Abstract
Background: Although diet beverages are typically consumed to promote weight control, positive associations with increased cardiometabolic risk have been reported.
Objective: The objective was to examine the joint and independent association between dietary pattern and diet beverage consumption with 20-y cardiometabolic risk.
Design: We analyzed a prospective 20-y cohort of young adults from the Coronary Artery Risk Development in Young Adults (CARDIA) Study. With the use of cluster analysis, we identified 2 baseline (year 0) dietary patterns [Prudent (higher intakes of fruit, whole grains, milk, and nuts and seeds; n = 1778) and Western (higher intakes of fast food, meat and poultry, pizza, and snacks; n = 2383)] and examined the interaction with diet beverage consumption (Consumers compared with Nonconsumers) by using proportional hazards regression models.
Results: Among Consumers, 66% were classified as having a Prudent diet. In fully adjusted models, being a Nonconsumer with a Prudent diet was independently associated with a lower risk of the metabolic syndrome through year 20. Lower risk in the Prudent than in the Western dietary pattern was maintained after stratification by diet beverage consumption: Prudent Nonconsumers had the lowest risk of high waist circumference (HR: 0.78; 95% CI: 0.62, 0.97), high triglycerides (HR: 0.72; 95% CI: 0.56, 0.93), and the metabolic syndrome (HR: 0.64; 95% CI: 0.50, 0.82) compared with Western Consumers.
Conclusions: Our results suggest that both overall dietary pattern and diet beverage consumption are important, to various degrees, for different metabolic outcomes. This covariation and interaction may partially explain differences in the relation between diet beverage consumption and cardiometabolic health observed in previous studies.
INTRODUCTION
Several major longitudinal studies have reported that the consumption of diet beverages was linked to increased cardiometabolic risks (1–3). Currently, the American Diabetes Association and many weight-loss programs suggest these beverages as a means to reduce energy intake and therefore promote weight control and support weight loss, but the data supporting these recommendations are limited. Some corroborative evidence shows that the dietary habits of weight-loss maintainers include higher intakes of artificially sweetened beverages compared with persons who were always of normal weight (4), but there is still no consensus on the usefulness of substituting artificial sweeteners for sugar in the context of weight control (5, 6).
Short-term laboratory-based studies of the appetitive effects of artificial sweeteners have produced mixed results (7–11), and energy compensation has been shown to be incomplete in some (9, 12–14) but not all (15, 16) studies that used diet food and beverage products. In several widely cited observational epidemiologic studies (noted above), at least daily consumption of diet soda was associated with a greater risk of incident metabolic syndrome (1–3) and type 2 diabetes (3) and almost doubled risk of overweight or obesity (17). In these studies, diet beverage intake may be confounded with food patterns consumed by diet beverage drinkers, because a recent study showed that diet modifies the effect of cardiometabolic risk (18). Our objective was to examine how distinctly different dietary patterns may affect the association of diet beverage consumption with the risk of incident cardiometabolic outcomes, including the metabolic syndrome.
SUBJECTS AND METHODS
Study population
The CARDIA4 study is a prospective study of the evolution of cardiovascular disease risk. Baseline recruitment procedures were designed to balance age, sex, ethnicity, and education groups within each of 4 study sites (Birmingham, AL; Oakland, CA; Minneapolis, MN; and Chicago, IL). A total of 5115 young adults (aged 18–30 y) completed the baseline survey (1985–1986). Follow-up examinations were conducted 2, 5, 7, 10, 15, and 20 y after baseline with retention rates of 91%, 86%, 81%, 79%, 74%, and 72%, respectively. Detailed descriptions of the sampling plan and cohort characteristics are described elsewhere (19, 20). The data used for this study were from baseline (year 0) for diet and covariates and from all follow-up exams for the outcome variables. The full analytic sample included surviving cohort members who had complete outcome and covariate data (n = 4161). Depending on the outcome variable under analysis, we excluded persons whose year 0 data indicated prevalent high WC (n = 404), elevated BP (≥130/≥85 mm Hg or taking medication for elevated BP; n = 411), low HDL cholesterol (n = 1288), high fasting glucose (n = 743), high triglycerides (n = 262), and the metabolic syndrome (n = 155). The final sample sizes (fully adjusted models) varied by outcome as follows: high WC (n = 3524), elevated BP (n = 3500), low HDL cholesterol (n = 2699), high triglycerides (n = 3602), high fasting glucose (n = 3664), and the metabolic syndrome (n = 3728). CARDIA was approved by the local institutional review board at each center, and all participants provided written informed consent. All analyses were conducted in accordance with the ethical standards of the University of Chapel Hill.
