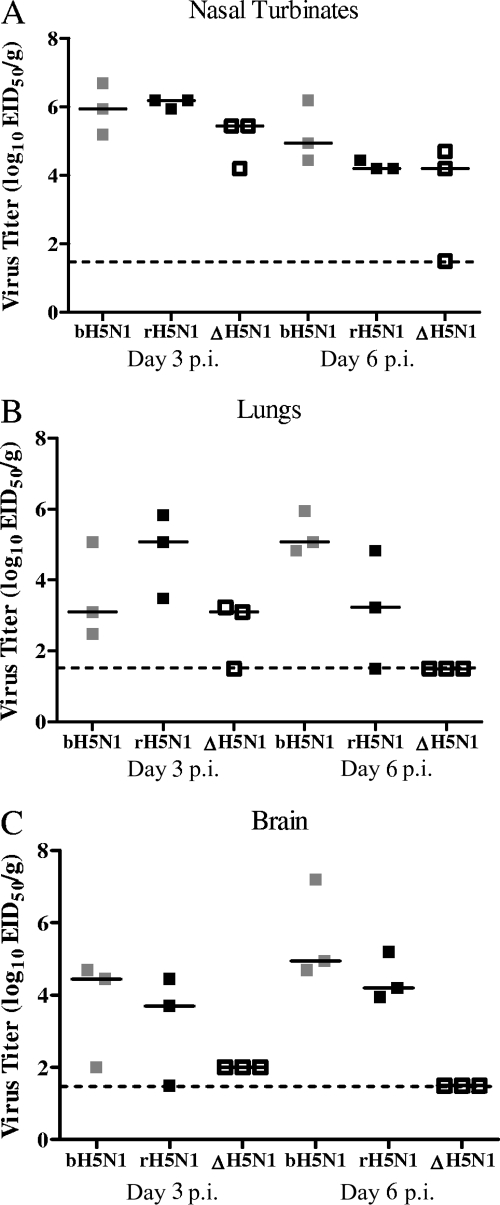
Virus replication in ferrets.
We next examined the relevance of the MBS to the virulence of H5N1 viruses in ferrets. The biological H5N1 (bH5N1) virus was included in this set of studies as a positive control. Only ferrets infected with the bH5N1 or rH5N1 virus displayed pronounced morbidity, as evidenced by elevated body temperatures, significant weight loss, and lethargy (data not shown). Moreover, bH5N1- and rH5N1-infected ferrets showed neurological symptoms such as hind limb paralysis, ataxia, and convulsions requiring euthanasia on day 6 and day 8 p.i., respectively. Ferrets infected with the ΔH5N1 virus showed no clinical signs of illness through 14 days p.i. The bH5N1, rH5N1, and ΔH5N1 viruses all replicated to similar mean titers in the upper respiratory tract of ferrets on days 3 and 6 p.i. (Fig. 5A). In the lungs, the rH5N1 virus replicated to higher titers than did the bH5N1 and ΔH5N1 viruses on day 3 p.i. (Fig. 5B), but on day 6 p.i., most of the ferrets infected with the rH5N1 and bH5N1 viruses continued to display robust virus replication while virus could no longer be detected in the lungs of ΔH5N1-infected ferrets. The bH5N1 and rH5N1 viruses consistently disseminated to and replicated in the brain while the replication of the ΔH5N1 virus in the brain was severely restricted (Fig. 5C). Lung histology findings within each animal and among each group ranged from normal to severe multifocal to locally extensive inflammation and necrosis of alveolar walls with infiltrates of neutrophils and macrophages in air spaces obliterating normal pulmonary architecture. There was no apparent correlation between the severity of histological findings and virus titer (data not shown). These results indicate that the MBS is a virulence determinant in ferrets as it is in mice; its removal from the H5N1 virus led to reduced virus replication in the lower respiratory tract, restricted the spread of the virus to extrapulmonary sites such as the brain, and was associated with significant reductions in mortality and morbidity.
Fig 5.
