Abstract
One barrier to genetic testing is the lack of access to genetic counselors. We provided cancer genetic counseling via telephone, through a pilot project for employees of a national health insurer, Aetna, Inc. Knowledge transfer, behavioral intentions, and patient satisfaction were assessed by survey after genetic counseling. Aetna sent an individual email to its employees nationwide notifying them of the availability of a new telephone genetic counseling and testing program and providing a link to take a brief screening questionnaire to determine whether they may be at risk of hereditary cancer. Employees completing the questionnaire received immediate feedback regarding whether there appeared to be a risk of hereditary cancer. If so, they were invited to schedule a telephonic genetic counseling session. After the session, respondents completed an online survey. 397 individuals completed the questionnaire. 39 proceeded with telephone genetic counseling, and 22 completed the follow-up survey, including all 11 women with family history warranting genetic testing. One third reported prior discussion about inherited cancer risk with their primary care provider (PCP); 12% were referred to a geneticist; 20% had an accurate perception of their own cancer risk. After counseling, 94% reported understanding their risk for cancer and 87% were aware of available risk-reduction strategies. 87% of high-risk respondents intended to engage in risk-management interventions. 93% reported high satisfaction. 66% indicated they would not have pursued genetic counseling if it had not been available by phone. Results suggest telephone counseling is a viable option for increasing access to genetic experts. In this sample, telephone counseling increases knowledge of cancer risk, motivates intention to change health-related behaviors, and elicits a high satisfaction level. Consequently, Aetna now offers telephone cancer genetic counseling nationwide as a covered benefit.
Keywords: BRCA 1/2, Cancer genetic counseling, Cancer risk assessment, Genetic testing, Hereditary cancer, Telephone genetic counseling
Introduction
National guidelines exist for appropriate referral of individuals to cancer genetic counseling and testing services [1]. NCCN guidelines state that referrals for genetic risk assessment and counseling should be made to cancer genetics professionals such as board-certified genetic counselors [1].
Commonly cited barriers to obtaining professional genetic counseling and testing include the lack of access to genetics experts [2]. In the United States, there are only 32 accredited genetic counseling graduate programs [3] and approximately 2400 board-certified genetic counselors. Approximately 500 of these specialists offer services related to adult diseases, including cancer [2]. The majority of these specialists reside in academic settings where they may be inaccessible to large population groups.
Other limitations of traditional genetic counseling include: (1) traditional genetic counseling requires at least one in-person visit taking up to 2 h to complete. Most cancer genetic counseling centers require a second office visit to discuss the results of any genetic testing performed; (2) appointments are only scheduled during typical office hours, may involve traveling a distance, and many counseling centers have long wait-times (months) for appointments.
Genetic counseling via telephone has been proposed to address these issues. Potential advantages include: (1) broader accessibility to trained genetic experts; (2) flexible appointment scheduling, including evenings and weekends; (3) decreased travel time and expense. Telephone-based genetic counseling may also be more acceptable to community health care providers who are reluctant to refer and potentially lose patients to a regional cancer genetic counseling center.
A number of studies conducted primarily at academic research institutions have compared telephone genetic counseling with face-to-face counseling, with favorable results. These studies showed that telephone genetic counseling is well received and similar to face-to-face counseling in decreasing worry [4], producing more accurate perception of risk [4], completeness of information provided [5], and patient satisfaction [6]. In fact, patients may prefer to receive telephone genetic counseling due to shorter wait times [6].
This innovative pilot project explores the acceptability and outcomes of telephone genetic counseling for hereditary cancer. Although several studies have been conducted in the research setting to assess delivery of cancer genetic counseling by telephone, those studies may not reflect “real world” or “real-patient” experience. This pilot, a collaboration between Aetna, Inc. (Aetna) and Informed Medical Decisions, Inc. (Informed), was conducted among Aetna’s 35,000 employees [7]. The primary aim was to address the satisfaction of participants with genetic counseling by board-certified genetic counselors via telephone. Additionally, this study assessed patients’ perceptions of the way the health care system evaluates cancer risk. It detected changes in patients’ knowledge of their hereditary cancer risk and of available medical management options. It detected intentions to change health behaviors after the genetic counseling session. It also explored the patients’ interactions with their physician after genetic counseling, and their assessment of privacy/confidentiality, and insurance-related issues.