Measurement of dietary intake and diet beverage consumption
Dietary intake was assessed at baseline by using the validated (21) interviewer-administered CARDIA Diet History questionnaire (22), which asks about general dietary practices. It was followed by a quantitative diet history, which ascertained information about consumption over the previous month. Foods and beverages from the baseline diet history were categorized by using the Nutrition Coordinating Center (Minneapolis, MN) algorithm into 43 food groups (measured as energy per day from food group). We used the “diet beverages” food group (measured as servings per day, because diet beverages have no calories) to identify baseline consumers of diet beverages. Those who consumed diet beverages are hereafter referred to as Consumers, whereas those who did not consume diet beverages are referred to as Nonconsumers. The remaining 42 food groups were converted to continuous standardized z scores of percentage of energy (kcal) and were used to derive dietary patterns via cluster analysis (23).
Dietary patterns: cluster development
Cluster analysis was performed in the pooled sample on the 42 baseline food groups, which excluded diet beverages (Stata CLUSTER, version 11.0; StataCorp). The purpose of cluster analysis is to place individuals into mutually exclusive groups (clusters) as suggested by the data and not defined a priori. Thus, individuals in a given cluster are distinctly similar to one another and distinctly different from individuals in other clusters with respect to the average dietary consumption of the set of food groups. This method has been used in previous studies of dietary and beverage patterns (23–27).
Stata's kmeans partition CLUSTER command uses Euclidean distances to create cluster centroids based on least-squares estimation over 10,000 iterations. Iterations that produced the largest r2 values indicated the best fit for the data and maximized the inter- to intracluster variability ratio (28).
To determine the most appropriate cluster solution, comparisons of cluster membership were made across increasingly complex cluster solutions: increasing from 2 to 5 clusters. To maintain within-cluster reliability, a cluster could contain no less than 5% of the sample. Increasingly complex cluster solutions (a larger number of clusters) did not break the original 2 clusters into meaningful subgroups, so the 2-cluster solution was favored. These represented the most robust patterns and maximized intercluster variability and intracluster correlation. Interpretation of the clusters was aided by comparing and describing the entire distribution of all food groups in a given cluster. A complete list of variables and z score values (each computed centered on whole-sample means and divided by whole sample SDs) for clusters is available elsewhere (see Supplemental Table 1 under “Supplemental data” in the online issue). Clustering on food groups averaged across exam year 0 and year 7 did not change our results; thus, only baseline clusters are presented herein.
Definition and components of the metabolic syndrome
The metabolic syndrome was considered present at any examination in which ≥3 of the following individual components were documented: WC >35 inches (>88 cm) for women or >40 inches (>102 cm) for men, fasting blood glucose ≥100 mg/dL (≥6.1 mmol/L) or use of diabetes medication, BP ≥130/≥85 mm Hg or use of antihypertensive medication, serum triglycerides ≥150 mg/dL (≥1.7 mmol/L) or use of cholesterol-lowering medication, or HDL cholesterol <50 mg/dL (<1.3 mmol/L) in women or <40 mg/dL (<1.03 mmol/L) in men or use of cholesterol-lowering medication (29). Standardized methods were used to collect these cardiometabolic variables and are described in detail elsewhere (30–32). Participants were asked to fast for ≥12 h and to refrain from smoking and physical activity for ≥2 h before the measurement. We excluded individuals who fasted for <8 h. Lipids, glucose, and insulin were assayed in fasting blood samples according to standardized CARDIA procedures (19). Glucose was measured by using hexokinase coupled to glucose-6-phosphate dehydrogenase. Measured height (nearest 0.5 cm), weight (nearest 0.1 kg), and WC (average of 2 measures at the minimum abdominal girth; nearest 0.5 cm) were collected by trained technicians. Seated BP (mm Hg) was measured 3 times after a 5-min rest; we used the average of the last 2 measurements. Metabolic syndrome components were assessed at each examination (except at years 2 and 5 for plasma glucose).
Covariates
Data on baseline sociodemographic characteristics and selected health behaviors were collected via self-report by using standardized questionnaires. The variables included race, sex, age, smoking status (current, former, or never), and highest education completed (continuous in years). A physical activity score, assessed by using the CARDIA physical activity questionnaire (33), was computed by multiplying the frequency of participation by the intensity of the activity and is reported as exercise units per week (most exercise captured is leisure-time physical activity). Family structure was defined by marital status and whether or not there were children living at home (single/married or with/without children). A measure of total energy intake was calculated by summing calories from all foods and beverages reported on the dietary-history questionnaire.
Statistical analysis
Baseline sociodemographic and anthropometric characteristics and energy from selected food groups were compared across dietary patterns by using Student's t tests (continuous variables) or chi-square tests (categorical variables); P < 0.05 indicated statistical significance. We examined the relation between dietary pattern, diet beverage consumption, and health by using 6 separate proportional hazards models of metabolic outcome (high WC, high fasting glucose, high triglycerides, low HDL cholesterol, elevated BP, and metabolic syndrome) on baseline dietary pattern, diet beverage use, or both. Time of occurrence of the outcome variables was set to 2, 5, 7, 10, 15, or 20 y after baseline, depending on when the outcome was first detected; those who never had the outcome condition were censored at the last visit they attended. We adjusted for important baseline covariates, including sex; age; CARDIA exam center; baseline weight, total physical activity, total energy intake, smoking status, and family structure; and maximum years of education attained ever during the study. Diet cluster membership was interacted with diet beverage consumption by adding a product term, with Consumers with a Western dietary pattern as the common referent group. Effect estimates were also generated comparing Prudent and Western dietary patterns within strata of Consumers and Nonconsumers. No sex-based or racial-ethnicity–based differences in the relations were detected.