The H5N1 virus replicated in the respiratory tract and brain of ferrets. Groups of ferrets (n = 4/group) were infected with 106 TCID50 of either bH5N1 (gray squares), rH5N1 (black squares), or ΔH5N1 virus (white squares) i.n., each symbol representing a discrete data point in each group. Nasal turbinates (A), lungs (B), and the brain (C) were harvested on days 3 and 6 p.i. Horizontal bars represent the median virus titer, expressed as log10 TCID50/g of tissue.
The H5 HA MBS and cytokine response in ferrets.
The lack of quality reagents specific to ferret proteins has hindered the development of quantitative assays to determine the level of cytokines and chemokines induced by immunization or natural infection in ferrets. Instead, a quantitative real-time PCR (qPCR) was employed to measure the level of mRNA transcripts in the nasal wash and peripheral blood mononuclear cells (PBMCs) of ferrets infected with the different H5N1 viruses, similar to the approach taken by other investigators (7, 46). The low concentration of total RNA isolated from the nasal washes precluded their use for further analysis, and so we focused on the PBMC samples instead. For the most part, the bH5N1 and rH5N1 viruses induced similar cytokine patterns, eliciting dramatically high mRNA levels for CXCL10 and modest fold increases of the proinflammatory cytokine IL-12 and several interferon-related genes such as MIG-1, MX-1, OAS, and RIG-I (Fig. 6), while no significant fold differences in the mRNAs for IFN-α, IFN-β, or IFN-γ were observed (data not shown). There were also no significant differences observed in IL-4, IL-5, IL-6, IL-10, IL-8, RANTES, and TNF-α levels for any of the H5N1 viruses evaluated (data not shown).
Fig 6.
Influence of H5 HA MBS on cytokine responses in ferrets. Groups of ferrets (n = 3/group) were infected i.n. with 106 TCID50 of either bH5N1 (gray squares), rH5N1 (black squares), or ΔH5N1 virus (white squares). mRNA levels for various cytokines and immune-related genes from PBMCs isolated on day 3 p.i. were measured by qPCR. The average of 4 CT values for each gene was normalized relative to that of GAPDH, a housekeeping gene, and fold differences were calculated compared to preinfection levels of the same animals. Horizontal bars represent the median fold change difference for each group.
Virus replication and pathogenicity in AGMs.
The replication of the H5N1 and ΔH5N1 viruses was also evaluated in African green monkeys (AGMs; Chlorocebus aethiops), animals that are more anatomically and physiologically related to humans than are mice and ferrets. After 2 × 106 TCID50 of the H5N1 or ΔH5N1 virus was administered i.n. and intratracheally to AGMs, they were observed daily for evidence of clinical illness. Both viruses replicated to modest peak titers of ∼103 TCID50/g in nasopharyngeal swabs (Table 1). Virus replication was far more restricted in the nasal turbinate tissue (Table 1); replication of the ΔH5N1 virus was detected only on day 2 p.i. while the H5N1 virus was detected at a low level until day 7 p.i. (Table 1). Neither virus was detected in the tracheal lavage samples (data not shown), but both viruses replicated to moderately high titers in the lungs (Table 1). The H5N1 virus replicated to a slightly higher titer than did the ΔH5N1 virus in the lungs, and the H5N1 virus was detected in the lungs of AGMs through day 7 p.i., by which time the ΔH5N1 virus was undetectable. Interestingly, despite virus replication to about 104 TCID50/g in the lungs, none of the AGMs infected with the H5N1 virus experienced weight loss or displayed any clinical illness during the course of the study. There was also no apparent difference in the histopathological analyses of lung tissue sections of AGMs infected with the H5N1 or ΔH5N1 virus or in the cytokine profiles displayed by animals infected with either virus (data not shown). Thus, the only remarkable effect of the removal of the H5 HA MBS in AGMs was earlier clearance of the virus from the lungs. We were unable to assess the effect on extrapulmonary spread because the H5N1 virus did not spread to the liver, spleen, or brain.
Table 1.
