Abstract
Purpose
Magnetic resonance imaging (MRI) has been successfully used in the determination of the adequacy of the surgical reduction of congenitally dislocated hips in children. We present the results of a prospective series of patients treated conservatively. MRI was performed in all hips after positioning was deemed adequate on radiographs after spica cast application. The goal of this study was to evaluate the usefulness of MRI in this indication.
Methods
After the study was approved by our local ethics committee, 31 patients for a total of 36 dislocated hips were included. After the traction period, hip testing was performed and a hip spica cast was applied under general anaesthesia. All children had MRI within 1 week of reduction, without the need for contention or general anaesthesia. Hip reduction was assessed on axial and coronal MRI images.
Results
The concentric reduction of the hip was confirmed in 30 cases out of 36. In three cases, the dislocation was retrospectively suspected on radiographs and then confirmed. In the three remaining cases, hip dislocation was only diagnosed on MRI.
Conclusions
MRI screening of congenitally dislocated hips after reduction procedures is a safe and reliable procedure to assess the concentric reduction of the hip. Even in doubtful cases, MRI detected persistent hip dislocations and was conducive to iterative reduction and satisfactory outcome and result.
Keywords: Congenital dislocation of the hip, MRI, Conservative treatment, Hip spica cast, Traction
Introduction
Assessment of the reduction of developmental dysplasia of the hip (DDH) has depended on radiography [1], arthrography [2, 3], ultrasound [4–6] or computed tomography (CT) examination [1, 7]. Neither radiography nor CT adequately images the cartilaginous femoral head, and its position must be extrapolated from that of the proximal femoral metaphysis [2, 8]. Even if the femoral head is partially ossified, its position cannot be assumed to be central. In conservative treatment, the interpretation of plain radiographs is even more demanding, especially due to spica cast interpositions and poorly ossified femoral head. In conservative treatment, arthrography was proposed but requires general anaesthesia [2]. Other alternative techniques such as ultrasonography remain of poor reliability [2]. Magnetic resonance imaging (MRI) has already been used in the determination of the adequacy of the surgical reduction of the dislocation of an immature hip [9–13]. Hip MRI protocols in post-reduction DDH patient assessment provides fast and adequate images without additional anaesthesia requirements or radiation exposure [9–13]. Since 2004, we have routinely used two-dimensional MRI in the coronal and axial planes to evaluate the adequacy of closed reduction of DDH in children. We present the results of a prospective series of patients treated conservatively for a DDH. Because in such treatment, the adequacy of reduction of the femoral head could be difficult to assess by conventional radiographs, MRI was performed after hip position was deemed adequate on radiographs after spica cast application. The aim of this study was to evaluate the usefulness of MRI in the determination of the adequacy of conservative reduction of the dislocation of an immature hip.
Materials and methods
After approval of the study by our local ethics committee, 31 children (4 boys and 27 girls) aged from 2.1 to 33.9 months were enrolled from 2004 to 2010. The diagnosis of DDH was made at birth in six cases and at various ages (from 2 weeks to 31 months) in the other cases. The DDH was right-sided in ten cases, left-sided in 16 cases and bilateral in five cases (Fig. 2a). A total of 36 dislocated hips was then included in the study. In 12 patients, a first conservative treatment by abduction diaper, traction or Pavlik harness was attempted but did not achieve and maintain concentric reduction of the dislocated hip. Conservative treatment was attempted in all the cases by zenith (90° hip flexed) traction over a period of 15 days in children under the age of 10 months (21 patients) or bed longitudinal traction over a period of 30 days (Somerville technique) in children older than 10 months (10 patients). The mean age at the onset of treatment was 9.7 months (range 2.1–33.9 months). After the traction period, hip testing was performed under general anaesthesia, confirming subluxation of the hip, and documenting reducibility and stability of the hip in various positions. Then, a hip spica cast was applied, taking into account the best stability position. A frontal radiograph of the pelvis was performed in every case before (Figs. 1a and 2b) and after hip a spica cast was applied (Figs. 1b and 2c) to assess the quality of hip reduction.