RESULTS
Clustering
Clustering showed 2 distinct baseline dietary pattern groups: one that consumed foods that are typically considered part of a Prudent diet, such as fruit, fish, and whole grains, and one that consumed foods that typify a less healthy Western diet, such as fast foods, refined grains, and sugar-sweetened soda. Briefly, the meats and poultry group most differentiated the 2 dietary patterns, with an absolute difference in z scores of 0.935. Next highest was low-fat whole grains, with a difference of 0.819. Eleven food groups had an absolute difference in z scores of ≥0.500, including whole and refined low-fat grains, high-fat refined grains, fats, fast food, fruit, cheese, and regular (nondiet) soda. A full list of z scores in increasing order of difference is available in the online supporting information (see Supplemental Table 1 under “Supplemental data” in the online issue).
The Prudent diet group constituted 42.7% and the Consumers constituted 22.2% of the total sample (total n = 4161). Among persons with a Prudent dietary pattern, 34.5% were Consumers compared with 13.1% among the Western dietary pattern group. Consumers were more likely to be in the Prudent (66.2%) than in the Western (36.0%) diet group (see Supplemental Table 2 under “Supplemental data” in the online issue). In both dietary patterns, Nonconsumers reported a greater amount of energy from both more healthy (nuts and seeds, vegetables, and milk; P < 0.05) and less healthy [high-fat refined grains and regular (sugar-sweetened) soda; P < 0.05] food groups. Nonconsumers in the Western dietary pattern also consumed a greater amount of energy from snacks and fast food than did Consumers of the Western dietary pattern, whereas Nonconsumers of the Prudent dietary pattern consumed more energy from fruit and low-fat refined grains (see Supplemental Table 2 under “Supplemental data” in the online issue). Total energy intake was higher for Nonconsumers than for consumers in both the Prudent and Western dietary pattern groups.
In the pooled sample (ie, no regard to diet beverage consumption status), persons with a Prudent dietary pattern were more often female, white, college educated, and smokers and self-reported greater amounts of physical activity. They also tended to have lower BMIs, dramatically lower percentages of overweight and obesity, and higher HDL-cholesterol concentrations than persons in the Western dietary pattern (see Supplemental Table 3 under “Supplemental data” in the online issue). Within both dietary patterns, Consumers were more likely to be females who were white, to be older, and to have a college education; tended to be nonsmokers; and had a higher percentage of baseline overweight (Table 1). Consumers (compared with Nonconsumers) in the Prudent dietary pattern also had higher levels of self-reported physical activity. Consumers (compared with Nonconsumers) in the Western dietary pattern had higher BMIs, higher percentage baseline obesity, larger WCs, lower triglyceride concentrations, and higher HDL-cholesterol concentrations (Table 1).
TABLE 1.
Differences in baseline characteristics between subjects with Prudent and Western dietary patterns by diet beverage consumption status1
| Diet beverage |
||||
| Consumers |
Nonconsumers |
|||
| Prudent (n = 613) | Western (n = 312) | Prudent (n = 1165) | Western (n = 2071) | |
| Sociodemographic characteristics | ||||
| Female (%) | 75.2 ± 1.7 | 53.8 ± 2.82 | 56.2 ± 1.53 | 45.2 ± 1.123 |
| Black (%) | 15.2 ± 1.5 | 35.3 ± 2.72 | 41.7 ± 1.43 | 72.6 ± 1.023 |
| Age (y) | 25.7 ± 0.13 | 25.1 ± 0.202 | 25.3 ± 0.13 | 24.2 ± 0.823 |
| Education (%) | ||||
| < High school | 2.6 ± 0.6 | 6.7 ± 1.42 | 6.0 ± 0.73 | 14.5 ± 0.823 |
| High school | 15.0 ± 1.4 | 21.2 ± 2.32 | 24.8 ± 1.33 | 38.5 ± 1.123 |
| Some college | 29.2 ± 1.8 | 33.7 ± 2.7 | 33.2 ± 1.4 | 33.6 ± 1.0 |
| College | 53.2 ± 2.0 | 38.5 ± 2.82 | 36.0 ± 1.43 | 13.4 ± 0.723 |
| Family structure (%) | ||||
