Abstract
Jejunal diverticulitis is a rare condition that can present with an acute abdomen and be referred for imaging. We present the case of an elderly patient who at CT was diagnosed with an intra-abdominal abscess involving both jejunum and transverse colon. However, the underlying eitiology was not initially clear until small bowel barium follow-through.
Pertinent points regarding CT findings in jejunal diverticulitis are discussed, and practical recommendations in small bowel diverticulum recognition and diagnosis are made.
Keywords: Computed tomography, jejunal diverticulitis, small bowel diverticula, small dowel diverticulitis
Case Report
A 90 year-old woman presented with an insidious history of painless per rectal bleeding followed by a brisk bleed that necessitated hospital admission, treatment and investigation. An initial upper GI endoscopy was negative and colonoscopy abandoned as the recto-sigmoid junction was impassable. A computed tomography (CT) angiogram was undertaken but no bleeding point could be identified. Symptoms persisted and a subsequent Meckel’s scan was negative. A barium enema demonstrated a 9mm pedunculated polyp in the descending colon but no other pathology. She was subsequently discharged with a presumed diagnosis of bleeding colonic polyp.
The patient re-presented a month later with left iliac-fossa pain and tenderness, pyrexia and raised inflammatory markers, including WBC and CRP. Initial plain film investigation showed a non-specific gas pattern. A subsequent portal-venous CT scan with oral contrast demonstrated an inflammatory mass involving the jejunum and transverse colon (Fig. 1). Several etiologies were suggested including large bowel diverticulitis or malignancy with a collection and possible fistulation involving the jejunum. However the preceding barium enema (Fig. 2) showed no lesion in that area. The patient was managed conservatively with intra-venous antibiotics and following discharge was investigated with a small bowel follow-through. This elegantly demonstrated extensive jejunal diverticulosis (Fig. 3). Subsequent review of CT coronal reconstructions and MIP images revealed multiple small bowel diverticula in close association to the abscess and a diverticulum situated within the abscess itself (Fig. 4, Fig. 5).
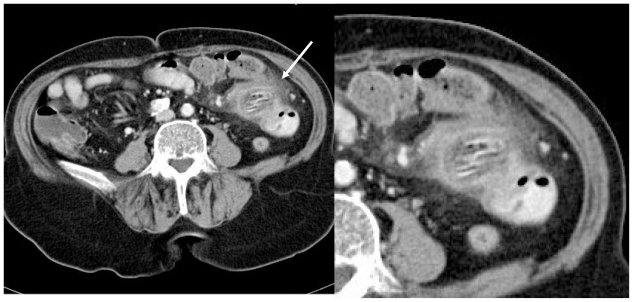
Figure 1.
a (left) and b (right). Contrast enhanced axial CT (1mm thickness at 3mm intervals) demonstrating a) Inflammatory mass involving jejunum and transverse colon with associated mesenteric fat stranding and containing gas-filled structures (arrow) b) Magnified view.
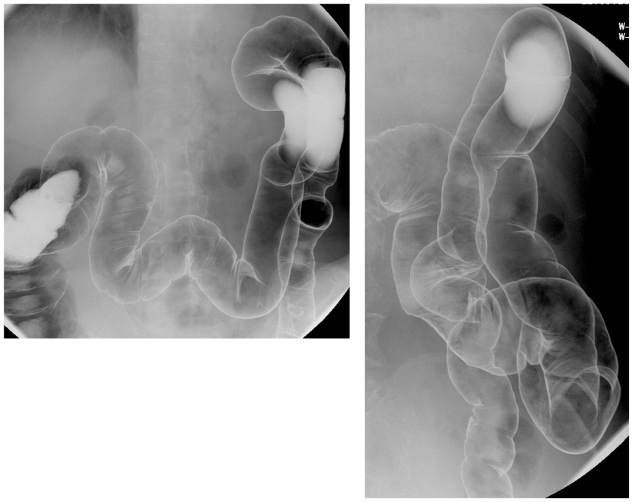
Figure 2.
a (top) and b (right). Barium enema demonstrating no lesion in the transverse colon or splenic flexure in the region affected by the abscess.
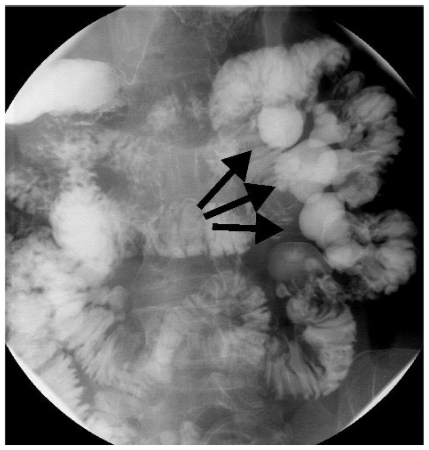
Figure 3.
Small bowel follow-through demonstrating jejunal diverticulosis as multiple contrast-filled pouches associated with the small bowel (arrows).
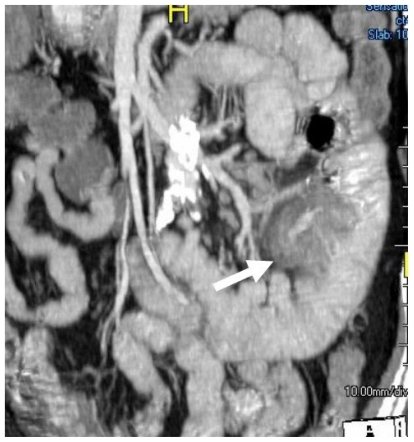
Figure 4.
Coronal reconstruction of a contrast enhanced CT with oral contrast (2D maximal intensity projection) images showing abscess (arrow) in association with a loop of jejunum. The jejunum exhibits several diverticula and a diverticulum at the centre of the thick-walled gas-containing structure with surrounding inflammatory change.
