Abstract
Background
The recognition of the importance of femoral acetabular impingement (FAI) as a potential cause of hip pain has been stimulated by major efforts to salvage hip joints by reconstruction in order to prevent or delay the need for replacement. The purpose of this review is to define the nature of FAI, the various types, and how to make the diagnosis.
Methods
The review describes the characteristics of the hip that cause FAI and emphasizes understanding that the femoral and acetabular components normally function as a unit, complementing each other.
Results/Conclusion
The methods of making the diagnosis of FAI and their limitations are described. If the acetabulum and femur are considered to be independent of each other, conflict may occur, hindering function, and not be apparent. The increasing frequency of making this diagnosis based on abnormal anatomy on one side of the joint, often in face of unclear physical findings, can bring the diagnosis into question. FAI seen in Perthes disease and acetabular dysplasia is explained. Knowing how to analyze the hip, being aware of the limitations of various available clinical and diagnostic studies, and recognizing the continued and ever-changing extensive body of literature is important and challenging. This primer is just the beginning.
Keywords: Femoro-acetabular impingement, Pincer impingement, Cam impingement, Acetabular retroversion, Posterior wall sign, Ischial spine sign, Crossover sign
Introduction
The recognition of the importance of femoro-acetabular impingement (FAI) as a potential cause of hip pain in recent years has been stimulated by the major efforts to salvage hip joints by reconstruction to either prevent or delay the need for replacement. The intense interest in this goal is reflected in the literally hundreds of articles published in the last 10 years; new studies examining different aspects of the problem are being published monthly.
FAI occurs when there is abnormal contact of the femur with the acetabulum. This can occur anteriorly or posteriorly, with the former being more common.
The purpose of this review is to define the nature of FAI, the various types, and how to make the diagnosis. Understanding the labrum of the hip, the structure caught, so to speak, in the impingement is the subject of a forthcoming review.
The diagnosis
Impingement occurs as a result of acetabular and/or femoral pathology or misalignment, most often involving the anterior aspect of the hip. There are two types of impingement, pincer and cam [1] (Fig. 1).
Fig. 1.
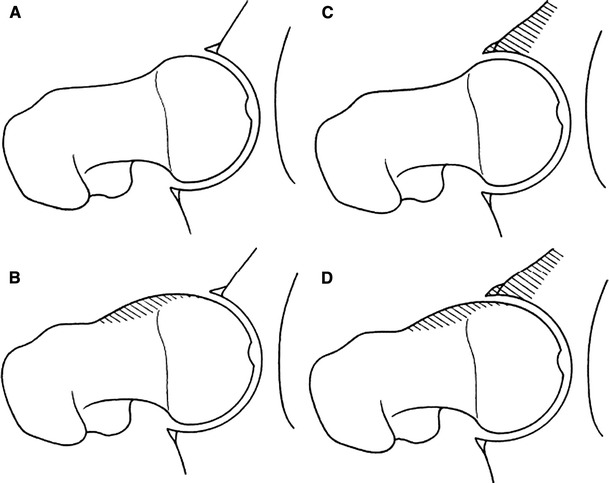
The factors causing femoro-acetabular impingement (FAI) are shown. The reduced clearance during motion leads to repetitive abutment between the proximal femur and the anterior acetabular rim. a Normal clearance of the hip. b Reduced femoral head and neck offset. c Excessive overcoverage of the femoral head by the acetabulum. d Combination of reduced head and neck offset and excessive overcoverage can be seen (reproduced with permission from Lavigne et al. [1], Fig. 1)
Impingement due to an abnormally long anterior or posterior acetabular structure contacting the femoral neck is called pincer impingement (Fig. 1c). Anterior acetabular impingement is more common. When the abnormal contact is due to abnormality in the femoral neck, such as a decreased femoral head–neck offset, so called cam impingement occurs (Fig. 1b). In many instances of clinically evident impingement, both cam and pincer are present [1] (Fig. 1d).
The proper function of the hip joint requires that the anatomic characteristics of the acetabulum and femoral neck complement each other. Proper function in face of a structural abnormality of one requires a structural adjustment in the other, otherwise, abnormal function and symptoms will likely occur. Understanding FAI thus requires appreciation of how the relationship of the acetabulum to the proximal femur influences impingement. It is necessary to recognize the influence that proximal femoral and acetabular pathology has on FAI, and, ultimately, how FAI can cause acetabular and proximal femoral pathology.
The classic article by Tönnis and Heinecke [2] describes how the coupling of different degrees of acetabular and femoral version influences the function of the hip and resultant severity of pain. Range of motion and severity of pain vary with different combinations of version. Increased pain is noted with either decreased acetabular anteversion (acetabular retroversion) or decreased femoral anteversion, with the symptoms worsening with the severity of abnormal version.
Tönnis and Heinecke compare different variations in the degrees of abnormal acetabular and femoral version. It is evident that decreased femoral anteversion is more likely to cause pain than decreased acetabular anteversion (retroversion), and the severity of the pain is worse. The reason for this is clear. Internal femoral rotation is required for normal gait. It is limited with decreased femoral anteversion and further movement internally causes impingement and pain. This is lessened if the decreased femoral anteversion is associated with increased acetabular anteversion (anterior uncovering).
The study also indicates that impingement and pain associated with decreased acetabular version (retroversion) occurs with or without decreased femoral version, but is noticeably worse if there is decreased femoral anteversion.
It is clearly evident from the study by Tönnis and Heinecke that the acetabulum and proximal femur behave as a matched pair with regard to function, impingement, and pain. Therefore, to understand the effect of the version of either the acetabulum or the femur, it is necessary to know the version of both in any given case. Version studies can provide this information.
The physical findings in FAI are specific. Anterior FAI, more common than posterior FAI, occurs when the hip is flexed and internally rotated, bringing the femoral neck against the anterior acetabulum and labrum. Posterior FAI occurs when the hip is extended and externally rotated. Given the patient with anterior or posterior hip pain, these maneuvers confirm the appropriate diagnosis [3] (Fig. 2).