Methods
All Aetna employees received an individual email notifying them that: formal genetic counseling was available via telephone through Informed, Aetna’s contracted provider of telephonic cancer genetic counseling services; genetic counseling and testing were covered medical benefits for employees who met certain criteria; and all communications with Informed were confidential and test results would not be shared with Aetna. Interested individuals were directed to complete a 5-question hereditary cancer-risk screening tool (Table 1).
Table 1.
Brief online risk screening tool
You or any close family member, has had cancer diagnosed at an early age including
|
You, or any close family member, has been diagnosed with more than one cancer. Examples include
|
You, or any close family member, has been diagnosed with a rare cancer or rare pre-cancerous finding, such as
|
Two or more people in your family have been diagnosed with the same type of cancer (such as 2 or more family members diagnosed with colon cancer) or related cancers. This might be
|
| You have any Ashkenazi (Eastern European) Jewish ancestry in your family. If so, you or a family member has had a diagnosis of breast, ovarian, or pancreatic cancer at any age |
| A health care provider has talked to you or a close family member about hereditary cancer |
Based on their answers, individuals with the potential for hereditary cancer received a message that their risk for cancer may be elevated and they may benefit from genetic counseling. The secure website guided participants through an online family and personal medical history questionnaire typically used by genetic counselors to assess hereditary risk. Answers were used to produce a three-generation pedigree viewable by Informed’s genetic counselor. Participants were guided through a simple online process to schedule an appointment. At the scheduled appointment time, a board-certified genetic counselor (Heather Shappell) called the patient and conducted a full genetic counseling session. This session included:
Review/verification of the family history provided in the online survey
Outline of risk factors for inherited forms of cancer
Personalized cancer risk assessment
Review of genetic testing criteria (appropriateness of genetic testing)
Informed consent for genetic testing (when indicated)
Discussion of personalized screening and risk reduction recommendations
No visual aids or other material were used.
Eligible individuals who chose to pursue testing were mailed a test kit (Myriad Genetic Laboratories, Inc.) containing all necessary information for the member’s designated physician to order the test. The designated ordering physician received a summary of the genetic consultation describing the patient’s desire to test, the details of the test ordering, and applicable paperwork pre-completed by the genetic counselor. The patients were instructed to schedule a brief visit and blood draw with their physician and to take the completed test kit to their doctor’s office for his/her signature. Test results were mailed directly to Informed. Informed contacted the patient by e-mail to schedule a telephone result disclosure. At the scheduled time, the Informed counselor called the patient to disclose and review the results, including personalized risk estimates and risk management options based on the genetic test results and the individual’s personal and family history. For every patient, their Informed genetic counselor provided a written summary of the information discussed during their telephone consult(s), a copy of their 3-generation pedigree and genetic test results (if pursued), and risk management/reduction recommendations. The patient’s summary letter and attachments were mailed to their chosen physician. The content of the genetic consult and test results were not shared with Aetna. Genetic counseling and testing were covered benefits for participants and subject to their health insurance benefits plan, with applicable co-payments and deductibles applied.
Within 1–2 months of completing their telephone genetic counseling, each participant was asked to complete a web-based survey. The survey covered four domains: baseline knowledge of personal genetic risk and experience in the health care system regarding genetic risk assessment; knowledge transfer as a result of formal genetic counseling; utility of the information provided during the genetic counseling session(s); and satisfaction and assurance of confidentiality with the services provided. For questions related to knowledge prior to genetic counseling, respondents were asked to rate their responses to each question using a Likert-type response format (1 = good, 2 = average, 3 = poor). For the remaining items, including post-counseling knowledge, behavioral intentions, satisfaction, and confidentiality/privacy, respondents were asked to rate their responses using a Likert-type response format (1 = strongly agree, 2 = agree, 3 = don’t know, 4 = disagree, 5 = strongly disagree). For analysis, responses were collapsed into 3 categories: (1) those who responded strongly agree or agree and (2) those who responded strongly disagree or disagree (3) not certain.