| Single | 58.5 ± 2.0 | 62.3 ± 2.8 | 54.8 ± 1.5 | 56.7 ± 1.1 |
| Married | 24.8 ± 1.8 | 14.5 ± 2.02 | 19.2 ± 1.23 | 10.5 ± 0.72 |
| Single with children | 4.8 ± 0.9 | 6.1 ± 1.4 | 8.0 ± 0.83 | 13.2 ± 0.723 |
| Married with children | 12.0 ± 1.3 | 17.1 ± 2.12 | 17.9 ± 1.13 | 19.7 ± 0.9 |
| Health behaviors | ||||
| Physical activity (EU/wk) | 482 ± 11 | 402 ± 172 | 452 ± 93 | 398 ± 72 |
| Smoking status (%) | ||||
| Former | 20.0 ± 1.6 | 11.9 ± 1.82 | 17.0 ± 1.1 | 8.5 ± 0.62 |
| Current | 17.6 ± 1.5 | 31.0 ± 2.62 | 24.3 ± 1.33 | 37.2 ± 1.123 |
| Never | 62.4 ± 2.0 | 57.1 ± 2.8 | 58.7 ± 1.4 | 54.3 ± 1.12 |
| Anthropometric measures | ||||
| BMI (kg/m2) | 24.4 ± 0.18 | 26.3 ± 0.312 | 24.0 ± 0.14 | 24.5 ± 0.1223 |
| Overweight (%) | 25.2 ± 1.8 | 32.3 ± 2.72 | 19.9 ± 1.23 | 23.6 ± 0.923 |
| Obese (%) | 0.9 ± 1.2 | 19.7 ± 2.32 | 1.0 ± 0.9 | 12.0 ± 0.723 |
| Waist circumference (cm) | 76.0 ± 0.4 | 82.4 ± 0.72 | 76.9 ± 0.3 | 78.1 ± 0.2623 |
| BP and lipids | ||||
| Glucose (mg/dL) | 84.0 ± 1.0 | 83.9 ± 1.2 | 82.8 ± 0.3 | 82.0 ± 0.3 |
| Triglycerides (mg/dL) | 69.8 ± 1.5 | 91.1 ± 5.02 | 70.5 ± 1.2 | 72.8 ± 1.03 |
| HDL cholesterol (mg/dL) | 55.4 ± 0.6 | 50.7 ± 0.72 | 53.6 ± 0.4 | 52.7 ± 0.33 |
| Systolic BP (mm Hg) | 107.4 ± 0.4 | 110.6 ± 0.62 | 110.4 ± 0.3 | 111.6 ± 0.22 |
| Diastolic BP (mm Hg) | 67.8 ± 0.4 | 69.3 ± 0.52 | 68.8 ± 0.3 | 68.7 ± 0.2 |
All values are means ± SEs. Consumers reported any consumption of diet beverages, and Nonconsumers reported no diet beverage consumption. BP, blood pressure; EU, exercise units.
Significantly different from Prudent (P < 0.05, Student's t test for continuous variables or chi-square tests for categorical variables) within the diet beverage consumption group (ie, Consumers or Nonconsumers) and in the pooled sample.
Significantly different from Consumers (P < 0.05, Student's t test for continuous variables or chi-square tests for categorical variables) within dietary pattern (ie, Prudent or Western dietary pattern).
Prediction of outcomes (ever by year 20)
Without consideration of diet beverage consumption, there was a significantly lower risk of the metabolic syndrome and its components (low HDL cholesterol, high triglycerides, and elevated BP) in the Prudent diet group than in the Western diet group, with nonsignificantly lower point estimates of risk of high WC and high fasting glucose (Table 2). Without consideration of dietary pattern, Nonconsumers had a significantly lower risk (compared with Consumers) of the metabolic syndrome, but there was no consistency observed among its components (significantly lower risk was observed for high WC only). Analysis of joint dietary pattern and diet beverage consumption found a statistically significant interaction in the prediction of high fasting glucose, low HDL cholesterol, and high BP (Table 3).
TABLE 2.
Association between dietary pattern and diet beverage consumption with 20-y cardiometabolic outcomes1
| High WC(n = 3524) | High fasting glucose (n = 3664) | Low HDL-C (n = 2699) | High TGs (n = 3602) | High BP (n = 3500) | Metabolic syndrome (n = 3728) | |
| Prudent compared with Western pattern | 0.92 (0.80, 1.06) | 0.93 (0.80, 1.09) | 0.87 (0.75, 0.99)2 | 0.78 (0.67, 0.92)2 | 0.84 (0.73, 0.98)2 | 0.77 (0.66, 0.91)2 |
| Nonconsumer compared with Consumer | 0.84 (0.73, 0.97)2 | 1.07 (0.91, 1.26) | 1.02 (0.88, 1.18) | 0.92 (0.78, 1.08) | 1.00 (0.85, 1.17) | 0.81 (0.69, 0.95)2 |
All values are HRs (95% CIs) derived from proportional hazards models adjusted for race; sex; CARDIA study center; baseline age, BMI, smoking status, family structure, total energy (kcal/d), and physical activity (exercise units/wk); maximum education reported during the study (in y); and either diet beverage consumption (in dietary pattern model) or dietary pattern (in diet beverage consumption model). BP, blood pressure; CARDIA, Coronary Artery Risk Development in Young Adults; HDL-C, HDL cholesterol; TGs, triglycerides; WC, waist circumference.
Significantly different from zero, P < 0.05.