Fig. 2.
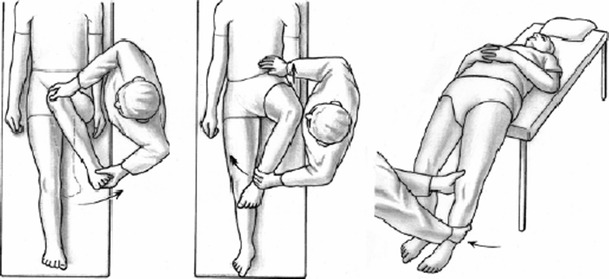
Clinical tests to assess FAI. Anterior impingement sign (left) is positive with forced internal rotation at 90° hip flexion. In extremes, unavoidable external rotation occurs during hip flexion when attempting internal rotation—Drehamann’s sign (center). Posterior impingement is positive with external rotation and hip extension (right) (reproduced with permission from Tannast et al. [7], Fig. 3)
Is the increasing diagnosis of FAI justified?
Using these indicated maneuvers, the diagnosis of FAI has been made with increasing frequency, resulting in frequent surgical indications, with or without extensive physical therapy. Various radiographic and imaging techniques are rapidly invoked to demonstrate abnormality and justify the FAI diagnosis. The limitations of these studies and the requirement for exactness are seldom either understood or recognized. These limitations and requirements will be defined.
Anterior hip pain can have many other causes. This includes both acute and chronic problems with extraarticular structures, muscular, neurovascular, and osseous structures in that region, as well as the capsule and synovium of the intraarticular space. The use of special studies, including routine and enhanced computed tomography (CT) and magnetic resonance imaging (MRI), may be needed to clarify the cause of these symptoms.
Pincer impingement: the acetabular causes of FAI
Pincer impingement occurs with acetabular retroversion, coxa profunda, or protrusio acetabuli. It is more common in females (M:F 1:3) and the average age of occurrence of symptoms is 40 years of age. Associated pathology includes bladder exstrophy, proximal femoral focal deficiency, posttraumatic or residual acetabular dysplasia, Legg–Perthes disease, slipped proximal femoral epiphysis, idiopathic retroversion, and after periacetabular osteotomy (PAO) [4]. Many of these conditions, which are femoral abnormalities with large femoral heads or abnormal head–neck offset, often have an associated anterior acetabular prominence, hence, pincer impingement can occur.
Radiographic and imaging studies include well-positioned antero-posterior (AP) and lateral views of the pelvis, faux profile views of the hip, CT scans, and MRI scans [4].
On the AP view of the pelvis, three signs indicate acetabular abnormality associated with FAI: the crossover sign, the posterior wall sign, and the ischial spine sign (Fig. 3). They are usually present together. Normally, the anterior and posterior walls of the acetabulum, seen on the AP study, meet at the lateral edge of the acetabulum. When there is retroversion, they cross over each other rather than meeting at the lateral edge—the crossover sign. In these instances, the posterior wall projection on the AP view falls medial to the center of the femoral head, the posterior wall sign, rather than the norm, where the posterior wall projects lateral to that center. It has been noted that, in all instances of acetabular retroversion, the ischial spine, normally hidden on the AP view, is clearly visualized—the ischial spine sign [3, 5, 6].
Fig. 3.
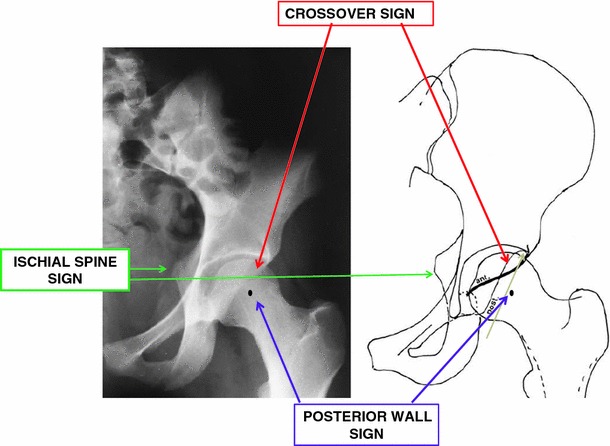
Signs of acetabular retroversion on antero-posterior (AP) X-ray. Crossover sign: when the projection of the anterior acetabular wall crosses the posterior wall instead of meeting at the top of the acetabulum. Posterior wall sign: when the projection of the posterior acetabular wall is medial to the center of the femoral head. Ischial spine sign: when the ischial spine is seen on the AP X-ray (modified with permission from Reynolds et al. [6], Fig. 6)
Coxa profunda, the deep socket, is identified on the AP view when the medial wall of the acetabulum either is at or crosses the ilioischial line. Protrusio acetabuli is noted when the femoral head either is at or crosses that same ilioischial line [4] (Fig. 4). In each instance, the anterior wall of the acetabulum covers more of the femoral head than normal, which can result in pincer impingement.
Fig. 4.
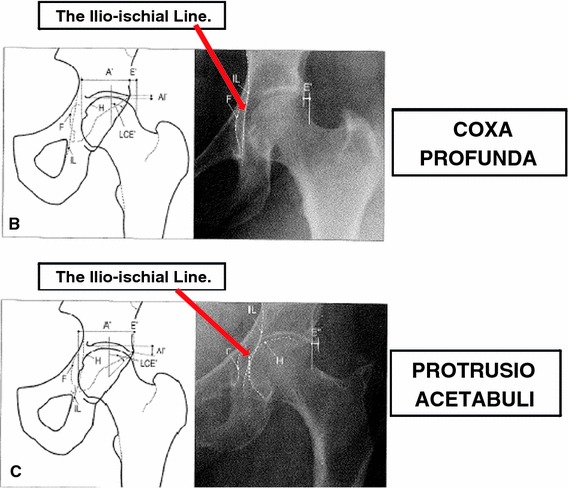
Coxa profunda: the medial wall of the acetabulum is on or medial to the ilioischial line. Protrusio acetabuli: the medial edge of the femoral head is on or crosses the ilioischial line (modified with permission from Tannast and Siebenrock [4], Fig. 3b, c)
The problem in using the AP view of the pelvis to identify these signs and make the diagnosis is the accuracy in positioning the view. How the beam of the X-ray is centered and how the pelvis is tilted and/or rotated radically affects these signs. The beam should be centered on the pelvis, not the hip. The beam centered over the hip increases the degree of acetabular anteversion, decreasing the crossover and posterior wall signs. For example, in the case in Fig. 4, the retroversion would have been completely missed [7] (Fig. 5). Additionally, centering the beam over the hip causes coxa profunda to be seen as protrusio acetabuli [4] (Fig. 6).
