Abstract
Tuberculosis (TB) of the scapula is an unusual presentation of musculoskeletal tuberculosis. In an endemic area, this rare presentation may become more frequent. The indolent nature of tuberculous bone and joint disease often leads to delayed or missed diagnosis. It is not uncommon for this disease to mimic malignancy. Therefore, the prompt recognition of distinguishing features is vital for correct diagnosis. In particular, imaging is a key tool in helping to make the diagnosis, through the recognition of certain key radiological patterns. However, as there are no pathognomonic imaging findings, the diagnosis rests on histopathological and microbiological confirmation. We report a case of tuberculous osteomyelitis of the scapula. This entity has not received much attention in literature. Pure tuberculous osteomyelitis involving flat membranous bone, as depicted in this report, is rare. Our patient also had an ovarian malignancy, which had decreased our index of suspicion. We therefore present this case as tuberculosis masquerading a cystic scapular metastases.
Keywords: Tuberculosis, osteomyelitis
CASE REPORT
A 49 year-old lady presented with swelling and pain in the lower left scapular region for the last 2 months, reportedly gradually increasing in size. This was painless and no fever or local redness was present. She was diagnosed to have papillary adenocarcinoma of the right ovary 2 years ago and was treated with three cycles of standard neoadjuvant chemotherapy with Paclitaxel and Carboplatin followed by interval debulking and further 3 cycles of the same chemotherapy which she completed in the following year. The disease was in remission when she was last followed up in January 2008. There was no history of trauma, fever, loss of appetite, chronic cough, the patient had no chest complaints or other constitutional symptoms. There was no past history of tuberculosis in her and no history of contact with TB.
On examination, swelling was found over inferior left scapular region and to be approximately 100 mm × 80 mm in size, soft, fluctuant, globular and non-tender with restricted mobility at the posterolateral aspect of the left side of the chest wall near the superior part of the scapula. Skin over the swelling was normal and was not adherent to it. There was no discharging sinus or pointing abscess. No bruit or pulsation was present in the swelling. Temperature was not raised. Examination of the left shoulder revealed full range of motion. Blood profile revealed PCV of 32% the white blood cell count was normal. Other routine blood investigations, urine analysis and serum chemistry were found to be normal. HIV ELISA was negative.
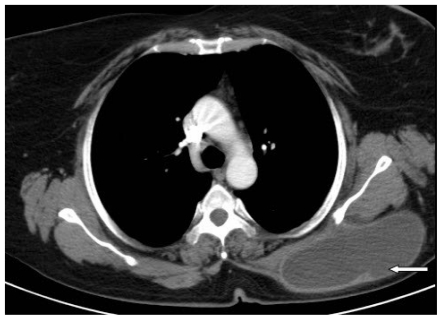
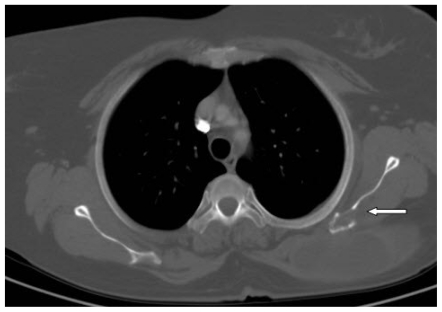
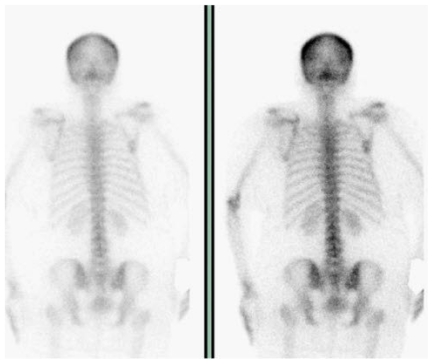
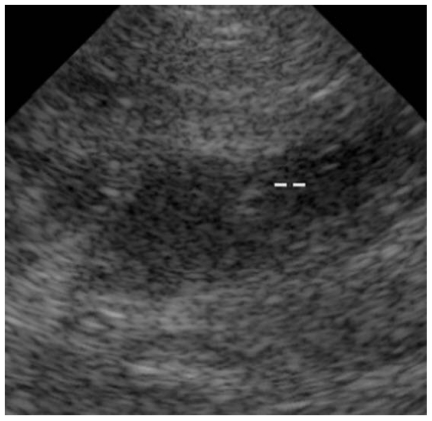
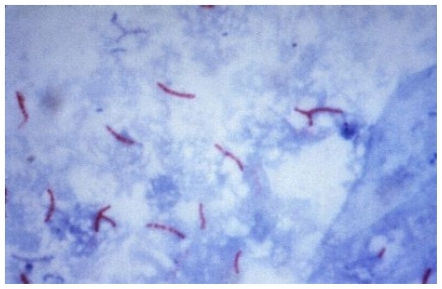