The influence of the H5 HA MBS on the replication of the H5N1 virus in African green monkeysa
| Sample | Virus | Mean virus titer ± SE (log10 TCID50/ml org) in tissue samples collected on indicated day p.i.: |
||||
|---|---|---|---|---|---|---|
| Day 1 | Day 2 | Day 3 | Day 4 | Day 7 | ||
| Nasopharyngeal swab | H5N1 | 3.6 ± 0.5 | 2.6 ± 0.5 | 1.7 ± 0.7 | 1.6 ± 0.5 | 2.4 ± 0.9 |
| ΔH5N1 | 2.5 ± 0.8 | 1.8 ± 0.6 | 0.8 ± 0.1 | 1.4 ± 0.8 | 0.8 ± 0.3 | |
| Nasal turbinates | H5N1 | ND | 2.3 ± 0.3 | ND | 2.0 ± 0.5 | 2.3 ± 0.8 |
| ΔH5N1 | ND | 2.0 ± 0.5 | ND | ≤1.5b | ≤1.5b | |
| Lungs | H5N1 | ND | 4.0 ± 0.6 | ND | 4.1 ± 0.3 | 2.4 ± 0.2 |
| ΔH5N1 | ND | 3.6 ± 0.5 | ND | 3.0 ± 0.4 | ≤1.5b | |
AGMs were infected with 2 × 106 TCID50 of either the H5N1 or ΔH5N1 virus i.n. and intratracheally. Nasal swabs were collected on the indicated days while nasal turbinates and lungs were harvested on days 2, 4, and 7 p.i. Virus titers are expressed as mean ± standard error log10 TCID50/g of tissue or per ml of swabs. ND, not determined.
Lower limit of detection.
DISCUSSION
The virulence of human influenza viruses is not associated with an MBS motif at the HA cleavage site (52). Although the reconstructed 1918 H1N1 pandemic virus has a highly cleavable HA, an MBS motif is not present in its connecting peptide; an interaction between the HA and NA proteins of this virus might be involved in HA activation through a yet-undefined mechanism (48). The deletion of potential glycosylation sites and insertion of multiple basic amino acid residues in the cleavage site of the HA of the human influenza virus A/Aichi/2/1968 (H3N2) failed to confer enhanced cleavability of the H3 HA to the extent seen in highly pathogenic avian influenza viruses (22). Even when insertion of a polybasic cleavage site in the HA of an H3N8 virus resulted in its cleavability in the absence of exogenous trypsin and enhanced replication in vivo, the modification was still not sufficient to render the virus highly pathogenic for poultry, indicating that a highly cleavable HA is necessary but not sufficient to confer virulence for poultry (37). Structural constraints posed by amino acid insertions in the connecting peptide of non-H5 or -H7 HAs likely inhibit the generation of these types of viruses in nature (16).
Among influenza A H5 and H7 subtype viruses, the presence of an MBS in the HA protein is highly indicative of its cleavability and is clearly associated with virulence in poultry, but the impact of the H5 HA MBS on the virulence of HPAI H5N1 wt viruses in mammals is unclear. While all H5N1 viruses that have infected humans since 1997 possess the MBS in the H5 HA (1, 42), disease associated with these infections ranges in severity from mild to fatal, indicating possible contributions of other virus proteins to virulence and/or the potential role of host factors in determining disease susceptibility. Chen et al. (2007) investigated virulence determinants of the 1997 Hong Kong H5N1 wt viruses and concluded that the pathogenicity of these viruses for mice is polygenic and that the HA and NA genes, as well as an E627K substitution in the polymerase basic protein 2 (PB2), of these viruses make independent contributions to virulence (8). The E627K mutation in PB2 has been implicated in the systemic dissemination and virulence of an H5N1 wt virus (15), as well as in the impairment of the host immune response in mice (12), but this mutation is not essential for virulence in ferrets (14, 28) or in humans (11). The contribution of the other polymerase proteins to the virulence of H5N1 viruses in ferrets and mice has also been reported (10, 13, 33, 35, 38), demonstrating the complex interplay among various viral gene products that determine the virulence of H5N1 viruses.