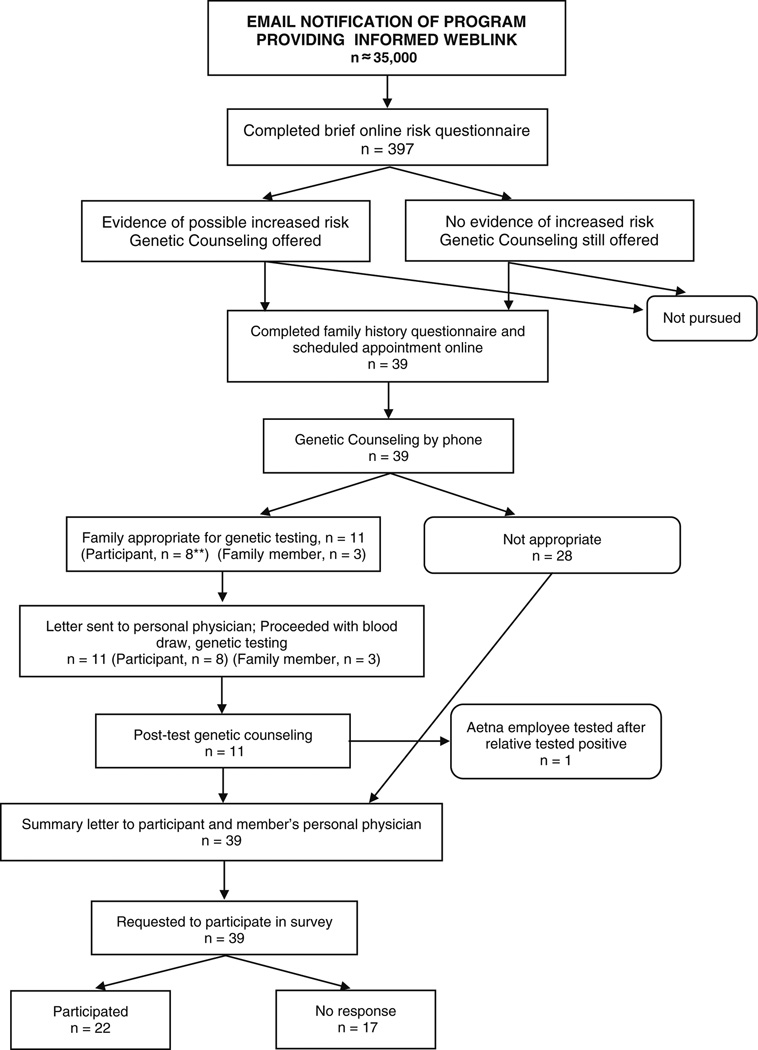
The project flow chart is seen in Fig. 1.
Fig. 1.
Project flow chart
Eleven participants met Aetna’s coverage criteria to proceed with genetic testing at the time of the initial genetic consultation. In 3 of 11 cases, Informed recommended that an affected relative would be the most appropriate person to be tested first. Aetna pays for other relatives to be tested if the test results are used to support a covered member’s care. Relative testing was completed in each of these three cases. One relative tested positive and the Aetna member then tested “true negative”. The other two relatives tested negative; thus, no testing was indicated in the Aetna member.
Although designed as a 3-year project, the positive responses to the program during the initial six months prompted Aetna to suspend the pilot and offer the services nationwide as a covered benefit to their entire membership. Deidentified data from the 6-month pilot was analyzed under approval of University of South Florida Institutional Review Board.
Results
Demographic characteristics (Table 2)
Table 2.
Demographic and clinical characteristics of respondents (N = 22)
| Variable | % (N) |
|---|---|
| Demographic characteristics | |
| Age | |
| 20–29 | 9.1 (2) |
| 30–39 | 9.1 (2) |
| 40–49 | 40.9 (9) |
| 50–59 | 27.3 (6) |
| 60–69 | 9.1 (2) |
| Unknown | 4.5 (1) |
| Race | |
| White, Not Hispanic | 81.8 (18) |
| White, Hispanic | 4.5 (1) |
| Ashkenazi Jewish | 9.1 (2) |
| Unknown | 4.5 (1) |
| Gender | |
| Female | 90.9 (20) |
| Male | 4.5 (1) |
| Unknown | 4.5 (1) |
| Clinical characteristics | |
| Personal cancer history | |
| None | 68.2 (15) |
| Cervical | 4.5 (1) |
| Breast | 13.6 (3) |
| Ovarian | 4.5 (1) |
| Skin | 4.5 (1) |
| Unknown | 4.5 (1) |
| Age at Diagnosis | |
| 20–29 | 4.5 (1) |
| 30–39 | 4.5 (1) |
| 40–49 | 9.1 (2) |
| 50–59 | 9.1 (2) |
| 60–69 | 0 (0) |
| Unknown | 4.5 (1) |
| FDRas with Cancer | 72.7 (16) |
| SDRas with Cancer | 59.1 (13) |
First degree relative (FDR)/second degree relative (SDR)
All Aetna employees (n ≈ 35,000) received notification of the program via email and the employee newsletter. Based on mutation prevalence estimates, we expected approximately 117 employees to have an elevated hereditary cancer risk. 397 employees completed the brief online screening tool. Thirty-nine of these employees pursued telephone genetic counseling, none of whom had previously had cancer genetic counseling. For 11 (31%) of the 39, either the participant or a family member was eligible for BRCA 1/2 genetic testing (no individuals met criteria for other genetic tests.) In all cases, either the Aetna member or the affected relative pursued genetic testing and all were women. Of the 3 relatives eligible for testing, 2 tested negative for hereditary cancer gene mutations and one tested positive for a BRCA gene mutation. None of the Aetna members tested positive for a hereditary cancer gene mutation and one was considered a “true negative” after a positive BRCA test in her relative. Of the 39 Aetna employees who completed genetic counseling, 22 (56%) responded to the post-counseling survey, including all individuals who underwent testing.