Fig. 5.
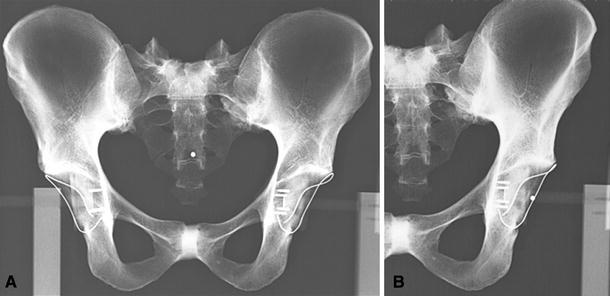
Retroversion can be missed if the X-ray beam is not directed correctly. a Radiograph shows cranial acetabular retroversion on the left (beam location marked by a dot in the center of the pelvis. b Radiograph shows the retroversion falsely gone when the beam center (dot) is over the hip (reproduced with permission from Tannast et al. [7], Fig. 13)
Fig. 6.

Coxa profunda becomes protrusio acetabuli as the X-ray beam shifts from the center of the pelvis to the center of the hip (modified with permission from Tannast and Siebenrock [4], Fig. 5)
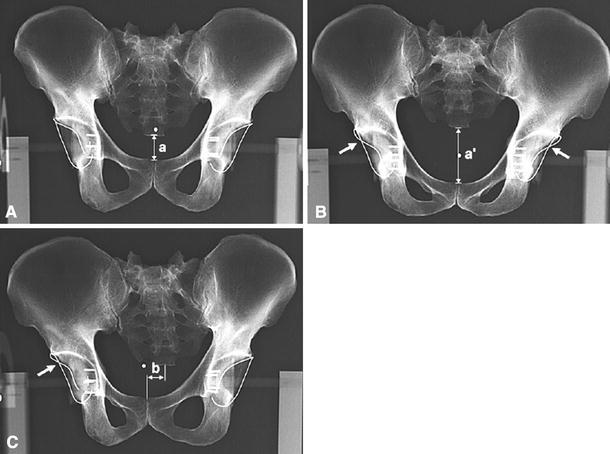
Pelvic tilt and rotation, masking the true pelvic orientation, can be misleading. Tilt is measured as the distance between the sacrococcygeal joint (scj) and the top of the pubic symphysis, the sacrococcygeal-symphysis (sc-s) line [8] (Fig. 7). In the “normally” positioned pelvis, this distance is 3.2 cm in men and 4.7 cm in women. Tilt forward (inclination), the inlet view, increases the sc-s line (Fig. 7c). This falsely increases the signs of retroversion (Figs. 7c and 8b). Tilting backward (reclination), the outlet view, decreases the sc-s line (Fig. 7b). This falsely decreases the signs of retroversion (Fig. 8a). The graph [8] (Fig. 9) allows actually determining the degree of pelvic tilt (reclination and inclination) by measuring the length of the sc-s line.
Fig. 7.
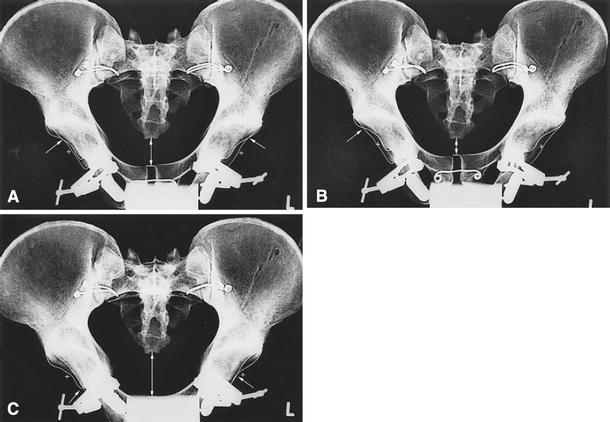
The degree of the pelvic tilt. Pelvic tilt is determined by measuring the length from the sacrococcygeal joint (scj) to the top of the pubic symphysis (sacrococcygeal-symphysis line, sc-s line). a Neutral (3.2 cm—males, 4.7 cm—females). b 6° reclination (outlet view). c 6° inclination (inlet view) (reproduced with permission from Siebenrock et al. [8], Fig. 1a–c)
Fig. 8.
Tilt and rotation changes the signs of FAI. a Neutral pelvic tilt. b Pelvis inclined, apparent retroversion, false crossover signs bilateral. c Rotation to the right, apparent crossover on right, pronounced anteversion on the left (reproduced with permission from Tannast et al. [7], Fig. 14a–c)
Fig. 9.
The pelvic inclination angle. The values of the sc-s line measure the pelvic inclination angles at different degrees of tilt (different for men and women). Neutral: 0°, tilt (men—3.2 cm, women—4.7 cm). Inclination (inlet view): positives values (greater than neutral sc-s values). Reclination (outlet view): negative values (less than neutral sc-s values). Using this graph, the degree of pelvic tilt can be determined by measuring the sc-s line (modified with permission from Siebenrock et al. [8], Fig. 4)
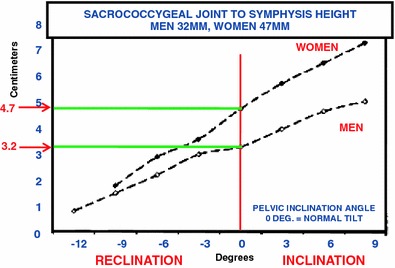
On a lateral X-ray of the pelvis, pelvic tilt is measured as an angle derived from a line made from the top of the sacral promontory to the top of the symphysis and the other being the horizontal. That angle is normally 60° [9] (Fig. 10a).