In order to control for virulence determinants in other gene segments, we used two isogenic recombinant H5N1 wt viruses that differed only in the presence or absence of the MBS in the H5 HA protein. When all other genetic characteristics of the HPAI A/Vietnam/1203/2004 (H5N1) wt virus were kept constant, the effect of the H5 HA MBS on virulence depended on the host. Despite sharing polymerase proteins, neuraminidase, matrix, and nonstructural proteins, the H5N1 and ΔH5N1 viruses differed in their replication efficiency in vivo, and this could have affected their ability to induce proinflammatory cytokines and modulate the immune response in specific mammalian hosts. In mice, the removal of the H5 HA MBS was sufficient to ameliorate the lethality of the H5N1 wt virus (15, 43). This is not too surprising given that the H5 HA MBS was associated with enhanced virus replication, systemic virus dissemination, and lymphopenia. Mice infected with the H5N1 virus had significantly elevated levels of inflammatory cytokines and chemokines in the lungs, associated with infiltration of macrophages and neutrophils. The recruitment of these cells to the lungs likely contributes to acute lung inflammation and severe lung pathology (31).
In ferrets, the H5 HA MBS was also associated with morbidity, inducing fever, significant weight loss, lethargy, and neurological symptoms. The H5N1 virus displayed enhanced magnitude and duration of virus replication in the lower respiratory tract and also disseminated to extrapulmonary sites. Using genomic microarray analysis, Cameron et al. (2008) showed that ferrets experience a dysregulation of the innate immune response that is characterized by upregulation of interferon response genes and robust expression of the inflammatory chemokine CXCL10 in the lungs upon H5N1 virus infection (7). Our data lend support to this report: elevated mRNA levels of CXCL10, as well as several interferon response genes, were detected in the peripheral blood of H5N1-infected ferrets. Ferrets are reported to display the same pattern of attachment of avian influenza viruses as do humans (51), and the clinical illness associated with H5N1 influenza virus infection in these animals resembles that seen in humans in several aspects (14, 55), although diarrhea, neurologic symptoms, and systemic dissemination are not commonly seen in human H5N1 cases.
In nonhuman primates, the replication of both the H5N1 and ΔH5N1 viruses in the respiratory tract of AGMs was modest and neither virus caused clinical symptoms. The H5N1 virus replicated to a slightly higher titer than did the ΔH5N1 virus in the lungs. The low virulence of H5N1 virus in AGMs contrasts with reports of severe disease in cynomolgus macaques (Macaca fascicularis), where alveolar and bronchiolar lesions were apparent within 24 h of infection and upregulation of the inflammatory and innate immune gene expression was observed (2). Host genetic differences between these two species of nonhuman primates might explain the difference in their susceptibilities to HPAI H5N1 virus infection. The restricted replication of the H5N1 virus in AGMs and the absence of clinical disease suggest that AGMs may reflect milder forms of human disease caused by avian influenza H5N1 viruses, but not the severe illness associated with acute respiratory distress syndrome and multiorgan failure. AGMs are clearly not the ideal model for exploring the virulence of the H5N1 viruses.
The recent identification and elucidation of human cellular factors and the signaling pathways that are crucial for influenza virus replication (21, 26, 34) highlight the role that host genetics play in determining susceptibility to infection and disease severity. Different inbred laboratory strains of mice differ in their kinetics of weight loss and survival rates after infection with an influenza A H1N1 virus, suggesting that the host genetic background has a great influence on the immune response to influenza virus infection (36), and genetic elements that map to different loci of the mouse genome have been associated with resistance to H5N1 virus infection (4). In contrast to mice, ferrets and AGMs are outbred animals and this is reflected in the variability in the data.
In summary, when all the genetic components of an HPAI H5N1 wt virus are kept equal, the MBS of the H5 HA protein acts as a virulence marker in a host-specific manner in mammals. The H5 HA MBS was associated with lethality, enhanced virus replication, and systemic dissemination in mice and ferrets. In AGMs, it was associated with mild enhancement of replication and delayed clearance from the respiratory tract. Thus, the contribution of H5 HA MBS to the virulence of the H5N1 HPAI virus varies among mammalian hosts and is significant in mice and ferrets and less remarkable in nonhuman primates, underscoring the role of host genetic differences in the susceptibility of mammals to HPAI H5N1 infection.