The largest fraction of respondents was between 40 and 49 years old, followed by those 50 to 59 years old. Most were white, non-Hispanic females. Approximately two-thirds (68.2%) had no personal cancer history while the rest reported a personal diagnosis of cervical, breast, ovarian or skin cancer. The most common reason for seeking genetic counseling was having a relative with a history of cancer [3]. Only one respondent reported having no family history of cancer but a personal cancer history.
Survey results (Table 3)
Table 3.
Survey results
| Knowledge: before Informed genetic counseling | Good | Average | Poor | |
| My risk for hereditary cancer | 5 | 12 | 5 | |
| The role of genetic tests to determine my risk for developing hereditary cancer | 6 | 12 | 4 | |
| Specific cancer screening recommendations (such as colonoscopies and mammograms) for people who are at risk for a hereditary cancer | 13 | 9 | 0 | |
| Specific actions (such as surgery or taking medications) that can be taken to reduce the risk of developing a hereditary cancer | 8 | 9 | 5 | |
| Knowledge: after Informed genetic counseling | Agree | Disagree | Not certain | No answer |
| My understanding of my risk for a hereditary cancer has increased | 19 | 0 | 2 | 1 |
| I am more knowledgeable about how a genetic test can help determine my risk for getting a hereditary cancer | 20 | 0 | 1 | 1 |
| I am more aware of specific cancer screening options available to me because of a cancer that runs in my family | 18 | 1 | 2 | 1 |
| I am more aware of specific actions to reduce my risk of getting of a cancer that runs in my family | 16 | 2 | 3 | 1 |
| Based on the results of my counseling session, I understand that I am at risk for or have a hereditary cancer | 5 | 13 | 3 | 1 |
| Behavioral intentions | Agree | Disagree | Not certain | No answer |
| I am planning to get earlier and more frequent cancer screening | 17 | 1 | 3 | 1 |
| I will take specific actions to reduce my risk | 19 | 1 | 1 | 1 |
| I have decided to change a specific behavior to reduce my risk | 10 | 10 | 1 | 1 |
| I have decided to have earlier/more frequent cancer screenings | 9 | 11 | 1 | 1 |
| I have decided to start one cancer reducing action (e.g. mastectomy) or medication (e.g. Tamoxifen) not considered before | 0 | 19 | 1 | 2 |
| Do you plan to share this information with at least one family member | 18 | 2 | 0 | 2 |
| As a result of learning that I am not at risk for a hereditary cancer, I plan to delay cancer screening or skip a behavior meant to reduce my cancer risk | 0 | 15 | 5 | 2 |
| Satisfaction | Agree | Disagree | Not certain | No answer |
| My genetic counselor seemed to understand the stresses I was facing | 18 | 0 | 0 | 4 |
| My genetic counselor helped me to identify what I needed to know to make decisions about what would happen | 16 | 0 | 2 | 4 |
| I feel better about my health after talking with my genetic counselor | 16 | 0 | 2 | 4 |
| The genetic counselor spent the right amount of time with me | 18 | 0 | 0 | 4 |
| My genetic counselor was truly concerned about my well-being | 16 | 1 | 1 | 4 |
| The telephone is an acceptable way to access genetic counseling for hereditary cancer | 17 | 0 | 1 | 4 |
| I was able to communicate adequately with the genetic counselor during my telephone call | 16 | 0 | 2 | 4 |
| I would not have pursued cancer genetic counseling if it had not been available by telephone | 12 | 2 | 4 | 4 |
| I feel that it is appropriate that Aetna provides access and.coverage for Informed cancer genetic counseling service | 18 | 0 | 1 | 3 |
| I feel that it is appropriate that Aetna provides access and coverage for cancer genetic counseling | 16 | 0 | 3 | 3 |
| I would have preferred genetic counseling in person | 3 | 8 | 7 | 4 |
| Informed Website | 14 | 2 | 2 | 4 |
| On-line information regarding hereditary cancer | 16 | 0 | 2 | 4 |