CT showed a thin walled cystic lesion with peripheral enhancement adjacent the medial aspect of the scapular body inferior to the spine measuring 12 × 12 × 5 cm with a lytic lesion in the adjacent bone with minimal surrounding sclerosis (Fig. 1 and Fig. 2). There was no abnormality in the rest of the thorax. Bone scan did not show any tracer uptake in the region of the left scapula (Fig. 3). High-resolution ultrasonography done as a screening before aspiration showed a cystic lesion having fluid with few low level internal echoes superficial to the left scapula (Fig. 4). The cystic lesion was aspirated, approximately 400 ml of fluid with debris was removed. A cytological examination of the aspirate showed necrotic material and inflammatory cells. Gram stain for bacteria was negative and no fungal elements were seen on smear. Ziehl-Neelsen stain showed the presence of a few acid-fast bacilli (Fig. 5).
Figure 1.
49 year female with tuberculous osteomyelitis of the scapula. Axial contrast enhanced CT scan showing a cystic lesion with an enhancing rim in relation to the left scapula.
Figure 2.
49 year female with tuberculous osteomyelitis of the scapula. Axial contrast enhanced CT scan in bone window showing bone lysis in the left scapula.
Figure 3.
49 year female with tuberculous osteomyelitis of the scapula. Bone scan - Technetium-99m methylene diphosphonate (MDP) showing no significant tracer uptake in the scapula, anterior and posterior views. (Right image: anterior view, left image:posterior view)
Figure 4.
49 year female with tuberculous osteomyelitis of the scapula. Grayscale ultrasound image of the left scapular region confirms the presence of central liquefaction.
Figure 5.
49 year female with tuberculous osteomyelitis of the scapula. Ziehl-Neelsen stain showing acid-fast bacilli [Fluid aspirate from scapular mass].
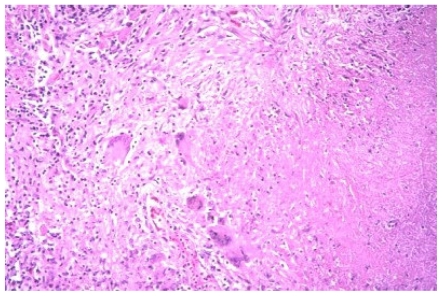
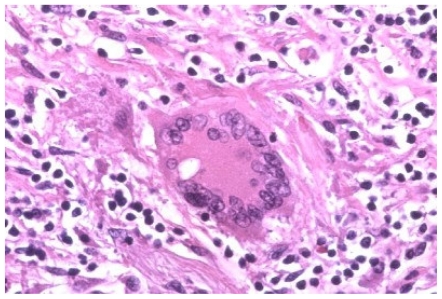
She underwent incision and drainage of this cold abscess and biopsy of the wall revealed large foci of necrosis and multiple granulomas composed of epithelioid histiocytes, lymphocytes, plasma cells and langhans type of giant cells (Fig. 6 and Fig. 7). There was proliferation of fibroblast and thin walled vascular channels. Acidfast bacilli or fungal organisms were not seen. Subsequent culture of fluid in Lowenstein-Jensen media grew 3 colonies of Mycobacterium tuberculosis (Fig. 8), which was sensitive to streptomycin, rifampicin, isoniazid, ethambutol and pyrazinamide. The culture examination for pyogenic bacteria and fungus did not grow any organisms. Cytological examination did not reveal any malignant cells. Based on the history, clinical examination, and investigations, she was diagnosed to have tuberculous osteomyelitis with a cold abscess in the scapular region. The patient was treated with antitubercular therapy using Isoniazid, Rifampicin, Pyrazinamide and Ethambutol. She had good response to treatment and was advised to continue treatment for 6–12 months.