TABLE 3.
Joint associations between dietary pattern and diet beverage consumption with 20-y cardiometabolic outcomes1
| High WC (n = 3524) | High fasting glucose (n = 3664) | Low HDL-C (n = 2699) | High TGs (n = 3602) | High BP (n = 3500) | Metabolic syndrome (n = 3728) | |
| Western Consumers | 1.0 | 1.0 | 1.0 | 1.0 | 1.0 | 1.0 |
| Western Nonconsumers | 0.85 (0.70, 1.04) | 0.92 (0.74, 1.16) | 0.85 (0.70, 1.05) | 0.93 (0.74, 1.18) | 1.21 (0.97, 1.53) | 0.85 (0.69, 1.07) |
| Prudent Consumers | 0.93 (0.73, 1.17) | 0.75 (0.57, 0.99)2 | 0.69 (0.54, 0.87)2 | 0.80 (0.61, 1.05) | 1.14 (0.87, 1.51) | 0.84 (0.64, 1.10) |
| Prudent Nonconsumers | 0.78 (0.62, 0.97)2 | 0.92 (0.73, 1.18) | 0.81 (0.65, 1.01) | 0.72 (0.56, 0.93)2 | 0.92 (0.72, 1.19) | 0.64 (0.50, 0.82)2 |
| P-interaction | 0.943 | 0.066 | 0.017 | 0.851 | 0.010 | 0.460 |
All values are HRs (95% CIs) derived from proportional hazards models of cardiometabolic outcome on dietary pattern, diet beverage consumption status, and the interaction of dietary pattern with diet beverage consumption, adjusted for race; sex; CARDIA study center; baseline age, BMI, smoking status, family structure, total energy (kcal/d), and physical activity (exercise units /wk); and maximum education reported during the study (in y). BP, blood pressure; CARDIA, Coronary Artery Risk Development in Young Adults; HDL-C, HDL cholesterol; TGs, triglycerides; WC, waist circumference.
Significantly different from the Western Consumer group, P < 0.05.
The predicted patterns for the individual components of the metabolic syndrome are less consistent. Consumers with a Prudent dietary pattern had the lowest risk of high fasting glucose (HR: 0.75; 95% CI: 0.57, 0.99) and low HDL cholesterol (HR: 0.69; 95% CI: 0.54, 0.87), which were significantly different from the Western Consumers. Nonconsumers with a Prudent dietary pattern, on the other hand, had lower risks of high WC and high triglycerides than did Consumers with a Western dietary pattern. Western Consumers and Prudent Nonconsumers were not statistically different with respect to high fasting glucose, low HDL cholesterol, and high BP (Table 3).
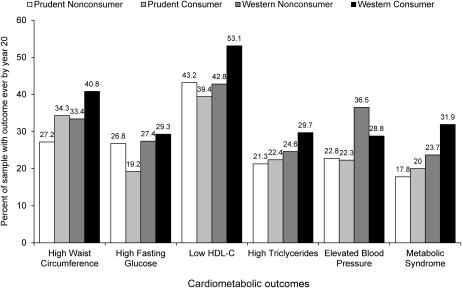
Findings were similar for unadjusted (Figure 1) and adjusted (Table 3) relations. Generally, Consumers with a Western dietary pattern had the highest percentage of the sample with the outcome ever by year 20, whereas the Prudent dietary pattern had the lowest (with the lowest percentage varying between Consumers and Nonconsumers by metabolic outcome). The largest exception was that the nearly identical unadjusted percentages (rates) of elevated BP between Consumers and Nonconsumers with a Prudent dietary pattern were altered with adjustment, such that the Consumers with a Prudent dietary pattern had a higher HR of elevated BP than did Nonconsumers.
FIGURE 1.
Age-adjusted cumulative distributions of year 20 cardiometabolic outcomes stratified by dietary pattern and diet beverage consumption status. The values represent the percentage of persons with the outcome shown ever by year 20. The number of observations in age-adjusted distributions varied by outcome as follows: high waist circumference (n = 3524), high fasting glucose (n = 3664), low HDL cholesterol (n = 2699), high triglycerides (n = 3602), elevated blood pressure (n = 3500), and the metabolic syndrome (n = 3728). HDL-C, HDL cholesterol.
DISCUSSION
To our knowledge this is the first study to specifically examine the interplay between dietary patterns and diet beverage consumption in prospective prediction of cardiometabolic health outcomes. Overall, a Prudent dietary pattern showed a lower risk of incident metabolic syndrome and each of its components than did a Western dietary pattern. Nonconsumers (compared with consumers) also had a lower risk of incident metabolic syndrome, but associations with the components of the metabolic syndrome were inconsistent. Furthermore, persons with a Prudent dietary pattern were more likely (compared with persons with a Western dietary pattern) to consume diet beverages. Looking jointly at dietary pattern and diet beverage consumption, it is clear that a Prudent dietary pattern is consistently associated with lower risk and being a diet beverage Nonconsumer sometimes, but not always, additionally lowers that risk.