Fig. 10.
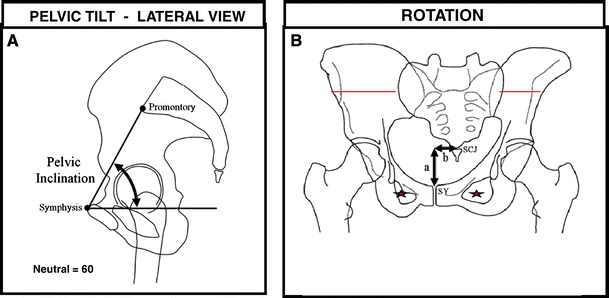
Pelvic inclination and rotation. a Pelvic inclination is measured on the lateral X-ray by measuring the angle between a horizontal line and a line connecting the upper border of the pubic symphysis and the sacral promontory. Neutral pelvic inclination is 60°. b Pelvic rotation: on the AP pelvic X-ray, a vertical line through the sacrococcygeal joint should lie on the vertical line through the pubic symphysis. If the pelvis is rotated, these two lines separate. The horizontal distance of separation indicates the amount of rotation (modified with permission from Tannast et al. [9], Figs. 1 and 2)
Rotation on the AP view is normal when the center of the scj is in line with the symphysis pubis. The two points shift away from each other with rotation; rotation is described as the distance of this shift [9] (Fig. 10b). As the hip and ipsilateral pelvis rotate posteriorly, all the impingement signs increase on that side [8] (Fig. 8c). Thus, measurements are confused and less reliable when the position of the X-ray beam is not centered exactly over the center of the pelvis and/or the pelvis cannot be positioned in neutral tilt and rotation. Therefore, when retroversion is suspected from the AP view, it is necessary to turn to other studies for clarification and accuracy.
MRI identifies the pathology of the labrum of the hip, as well as the extent of cartilage coverage of the femoral head. Radial MRI cuts can map the area as well as degree of cartilage damage of both the femoral head and acetabulum [4].
CT depicts the transverse position of the anterior and posterior acetabulum (the version) and the degree of coverage of the femoral head. This allows the direct measurement of acetabular version [5]. The acetabulum is usually stated as normally open 20° anteriorly [6]. However, CT permits measuring the version of the top (cranial), middle (central), and lower (caudal) portions of the acetabulum. Jamali et al. [5] found that significant differences normally occur in the version values at these different levels. The mean normal cranial anteversion is 8° and the mean central and caudal anteversion are both 20° (Fig. 11). This 12° difference is normally present between cranial and central or caudal version. Usually, central version is measured [5]. However, because of these differences, any stated degree of version should also report the level in the acetabulum from which it was made.
Fig. 11.
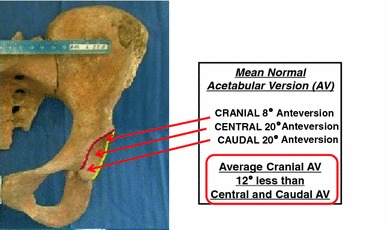
Acetabular version at the cranial, central, and caudal acetabulum. Cranial version is 12° less than the central and caudal acetabular version (modified with permission from Jamali et al. [5], Fig. 3)
This study demonstrates that, if the central measurement is below 10° of anteversion, the cranial part of the acetabulum will be retroverted 100% of the time. If the central anteversion is between 10° and 20°, cranial retroversion occurs 30% of the time. If central anteversion is greater than 20°, cranial retroversion occurs in only 1 of 45 cases [5]. Since most anterior impingement occurs towards the top of the acetabulum (zones 2 and 3), this is significant [10] (Fig. 12).
Fig. 12.
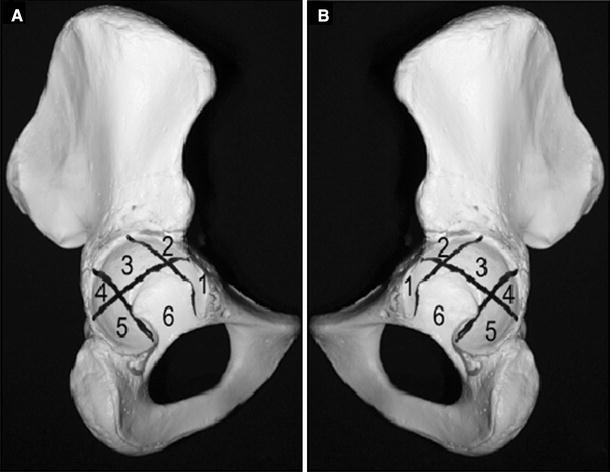
Acetabular zones. Right and left hemipelvis zones: (1) antero-inferior; (2) antero-superior; (3) central superior; (4) postero-superior; (5) postero-inferior; (6) central inferior (reproduced with permission from Ilizaliturri et al. [10], Fig. 3)
According to Ganz, the crossover sign seen on regular X-ray, when compared to CT, was found to be approximately 90% specific but less sensitive [5]. This has been further clarified by 3D-CT in two studies by Dandachli et al. [11, 12]. This method takes into consideration pelvic tilt and rotation. Using 3D-CT, the reliability of the crossover and posterior wall signs was measured. The crossover sign was sensitive enough to identify 92% of the retroverted hips. However, its specificity was low (55%), with just over half of the anteverted hips being identified as retroverted [12]. For example, 41 of 64 hips had a crossover sign but only 24 of the 41 (58%) had true retroversion [12].