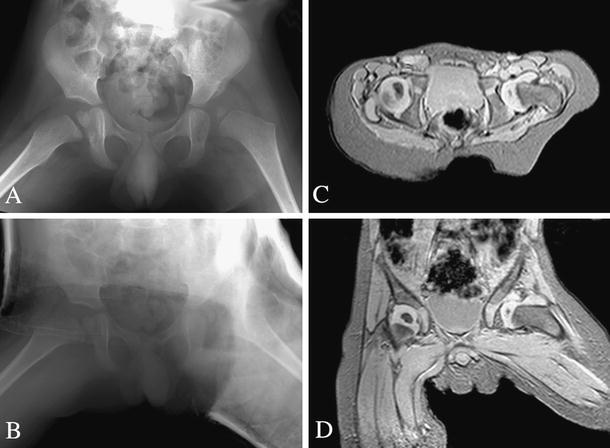
Fig. 2.
a Frontal radiograph of bilateral DDH in a 5-month-old girl (patient 18). b Post-traction frontal radiograph under general anaesthesia before hip spica cast application. c Same incidence after hip spica cast application showing concentric reduction in both hips. d Axial MRI image showing persistent dislocation of the right hip and reduction of the left hip e Coronal MRI image showing persistent dislocation of the right hip and reduction of the left hip
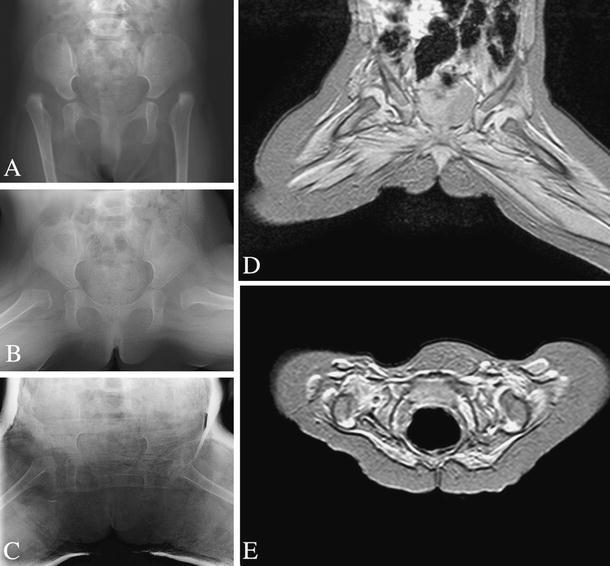
Fig. 1.
Left unilateral developmental dysplasia of the hip (DDH) in a 9-month-old girl (patient 20). a Post-traction frontal radiograph under general anaesthesia before hip spica cast application. b Same incidence after hip spica cast application showing concentric reduction of the left hip. c Axial magnetic resonance imaging (MRI) scan showing concentric reduction of the left hip. d Coronal MRI image showing concentric reduction of the left hip
All children had MRI within 1 week of reduction. Images were obtained using a 1.5-T MRI system (Achieva®; Royal Philips Electronics, the Netherlands). Both hips were explored with the same protocol. The MRI examination was carried without any sedation or general anaesthesia. All children were fed immediately prior to imaging and some examinations were then made during natural sleep in good conditions. In the other cases, the children were placed in a supine position in the hip spica cast and some restraints were applied (wrap around technique). After a localiser, axial and coronal sequences in T2-weighted fast field echo [repetition time (TR) 226 ms; echo time (TE) 9.6 ms; flip angle 25°; voxel size 1.12 × 1.39 × 3.5 mm; a time of acquisition of 3 min 02 s was obtained in all cases. Additional sequences at the radiologist’s request were performed: coronal and/or sagittal T1-weighted (T1-W) turbo-spin-echo (TSE) images (TR/TE 732/18 ms; voxel size 0.9 × 1.17 × 4 mm; turbo factor 3; time of acquisition 1 min 35 s).
