Abstract
A patient with neurological symptoms underwent CT scan that showed a sellar and suprasellar mass with bone erosions, involving especially the clivus and the right petrous apex. The first diagnostic hypothesis was chordoma in relation to the mass position. The MRI showed a solid well-enhancing mass; moreover another circumscribed lesion, with similar signal pattern, was found in the left mandibular condyle. the signal and the presence of another lesion did not agree with diagnosis of chordoma. FDG-PET/CT study showed multiple pathological uptakes suggesting a metastatic disease. A trans-sphenoidal excisional biopsy was performed and the histopathological analysis showed a population of cells consistent with a plasmacell tumor, confirmed by the presence of a monoclonal gammopathy on blood analysis. Our case suggests that FDG-PET/CT can modify the diagnostic and therapeutic procedures in myeloma, by evaluating the bone marrow involvement.
Keywords: Chordoma, plasmacytoma, clivus lesion, FDG-PET
INTRODUCTION
A correct differential diagnosis among tumoral lesions that arise from the clivus is important in order to define the most effective therapeutic and surgical approach due to the critical neural structures in that location which must be preserved.
The most frequent benign lesions of the clivus are meningioma and chordoma; in the malignant group there are chondrosarcoma, plasmacytoma and metastases. Different surgical approaches are used, according to the location and extension of the disease. A cranial-orbitozygomatic approach is the most versatile for lesions that are located in the upper clivus and extend laterally; a transcondylar approach is used to reach intracranial lesions located at the inferior clivus, and a transmaxillary approach is used for lesions that extend from the clivus into the nasopharynx(1). Surgical and radiotherapic procedures can cause complications such as bleeding, cerebrospinal fluid leakage, nerve injury and extraocular muscle deficits (2).
Computed Tomography (CT) scan is far more sensitive than radiographs in the assessment of trabecular and cortical bone destruction. Magnetic Resonance Imaging (MRI) allows visualization of bone marrow involvement and it is the most sensitive technique for the detection of pathologies confined to the bone marrow, even when trabecular bone is not destroyed. Skeletal scintigraphy permits a functional approach in the research of bone lesions but sometimes, as in plasmacytoma, can result negative. The use of combined Fluorodeoxyglucose Positron Emission Tomography/Computed Tomography (FDG-PET/CT) scanning technique in the evaluation and management of patients with malignancies is increasing. However, its role in the identification of bone metastases is far from clear (3).
CASE REPORT
A 75 year-old man was referred to our center in July 2008 with forehead headache, cervical pain and reduction of visual acuity on the right side. A non-enanched CT scan detected a sellar and suprasellar mass of about 6 cm in diameter with bone erosions, grossly involving the clivus and extending to the right petrous apex. Contrasted-enanched CT scan (performed at an outside institution) showed an homogeneous enhancing mass without intra-lesional calcifications. The first diagnostic hypothesis was chordoma in relation to the mass location. A few days later the patient underwent MRI that showed a solid lesion with homogeneous low signal intensity on T2 weighted images (Fig. 1) and homogeneous iso-hyperintense signal on T1 weighted images (Fig. 2). After gadolinium (Gadovist 0.1ml/Kg) a homogeneous contrast enhancement was detected (Fig. 3).. The mass was centered in the clivus, extending cranially to the sellar region and laterally to the right pars petrosa of the temporal bone, involving surrounding anatomical structures such as the cavernous sinus. The carotid space was also involved, without a clear infiltration of the vessel. Moreover another circumscribed lesion, with similar signal and enhancement pattern, was found in the right mandibular condyle. This finding was confirmed with another CT (Fig 4) scan that showed a small lytic lesion with well defined borders.
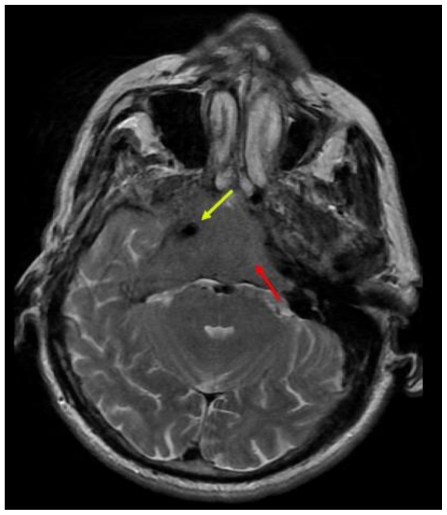
Figure 1.
75 year old man with plasmacell tumor arising from the clivus. Axial FSE T2 weighted image (1.5 T, TR 3540 msec, TE 106 msec) shows the presence of large lesion with homogeneous hypointense signal located in the clival region (red row) and extending to the right petrous apex (diameter 67×37 mm). There are encasement of the right internal carotid artery (yellow row) and mild compression of the pons. The first diagnostic hypothesis was chordoma in relation to the mass location.