This study also found that there was no difference in the amount of coverage of the femoral head in anteverted and retroverted acetabuli [12]. These acetabuli were retroverted at the expense of posterior coverage. This further emphasizes the need for CT evaluation of cases suspected of FAI. However, that is different from when the continued presence of anterior impingement causes secondary changes in the anterior boney structure with osteophyte formation; in effect, there is anterior elongation or enlargement. The retroversion is then due to an actual increase in the amount of anterior acetabulum (with additional femoral head being covered) [6]. In this instance, the anterior and posterior coverage of the head change independently of one another [6].
If the posterior wall is far lateral to the center of the femoral head, it is usually a sign of increased acetabular anteversion. In such instances, the anterior acetabulum will be deficient unless anterior osteophytes formation occurs [4]. Impingement, when it occurs, is due to femoral pathology.
The contrecoup lesion, in which the cartilage of the posterior surface of the acetabulum is damaged, is considered to be a major cause of change leading to arthritis [4]. This occurs when the femoral head, impinged anteriorly by the retroverted acetabulum, is thrust against the posterior acetabulum, damaging the cartilage.
Using 3D-CT, the frequency that pincer and cam combine as causes for impingement was observed. Thirty-eight percent (38%) of cam impingement cases had retroverted acetabuli with signs of pincer. Fifty-four percent (54%) of retroverted acetabuli had femoral pathology with signs of cam impingement, thus, confirming the frequent association of both pincer and cam [12].
In the symptomatic patient, the progress towards accurate diagnosis is, therefore, not a simple matter. These studies emphasize the need for carefully positioned patients, X-rays and/or beam position. If FAI is entertained from these standard films, properly positioned CT and/or 3D-CT should be used prior to definitive diagnosis and treatment.
Acetabular dysplasia
Classically, acetabular dysplasia is associated with uncovering of the anterior and lateral femoral head. 3D-CT studies show that in the normal hip, 71% of the femoral head is covered. In the dysplastic hip, 58% is covered [11, 12] (Fig. 13). How can there be an acetabular cause for impingement anteriorly in cases of hip dysplasia? The answer is that retroversion occurs; the anterior acetabulum moves anteriorly and laterally and the posterior wall moves anteriorly and medially. The coverage remains at 58% [11, 12] (Fig. 14). The frequency of retroversion in dysplastic hips is noted in three studies, two between 17.2 and 18.3%. In the third study, the frequency of 37% retroversion in dysplastic hips highlights the importance of how tilt is measured. Here, the distance between the variably positioned tip of the coccyx to the symphysis is used instead of the scj to symphysis) [3, 13, 14].
Fig. 13.
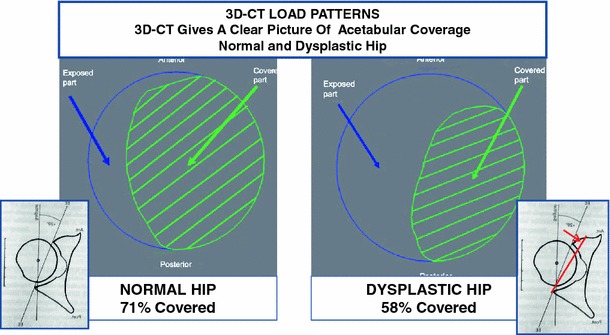
Extent of femoral head coverage in normal and dysplastic hips—computed tomography (CT) mapping. Blue circle femoral head, green oval acetabular size and position. Normal hip: 71% of the femoral head covered. Dysplastic hip: 58% of the femoral head covered with decreased anterior coverage (modified with permission from Dandachli et al. [11], Fig. 3a, b, and Reynolds et al. [6], Fig. 4)
Fig. 14.

Femoral head coverage in retroverted dysplastic hips—CT mapping. Blue circle femoral head, green oval dysplastic acetabular size and position, red oval retroverted and dysplastic acetabular size and position. With retroversion and dysplasia, the percentage of femoral head coverage remains the same. Coverage remaining the same, as the anterior wall moves further anterior and the posterior wall moves anterior as well. Thus, with retroversion and dysplasia, acetabular insufficiency is greater posteriorly (modified with permission from Dandachli et al. [11], Fig. 3b)
Radiographically, an important difference between the dysplastic and non-dysplastic hip with retroversion is the size of the posterior wall sign. The marked increase of that sign indicates a large decrease of posterior coverage. The posterior wall becomes the dysplastic area! [6] (Fig. 15). Therefore, a large posterior wall sign probably indicates acetabular dysplasia.
Fig. 15.
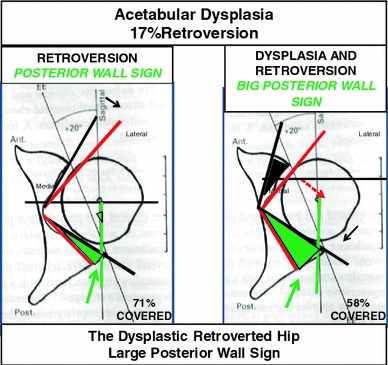
Acetabular CT images of retroversion versus retroversion accompanying dysplasia. In the dysplastic retroverted hip, the posterior acetabular wall becomes the dysplastic area, as evidenced by a large posterior wall sign (modified with permission from Reynolds et al. [6], Fig. 4)
Ganz noted morphologic changes in the anterior acetabulum in dysplasia, including retroversion, hypertrophy and tearing of the labrum, fatigue fractures of the rim, and degeneration with ganglion formation within the labrum, the capsule, and/or the adjacent acetabular bone [15, 16].
In the group of dysplastic hips with 18% retroversion reported by Fujii et al., pain occurred earlier (27.9 years of age) in the retroverted hips as compared to those dysplastic hips without retroversion (40.5 years of age), regardless of the severity of the dysplasia. They attributed the pain to posterior uncovering associated with retroversion and did not consider anterior impingement as a cause [17].
Acetabular dysplasia can be associated with various femoral deformities such as coxa valga (44%), post-VDO coxa vara (4%), aspherical femoral head (72%), and insufficient head–neck offset (4%) [18]. In instances of acetabular retroversion and dysplasia, the version of the femur can influence the likelihood of symptomatic FAI. For example, acetabular dysplasia associated with femoral head offset or coxa vara increases the likelihood of FAI and coxa valga decreases it.