| Satisfaction | Agree | Disagree | Not certain | No answer |
| On-line personal and family history tool | 13 | 3 | 2 | 4 |
| On-line appointment scheduling process | 16 | 1 | 1 | 4 |
| Initial telephone genetic counseling session | 17 | 0 | 1 | 4 |
| The amount of time it took to get my genetic test results | 11 | 1 | 6 | 4 |
| The information provided in the Informed summary letter | 13 | 2 | 3 | 4 |
| The telephone counseling session to discuss my genetic test results | 11 | 1 | 6 | 4 |
| Informed communication tools to use with your family member to explain your test results | 10 | 2 | 6 | 4 |
| Overall level of satisfaction | 16 | 1 | 1 | 4 |
| I would recommend Informed genetic counseling service to a relative or friend concerned about hereditary cancer | 16 | 2 | 0 | 4 |
| Confidentiality/privacy | Agree | Disagree | Not certain | No answer |
| I believe that Aetna will protect the confidentiality and privacy of my personal health information | 17 | 0 | 1 | 4 |
| Confidentiality was maintained during the process of entering personal and family health information via the web | 16 | 0 | 2 | 4 |
| Confidentiality was maintained during my phone call with the genetic counselor | 17 | 0 | 1 | 4 |
| Confidentiality was maintained in written communication to me and/or my physician | 14 | 0 | 4 | 4 |
| Confidentiality was maintained in email communications with Informed | 14 | 0 | 4 | 4 |
| Confidentiality was maintained in any interaction with Aetna | 16 | 0 | 2 | 4 |
Prior to genetic counseling, the majority rated their knowledge of their hereditary cancer risk, the role of genetic testing to determine risk, and risk reduction options as average to poor. Less than one-third reported that their physician had recommended enhanced cancer screening or risk reduction options. More participants rated their knowledge of general population screening recommendations as average to good. Upon completion of the session, their knowledge in each of these areas improved.
Regarding intentions to change behavior, most respondents planned to engage in earlier, more frequent screenings and take specific actions to reduce their risk. The majority planned to share test results with relatives and felt their results would not make them more likely to delay or not engage in a particular cancer screening behavior.
Overall, most participants were satisfied with the genetic counseling process including the rapport with the genetic counselor, time spent in the session, and the counselor’s empathy. Most reviewed the phone counseling favorably, agreeing that the phone session was acceptable, allowed for appropriate communication with the genetic counselor, and was convenient. Participants were satisfied with the Informed website, scheduling process, and summary letter.
Discussion
Previous research has demonstrated positive results regarding knowledge gained and satisfaction with cancer genetic counseling by telephone but these assessments were conducted in the research setting and highlighted the need for further study in more representative populations [5]. To our knowledge, this is the first study to evaluate theses issues in a “real world” scenario.
Knowledge
Many physicians do not feel they have the training or time to assess hereditary cancer risk in patients [8]. Although 89% of respondents reported that their physician had taken a family cancer history, the majority reported that their physicians never discussed their cancer risk or recommended more frequent screenings. The respondents who perceived themselves at risk of hereditary cancer after genetic counseling were those with a family history meeting eligibility criteria for testing and, 60% reported that their doctor had not discussed genetic testing with them. Less than one-third of respondents reported that their physician recommended a behavior change or enhanced cancer screenings (data not shown).
