Abstract
Ileocolic invagination in the adult may be caused by adenocarcinoma and lead to intestinal obstruction. We report a case of a cecal adenocarcinoma that was complicated by an ileocolic invagination in a 38 year old female, diagnosed on a contrast enhanced CT scan of the abdomen and highlights the importance of contrast enhanced CT for diagnosis of ileocolic invagination.
Keywords: Invagination, adenocarcinoma, adult, CT
Case Report
A 38 year old woman was admitted to the emergency department of our hospital with an ever-increasing colicky abdominal pain for 4 weeks, predominantly in the hypogastric region, associated with vomiting. Her past medical history was a Cesarean section one month previously, and left sided vesico-ureteral reflux.
Physical examination revealed a diffusely tender abdomen without rebound tenderness, and a palpable mass in the gastric region. All the laboratory results were normal, including inflammatory markers. Ultrasound of the upper abdomen, performed by the resident on call, showed thickening of the ascending colon wall and an invagination was presumed. A contrast enhanced multidetector CT scan of the abdomen demonstrated an ileocolic invagination including mesenterial fat, lymph nodes and vessels. There was edema of the colon wall at the distal part of the invagination, indicating early intestinal obstruction and ischemia of the bowel wall.
Laparotomy confirmed the presence of ileocolic invagination, and identified a solid mass at the ileocolic transition as the lead point of the invagination. An ileocecal surgical resection was performed.
Histopathological examination of the resected segment demonstrated an adenocarcinoma of the cecum with infiltration into the muscularis propria, but without lymph node involvement. Staging was T2N0M0.
DISCUSSION
Intussusception is the invagination of a bowel loop with its mesenteric fold into the lumen of a contiguous portion of bowel as a result of peristalsis (1). Intussusception amongst adults is rare, being responsible for only 5% of all intussusceptions and 1% of all bowel obstructions (2). An underlying cause is found in 80–90% of all adult cases; neoplasms being the most common one (2,3). When a neoplasm is involved, intussusception occurs when the mass in the bowel is pulled forward by normal peristalsis, resulting in an invagination of the involved wall (4).
Clinical findings are episodic colicky abdominal pain, nausea, vomiting, i.e. symptoms suggesting partial intestinal obstruction (5). When a lead point is involved, symptoms related to a neoplastic process can be manifest, including constipation, weight loss, melena, or a palpable abdominal mass (1).
The lead points of adult intussusceptions involving the colon are usually malignant, whereas those involving the small bowel tend to be benign (6). Examples of benign small bowel lead points are lipoma, polyp, adenoma, Meckel diverticulum (1).
Adenocarcinoma of the colon is the most common malignant neoplasm associated with colonic intussusception (1). Cecal adenocarcinomas have the tendency to be large, polypoid, and bulky and may act as the lead point for an intussusception. Adenocarcinomas of the terminal ileum are primarily annular and constricting. These lesions mostly present themselves as eccentric or circumferential wall thickening involving a short segment of the ileum. Rarely an adenocarcinoma of the terminal ileum manifests as a pedunculated polypoid mass that can lead to invagination (7).
Contrast enhanced multidetector CT scanning of the abdomen is proved to be the superior method in establishing rapid preoperative diagnosis of intussusception, with ultrasound being the second most accurate method (2,8).
On CT, the intussusception appears as a complex soft tissue mass, consisting of the outer intussuscipiens and the central intussusceptum. There is often an eccentric area of fat density within the mass representing the intussuscepted mesenteric fat, and the mesenteric vessels are often visible within it (4). Although not pathognomonic, CT visualizes intussusception as a “target” or “bull’s-eye” mass. The typical concentric hyperdense double ring, coupled with thickening of the intestinal walls, indicates that the neoformation has caused persistent invagination of the large bowel (9). The vascular perfusion may be compromised in the intussuscepted mesentery, resulting in venous congestion and edema, which causes fascial planes to become indistinct. As the edema and vascular compromise progress, the bowel wall becomes gangrenous as reflected by air in the bowel wall or the bowel necroses and appears as an amorphous mass associated with severe obstruction (10). Although the appearance of intussusception is characteristic on CT, one is seldom able to demonstrate the cause preoperatively (4,6,11).
Multidetector CT features of adenocarcinoma of the colon are marked asymmetric wall thickening, short segment involvement, and abrupt change from normal to abnormal segments of colon (7). If there is bowel wall edema due to impaired circulation of the mesenteric vessels, the thickened bowel loops make it difficult to differentiate a lead mass from inflammation. An invagination with a lead mass appears as an abnormal targetlike mass with a cross-sectional diameter greater than that of the normal bowel and may be associated with proximal bowel obstruction. Identification of distinct anatomic features is often challenging due to the complex appearance of both bowel edema and the lead mass (1).
More than half of the large bowel invaginations in adults are associated with malignant tumors and metastatic disease (2).
TEACHING POINT
The exclusion of a lead point in a case of invagination in adult patients is of high importance. Neoplasms are the most frequent cause. Contrast enhanced CT scan is the primary method of choice in determining the diagnosis of invagination, whereas ultrasound is the second most accurate method. On CT, an intussusception appears as a complex soft tissue mass, typically as a “target” or “bull’s-eye” mass.