Iatrogenic causes of FAI
Surgical procedures performed to correct acetabular dysplasia have the potential of creating or increasing retroversion. The classical procedures of Salter, Steel, and Sutherland increase anterior and lateral acetabular coverage, rotating the acetabulum from a point anterior to the joint. In doing so, as the anterior acetabulum moves anterior and lateral, the posterior acetabulum moves anterior and medial. The resultant vector retroverts the acetabulum [12] (Fig. 16). In this regard, the recent study of the degree of retroversion after innominate osteotomy from the Hospital for Sick Children (HSC) in Toronto is of interest [19]. Their study indicates an increase in the acetabular retroversion of 7°, which, they stated, was similar to the series reported by Dora et al. [20], in which, however, there was more evidence of persistent retroversion. The age-related remodeling potential of acetabular retroversion is seen by comparing these two studies. Remodeling was affected by the age at the time of osteotomy. In the study reported by the HSC, cases operated upon at 2.8 years showed long-term evidence of remodeling towards normal. In the series by Dora et al., cases operated at 4.5 years showed persistence of the retroversion. This may explain why we see fewer instances of retroversion after these osteotomies when done at a very young age than expected.
Fig. 16.
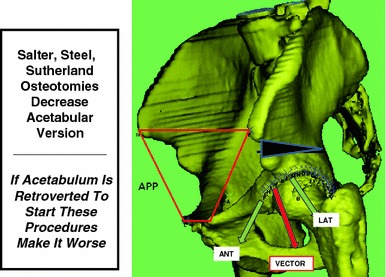
Acetabular osteotomies can cause retroversion. Salter, Steel, and Sutherland osteotomies move the acetabulum anterior and lateral (green arrows). The vector (red arrow) shows the resulting retroversion (modified with permission from Dandachli et al. [11], Fig. 1)
If retroversion is already present, as in the approximately 18% of hip dysplasia described above, the retroversion is made worse with these procedures [11, 12]. In procedures such as the Tönnis and Ganz periacetabular osteotomies, in which the movement of the acetabulum can be more accurately controlled, transverse rotation can correct the retroversion. The importance of this transverse correction is emphasized in this example of impingement where there is inadequate transverse correction after a Tönnis osteotomy seen in Fig. 17 [11, 12].
Fig. 17.
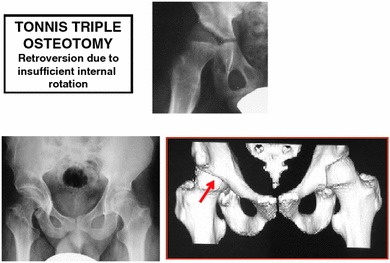
Tönnis with retroversion due to insufficient internal rotation
Cam impingement
Cam impingement occurs more frequently in men (M:F 14:1), average age 32 years, when the head–neck offset is decreased [4]. This causes limited internal rotation of the femur with terminal impingement. Impingement mostly occurs on the upper portions of the acetabulum; the area of femoral head cartilage damage is noted from 11 to 3 o’clock. The most common instances of such occurrence are seen in slipped proximal femoral epiphysis, Legg–Perthes disease, coxa vara, pistol grip deformity, head tilt deformity, femoral retroversion, and growth anomalies of the epiphysis [4].
These conditions all have in common reduced head–neck offset and/or reduced femoral version. The pistol grip deformity, horizontal growth plate, and a CCD (caput–collum–diaphyseal, i.e., the head–neck–shaft) angle less than 125° are signs on the AP X-ray view. Lateral X-ray measurements of the femoral head and neck taken in neutral rotation include head-neck offset, alpha angle, and beta angle. A head–neck offset of over 8 mm is considered to be diagnostic of cam. The alpha angle measures the degree of offset and the beta angle measures the degree at which the offset impinges on the acetabulum (at 90° of hip flexion).
The alpha angle is measured by placing a circle around the femoral head, one line along the center of the femoral neck and another line from where the first line meets the center of the femoral head to the point where the boney edge of the anterior head meets the circle. The normal alpha angle for men is 68° or less and for women, it is 50° or less [4, 21, 22].
The beta angle is the angular distance in degrees from the edge of the acetabulum to the point just before a concentric femoral head circle is disrupted by the offset. This should be done at 90° of flexion [23]; normal is 30°–57° and FAI is present at 15° (range 1°–29°).
Retroversion of the femoral neck, suspected clinically, is best measured by CT version studies. The angular pitch of the femoral neck (angle made between the line of the neck and the horizontal) is measured against the femoral condyle angle (the angle made between a line connecting the back of the condyles and the horizontal) [4]. These causes of labral impairment from cam impingement will be further discussed in the subsequent review of the labrum.
Combined pincer and cam
Cam and pincer deformities frequently occur together (86%). The entities that most often cause both cam and pincer impingements are slipped proximal epiphysis and Legg–Perthes disease [4]. Siebenrock et al. [14] reported that 24 of 26 cases undergoing periacetabular (PAO) surgery had cam with an abnormal head–neck offset. In 60 cases with surgery for cam, Espinosa et al. reported that all 60 had acetabular surgery, 25 rim and labrum resection, and 35 rim resection and labrum reattachment [24]. As stated above, Dandachli et al. [12], using 3D-CT, found that 38% of cases with cam also had acetabular retroversion and in 54% of cases of pincer, cam was also noted. Sink et al. [25] reported 30 girls and 5 boys, all with chronic hip pain related to sports. They found 43% pincer, 6% cam, and 51% combined causes of the pain in this group of patients. The proportion of cam to pincer appears to be related to the patient mix. For example, when more cases have had a slipped epiphysis, more head–neck offset, or other cause for pistol grip, more cam impingement is noted.