Specifically, we found that persons with a Western dietary pattern who were diet beverage Consumers had a higher risk of cardiometabolic outcomes, except for elevated BP, than did the other 3 groups. Nonconsumers with a Prudent dietary pattern had a lower risk of the metabolic syndrome, a high WC, and high triglycerides (compared with Consumers with a Western dietary pattern), but Consumers with a Prudent dietary pattern had a lower risk of high fasting glucose and low HDL cholesterol. Although both a Prudent dietary pattern and being a diet beverage Nonconsumer were associated with a lower risk of incident metabolic syndrome, our results suggest that dietary pattern and diet beverage consumption interact in predictions of cardiometabolic risks and should be examined jointly.
Previous studies have examined the relation between consumption of diet beverages and cardiometabolic outcomes (1, 3). Nettleton et al (3) reported that at least daily consumption of diet beverages was associated with an increased risk of incident metabolic syndrome (HR: 1.36; 95% CI: 1.11, 1.66) in an older sample of adults (3). Similarly, there was a 53% increase in the odds of incident metabolic syndrome (OR: 1.53; 95% CI: 1.10, 2.15) among older men and women in the Framingham Study (1). Each of these studies, however, had minimal control for confounding by diet: models adjusted for total energy intake (kcal) (3) or total energy intake (kcal) plus consumption of saturated fat, trans fat, and fiber (1). None of these studies considered the possibility of interaction.
An important new study by de Koning et al (18) found that an observed association between intake of artificially sweetened beverages and an increased risk of type 2 diabetes is attenuated and no longer statistically significant after multivariate adjustment for detailed measures of family history, previous weight change, dieting, Healthy Eating Index score, and total energy intake in a comparison of the top with the bottom quartile of intake (HR: 1.09; 95% CI: 0.98, 1.21; P-trend = 0.13). Although de Koning et al addressed possible confounding by diet more completely than did other studies, their results still could have missed important interactions between dietary pattern and diet beverage consumption, as our study shows. Inclusion of diet beverages in the creation of dietary patterns in our study would likely have resulted in an attenuation of the influence of eating a Prudent diet on cardiometabolic outcomes, which suggests that dietary pattern and diet beverage consumption should be examined independently from one another.
Our study is not without limitations. First, the use of observational, self-reported dietary data precluded us from ruling out residual confounding or making conclusive statements about a possible causal relation between overall dietary patterns and cardiometabolic risk among consumers of diet beverages. Retrospective self-report data are also subject to recall and response bias, which can lead to differential misclassification of dietary intake and is particularly problematic if subgroups of the sample (ie, blacks and whites) differentially report intake. It is also well known that overweight individuals are prone to underreporting energy intake and overreporting physical activity (34). Second, it is possible that persons meeting just 2 baseline criteria for metabolic syndrome were advised to make dietary changes. Because we did not exclude these persons from our analyses, it is possible that our results are slight underestimations of the association between dietary pattern, diet beverage consumption, and cardiometabolic risk. This would be an interesting question to examine with a little larger sample size; <10% of this sample met just 2 criteria (results not reported elsewhere). Finally, our group of Nonconsumers included persons who consume beverages that have been negatively associated with several of the metabolic outcomes examined (eg, sugar-sweetened beverages) and beverages that are arguably healthier (eg, water). This likely had a small effect on our results; however, because most of the Nonconsumers consumed these healthier beverages. For example, at baseline, 53% of the sample consumed water but not sugar-sweetened soda, 6.3% consumed sugar-sweetened soda but not water, and 7.3% consumed both (data not shown elsewhere).
Although the CARDIA Diet History and food-frequency questionnaire have been shown to be valid and reliable instruments, nutrient and energy estimates had larger variability among blacks than among whites (21, 22). Finally, our analyses are limited to the baseline (1985–1986) measure of Consumers; thus, our numbers are small compared with recent estimates, which show considerable increases in diet beverage consumption in the United States over the past decade (5). However, this is also a strength, because it shows that a behavior that was in place by age 18–30 y predicted metabolic outcomes as far as 20 y into the future. Furthermore, there was considerable stability in dietary patterning and diet beverage consumption across time (73% of the baseline sample consumed the same dietary pattern at year 7, 78% of whom consumed the same dietary pattern at year 20; data not shown elsewhere), which suggests that baseline measures are relatively good proxies for later behaviors.
In conclusion, our study found that dietary pattern and diet beverage consumption were each independently associated with incident metabolic syndrome and high WC. Consumption of diet beverages in the context of a Western dietary pattern was generally associated with a higher risk of metabolic outcomes compared with all other groups. Our results suggest that both overall dietary pattern and diet beverage consumption status are important, to various degrees, for different metabolic outcomes. Their covariation and interaction partially explain differences in the relation between diet beverage consumption and metabolic health, which has been observed in previous studies. Further research is needed to more completely understand the dietary patterns and consumption decisions of diet beverages consumers; especially important is research that can help elucidate the motivation of diet beverage consumption among persons with less healthy food patterning.