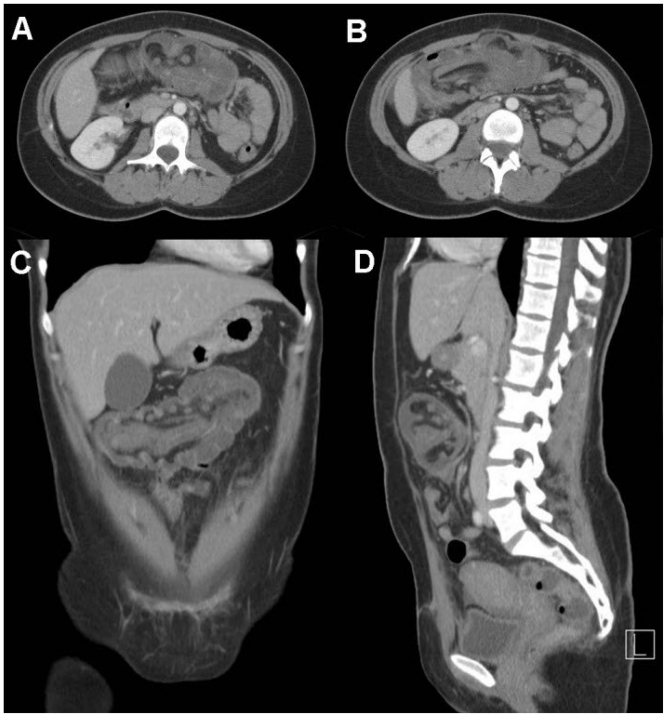
Figure 1.
Axial (A and B), coronal (C) and sagittal (D) multiplanar reformatted computed tomography images show an ileocolic invagination including mesenterial fat, lymph nodes and vessels.
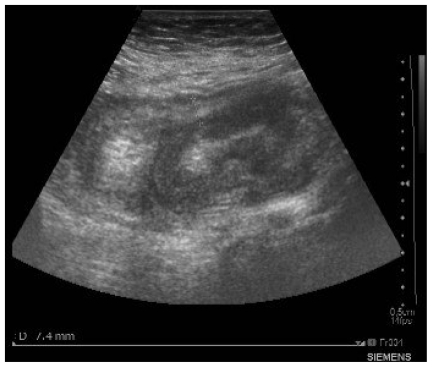
Figure 2.
The transverse grayscale ultrasound image reveals multiple concentric hypoechoic peripheral rings formed by the intussuscipiens and the intussusceptum. The center is hyperechogenic and crescent-shaped owing to the mesentery.
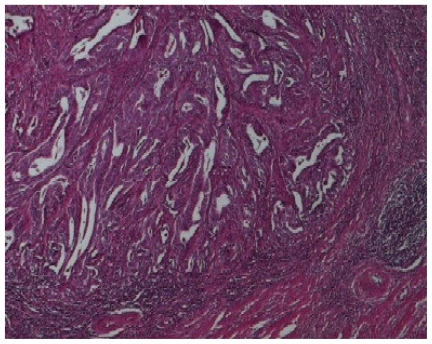
Figure 3.
On histology with hematoxylin-eosin-safran staining and at 40X magnification low grade adenocarcinoma invading the muscularis propria is detected.
ABBREVIATIONS
- CT
Computed tomography
REFERENCES
- 1.Kim YH, Blake MA, Harisinghani MG, et al. Adult intestinal intussusception: CT appearances and identification of a causative lead point. RadioGraphics. 2006;26:733–744. doi: 10.1148/rg.263055100. [DOI] [PubMed] [Google Scholar]
- 2.Azar T, Berger DL. Adult intussusception. Ann Surg. 1997;226:134–138. doi: 10.1097/00000658-199708000-00003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Warshauer DM, Lee JKT. Adult intussusception detected at CT or MR imaging: Clinical-imaging correlation. Radiology. 1999;212:853–860. doi: 10.1148/radiology.212.3.r99au43853. [DOI] [PubMed] [Google Scholar]
- 4.Gayer G, Zissin R, Apter S, et al. Adult intussusception-a CT diagnosis. Br J Radiol. 2002;75:185–190. doi: 10.1259/bjr.75.890.750185. [DOI] [PubMed] [Google Scholar]
- 5.Felix EL, Cohen MH, Bernstein AD, et al. Adult intussusception: case report of recurrent intussusception and review of literature. Am J Surg. 1976;131:758–761. doi: 10.1016/0002-9610(76)90196-3. [DOI] [PubMed] [Google Scholar]
- 6.Urbano J, Serantes A, Hernandez L, et al. Lipoma-induced jejunojejunal intussusception : US and CT diagnosis. Abdom Imaging. 1996;21:522–524. doi: 10.1007/s002619900118. [DOI] [PubMed] [Google Scholar]
- 7.Hoeffel C, Cream MD, Belkacem A, et al. Multi-detector row CT: Spectrum of diseases involving the ileocaecal area. RadioGraphics. 2006;26:1373–1390. doi: 10.1148/rg.265045191. [DOI] [PubMed] [Google Scholar]
- 8.Mussack T, Szeimies U. Sigmoidorectal intussusception caused by rectal carcinoma: multislice CT findings. Abdom Imaging. 2002;27:566–569. doi: 10.1007/s00261-001-0105-9. [DOI] [PubMed] [Google Scholar]
- 9.Lorenzi M, Iroatulam AJ, Vemillo R, et al. Adult colonic intussusception caused by malignant tumor of the transverse colon. Am Surg. 1999;65:11–14. [PubMed] [Google Scholar]
- 10.Iko BO, Teal JS, Siram SM, et al. Computed tomography of adult colonic intussusception: clinical and experimental studies. AJR. 1984;143:769–772. doi: 10.2214/ajr.143.4.769. [DOI] [PubMed] [Google Scholar]
- 11.Ross GJ, Amilineni V. Case 26: Jejunojejunal intussusception secondary to a lipoma. Radiology. 2000;216:727–730. doi: 10.1148/radiology.216.3.r00se33727. [DOI] [PubMed] [Google Scholar]