Figure 6.
49 year female with tuberculous osteomyelitis of the scapula. Central necrosis, Langhans-type giant cells, fibrosis, epithelioid cells [H&E original magnification × 80] [Biopsy specimen].
Figure 7.
49 year female with tuberculous osteomyelitis of the scapula. Langhans-type giant cell, epithelioid cells, lymphocytes, and fibrosis [ H&E original magnification × 200] [Biopsy specimen]
Figure 8.
49 year female with tuberculous osteomyelitis of the scapula. Gross appearance of Mycobacterium colonies on Lowenstein Jensen medium.
DISCUSSION
Tuberculosis, including skeletal tuberculosis, is an ancient infection based upon evidence from archaeological remnants. Typical features of spinal TB have been identified in Egyptian mummies dating back to almost 4000 BC. Mycobacterium tuberculosis was revealed by DNA analysis in a vertebral lesion of a young girl who lived about 1000 AD (1).
Musculoskeletal infection may account for 10 to 35 percent of cases of extrapulmonary tuberculosis and overall, for almost 2 percent of all cases of TB (2). The spine is involved in approximately half of patients (2). The next most common is tuberculous arthritis followed by extra spinal tuberculous osteomyelitis (2). Skeletal tuberculosis can clinically simulate metastases leading to delay in correct diagnosis and the institution of appropriate therapy (3).
Solitary tuberculous osteomyelitis involving flat membranous bones is a rare described entity. Very few cases of tubercular osteomyelitis of scapula have been reported till date and all of these were associated with other forms of tubercular osteomyelitis. To the best of our knowledge, only five cases of tuberculous osteomyelitis of the scapula have been reported in literature, one involving acromian (4) and, one involving the inferior angle and the other three the body of the scapula (4–6). In the present case, no other focus could be detected.
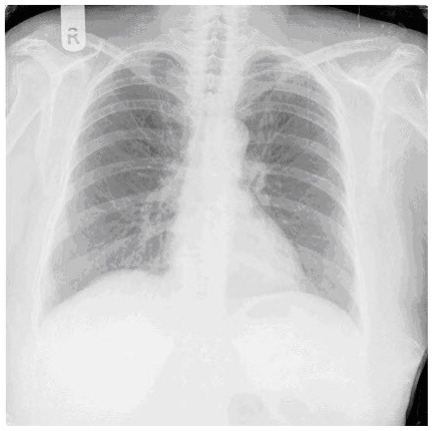
Although a positive tuberculin test and chest imaging findings are supportive of the diagnosis, absence of these does not exclude it (7). Therefore other diagnostic tests need to be used, combined with a high index of clinical suspicion. As highlighted by the above case, a multimodality imaging approach assists in the early diagnosis, enabling the timely initiation of appropriate therapy.