ACKNOWLEDGMENTS
We thank Chris O'Donnell, Kobporn Boonnak, Elaine Lamirande of LID, Jadon Jackson, and the staff of the Comparative Medicine Branch, NIAID, for superior technical support for the animal studies conducted at the NIH and Brad Finneyfrock for excellent assistance in performing the studies in ferrets and AGMs at Bioqual. We are grateful to Hong Jin and George Kemble of MedImmune and Li-Mei Chen and Ruben Donis from the CDC for the reverse genetics plasmids and to Le Quynh Mai, National Institute of Hygiene and Epidemiology (NIHE), Vietnam, for providing the A/Vietnam/1203/2004 (H5N1) virus used in this study, which was made available to us by Nancy Cox and Alexander Klimov, Influenza Division, Centers for Disease Control and Prevention (CDC), Atlanta, GA. We also thank David Tabor, Kathy Wang, and Xiamou Chen of MedImmune for their assistance and support in conducting the qPCR assays for ferret cytokine and chemokine genes.
Footnotes
Published ahead of print 28 December 2011
REFERENCES
- 1. Abdel-Ghafar AN, et al. 2008. Update on avian influenza A (H5N1) virus infection in humans. N. Engl. J. Med. 358:261–273 [DOI] [PubMed] [Google Scholar]
- 2. Baskin CR, et al. 2009. Early and sustained innate immune response defines pathology and death in nonhuman primates infected by highly pathogenic influenza virus. Proc. Natl. Acad. Sci. U. S. A. 106:3455–3460 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Bhatia M, Moochhala S. 2004. Role of inflammatory mediators in the pathophysiology of acute respiratory distress syndrome. J. Pathol. 202:145–156 [DOI] [PubMed] [Google Scholar]
- 4. Boon AC, et al. 2009. Host genetic variation affects resistance to infection with a highly pathogenic H5N1 influenza A virus in mice. J. Virol. 83:10417–10426 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Bosch FX, Garten W, Klenk HD, Rott R. 1981. Proteolytic cleavage of influenza virus hemagglutinins: primary structure of the connecting peptide between HA1 and HA2 determines proteolytic cleavability and pathogenicity of avian influenza viruses. Virology 113:725–735 [DOI] [PubMed] [Google Scholar]
- 6. Bosch FX, Orlich M, Klenk HD, Rott R. 1979. The structure of the hemagglutinin, a determinant for the pathogenicity of influenza viruses. Virology 95:197–207 [DOI] [PubMed] [Google Scholar]
- 7. Cameron CM, et al. 2008. Gene expression analysis of host innate immune responses during lethal H5N1 infection in ferrets. J. Virol. 82:11308–11317 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Chen H, et al. 2007. Polygenic virulence factors involved in pathogenesis of 1997 Hong Kong H5N1 influenza viruses in mice. Virus Res. 128:159–163 [DOI] [PubMed] [Google Scholar]
- 9. Chen H, et al. 2006. Establishment of multiple sublineages of H5N1 influenza virus in Asia: implications for pandemic control. Proc. Natl. Acad. Sci. U. S. A. 103:2845–2850 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Conenello GM, Zamarin D, Perrone LA, Tumpey T, Palese P. 2007. A single mutation in the PB1-F2 of H5N1 (HK/97) and 1918 influenza A viruses contributes to increased virulence. PLoS Pathog. 3:1414–1421 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. de Jong MD, et al. 2006. Fatal outcome of human influenza A (H5N1) is associated with high viral load and hypercytokinemia. Nat. Med. 12:1203–1207 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Fornek JL, et al. 2009. A single-amino-acid substitution in a polymerase protein of an H5N1 influenza virus is associated with systemic infection and impaired T-cell activation in mice. J. Virol. 83:11102–11115 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Gao Y, et al. 2009. Identification of amino acids in HA and PB2 critical for the transmission of H5N1 avian influenza viruses in a mammalian host. PLoS Pathog. 5:e1000709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Govorkova EA, et al. 2005. Lethality to ferrets of H5N1 influenza viruses isolated from humans and poultry in 2004. J. Virol. 79:2191–2198 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Hatta M, Gao P, Halfmann P, Kawaoka Y. 2001. Molecular basis for high virulence of Hong Kong H5N1 influenza A viruses. Science 293:1840–1842 [DOI] [PubMed] [Google Scholar]