Research shows that an individual’s perceived cancer risk may be higher than their actual risk, as assessed by a genetic expert [9]. Genetic counseling can assist individuals in gaining a more realistic understanding of their cancer risk and what options are available. Half of the respondents reported being concerned about hereditary cancer prior to genetic counseling through Informed. An ideal outcome of this pilot project would be to increase the patient’s knowledge of their cancer risk and make them aware of preventative measures and screening appropriate for them based on their individual risks. Before telephone genetic counseling, over 20% of the respondents reported below average knowledge of their risk for a hereditary cancer and or/specific actions to reduce this risk. After counseling, over 90% of respondents reported improved understanding of their personal cancer risks, as well as a greater knowledge of their genetic testing, risk-reduction and screening options. This increase in knowledge demonstrates a positive impact of telephone genetic counseling on risk perception, understanding and management.
Intentions to change behavior
Over 75% of respondents reported being the first in their family to receive genetic counseling. After genetic counseling, all of the respondents whose risk was sufficiently high to warrant genetic testing either pursued or (for the three who had a relative more appropriate for testing) reported that they considered genetic testing for themselves.
In successful genetic counseling, the behavioral intentions of a patient after genetic testing should be appropriately aligned with their test results. A positive test result provides an individual the opportunity to take proactive steps to prevent the onset of cancer. Genetic counseling can also help individuals who have an inflated risk perception gain a more realistic assessment of their actual risks. After telephone genetic counseling, 87% of the respondents planned to take specific actions to reduce their risk through behaviors such as increasing physical activity and eating a healthier diet, whether they had genetic testing or not. The majority of individuals who perceived themselves at risk for hereditary cancer after counseling planned to pursue enhanced cancer screenings while those who did not perceive themselves at high risk did not plan on stopping or decreasing their cancer screening below that recommended for the general population.
Satisfaction
Patient satisfaction is critical in assessing feasibility and acceptability of telephone-based genetic counseling. Visual cues and body language are absent in a telephone counseling session; therefore a counselor must be perceptive to a patient’s vocal cues and tone of voice [10] in order to ensure the patient understands the information presented and feels comfortable during the session. Eighteen respondents (81%) indicated that their genetic counselor seemed to understand their stress and spent the right amount of time with them. Sixteen respondents (72%) reported that the information relayed to them during the sessions helped them in making decisions about their healthcare. Over 70% of the respondents reported that the counselor communicated an effective cancer-risk management plan.
Only one respondent did not consider the telephone acceptable for genetic counseling. In fact, the majority indicated that they would not have pursued genetic counseling had it not been available by telephone. Over 70% of the respondents indicated that they would recommend Informed’s telephone genetic counseling services.
Confidentiality/privacy
Individuals may be concerned that their genetic information may be used by health insurance companies to discriminate against them. Employer-sponsored health insurance plans in the private sector provide health insurance for more than 50% of Americans [11]. Since Aetna was both the employer and health insurance provider for the respondents, concerns about privacy and confidentiality were important in determining the success of telephone genetic counseling. All respondents indicated that it was appropriate for Aetna as both their health insurance provider and employer to provide them with access to and coverage for Informed’s cancer genetic counseling service for genetic testing. The majority also felt that Aetna would protect the confidentiality and privacy of their information.
Ensuring confidentiality when conducting genetic counseling via the telephone is important [10]. The participants in this pilot believed that their health information was kept confidential throughout the genetic counseling and testing process, while entering their personal and family history information via the website, during their telephone call with the genetic counselor, in written communications with them and their physicians, as well as in email communications.
Study limitations
Due to the small size of the study the results must be considered exploratory. Limited enrollment may have been due to limited notification about the newly-offered service. It is unknown whether concerns regarding the program being offered by the employer may also have contributed to relatively low enrollment. Among participants, more than 20% reported having inadequate awareness of their risk for hereditary cancer. Thus, overall lack of baseline understanding of cancer risk could have been a contributing factor.
The mostly white, non-Hispanic respondents reflect the current profile of individuals being referred for genetic counseling [12]. Many researchers are studying ways to improve access for underserved populations.
The participants in this pilot were employees of Aetna and pursued genetic counseling after receiving notification of its availability through their employer. The participants may not be representative of individuals in the community who pursue genetic counseling because they or their doctors perceive them to be at high risk. No participants were newly diagnosed patients with cancer—it will be important to assess the impact of telephone genetic counseling services in this group, in addition to expansion of the assessment in other aspects. Since no tested individual had positive results, this pilot study only evaluated for negative results—it is possible that different results might be obtained from respondents with positive genetic test results. Additionally, the project did not track employees who went directly to their doctor without using Informed.