All MRI scans were evaluated by three senior surgeons (MB, CT-L and RV). Analysis was performed on a dedicated workstation (Kodak Carestream® PACS). Hip reduction was studied in the axial and coronal planes by assessing the position of the femoral head in relation to the triradiate cartilage of the acetabulum.
Results
The hip reduction was documented by frontal radiographs made under general anaesthesia prior to and after the application of a hip spica cast in all the cases. In 12 cases, the quality of radiographs was noted as being poor and responsible for difficulties in assessing the concentric reduction of the hip. In three cases, persistent dislocation was suspected on frontal radiographs made after cast application. In all the cases, MRI was done without the need for contention or general anaesthesia. The quality of MRI scans was noted as being good in all the cases by the three examiners. The concentric reduction of the hip was confirmed in 30 cases out of 36 (Fig. 1c, d). In six cases, hip dislocation was diagnosed on coronal (Fig. 2d) and axial (Fig. 2e) images. In three cases, the dislocation was previously suspected on radiographs and then confirmed. In the three remaining cases, despite good-quality radiographs in two cases, hip dislocation was only diagnosed on MRI (Table 1).
Table 1.
Epidemiological data
| Patient number | Gender | Side | Age at diagnosis (months) | First treatment | Age at treatment (months) | Treatment | Frontal radiographs quality | X-ray result | Delay before MRI (days) | MRI result |
|---|---|---|---|---|---|---|---|---|---|---|
| 1 | M | Right | 0 | Traction | 7.6 | Zenith traction (15 days)—spica cast | Poor | Reduction OK | 1 | Hip dislocation |
| 2 | F | Left | 0.5 | None | 5.6 | Zenith traction (15 days)—spica cast | Good | Reduction OK | 1 | Concentric reduction |
| 3 | F | Left | 13 | None | 15.8 | Axial traction and progressive reduction (30 days)—spica cast | Poor | Reduction OK | 1 | Concentric reduction |
| 4 | F | Left | 1 | Abduction diaper/traction/Pavlik harness | 5.4 | Zenith traction (15 days)—spica cast | Good | Reduction OK | 0 | Concentric reduction |
| 5 | F | Right | 0 | Abduction diaper/traction/Pavlik harness | 9.7 | Zenith traction (15 days)—spica cast | Good | Reduction OK | 2 | Concentric reduction |
| 6 | M | Left | 1 | None | 8.4 | Zenith traction (15 days)—spica cast | Poor | Reduction OK | 0 | Concentric reduction |
| 7 | F | Left | 3 | Abduction diaper/traction/Pavlik harness | 4.5 | Zenith traction (15 days)—spica cast | Poor | Dislocation suspected | 0 | Hip dislocation |
| 8 | F | Left | 0 | None | 30.6 | Axial traction and progressive reduction (30 days)—spica cast | Good | Reduction OK | 1 | Concentric reduction |
| 9 | F | Left | 8 | Abduction diaper/traction | 13.8 | Axial traction and progressive reduction (30 days)—spica cast | Good | Dislocation suspected | 1 | Hip dislocation |
| 10 | F | Right | 8 | None | 10.4 | Axial traction and progressive reduction (30 days)—spica cast | Poor | Reduction OK | 2 | Concentric reduction |
| 11 | F | Bilateral | 5 | None | 10.2 | Axial traction and progressive reduction (30 days)—spica cast | Poor | Reduction OK | 1 | Concentric reduction |
| 12 | F | Right | 0 | None | 33.9 | Axial traction and progressive reduction (30 days)—spica cast | Good | Reduction OK | 1 | Concentric reduction |