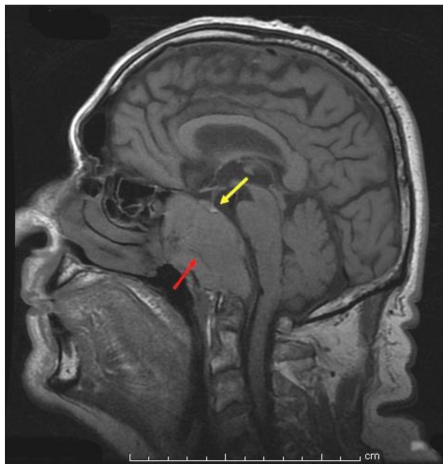
Figure 2.
75 year old man with plasmacell tumor arising from the clivus. Sagittal SE T1 (1.5 T, TR 560 msec, TE 12 msec) without contrast shows a lesion involving the clivus with homogeneous iso-hyperintense signal (red row) (diameter 60×37 mm). The sella turcica is also involved but pituitary gland is normally seen (yellow row).
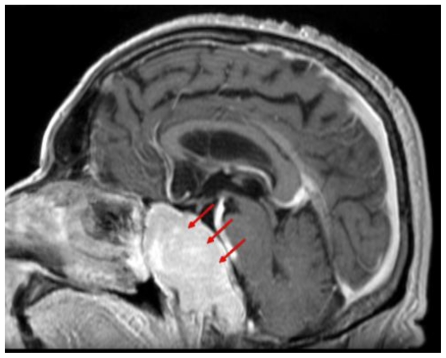
Figure 3.
75 year old man with plasmacell tumor arising from the clivus. Sagittal Gadolinium-enhanced T1-weighted SE image (1.5 T, TR 560 msec, TE 12 msec) showing a solid well-enhancing mass with extension and erosion of the clivus (diameter 67×37mm). The first diagnostic hypothesis was chordoma in relation to the mass location.
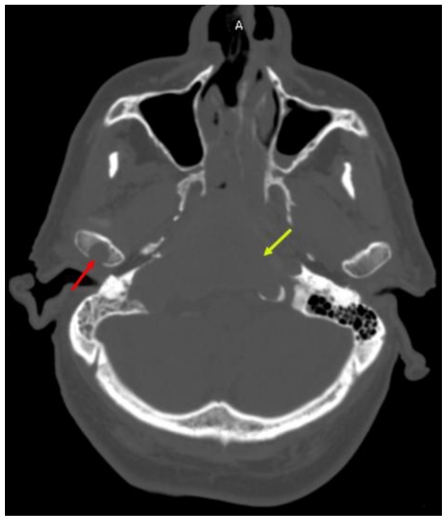
Figure 4.
75 year old man with plasmacell tumor arising from the clivus. Axial contrast enhanced CT scan in bone window (318 mAS, 140 KeV) shows a large lesion involving the clivus (yellow row) and extending to the right petrous apex with extensive bone erosion. A second small lytic lesion with well defined borders in the right mandibolar condyle is also present (red row).
The location of the mass was highly indicative of chordoma, but the signal, the enhancement pattern and the presence of another similar lesion in the mandibular condyle did not agree with this hypothesis. In order to exclude metastatic lesions a skeletal Technetium 99m-MDP scintigraphy was performed but no obvious pathological uptakes were detected.
In order to complete the staging and to define a metabolic characterization a FDG-PET/CT was performed using a PET total-body scan acquired 60 minutes after intravenous injection of FDG (248 MBq), using an integrated PET-CT device (Discovery ST, General Electric Medical Systems). Analysis of PET images showed an area of extensive and intense high radiotracer uptake in the clival and the sphenoid region (Fig. 5). Further pathological tracer uptakes were detected in the right clavicle, the right scapula, two thoracic vertebrae and right iliac bone, suggesting metastatic disease. (Fig. 6 and 7).
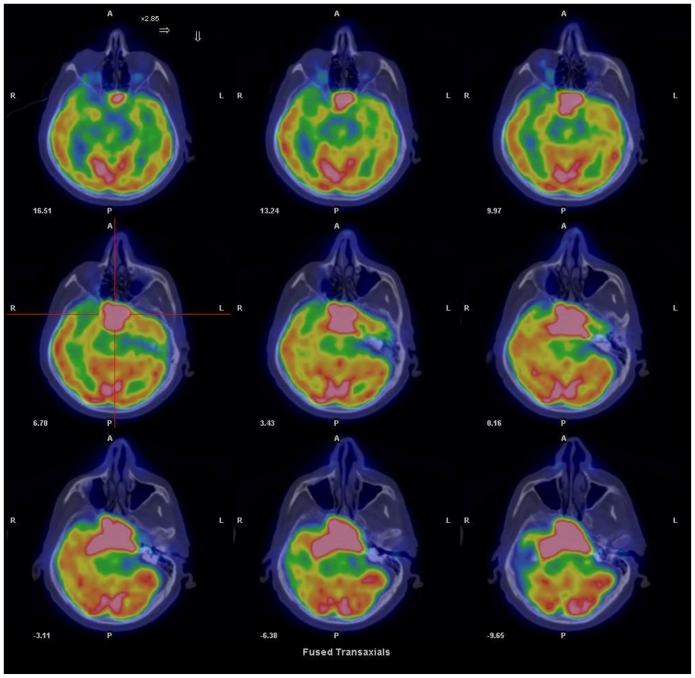
Figure 5.