Understanding of the reasons why Perthes causes both cam and pincer impingement FAI was furthered by Kim and Novais in 2011 [26]. Acetabular dysplasia occurs secondarily as a result of the enlarged femoral head in Perthes. Kim and Wenger [27] described the head as really being in two parts. The antero-lateral part is uncovered, enlarged, and stops internal rotation. The postero-medial part, representing the original head, articulates with the misshapen acetabulum. This is the articular part head; it is retroverted in relation to the femoral neck, causing functional retroversion. This plus the associated coxa breva and prominent greater trochanter perpetuate FAI. Sankar and Flynn reported that Perthes in immature hips, the acetabulum is anteverted. However, as the patients matured, retroversion occurred in 31% of their cases, mostly in the severe cases [28]. Snow et al. [29] reported four cases of impingement due to the enlarged Perthes head as early as 1993.
Discussion
What, then, is the acetabular version of the asymptomatic hip? 3D-CT examination of “normal” hips revealed 12 of 36 cases with acetabular retroversion from 5 to 12.5°. The average mid-acetabular anteversion of 19.9° was confirmed on skeletons by Maeyama, but the range of 7° to 42° did not indicate a symptomatic state. Therefore, it becomes important to know when the retroverted acetabulum becomes symptomatic. This is clearly answered in Tönnis and Heinecke’s study [2]. It depends on the version of the femur. Any decrease in functional femoral antetorsion will always cause symptoms if there is any acetabular retroversion; it is the main cause of impingement symptoms.
It is of interest that a recent study of military femoral neck fractures recognized the implication of retroversion. 31 of 57 soldiers with neck fractures had retroversion, resulting in an impingement fracture [30].
Genetics has a significant influence on the occurrence of FAI. Pollard et al. revealed that the siblings of patients with FAI have a significantly greater likelihood of having a similar problem. Siblings of patients with cam were 2.8 times more likely to have cam problems and those of patients with pincer were 2 times more likely to have pincer problems than the general population. In addition, both are more likely to be bilateral and symptomatic [31].
This review has described the characteristics of the hip that cause FAI. Emphasis has been placed on understanding that the femoral and acetabular components normally function as a unit, complementing each other. Considered independent of each other, conflict may be occurring, hindering function, and not be apparent. The increasing frequency of making this diagnosis based on abnormal anatomy on one side of the joint, often in face of unclear physical findings, can bring the diagnosis into question. Knowing how to analyze the hip, knowing the limitations of various available clinical and diagnostic studies, and recognizing the continued and ever-changing bulk of literature is important and challenging. This primer is just the beginning.
Conflict of interest
None of the authors received financial support for this study.
References
- 1.Lavigne M, Parvizi J, Beck M, Siebenrock KA, Ganz R, Leunig M. Anterior femoroacetabular impingement: part I. Techniques of joint preserving surgery. Clin Orthop Relat Res. 2004;418:61–66. doi: 10.1097/00003086-200401000-00011. [DOI] [PubMed] [Google Scholar]
- 2.Tönnis D, Heinecke A. Acetabular and femoral anteversion: relationship with osteoarthritis of the hip. J Bone Joint Surg Am. 1999;81:1747–1770. doi: 10.2106/00004623-199912000-00014. [DOI] [PubMed] [Google Scholar]
- 3.Kalberer F, Sierra RJ, Madan SS, Ganz R, Leunig M. Ischial spine projection into the pelvis: a new sign for acetabular retroversion. Clin Orthop Relat Res. 2008;466:677–683. doi: 10.1007/s11999-007-0058-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Tannast M, Siebenrock KA. Conventional radiographs to assess femoroacetabular impingement. Instr Course Lect. 2009;58:203–212. [PubMed] [Google Scholar]
- 5.Jamali AA, Mladenov K, Meyer DC, Martinez A, Beck M, Ganz R, Leunig M. Anteroposterior pelvic radiographs to assess acetabular retroversion: high validity of the “cross-over-sign”. J Orthop Res. 2007;25:758–765. doi: 10.1002/jor.20380. [DOI] [PubMed] [Google Scholar]
- 6.Reynolds D, Lucas J, Klaue K. Retroversion of the acetabulum. A cause of hip pain. J Bone Joint Surg Br. 1999;81:281–288. doi: 10.1302/0301-620X.81B2.8291. [DOI] [PubMed] [Google Scholar]
- 7.Tannast M, Siebenrock KA, Anderson SE. Femoroacetabular impingement: radiographic diagnosis—what the radiologist should know. AJR Am J Roentgenol. 2007;188:1540–1552. doi: 10.2214/AJR.06.0921. [DOI] [PubMed] [Google Scholar]
- 8.Siebenrock KA, Kalbermatten DF, Ganz R. Effect of pelvic tilt on acetabular retroversion: a study of pelves from cadavers. Clin Orthop Relat Res. 2003;407:241–248. doi: 10.1097/00003086-200302000-00033. [DOI] [PubMed] [Google Scholar]
- 9.Tannast M, Zheng G, Anderegg C, Burckhardt K, Langlotz F, Ganz R, Siebenrock KA. Tilt and rotation correction of acetabular version on pelvic radiographs. Clin Orthop Relat Res. 2005;438:182–190. doi: 10.1097/01.blo.0000167669.26068.c5. [DOI] [PubMed] [Google Scholar]