- 16. Horimoto T, Kawaoka Y. 1997. Biologic effects of introducing additional basic amino acid residues into the hemagglutinin cleavage site of a virulent avian influenza virus. Virus Res. 50:35–40 [DOI] [PubMed] [Google Scholar]
- 17. Horimoto T, Kawaoka Y. 1994. Reverse genetics provides direct evidence for a correlation of hemagglutinin cleavability and virulence of an avian influenza A virus. J. Virol. 68:3120–3128 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Horimoto T, Nakayama K, Smeekens SP, Kawaoka Y. 1994. Proprotein-processing endoproteases PC6 and furin both activate hemagglutinin of virulent avian influenza viruses. J. Virol. 68:6074–6078 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Jackson D, Hossain MJ, Hickman D, Perez DR, Lamb RA. 2008. A new influenza virus virulence determinant: the NS1 protein four C-terminal residues modulate pathogenicity. Proc. Natl. Acad. Sci. U. S. A. 105:4381–4386 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Kandun IN, et al. 2006. Three Indonesian clusters of H5N1 virus infection in 2005. N. Engl. J. Med. 355:2186–2194 [DOI] [PubMed] [Google Scholar]
- 21. Karlas A, et al. 2010. Genome-wide RNAi screen identifies human host factors crucial for influenza virus replication. Nature 463:818–822 [DOI] [PubMed] [Google Scholar]
- 22. Kawaoka Y. 1991. Structural features influencing hemagglutinin cleavability in a human influenza A virus. J. Virol. 65:1195–1201 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Kawaoka Y, Webster RG. 1989. Interplay between carbohydrate in the stalk and the length of the connecting peptide determines the cleavability of influenza virus hemagglutinin. J. Virol. 63:3296–3300 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Kawaoka Y, Webster RG. 1988. Sequence requirements for cleavage activation of influenza virus hemagglutinin expressed in mammalian cells. Proc. Natl. Acad. Sci. U. S. A. 85:324–328 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Klenk HD, Rott R, Orlich M, Blodorn J. 1975. Activation of influenza A viruses by trypsin treatment. Virology 68:426–439 [DOI] [PubMed] [Google Scholar]
- 26. Konig R, et al. 2010. Human host factors required for influenza virus replication. Nature 463:813–817 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Maeda T, Ohnishi S. 1980. Activation of influenza virus by acidic media causes hemolysis and fusion of erythrocytes. FEBS Lett. 122:283–287 [DOI] [PubMed] [Google Scholar]
- 28. Maines TR, et al. 2005. Avian influenza (H5N1) viruses isolated from humans in Asia in 2004 exhibit increased virulence in mammals. J. Virol. 79:11788–11800 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Maines TR, et al. 2008. Pathogenesis of emerging avian influenza viruses in mammals and the host innate immune response. Immunol. Rev. 225:68–84 [DOI] [PubMed] [Google Scholar]
- 30. Nicholls JM, et al. 2007. Tropism of avian influenza A (H5N1) in the upper and lower respiratory tract. Nat. Med. 13:147–149 [DOI] [PubMed] [Google Scholar]
- 31. Perrone LA, Plowden JK, Garcia-Sastre A, Katz JM, Tumpey TM. 2008. H5N1 and 1918 pandemic influenza virus infection results in early and excessive infiltration of macrophages and neutrophils in the lungs of mice. PLoS Pathog. 4:e1000115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Rott R, Klenk HD, Nagai Y, Tashiro M. 1995. Influenza viruses, cell enzymes, and pathogenicity. Am. J. Respir. Crit. Care Med. 152:S16–S19 [DOI] [PubMed] [Google Scholar]
