Abstract
Bouveret’s syndrome is a well known clinical entity; its incidence however, is uncommon. An unusual complication of cholelithiasis, Bouveret’s syndrome should be considered in an elderly patient presenting with acute gastric outlet obstruction.
We describe a case of an elderly female patient presenting with acute gastric outlet obstruction secondary to a massive gallstone and discuss the imaging appearances and therapeutic options for this rare condition.
An eighty year-old lady was admitted with a five day history of right sided upper abdominal pain with concomitant non-bilious vomiting. She had been admitted three months previously with acute cholecystitis and was awaiting out-patient review. Clinical evaluation confirmed right upper quadrant tenderness with associated fullness but no discernable mass was identified; there was no clinical evidence of jaundice. The patient had mild pyrexia of 37.8 °C, all other vital parameters were within normal limits; specifically she was normotensive and not tachycardic. The working diagnosis was of recurrent acute cholecystitis and thus the patient was managed as such with intravenous fluids and antibiotics. Blood investigations revealed a mild leukocytosis (WCC 9.4 × 103/μL) and mildly raised C – reactive protein (18.4 mg/L), with elevated alkaline phosphatase (321 U/L), alanine aminotransferase (258 U/L) and gamma glutamyl transpeptidase (563 U/L). Bilirubin levels and renal function were normal. An abdominal ultrasound scan was requested for further evaluation.
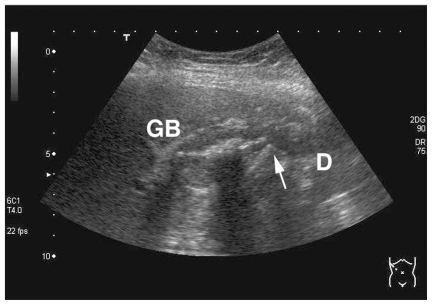
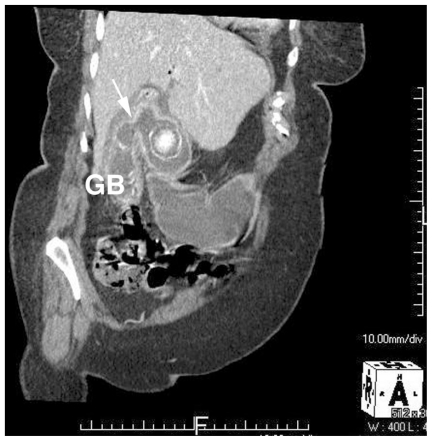
Ultrasound imaging revealed pneumobilia with complex inflammatory change between the gallbladder and duodenum, with appearances highly suggestive of a cholecystoduodenal fistula (Fig. 1); the distal small bowel was seen to be collapsed whilst the stomach was distended and fluid filled. Further evaluation with abdominal contrast enhanced computed tomography (CT) confirmed the fistulous connection between gallbladder and duodenum with a large (4.8cm maximum diameter) gallstone impacted in the duodenal cap with resultant gastric outlet obstruction – Bouveret’s syndrome (Fig. 2).
Figure 1.
Oblique ultrasound right upper quadrant of abdomen demonstrates fistulous communication (arrow) between the gall-bladder (GB) and duodenum (D), residual calculus seen within the gallbladder with associated posterior acoustic shadowing.
Figure 2.
Oblique reconstruction CT image confirms the fistulous connection (arrow) between gallbladder (GB) and duodenum with a large (4.8cm maximum diameter) gall-stone impacted in the duodenal cap with resultant gastric outlet obstruction - Bouveret’s syndrome.