Supplementary Material
Acknowledgments
We thank Frances Dancy for administrative assistance, Tom Swasey for graphic support, and the CARDIA Study participants for their important contributions.
The authors’ responsibilities were as follows—KJD and BMP: designed the study; KJD, BMP, and DRJ: conducted the research, analyzed and interpreted the data, had primary responsibility for the final content, and provided statistical expertise; BMP and DRJ: provided essential data and materials; KJD: drafted the manuscript; BMP, DRJ, LVH, and LMS: critically revised the manuscript for important intellectual content; and BMP: supervised the study. None of the authors had any conflicts of interest with respect to the manuscript.
Footnotes
Abbreviations used: BP, blood pressure; CARDIA, Coronary Artery Risk Development in Young Adults; WC, waist circumference.
REFERENCES
- 1.Dhingra R, Sullivan L, Jacques PF, Wang TJ, Fox CS, Meigs JB, D'Agostino RB, Gaziano JM, Vasan RS. Soft drink consumption and risk of developing cardiometabolic risk factors and the metabolic syndrome in middle-aged adults in the community. Circulation 2007;116:480–8 [DOI] [PubMed] [Google Scholar]
- 2.Lutsey PL, Steffen L, Stevens J. Dietary intake and the development of the metabolic syndrome: the Atherosclerosis Risk in Communities study. Circulation 2008;117:754–61 [DOI] [PubMed] [Google Scholar]
- 3.Nettleton JA, Lutsey P, Wang Y, Lima J, Michos E, Jacobs D., Jr Diet soda intake and risk of incident metabolic syndrome and type 2 diabetes in the Multi-Ethnic Study of Atherosclerosis (MESA). Diabetes Care 2009;32:688–94 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Phelan S, Lang W, Jordan D, Wing RR. Use of artificial sweeteners and fat-modified foods in weight loss maintainers and always-normal weight individuals. Int J Obes (Lond) 2009;33:1183–90 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Mattes RD, Popkin BM. Nonnutritive sweetener consumption in humans: effects on appetite and food intake and their putative mechanisms. Am J Clin Nutr 2009;89:1–14 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Drewnowski A. Intense sweeteners and energy density of foods: implications for weight control. Eur J Clin Nutr 1999;53:757–63 [DOI] [PubMed] [Google Scholar]
- 7.Blundell JE, Hill AJ. Paradoxical effects of an intense sweetener (aspartame) on appetite. Lancet 1986;1:1092–3 [DOI] [PubMed] [Google Scholar]
- 8.Canty DJ, Chan MM. Effects of consumption of caloric vs noncaloric sweet drinks on indices of hunger and food consumption in normal adults. Am J Clin Nutr 1991;53:1159–64 [DOI] [PubMed] [Google Scholar]
- 9.Lavin JH, French SJ, Read NW. The effect of sucrose- and aspartame-sweetened drinks on energy intake, hunger and food choice of female, moderately restrained eaters. Int J Obes Relat Metab Disord 1997;21:37–42 [DOI] [PubMed] [Google Scholar]
- 10.Rolls BJ, Laster LJ, Summerfelt A. Hunger and food intake following consumption of low-calorie foods. Appetite 1989;13:115–27 [DOI] [PubMed] [Google Scholar]
- 11.Rogers PJ, Blundell JE. Separating the actions of sweetness and calories: effects of saccharin and carbohydrates on hunger and food intake in human subjects. Physiol Behav 1989;45:1093–9 [DOI] [PubMed] [Google Scholar]
- 12.Anderson GH, Saravis S, Schacher R, Zlotkin S, Leiter LA. Aspartame: effect on lunch-time food intake, appetite and hedonic response in children. Appetite 1989;13:93–103 [DOI] [PubMed] [Google Scholar]
- 13.Drewnowski A, Massien C, Louis-Sylvestre J, Fricker J, Chapelot D, Apfelbaum M. The effects of aspartame versus sucrose on motivational ratings, taste preferences, and energy intakes in obese and lean women. Int J Obes Relat Metab Disord 1994;18:570–8 [PubMed] [Google Scholar]
- 14.Rolls BJ, Fedoroff IC, Guthrie JF, Laster LJ. Foods with different satiating effects in humans. Appetite 1990;15:115–26 [DOI] [PubMed] [Google Scholar]
- 15.Black RM, Leiter LA, Anderson GH. Consuming aspartame with and without taste: differential effects on appetite and food intake of young adult males. Physiol Behav 1993;53:459–66 [DOI] [PubMed] [Google Scholar]
- 16.Foltin RW, Fischman MW, Moran TH, Rolls BJ, Kelly TH. Caloric compensation for lunches varying in fat and carbohydrate content by humans in a residential laboratory. Am J Clin Nutr 1990;52:969–80 [DOI] [PubMed] [Google Scholar]