- 33. Salomon R, et al. 2006. The polymerase complex genes contribute to the high virulence of the human H5N1 influenza virus isolate A/Vietnam/1203/04. J. Exp. Med. 203:689–697 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Shapira SD, et al. 2009. A physical and regulatory map of host-influenza interactions reveals pathways in H1N1 infection. Cell 139:1255–1267 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Song MS, et al. 2009. The polymerase acidic protein gene of influenza a virus contributes to pathogenicity in a mouse model. J. Virol. 83:12325–12335 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Srivastava B, et al. 2009. Host genetic background strongly influences the response to influenza A virus infections. PLoS One 4:e4857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Stech O, et al. 2009. Acquisition of a polybasic hemagglutinin cleavage site by a low-pathogenic avian influenza virus is not sufficient for immediate transformation into a highly pathogenic strain. J. Virol. 83:5864–5868 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Steel J, Lowen AC, Mubareka S, Palese P. 2009. Transmission of influenza virus in a mammalian host is increased by PB2 amino acids 627K or 627E/701N. PLoS Pathog. 5:e1000252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Steiner DF, Smeekens SP, Ohagi S, Chan SJ. 1992. The new enzymology of precursor processing endoproteases. J. Biol. Chem. 267:23435–23438 [PubMed] [Google Scholar]
- 40. Steinhauer DA. 1999. Role of hemagglutinin cleavage for the pathogenicity of influenza virus. Virology 258:1–20 [DOI] [PubMed] [Google Scholar]
- 41. Stieneke-Grober A, et al. 1992. Influenza virus hemagglutinin with multibasic cleavage site is activated by furin, a subtilisin-like endoprotease. EMBO J. 11:2407–2414 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Subbarao K, et al. 1998. Characterization of an avian influenza A (H5N1) virus isolated from a child with a fatal respiratory illness. Science 279:393–396 [DOI] [PubMed] [Google Scholar]
- 43. Suguitan AL, Jr, et al. 2009. The influence of the multi-basic cleavage site of the H5 hemagglutinin on the attenuation, immunogenicity and efficacy of a live attenuated influenza A H5N1 cold-adapted vaccine virus. Virology 395:280–288 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Suguitan AL, Jr, et al. 2006. Live, attenuated influenza A H5N1 candidate vaccines provide broad cross-protection in mice and ferrets. PLoS Med. 3:e360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Suzuki Y, et al. 2000. Sialic acid species as a determinant of the host range of influenza A viruses. J. Virol. 74:11825–11831 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Svitek N, von Messling V. 2007. Early cytokine mRNA expression profiles predict morbillivirus disease outcome in ferrets. Virology 362:404–410 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Szretter KJ, et al. 2007. Role of host cytokine responses in the pathogenesis of avian H5N1 influenza viruses in mice. J. Virol. 81:2736–2744 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Tumpey TM, et al. 2005. Characterization of the reconstructed 1918 Spanish influenza pandemic virus. Science 310:77–80 [DOI] [PubMed] [Google Scholar]
- 49. Tumpey TM, Lu X, Morken T, Zaki SR, Katz JM. 2000. Depletion of lymphocytes and diminished cytokine production in mice infected with a highly virulent influenza A (H5N1) virus isolated from humans. J. Virol. 74:6105–6116 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Ungchusak K, et al. 2005. Probable person-to-person transmission of avian influenza A (H5N1). N. Engl. J. Med. 352:333–340 [DOI] [PubMed] [Google Scholar]
- 51. van Riel D, et al. 2007. Human and avian influenza viruses target different cells in the lower respiratory tract of humans and other mammals. Am. J. Pathol. 171:1215–1223 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Webster RG, Rott R. 1987. Influenza virus A pathogenicity: the pivotal role of hemagglutinin. Cell 50:665–666 [DOI] [PubMed] [Google Scholar]
- 53. White J, Matlin K, Helenius A. 1981. Cell fusion by Semliki Forest, influenza, and vesicular stomatitis viruses. J. Cell Biol. 89:674–679 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. World Health Organization 20 November 2011, access date Cumulative number of confirmed human cases of avian influenza A/(H5N1) reported to WHO. World Health Organization, Geneva, Switzerland: http://www.who.int/influenza/human_animal_interface/H5N1_cumulative_table_archives/en/ [Google Scholar]
- 55. Zitzow LA, et al. 2002. Pathogenesis of avian influenza A (H5N1) viruses in ferrets. J. Virol. 76:4420–4429 [DOI] [PMC free article] [PubMed] [Google Scholar]