While the most common site of osseous involvement is the spine, followed by the femur, tibia and the small bones of the hands and feet, any bone can potentially be affected (1,8,9,10). The most common presenting symptoms of tuberculous osteomyelitis are non-specific pain and swelling. Radiographic findings in bony tuberculosis include osteopenia, osteolytic foci with poorly defined edges, and varying amounts of sclerosis and periostitis (1,9,11). The metaphysis is typically involved, although epiphyseal involvement also occurs (1). A particular type of tuberculous osteomyelitis, cystic tuberculosis, produces round or oval radiolucencies with variable amounts of sclerosis (1,12). These findings are, however, non-specific, and can be found in a range of pathological processes, including neoplasia. For instance, osteolytic and osteosclerotic foci can be found in metastases from various primary tumors, such as prostate, breast and renal cell carcinoma, whilst sclerosis and a periosteal reaction may suggest a primary bone tumor. Even the radiographic characteristics of cystic tuberculosis can also be found in metastatic carcinoma or germ cell tumors, and plasma cell myeloma (1,4). There are a few radiographic features, however, that favour tuberculous infection over neoplasia. These include the presence of small juxtacortical abscesses or rings of inflammatory tissue, due to cortical destruction and spread of infection to the extraosseous tissues (11). Regardless, the features of tuberculous osteomyelitis are so variable and inconstant that further investigation is usually required.
Tuberculosis (TB) of the chest wall constitutes 1% to 5% of all cases of musculoskeletal TB (1–5) which in turn is far less frequently encountered than pulmonary infection alone and represents between 1% and 2% of TB overall (12–14). TB of bone is thought to result from either lymphatic or haematogenous dissemination of bacilli from a site of primary infection from a Ghon focus, in the lungs. Erosion of bone in TB results from pressure necrosis by granulation tissue and also by the direct action of invading organisms. Faure et al (15) hypothesized that infection of lymph nodes in the chest results from pleuritis caused by invasion of the tubercle bacilli. The extraparenchymal (subpleural) collections made up of caseous material from the necrosed lymph nodes are termed “cold abscesses”. These can burrow through the chest wall to form visible swellings on the exterior without erythema or tenderness. These can sometimes be contiguous with enlarged and intrathoracic lymph nodes. The onset of these infections is often insidious but rarely onset may be acute or subacute. Spontaneous drainage of such cold abscesses may occur. Virtually any bone can be infected (including the ribs, skull, phalanx, pelvis and long bones).
Unfortunately, there is frequently a delay in the diagnosis of this entity (1). The reasons behind the delay in early diagnosis in the present case are no pulmonary involvement, history of known malignancy, insidious onset of symptoms with minimal signs of local inflammation. Involvement of multiple bones (which is rare) may result in an erroneous diagnosis of widespread metastatic malignancy (16,17). An antecedent history of trauma may also lead to diagnostic confusion.
Most authors feel that the sequestra of tuberculous osteomyelitis are absorbed under adequate antituberculosis therapy and surgical removal is not needed in most of the cases (5). Surgical removal is required in patients with giant sequestra or where the response to conservative treatment of 4 to 6 weeks is not satisfactory (18). In the present case, as we achieved symptomatic improvement with antitubercular drugs, we had decided to continue the same. The highly variable and unpredictable location of tuberculous osteomyelitis is illustrated by reports from several authors, sternal osteomyelitis due to M. tuberculosis may follow coronary artery bypass surgery (19).Bony tuberculosis of the rib may present as a breast mass or chest wall mass (20,21). Tuberculosis of the small bones of the hand can occur spontaneously in patients with no signs of pulmonary tuberculosis (22). Tuberculous mastoiditis can extend into the skull and produce facial nerve palsy (23). Lytic bony tubercular lesions in areas as unusual as the symphysis pubis, sacroiliac joint, and elbow can be mistaken for metastatic malignancy (2).
The differential diagnosis of skeletal TB includes subacute or chronic infections due to organisms such as Staphylococcus aureus, brucellosis, melioidosis, actinomycosis, candidiasis and histoplasmosis, depending upon epidemiologic factors. As noted above, metastatic disease to bone may also be considered.