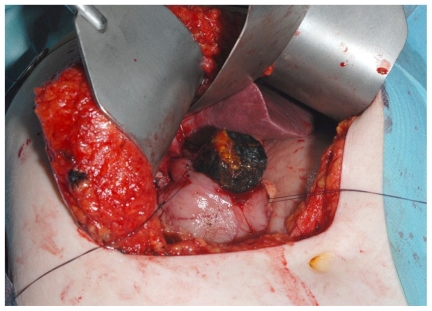
The patient underwent surgical management with partial cholecystectomy and open stone removal from the first part of the duodenum (D1) (Fig. 3 & Fig. 4). At operation the fistula between the gallbladder neck and D1 was visualised; the gallbladder fundus was found to be full of calculi and hence a partial cholecystectomy was performed and the gallbladder neck closed with sutures. Both the pyloric canal and D1 were opened with a longitudinal incision to facilitate stone removal, closed transversely as a pyloroplasty. The patient made an uneventful recovery.
Figure 3.
Intraoperative image: large gallstone surgically removed from first part of Duodenum
Figure 4.
Large gallstone surgically removed from first part of Duodenum
DISCUSSION
Bouveret’s syndrome, described by Léon Bouveret in 1896 (1), represents gastric obstruction secondary to an intra-luminal gallstone from a cholecystoenteric fistula (2). In an elderly patient presenting with acute gastric outlet obstruction (GOO) the working differential diagnosis is extensive (table 1).
Table 1.
Differential diagnoses of acute gastric outlet obstruction in elderly patients.
Inflammatory
|
A form of proximal gallstone ileus, Bouveret’s syndrome affects either the stomach or duodenum, with the offending calculus resulting in clinical gastric outlet obstruction (3, 4). It is most prevalent in elderly females and, as with other forms of gallstone ileus, typically occurs over 65 years of age. Gallstone ileus accounts for up-to 25% of all non-strangulated small bowel obstructions in patients over the age of sixty five (5,6). Gallstone ileus most commonly occurs within the terminal ileum (70%), a luminal narrowing anywhere however, smaller than the calibre of the stone itself, may result in ileus (6,7). Rarely does the obstructing calculus lodge within the duodenum (3,8).
The classical imaging triad of gallstone ileus were described by Rigler et al. as partial or complete intestinal obstruction, pneumobilia and ectopic gallstone, commonly over 2.5 cm in diameter (9). Rigler’s findings were initially described on plain abdominal radiographs, the appearances however are applicable to multi-modality imaging; in the described case the classical imaging characteristics were detected on both ultrasound and multislice CT. Reliance upon plain film demonstration of the classical triad alone is imprudent as the complete triad may be present as infrequently as 10% of confirmed cases; in one study Lassandro et al demonstrated Rigler’s triad in only 14.8% cases of gallstone ileus with plain abdominal film, 11.1% cases on ultrasound and 77.8% with CT (10). Ultrasound has been shown to be a useful adjunct to a plain radiograph in demonstration of the triad (11). Computed tomography not only enables early accurate diagnosis and assessment of associated complications but also determination of size of the offending calculus and presence of any other ectopic intraluminal calculi (12). In an elderly patient with acute GOO, early cross section imaging is therefore paramount to establish the underlying aetiology and facilitate expeditious intervention where clinically appropriate.
Bouveret’s syndrome is associated with considerable morbidity; mortality rates have fallen but remain as high as 12% consequential to significant associated co-morbidities in this patient group (13). Various management strategies exist with no unanimous best line approach. In our case a sub-total cholecystectomy was performed; with inflammatory conditions affecting the gallbladder, dissection of Calot’s triangle can be difficult and resultantly if the anatomy remains obscured it is unsafe to proceed with a complete cholecystectomy and in such instances a subtotal procedure may be opted for, during which any gallbladder calculi can be removed. Some authors propose surgical intervention with either a one-stage (enterolithotomy, fistula repair and cholecystectomy) or two-stage (enterolithotomy plus subsequent cholecystectomy) procedure; however, in view of the often high operative risk of patients presenting with this condition, endoscopic therapeutic intervention offers a viable alternative in selected cases, obviating the need for surgery and it’s associated risks (3,7,14).
TEACHING POINT
An unusual complication of cholelithiasis, Bouveret’s syndrome should be considered in an elderly patient presenting with acute gastric outlet obstruction.