| 13 | F | Right | 10 | None | 12.0 | Axial traction and progressive reduction (30 days)—spica cast | Good | Reduction OK | 8 | Concentric reduction |
| 14 | F | Right | 1.5 | None | 2.1 | Zenith traction (15 days)—spica cast | Good | Reduction OK | 1 | Concentric reduction |
| 15 | F | Left | 4 | None | 5.4 | Zenith traction (15 days)—spica cast | Good | Reduction OK | 2 | Concentric reduction |
| 16 | F | Right | 0 | None | 6.6 | Zenith traction (15 days)—spica cast | Good | Reduction OK | 0 | Concentric reduction |
| 17 | F | Bilateral | 0 | Abduction diaper | 5.0 | Zenith traction (15 days)—spica cast | Poor | Reduction OK | 2 | Concentric reduction |
| 18 | F | Bilateral | 0 | Abduction diaper | 5.0 | Zenith traction (15 days)—spica cast | Good | Reduction OK | 1 | Hip dislocation |
| 19 | F | Bilateral | 0 | Abduction diaper | 4.7 | Zenith traction (15 days)—spica cast | Poor | Reduction OK | 1 | Concentric reduction |
| 20 | F | Left | 0.5 | None | 9.0 | Zenith traction (15 days)—spica cast | Good | Reduction OK | 2 | Concentric reduction |
| 21 | F | Left | 3 | None | 4.6 | Zenith traction (15 days)—spica cast | Good | Reduction OK | 1 | Concentric reduction |
| 22 | F | Left | 4 | None | 6.5 | Zenith traction (15 days)—spica cast | Good | Reduction OK | 1 | Concentric reduction |
| 23 | F | Right | 18 | None | 19.9 | Axial traction and progressive reduction (30 days)—spica cast | Poor | Reduction OK | 1 | Concentric reduction |
| 24 | F | Right | 6 | Abduction diaper | 7.5 | Zenith traction (15 days)—spica cast | Poor | Reduction OK | 0 | Concentric reduction |
| 25 | F | Left | 0 | None | 5.3 | Zenith traction (15 days)—spica cast | Good | Reduction OK | 2 | Concentric reduction |
| 26 | F | Left | 0 | Abduction diaper | 5.8 | Zenith traction (15 days)—spica cast | Good | Reduction OK | 0 | Concentric reduction |
| 27 | F | Right | 4 | Pavlik harness | 6.2 | Zenith traction (15 days)—spica cast | Good | Reduction OK | 1 | Concentric reduction |
| 28 | F | Left | 0 | None | 11.6 | Axial traction and progressive reduction (30 days)—spica cast | Poor | Reduction OK | 2 | Concentric reduction |
| 29 | F | Left | 17 | None | 19.3 | Axial traction and progressive reduction (30 days)—spica cast | Poor | Dislocation suspected | 1 | Hip dislocation |
| 30 | M | Left | 1 | None | 3.2 | Zenith traction (15 days)—spica cast | Good | Reduction OK | 1 | Hip dislocation |
| 31 | M | Bilateral | 1.5 | Pavlik harness | 6.3 | Zenith traction (15 days)—spica cast | Poor | Reduction OK | 1 | Concentric reduction |
Patients diagnosed with persistent hip dislocation had another hip testing and hip spica cast application under general anaesthesia and then MRI scanning to assess hip reduction. In three cases, the hip reduction was successful using conservative treatment. In the three other cases, because of remaining hip instability following closed reduction, an open reduction and stabilisation was performed. All patients who were treated conservatively wore two successive hip spica casts for a total period of 3 months and then progressive return to weight-bearing and normal gait and activities.
At final follow-up (from 18 to 76 months), no patient had persistent hip dislocation. Four patients have undergone pelvic innominate osteotomy of Salter for residual acetabular dysplasia around the age of 5 months.