Pitfalls in diagnosis - The most common cause of delay in the diagnosis of bony tuberculosis is failure to consider the diagnosis, especially in patients who have normal chest radiographs. A number of other problems also can occur. In patients who present with draining sinuses, cultures of the sinus exudate may reveal colonizing bacteria or fungi that are erroneously assumed to be the causative pathogen. Failure to biopsy synovium or periarticular bone may lead to falsely-negative cultures in patients with articular tuberculosis. The diagnosis of skeletal tuberculosis is easily overlooked in patients with HIV infection who have relatively high CD4 counts, no other symptoms of tuberculosis, and a tuberculin skin test that is negative or weakly positive. Tuberculous infection can develop in a bone or joint injured by previous trauma or surgery. In such cases, the possibility of a superimposed infectious process must be considered before a diagnosis of tuberculosis can be pursued.
TEACHING POINT
This case highlights the importance of a high index of suspicion for early diagnosis of extra pulmonary tuberculosis, especially in the context of an immunosuppressed state. Features of extra pulmonary tuberculosis often mimic those of malignancy. Tuberculosis can be diagnosed easily based on characteristic histopathology supported by microbiological evidence and cure is achievable with appropriate treatment.
Figure 9.
49 year female with tuberculous osteomyelitis of the left scapula. Frontal chest radiograph showing no significant abnormality.
ABBREVIATIONS
- TB
Tuberculosis
- CT
Computed Tomography
- HIV
Human Immunodeficiency Virus
- ELISA
Enzyme Linked Immunosorbent Assay
- PCV
Packed Cell Volume
- MDP
Methylene Diphosphonate
REFERENCES
- 1.Arriaza BT, Salo W, Aufderheide AC, Holcomb TA. Pre-Columbian tuberculosis in northern Chile: Molecular and skeletal evidence. Am J Phys Anthropol. 1995;98:37. doi: 10.1002/ajpa.1330980104. [DOI] [PubMed] [Google Scholar]
- 2.Tuli SM. Tuberculosis of the Skeletal System (bones, joints, spine and bursal sheaths) 1st edn. Jaypee Brothers Medical Publishers (P) Ltd; New Delhi (India): 1993. p. 121. [Google Scholar]
- 3.Tsay MH, Chen MC, Jaung GY, et al. Atypical skeletal tuberculosis mimicking tumor metastasis: Report of a case. J Formos Med Assoc. 1995;94:428. [PubMed] [Google Scholar]
- 4.Kam WL, Leung YF, Chung OM, Wai YL. Tuberculous osteomyelitis of the scapula. Int Orthop. 2000;24:301–2. doi: 10.1007/s002640000165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Martini M, Adjrad A, Boudjemaa A. Tuberculous osteomyelitis. A review of 125 cases. Int Orthop. 1986;10:201–7. doi: 10.1007/BF00266209. [DOI] [PubMed] [Google Scholar]
- 6.Vohra R, Kang HS, Dogra S, Saggar RR, Sharma R. Tuberculous osteomyelitis. J Bone Joint Surg Br. 1997;79:562–6. doi: 10.1302/0301-620x.79b4.7618. [DOI] [PubMed] [Google Scholar]
- 7.Glicklich M, Mendelson DS, Gendal ES, Teirstein AS. Tuberculous empyema necessitatis. Computed tomography findings. Clin Imaging. 1990;14:23–5. doi: 10.1016/0899-7071(90)90113-p. [DOI] [PubMed] [Google Scholar]