ABBREVIATIONS
- WCC
White cell count
- CT
Computed tomography
- D1
First part of the duodenum
- GOO
Gastric outlet obstruction
REFERENCES
- 1.Bouveret L. Sténose de pylore adhèrent à la vesicule caleuse. Rev Med (Paris) 1896;16:1–16. [Google Scholar]
- 2.Lowe AS, Stephenson S, Kay CL, May J. Duodenal obstruction by gallstones (Bouveret’s syndrome): a review of the literature. Endoscopy. 2005 Jan;37(1):82–7. doi: 10.1055/s-2004-826100. [DOI] [PubMed] [Google Scholar]
- 3.Brennan GB, Rosenberg RD, Arora S. Bouveret syndrome. Radiographics. 2004 Jul-Aug;24(4):1171–5. doi: 10.1148/rg.244035222. [DOI] [PubMed] [Google Scholar]
- 4.Singh AK, Shirkhoda A, Lal N, Sagar P. Bouveret’s syndrome: appearance on CT and upper gastrointestinal radiography before and after stone obturation. AJR Am J Roentgenol. 2003 Sep;181(3):828–30. doi: 10.2214/ajr.181.3.1810828. [DOI] [PubMed] [Google Scholar]
- 5.Reisner RM, Cohen JR. Gallstone ileus: a review of 1001 reported cases. Am Surg. 1994 Jun;60(6):441–6. [PubMed] [Google Scholar]
- 6.Masannat Y, Masannat Y, Shatnawei A. Gallstone ileus: a review. Mt Sinai J Med. 2006;73(8):1132–4. [PubMed] [Google Scholar]
- 7.Wittenburg H, Mössner J, Caca K. Endoscopic treatment of duodenal obstruction due to a gallstone (“Bouveret’s syndrome”) Ann Hepatol. 2005;4(2):132–134. [PubMed] [Google Scholar]
- 8.Abou-Saif A, Al-Kawas FH. Complications of gallstone disease: Mirizzi syndrome, cholecystocholedochal fistula, and gallstone ileus. Am J Gastroenterol. 2002 Feb;97(2):249–54. doi: 10.1111/j.1572-0241.2002.05451.x. [DOI] [PubMed] [Google Scholar]
- 9.Rigler LG, Borman CN, Noble JF. Gallstone obstruction. Pathogenesis and roentgen manifestations. JAMA. 1941;117:1753–1759. [Google Scholar]
- 10.Lassandro F, Gagliardi N, Scuderi M, Pinto A, Gatta G, Mazzeo R. Gallstone ileus analysis of radiological findings in 27 patients. Eur J Radiol. 2004;50(1):23–29. doi: 10.1016/j.ejrad.2003.11.011. [DOI] [PubMed] [Google Scholar]
- 11.Ripollés T, Miguel-Dasit A, Errando J, Morote V, Gomez-Abril SA, Richart J. Gallstone ileus: increased diagnostic sensitivity by combining plain film and ultrasound. Abdom Imaging. 2001;26(4):401–5. doi: 10.1007/s002610000190. [DOI] [PubMed] [Google Scholar]
- 12.Lassandro F, Romano S, Ragozzino A, Rossi G, Valente T, Ferrara I, Romano L, Grassi R. Role of helical CT in diagnosis of gallstone ileus and related conditions. AJR Am J Roentgenol. 2005 Nov;185(5):1159–65. doi: 10.2214/AJR.04.1371. [DOI] [PubMed] [Google Scholar]
- 13.Frattaroli FM, Reggio D, Gaudalaxara A, Illomei G, Lomanto D, Pappalardo G. Bouveret’s syndrome: case report and review of the literature. Hepatogastroenterology. 1997;44:1019–1022. [PubMed] [Google Scholar]
- 14.Lubbers H, Mahlke R, Lankisch PG. Gallstone ileus: endoscopic removal of a gallstone obstructing the upper jejunum. J Intern Med. 1999 Dec;246(6):593–7. doi: 10.1046/j.1365-2796.1999.00597.x. [DOI] [PubMed] [Google Scholar]