Discussion
Imaging methods of DDH include frontal radiographs, arthrography, ultrasonography or CT scan. If neither radiographs nor CT scan adequately shows the cartilaginous femoral head in younger patients, then its position must be extrapolated from that of the proximal femoral metaphysis [11]. Even if the bony nucleus of the femoral head is present, its position cannot be assumed to be central, which then leads to misdiagnoses of the hip and unsatisfactory reduction. Arthrography is an invasive technique that requires general anaesthesia and articular function. It is widely used before the reduction of a dislocated hip, but it cannot be repeated once the spica is in place [11]. CT scan is responsible for pelvis X-ray exposure and must be avoided in routine practice, especially in young children [7]. Although ultrasonography is informative about the position of the femoral head in newborns, the accuracy of this technique drastically decreases in older children with calcified structures. In young children, it is possible to use ultrasound to assess the hip after reduction, but it is difficult once a spica has been applied [5]. MRI is a superior soft-tissue contrast resolution which allows differentiation between articular structures such as bone, hyaline and fibrous cartilage, ligaments, joint capsule, intra-articular tissues and fluids [14–16]. The appearance of the paediatric hip has been widely documented in control patients and in DDH cases [9–13, 17–24].
The ability to carry out some angular measurements of bony and cartilaginous landmarks of the acetabulum should be kept in mind. As a matter of fact, MRI could be a powerful examination to quantify the degree of dysplasia found in dislocated hips [25]. Such information could be obtained from this series in terms of head coverage and a study is currently being conducted in our department to assess which anatomical factors are determinants for hips requiring early osteotomy.
In our study, the advantage of the post-operative hip spica in keeping an infant still for MRI investigation must be stressed. No child taking part in this study required sedation for their MRI screening thanks to the presence of the spica. For children not in a spica undergoing MRI examination for other conditions, general anaesthesia is required.
We found MRI to be a precise and useful way for assessing the adequacy of reduction of the femoral head in DDH. Despite the fact that we used limited pelvic sequences, we reported a total pelvic MRI charge of approximately $450. Although pelvic MRI is more expensive than CT or conventional radiograph examinations, we feel that such reduced charges are reasonable.
Concentric reduction and dislocation are easily documented, especially in difficult cases or in case of poor-quality radiographs. In the current series, 12 patients had poor-quality radiographs made after hip spica cast application, making it difficult to prove the concentric reduction of the hip. Especially in the three suspicious cases, MRI was able to clearly depict residual dislocation. The three remaining dislocated hips had not been suspected by hip testing or frontal radiographs made under general anaesthesia, even if radiographs made after hip spica cast applications were considered as informative and of good quality. In these three remaining cases, MRI detected persistent hip dislocations and was conducive to iterative reduction and satisfactory outcome and result. Because proximal femoral focal deficiency can masquerade as hip dysplasia, because the femoral head does not ossify and because of plaster superposition, the radiographic appearance may also be deceiving and be responsible for a high false-negative rate and failure to detect hip luxation.
We stress the importance of such systematic MRI screening of congenitally dislocated hips after reduction procedures in order to avoid occult dislocation or incomplete reduction responsible for inadequate acetabular remodelling or persistent dislocation. We do not agree with Laor et al. that a simple visualisation of the capital femoral epiphysis in contact with the posterior margin of the acetabulum is sufficient to confirm adequate reduction of the hip [26]. We found it mandatory to confirm the centred position of the femoral head into the acetabulum on coronal and axial views passing through the triradiate cartilage. An interposition of labral elements, between the epiphysis and the fossa, even if the head itself is centred, could be recognised on MRI and lead to supplementary repositioning procedures. A key component to implement this procedure in one institution is the timely communication between the surgical team and the MRI technologists to reduce the delay between the DDH reduction and MRI assessment. The MRI department has to be notified of the time of the spica cast procedure in advance. Nevertheless, some technical or medical reasons could generate schedule disturbances and additional delay before MRI screening. This was the case in one of our patients (patient 13) who had MRI on day 8 because of technical reasons. In these cases, clinicians should be aware of the possibility of secondary hip dislocation in a severe hip dysplasia, in which the spica cast was not efficient enough to maintain centralisation of the hip.