Conclusion
The goals of traditional genetic counseling such as patient comprehension of risk, genetic testing options, and the understanding of appropriate management plans were accomplished through this telephone delivery model. In addition to increased knowledge and appropriate changes in relevant behavioral intentions, subjects also reported satisfaction with Informed’s telephone cancer genetic counseling services. Importantly, most of the respondents reported that they would not have pursued cancer genetic counseling if it had not been available by telephone.
Informed’s telephone genetic counseling service is a viable and important option for increasing access to cancer genetic experts. Preliminary results suggest that this delivery model increases knowledge of hereditary cancer risk, and results in a high level of satisfaction, as well as intentions to utilize screening and risk-reducing behaviors that are appropriate based on the information exchanged during genetic counseling.
Telephone delivery of cancer genetic counseling may represent an ideal model for increasing access to this important healthcare service.
Contributor Information
Rebecca Sutphen, Email: rebecca.sutphen@epi.usf.edu, University of South Florida College of Medicine, Tampa, FL, USA.
Barbara Davila, Email: bdavila@mail.usf.edu, University of South Florida College of Medicine, Tampa, FL, USA.
Heather Shappell, Informed Medical Decisions, Inc., St. Petersburg, FL, USA.
Tricia Holtje, Email: tricia.holtje@epi.usf.edu, University of South Florida College of Medicine, Tampa, FL, USA.
Susan Vadaparampil, Email: susan.vadaparampil@moffitt.org, H. Lee Moffitt Cancer Center & Research Institute, Tampa, FL, USA.
Sue Friedman, Facing Our Risk of Cancer Empowered, Inc., http://www.facingourrisk.org/.
Michele Toscano, Aetna, Inc., Hartford, CT, USA.
Joanne Armstrong, Aetna, Inc., Hartford, CT, USA.
References
- 1.National Comprehensive Cancer Network Cancer Guidelines for Patients and Physicians by Cancer Experts. 2010 [Google Scholar]
- 2.Women’s Health: Issues Surrounding Cancer Risk Assessment for Hereditary Breast and Ovarian Cancer and BRCA 1/2 Genetic Testing, Research Forum of the Society of Women’s Health Research White Paper. 2007 [Google Scholar]
- 3.Elements of Cancer Genetics Risk Assessment and Counseling, National Cancer Institute, U.S. Nationals Institutes of Health. 2008 [Google Scholar]
- 4.Helmes AW, Culver JO, Bowen DJ. Results of a randomized study of telephone versus in-person breast cancer risk counseling. Patient Educ Couns. 2006;64:96–103. doi: 10.1016/j.pec.2005.12.002. [DOI] [PubMed] [Google Scholar]
- 5.Peshkin BN, Demarco TA, Graves KD, et al. Telephone genetic counseling for high-risk women undergoing BRCA1 and BRCA2 testing: rationale and development of a randomized controlled trial. Genet Test. 2008;12:37–52. doi: 10.1089/gte.2006.0525. [DOI] [PubMed] [Google Scholar]
- 6.Baumanis L, Evans JP, Callanan N, et al. Telephoned BRCA1/2 genetic test results: prevalence, practice, and patient satisfaction. J Genet Couns. 2009;18:447–463. doi: 10.1007/s10897-009-9238-8. [DOI] [PubMed] [Google Scholar]
- 7.Aetna At-A-Glance. Aetna facts. Hartford: Aetna, Inc; 2007. [Google Scholar]
- 8.Wideroff L, Freedman AN, Olson L, et al. Physician use of genetic testing for cancer susceptibility: results of a national survey. Cancer Epidemiol Biomarkers Prev. 2003;12:295–303. [PubMed] [Google Scholar]
- 9.Evans DG, Burnell LD, Hopwood P, et al. Perception of risk in women with a family history of breast cancer. Br J Cancer. 1993;67:612–614. doi: 10.1038/bjc.1993.112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ormond K, Haun J, Cook L, et al. Recommendations for Telephone Counseling. J Genet Couns. 2000;9 doi: 10.1023/A:1009433224504. [DOI] [PubMed] [Google Scholar]
- 11.Genetic Information Nondiscrimination Act of 2008, National Human Genome Research Institute, National Institutes of Health. 2008 [Google Scholar]
- 12.Myriad Genetic Laboratories, Inc. 2008 [Google Scholar]