Figure 5.
Coronal reconstruction of a contrast enhanced CT with oral contrast (3D maximal intensity projection) images showing abscess (arrow) in association with loop of jejunum. The jejunum exhibits several diverticula and a diverticulum at the centre of the thick-walled gas-containing structure with surrounding inflammatory change.
DISCUSSION
Jejunal and ileal diverticulosis is an uncommon acquired condition. A prevalence of 1.3% and 2.3% has been identified in autopsy and radiology based series respectively (1,2), slightly higher in men than women (3). The majority of cases are asymptomatic or are associated with non-specific gastrointestinal symptoms (3). They rarely occur in patients below the age of 40 (2). The incidence and size of diverticula decreases as one moves distally from jejunum to terminal ileum. They may be solitary, however they are usually multiple with a mean number of ten to fifteen; patients may exhibit up to a hundred (4,5). They are always situated on the mesenteric border (4,5).
Acute complications including diverticulitis, haemorrhage, mechanical obstruction and perforation have been found to occur in 6–18% of cases (3,4,5). Another complication is that of vitamin B12 malabsorption because of stagnation and bacterial overgrowth in large diverticula (2). Perhaps the commonest complication, small bowel diverticulitis (5) often presents with non-specific symptoms or with features that mimic other symptom complexes including appendicitis, colonic diverticulitis or Crohn’s disease. Indeed, before CT was commonly used in the assessment of the acute abdomen, 90% of small bowel diverticulitis was diagnosed at laparotomy (6). The role of CT in the diagnosis of this condition has been previously highlighted as a useful tool (4,5,7).
Jejunal diverticula appear on CT as distinct round or ovoid, fluid, contrast, or air-containing structures outside the expected lumen of the small bowel, with a smooth, wall and no recognizable small bowel folds. They are often seen to communicate directly with an adjacent loop of small bowel (8). However, they can be difficult to identify but can be appreciated by scrolling through the image stack. CT findings in jejunal diverticulitis include non specific signs such as an inflammatory mass containing gas and feces-like material, and oedema in the surrounding tissue such as intraperitoneal fat or fascial layers (5,7). More specifically, a focal area of asymmetrical small bowel wall thickening or intraluminal contrast enhanced out-pouching on the mesenteric side of the bowel may be seen, the presence of which may be within or in close proximity to an abscess cavity (5).
However, the CT diagnosis is not straight-forward, especially if the inflammatory mass or an associated abscess involves adjacent structures such as the large bowel, and if diverticula are small and low in number. In these instances it is not unreasonable to entertain alternative diagnoses of more frequently occurring pathologies including colonic diverticulitis or malignancy, appendicitis or inflammatory bowel disease. Alternatively, rarer conditions of the small bowel, particularly foreign body perforation or lymphoma could be added to the list of differential diagnoses. In this particular case, we found identification of diverticula particularly difficult on axial scans given the tortuous course of small bowel within the peritoneal cavity. The use of coronal reformatted images was extremely useful in diverticula identification both within the abscess and in adjacent jejunal loops. Multiplanar maximum intensity projection (MIP) imaging helped further orientate the image along the course of the small bowel and confirmed association between diverticula and abscess.
TEACHING POINT
Although a rare phenomenon, jejunal or ileal diverticulitis should be considered in the differential diagnosis of abdominal pain with raised inflammatory markers in an elderly patient. The condition should certainly be considered if an abscess or inflammatory mass are identified involving the small bowel on CT with coronal reconstruction being a valuable aid in its diagnosis.
ABBREVIATIONS
- CT
Computed Tomography
- MIP
Maximum intensity projection
- WBC
White blood cell count
- CRP
C-reactive protein
REFERENCES
- 1.Edwards HC. Diverticulosis of the small intestine. Ann Surg. 1936;103:230–54. doi: 10.1097/00000658-193602000-00006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Maglminte DT, Chemish SM, DeWeese A, et al. Acquired jejunoileal diverticular disease: subject review state of the art. Radiol. 1986;158:577–80. doi: 10.1148/radiology.158.3.3080802. [DOI] [PubMed] [Google Scholar]
- 3.Tsiotos GG, Farnell MB, Ilstup DM. Non-Meckelian jejunal or ileal diverticulosis: an analysis of 112 cases. Surgery. 1994;116:726–34. [PubMed] [Google Scholar]
- 4.Gayer G, Zissin R, Apter S, et al. Acute diverticulitis of the small bowel: CT findings. Abdom Imaging. 1999;24:452–5. doi: 10.1007/s002619900538. [DOI] [PubMed] [Google Scholar]
- 5.Coulier B, Maldague P, Bourgeois A, et al. Diverticulitis of the small bowel: CT diagnosis. Abdom Imaging. 2007;32:228–33. doi: 10.1007/s00261-006-9045-8. [DOI] [PubMed] [Google Scholar]
- 6.Peters R, Grust A, Gerharz CD, et al. Perforated jejunal diverticulitis as a rare cause of acute abdomen. Eur Radiol. 1999;9:1426–8. doi: 10.1007/s003300050862. [DOI] [PubMed] [Google Scholar]
- 7.Greenstein S, Jones B, Fishman E, et al. Small-Bowel Diverticulitis: CT Findings. Am J Radiol. 1986;147:271–4. doi: 10.2214/ajr.147.2.271. [DOI] [PubMed] [Google Scholar]
- 8.Fintelmann F, Levine MS, Rubesin SE. Jejunal Diverticulosis: Findings on CT in 28 Patients. Am J Radiol. 2008;190:1286–90. doi: 10.2214/AJR.07.3087. [DOI] [PubMed] [Google Scholar]