In conclusion, our MRI protocol in post-reduction DDH patient assessment provides fast and adequate images without additional anaesthesia requirements or radiation exposure. MRI appears as a “gold standard” to early depict residual dislocation after closed treatment of DDH. In these cases, another hip testing and hip spica cast application under general anaesthesia should be performed.
References
- 1.Donaldson JS, Feinstein KA. Imaging of developmental dysplasia of the hip. Pediatr Clin North Am. 1997;44:591–614. doi: 10.1016/S0031-3955(05)70495-8. [DOI] [PubMed] [Google Scholar]
- 2.Grissom L, Harcke HT, Thacker M. Imaging in the surgical management of developmental dislocation of the hip. Clin Orthop Relat Res. 2008;466:791–801. doi: 10.1007/s11999-008-0161-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Gerscovich EO. A radiologist’s guide to the imaging in the diagnosis and treatment of developmental dysplasia of the hip. I. General considerations, physical examination as applied to real-time sonography and radiography. Skeletal Radiol. 1997;26:386–397. doi: 10.1007/s002560050253. [DOI] [PubMed] [Google Scholar]
- 4.Roposch A, Wright JG. Increased diagnostic information and understanding disease: uncertainty in the diagnosis of developmental hip dysplasia. Radiology. 2007;242:355–359. doi: 10.1148/radiol.2422051937. [DOI] [PubMed] [Google Scholar]
- 5.Harcke HT (2005) Imaging methods used for children with hip dysplasia. Clin Orthop Relat Res (434):71–77 [DOI] [PubMed]
- 6.Roberts CS, Beck DJ Jr, Heinsen J, Seligson D (2002) Review article: diagnostic ultrasonography: applications in orthopaedic surgery. Clin Orthop Relat Res (401):248–264 [DOI] [PubMed]
- 7.Atar D, Lehman WB, Grant AD. 2-D and 3-D computed tomography and magnetic resonance imaging in developmental dysplasia of the hip. Orthop Rev. 1992;21:1189–1197. [PubMed] [Google Scholar]
- 8.Pirpiris M, Payman KR, Otsuka NY. The assessment of acetabular index: is there still a place for plain radiography? J Pediatr Orthop. 2006;26:310–315. doi: 10.1097/01.bpo.0000214920.54619.c7. [DOI] [PubMed] [Google Scholar]
- 9.Ranawat V, Rosendahl K, Jones D. MRI after operative reduction with femoral osteotomy in developmental dysplasia of the hip. Pediatr Radiol. 2009;39:161–163. doi: 10.1007/s00247-008-1071-y. [DOI] [PubMed] [Google Scholar]
- 10.Westhoff B, Wild A, Seller K, Krauspe R. Magnetic resonance imaging after reduction for congenital dislocation of the hip. Arch Orthop Trauma Surg. 2003;123:289–292. doi: 10.1007/s00402-003-0518-8. [DOI] [PubMed] [Google Scholar]
- 11.Duffy CM, Taylor FN, Coleman L, Graham HK, Nattrass GR. Magnetic resonance imaging evaluation of surgical management in developmental dysplasia of the hip in childhood. J Pediatr Orthop. 2002;22:92–100. [PubMed] [Google Scholar]
- 12.Omeroğlu H. MRI after operative reduction for developmental dysplasia of the hip. J Bone Joint Surg Br. 1998;80:556. [PubMed] [Google Scholar]
- 13.McNally EG, Tasker A, Benson MK. MRI after operative reduction for developmental dysplasia of the hip. J Bone Joint Surg Br. 1997;79:724–726. doi: 10.1302/0301-620X.79B5.7772. [DOI] [PubMed] [Google Scholar]