- 17.Fowler SP, Williams K, Resendez R, Hunt K, Hazuda H, Stern M. Fueling the obesity epidemic? Artificially sweetened beverage use and long-term weight gain. Obesity (Silver Spring) 2008;16:1894–900 [DOI] [PubMed] [Google Scholar]
- 18.de Koning L, Malik VS, Rimm EB, Willett WC, Hu FB. Sugar-sweetened and artificially sweetened beverage consumption and risk of type 2 diabetes mellitus among men. Am J Clin Nutr 2011;93:1321–7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Friedman GD, Cutter G, Donahue R, Hughes G, Hulley S, Jacobs D, Liu K, Savage P. CARDIA: study design, recruitment, and some characteristics of the examined subjects. J Clin Epidemiol 1988;41:1105–16 [DOI] [PubMed] [Google Scholar]
- 20.Hughes GH, Cutter G, Donahue R, Friedman GD, Hulley S, Hunkeler E, Jacobs DR Jr, Liu K, Orden S, Pirie P, et al. Recruitment in the Coronary Artery Disease Risk Development in Young Adults (Cardia) Study. Control Clin Trials 1987;8(suppl):68S–73S [DOI] [PubMed] [Google Scholar]
- 21.Liu K, Slattery ML, Jacobs DR, Jr, Cutter G, McDonald A, Van Horn L, Hilner JE, Caan B, Bragg C, Dyer A, et al. A study of the reliability and comparative validity of the CARDIA dietary history. Ethn Dis 1994;4:15–27 [PubMed] [Google Scholar]
- 22.McDonald A, Van Horn L, Slattery ML, Hilner JE, Bragg C, Caan BJ, Jacobs DR, Jr, Liu K, Hubert H, Gernhofer N, et al. The CARDIA dietary history: development, implementation, and evaluation. J Am Diet Assoc 1991;91:1104–12 [PubMed] [Google Scholar]
- 23.Duffey KJ, Popkin BM. Adults with healthier dietary patterns have healthier beverage patterns. J Nutr 2006;136:2901–7 [DOI] [PubMed] [Google Scholar]
- 24.Knol LL, Haughton B, Fitzhugh EC. Dietary patterns of young, low-income US children. J Am Diet Assoc 2005;105:1765–73 [DOI] [PubMed] [Google Scholar]
- 25.Millen BE, Quatromoni PA, Pencina M, Kimokoti R, Nam BH, Cobain S, Kozak W, Appugliese DP, Ordovas J, D'Agostino RB. Unique dietary patterns and chronic disease risk profiles of adult men: the Framingham nutrition studies. J Am Diet Assoc 2005;105:1723–34 [DOI] [PubMed] [Google Scholar]
- 26.Popkin BM, Barclay DV, Nielsen SJ. Water and food consumption patterns of U.S. adults from 1999 to 2001. Obes Res 2005;13:2146–52 [DOI] [PubMed] [Google Scholar]
- 27.Villegas R, Salim A, Collins MM, Flynn A, Perry IJ. Dietary patterns in middle-aged Irish men and women defined by cluster analysis. Public Health Nutr 2004;7:1017–24 [DOI] [PubMed] [Google Scholar]
- 28.Nelson MC, Gordon-Larsen P, Adair L, Popkin B. Adolescent physical activity and sedentary behavior patterning and long-term maintenance. Am J Prev Med 2005;28:259–66 [DOI] [PubMed] [Google Scholar]
- 29.National Heart, Lung, and Blood Institute. Third Report of the Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III). In: Grundy SM, ed. Bethesda, MD: National Cholesterol Education Program, National Heart, Lung, and Blood Institute, NIH, 2002 (NIH publication no. 02-5215)
- 30.Carnethon MR, Gidding SS, Nehgme R, Sidney S, Jacobs DR, Jr, Liu K. Cardiorespiratory fitness in young adulthood and the development of cardiovascular disease risk factors. JAMA 2003;290(23):3092–100 [DOI] [PubMed] [Google Scholar]
- 31.Kizilbash MA, Carnethon MR, Chan C, Jacobs DR, Sidney S, Liu K. The temporal relationship between heart rate recovery immediately after exercise and the metabolic syndrome: the CARDIA study. Eur Heart J 2006;27:1592–6 [DOI] [PubMed] [Google Scholar]
- 32.Pereira MA, Kartashov AI, Ebbeling CB, Van Horn L, Slattery ML, Jacobs DR., Jr Fast-food habits, weight gain and insulin resistance (the CARDIA) study: 15-year prospective analysis. Lancet 2005;365:36–42 [DOI] [PubMed] [Google Scholar]
- 33.Jacobs D, Hahn L, Haskell W, Pirie P, Sidney S. Validity and reliability of short physical activity history: CARDIA and the Minnesota Heart Healthy Program. J Cardiopulm Rehabil 1989;9(11):448–59 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Neuhouser ML, Tinker L, Shaw P, Schoeller D, Bingham S, Van Horn L, Beresford S, Caan B, Thomson C, Satterfield S, et al. Use of recovery biomarkers to calibrate nutrient consumption self-reports in the Women's Health Initiative. Am J Epidemiol 2008;167:1247–59 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.