- 10.Ilizaliturri VM, Jr, Byrd JW, Sampson TG, Guanche CA, Philippon MJ, Kelly BT, Dienst M, Mardones R, Shonnard P, Larson CM. A geographic zone method to describe intra-articular pathology in hip arthroscopy: cadaveric study and preliminary report. Arthroscopy. 2008;24:534–539. doi: 10.1016/j.arthro.2007.11.019. [DOI] [PubMed] [Google Scholar]
- 11.Dandachli W, Kannan V, Richards R, Shah Z, Hall-Craggs M, Witt J. Analysis of cover of the femoral head in normal and dysplastic hips: new CT-based technique. J Bone Joint Surg Br. 2008;90:1428–1434. doi: 10.1302/0301-620X.90B11.20073. [DOI] [PubMed] [Google Scholar]
- 12.Dandachli W, Islam SU, Liu M, Richards R, Hall-Craggs M, Witt J. Three-dimensional CT analysis to determine acetabular retroversion and the implications for the management of femoro-acetabular impingement. J Bone Joint Surg Br. 2009;91:1031–1036. doi: 10.1302/0301-620X.91B8.22389. [DOI] [PubMed] [Google Scholar]
- 13.Kiyama T, Naito M, Shiramizu K, Shinoda T. Postoperative acetabular retroversion causes posterior osteoarthritis of the hip. Int Orthop. 2009;33:625–631. doi: 10.1007/s00264-007-0507-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Siebenrock KA, Schoeniger R, Ganz R. Anterior femoro-acetabular impingement due to acetabular retroversion. Treatment with periacetabular osteotomy. J Bone Joint Surg Am. 2003;85:278–286. doi: 10.2106/00004623-200302000-00015. [DOI] [PubMed] [Google Scholar]
- 15.Ganz R, Leunig M. Morphological variations of residual hip dysplasia in the adult. Hip Int. 2007;17(Suppl 5):S22–S28. [PubMed] [Google Scholar]
- 16.Li PL, Ganz R. Morphologic features of congenital acetabular dysplasia: one in six is retroverted. Clin Orthop Relat Res. 2003;416:245–253. doi: 10.1097/01.blo.0000081934.75404.36. [DOI] [PubMed] [Google Scholar]
- 17.Fujii M, Nakashima Y, Yamamoto T, Mawatari T, Motomura G, Matsushita A, Matsuda S, Jingushi S, Iwamoto Y. Acetabular retroversion in developmental dysplasia of the hip. J Bone Joint Surg Am. 2010;92:895–903. doi: 10.2106/JBJS.I.00046. [DOI] [PubMed] [Google Scholar]
- 18.Clohisy JC, Nunley RM, Carlisle JC, Schoenecker PL. Incidence and characteristics of femoral deformities in the dysplastic hip. Clin Orthop Relat Res. 2009;467:128–134. doi: 10.1007/s11999-008-0481-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Barnes JR, Thomas SR, Wedge J. Acetabular coverage after innominate osteotomy. J Pediatr Orthop. 2011;31:530–533. doi: 10.1097/BPO.0b013e31821991ee. [DOI] [PubMed] [Google Scholar]
- 20.Dora C, Mascard E, Mladenov K, Seringe R. Retroversion of the acetabular dome after Salter and triple pelvic osteotomy for congenital dislocation of the hip. J Pediatr Orthop B. 2002;11:34–40. doi: 10.1097/00009957-200201000-00006. [DOI] [PubMed] [Google Scholar]
- 21.Beaulé PE, O’Neill M, Rakhra K. Acetabular labral tears. J Bone Joint Surg Am. 2009;91:701–710. doi: 10.2106/JBJS.H.00802. [DOI] [PubMed] [Google Scholar]
- 22.Hack K, Di Primio G, Rakhra K, Beaulé PE. Prevalence of cam-type femoroacetabular impingement morphology in asymptomatic volunteers. J Bone Joint Surg Am. 2010;92:2436–2444. doi: 10.2106/JBJS.J.01280. [DOI] [PubMed] [Google Scholar]
- 23.Brunner A, Hamers AT, Fitze M, Herzog RF. The plain beta-angle measured on radiographs in the assessment of femoroacetabular impingement. J Bone Joint Surg Br. 2010;92:1203–1208. doi: 10.1302/0301-620X.92B9.24410. [DOI] [PubMed] [Google Scholar]
- 24.Espinosa N, Beck M, Rothenfluh DA, Ganz R, Leunig M. Treatment of femoro-acetabular impingement: preliminary results of labral refixation. Surgical technique. J Bone Joint Surg Am. 2007;89:36–53. doi: 10.2106/JBJS.F.01123. [DOI] [PubMed] [Google Scholar]
- 25.Sink EL, Gralla J, Ryba A, Dayton M. Clinical presentation of femoroacetabular impingement in adolescents. J Pediatr Orthop. 2008;28:806–811. doi: 10.1097/BPO.0b013e31818e194f. [DOI] [PubMed] [Google Scholar]
- 26.Kim YJ, Novais EN. Diagnosis and treatment of femoroacetabular impingement in Legg–Calvé–Perthes disease. J Pediatr Orthop. 2011;32(2 Suppl):S235–S240. doi: 10.1097/BPO.0b013e3182260252. [DOI] [PubMed] [Google Scholar]
- 27.Kim HT, Wenger DR. “Functional retroversion” of the femoral head in Legg–Calvé–Perthes disease and epiphyseal dysplasia: analysis of head–neck deformity and its effect on limb position using three-dimensional computed tomography. J Pediatr Orthop. 1997;17:240–246. doi: 10.1097/00004694-199703000-00019. [DOI] [PubMed] [Google Scholar]
- 28.Sankar WN, Flynn JM. The development of acetabular retroversion in children with Legg–Calvé–Perthes disease. J Pediatr Orthop. 2008;28:440–443. doi: 10.1097/BPO.0b013e318168d97e. [DOI] [PubMed] [Google Scholar]
- 29.Snow SW, Keret D, Scarangella S, Bowen JR. Anterior impingement of the femoral head: a late phenomenon of Legg–Calvé–Perthes’ disease. J Pediatr Orthop. 1993;13:286–289. doi: 10.1097/01241398-199305000-00002. [DOI] [PubMed] [Google Scholar]
- 30.Kuhn KM, Riccio AI, Saldua NS, Cassidy J. Acetabular retroversion in military recruits with femoral neck stress fractures. Clin Orthop Relat Res. 2010;468:846–851. doi: 10.1007/s11999-009-0969-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Pollard TC, Villar RN, Norton MR, Fern ED, Williams MR, Murray DW, Carr AJ. Genetic influences in the aetiology of femoroacetabular impingement: a sibling study. J Bone Joint Surg Br. 2010;92:209–216. doi: 10.1302/0301-620X.92B2.22850. [DOI] [PubMed] [Google Scholar]