- 14.Remes V, Tervahartiala P, Helenius I, Peltonen J. Magnetic resonance imaging analysis of hip joint development in patients with diastrophic dysplasia. J Pediatr Orthop. 2002;22:212–216. [PubMed] [Google Scholar]
- 15.Suzuki S, Kashiwagi N, Seto Y, Mukai S. Location of the femoral head in developmental dysplasia of the hip: three-dimensional evaluation by means of magnetic resonance image. J Pediatr Orthop. 1999;19:88–91. [PubMed] [Google Scholar]
- 16.Petersilge CA. Current concepts of MR arthrography of the hip. Semin Ultrasound CT MR. 1997;18:291–301. doi: 10.1016/S0887-2171(97)80020-0. [DOI] [PubMed] [Google Scholar]
- 17.Yüksel HY, Yilmaz S, Aksahin E, Celebi L, Duran S, Muratli HH, Biçimoğlu A. The evaluation of hip muscles in patients treated with one-stage combined procedure for unilateral developmental dysplasia of the hip: part I: MRI evaluation. J Pediatr Orthop. 2009;29:872–878. doi: 10.1097/BPO.0b013e3181c29cc9. [DOI] [PubMed] [Google Scholar]
- 18.Tiderius C, Jaramillo D, Connolly S, Griffey M, Rodriguez DP, Kasser JR, Millis MB, Zurakowski D, Kim YJ. Post-closed reduction perfusion magnetic resonance imaging as a predictor of avascular necrosis in developmental hip dysplasia: a preliminary report. J Pediatr Orthop. 2009;29:14–20. doi: 10.1097/BPO.0b013e3181926c40. [DOI] [PubMed] [Google Scholar]
- 19.Steppacher SD, Tannast M, Werlen S, Siebenrock KA. Femoral morphology differs between deficient and excessive acetabular coverage. Clin Orthop Relat Res. 2008;466:782–790. doi: 10.1007/s11999-008-0141-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Mitchell PD, Chew NS, Goutos I, Healy JC, Lee JC, Evans S, Hulme A. The value of MRI undertaken immediately after reduction of the hip as a predictor of long-term acetabular dysplasia. J Bone Joint Surg Br. 2007;89:948–952. doi: 10.1302/0301-620X.89B7.18751. [DOI] [PubMed] [Google Scholar]
- 21.Watanabe W, Itoi E, Sato K. Intra-articular membranous interposition detected by MRI in developmental dysplasia of the hip. Skeletal Radiol. 2000;29:726–728. doi: 10.1007/s002560000293. [DOI] [PubMed] [Google Scholar]
- 22.Tennant S, Kinmont C, Lamb G, Gedroyc W, Hunt DM. The use of dynamic interventional MRI in developmental dysplasia of the hip. J Bone Joint Surg Br. 1999;81:392–397. doi: 10.1302/0301-620X.81B3.8964. [DOI] [PubMed] [Google Scholar]
- 23.Greenhill BJ, Hugosson C, Jacobsson B, Ellis RD. Magnetic resonance imaging study of acetabular morphology in developmental dysplasia of the hip. J Pediatr Orthop. 1993;13:314–317. doi: 10.1097/01241398-199305000-00007. [DOI] [PubMed] [Google Scholar]
- 24.Dwek JR. The hip: MR imaging of uniquely pediatric disorders. Magn Reson Imaging Clin N Am. 2009;17:509–520. doi: 10.1016/j.mric.2009.03.003. [DOI] [PubMed] [Google Scholar]
- 25.Douira-Khomsi W, Smida M, Louati H, Hassine LB, Bouchoucha S, Saied W, Ladeb MF, Ghachem MB, Bellagha I. Magnetic resonance evaluation of acetabular residual dysplasia in developmental dysplasia of the hip: a preliminary study of 27 patients. J Pediatr. 2010;30:37–43. doi: 10.1097/BPO.0b013e3181c877d7. [DOI] [PubMed] [Google Scholar]
- 26.Laor T, Roy DR, Mehlman CT. Limited magnetic resonance imaging examination after surgical reduction of developmental dysplasia of the hip. J Pediatr Orthop. 2000;20:572–574. doi: 10.1097/01241398-200009000-00005. [DOI] [PubMed] [Google Scholar]