- 8.Sahoo M, Sahai K, Nayak VM. Scapulohumeral tuberculosis diagnosed by fine needle aspiration cytology. Acta cytologica. 1998;42:435–6. doi: 10.1159/000331632. [DOI] [PubMed] [Google Scholar]
- 9.Lee S, Abramson S. Infections of the musculoskeletal system by M tuberculosis. In: Rom W, Garay S, editors. Tuberculosis. Boston: Little Brown; 1996. pp. 635–44. [Google Scholar]
- 10.Tatelman M, Drouillard EJP. Tuberculosis of the ribs. Am J Roentgenol Radium Ther Nucl Med. 1953;70:923–35. [PubMed] [Google Scholar]
- 11.Mathlouthi A, Ben M’Rad S, Merai S, Friaa T, Mestiri I, Ben Miled K, et al. Tuberculosis of the thoracic wall. Presentation of 4 personal cases and review of literature. Rev Pneumol Clin. 1998;54:182–6. [PubMed] [Google Scholar]
- 12.Eid A, Chaudry N, el-Ghoroury M, Hawasli A, Salot WL, Khatib R. Multifocal musculoskeletal cystic tuberculosis without systemic manifestations. Scand J Infect Dis. 1994;26:761–4. doi: 10.3109/00365549409008649. [DOI] [PubMed] [Google Scholar]
- 13.Garcia S, Combalia A, Serra A, Segur JM, Ramon R. Unusual locations of osteoarticular tuberculosis. Arch Orthop Trauma Surg. 1997;116:321–3. doi: 10.1007/BF00433981. [DOI] [PubMed] [Google Scholar]
- 14.Chang DS, Rafii M, McGuinness G, Jagirdar JS. Primary multifocal tuberculous osteomyelitis with involvement of the ribs. Skeletal Radiol. 1998;27:641–5. doi: 10.1007/s002560050451. [DOI] [PubMed] [Google Scholar]
- 15.Faure E, Souilamas R, Riquet M, Chehab A, Le Pimpec-Barthes F, Manac’h D, et al. Cold abscess of the chest wall: a surgical entity? Ann Thorac Surg. 1998;66:1174–8. doi: 10.1016/s0003-4975(98)00770-x. [DOI] [PubMed] [Google Scholar]
- 16.Muradali D, Gold WL, Vellend H, Becker E. Multifocal osteoarticular tuberculosis: Report of four cases and review of management. Clin Infect Dis. 1993;17:204. [PubMed] [Google Scholar]
- 17.Ormerod LP, Grundy M, Rahman MA. Multiple tuberculous bone lesions simulating metastatic disease. Tubercle. 1989;70:305. doi: 10.1016/0041-3879(89)90027-5. [DOI] [PubMed] [Google Scholar]
- 18.Khan SA, Zahid M, Sharma B, Hasan AS. Tuberculosis of frontal bone: a case report. Indian J Tub. 2001;48:95–6. [Google Scholar]
- 19.Rubinstien EM, Lehmann T. Sternal osteomyelitis due to Mycobacterium tuberculosis following coronary artery bypass surgery. Clin Infect Dis. 1996;23:202. doi: 10.1093/clinids/23.1.202. [DOI] [PubMed] [Google Scholar]
- 20.Frouge C, Miquel A, Cochan-Priollet B, et al. Breast mass due to rib tuberculosis. Eur J Radiol. 1995;19:118. doi: 10.1016/0720-048x(94)00576-x. [DOI] [PubMed] [Google Scholar]
- 21.Kim YT, Han KN, Kang CH, et al. Complete resection is mandatory for tubercular cold abscess of the chest wall. Ann Thorac Surg. 2008;85:273. doi: 10.1016/j.athoracsur.2007.08.046. [DOI] [PubMed] [Google Scholar]
- 22.Karanas YL, Kim KK. Mycobacterium tuberculosis infection of the hand: A case report and review of the literature. Ann Plast Surg. 1998;40:65. doi: 10.1097/00000637-199801000-00014. [DOI] [PubMed] [Google Scholar]
- 23.Hadfield PJ, Shah BK, Glover GW. Facial palsy due to tuberculosis: The value of CT. J Laryngol Otol. 1995;109:1010. doi: 10.1017/s0022215100131895. [DOI] [PubMed] [Google Scholar]