75 year old man with plasmacell tumor arising from the clivus. Transverse FDG-PET/CT fusion images at level of lesion, at 60 min. post administration 248 MBq of 18F-FDG. The PET image shows an area of extensive and intense radiotracer uptake along the clivus and the sphenoid region, indicanting a lesion with features of high metabolic activity.
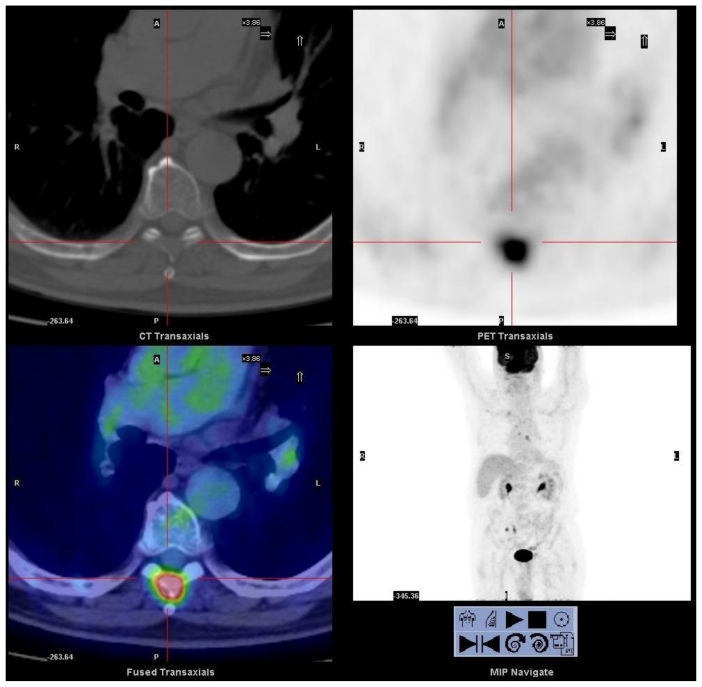
Figure 6.
75 year old man with plasmacell tumor arising from the clivus. An axial CT and FDG-PET/CT fusion images, at 60 min. post administration of 248 MBq 18F-FDG. At level of unexpected site of bone involvement, image shows a focal radiotracer uptake on spinous process of seventh thoracic vertebra.
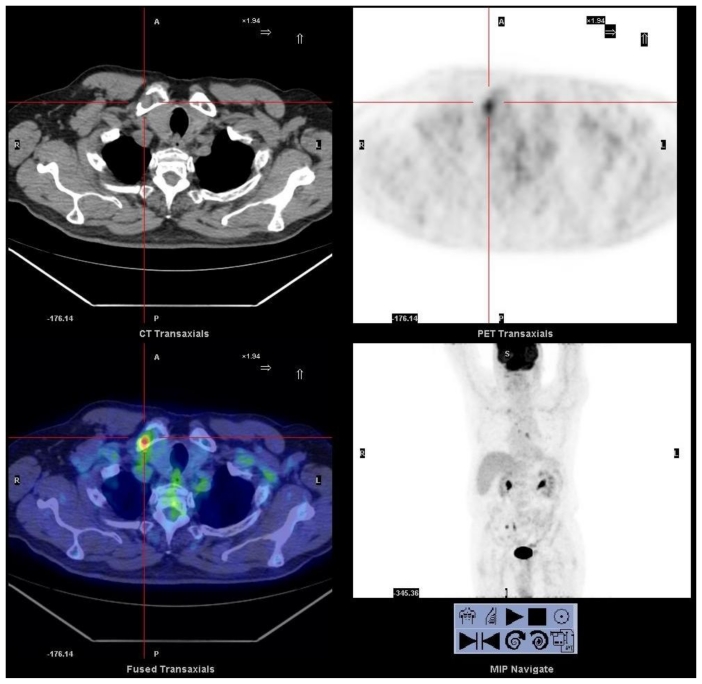
Figure 7.
75 year old man with plasmacell tumor arising from the clivus. An axial CT and FDG-PET/CT fusion images, at 60 min. post administration of 248 MBq 18F-FDG. At level of unexpected site of bone involvement image shows a focal pathological radiotracer uptake on right clavicle.
A trans-sphenoidal excisional biopsy was performed and the histopathological analysis showed a population of cells consistent with a plasmacell tumor, confirmed on blood analysis by the presence of a monoclonal gammopathy (Fig. 8). Then, the patient was referred to oncohaematological department and underwent to chemotherapy treatment.
Figure 8.
75 year old man with plasmacell tumor arising from the clivus. Photomicrograph of trans-sphenoidal excisional biopsy (original magnification, X100; hematoxylin-eosin stain) population of cells consistent with a plasmacell tumor, confirmed by the presence of a monoclonal gammopathy on blood analysis.
DISCUSSION
Chordomas are relatively rare tumors that arise from embryonic remnants of the primitive notochord, a primitive cell line around which the skull base and the vertebral column develops. Intracranial chordomas constitute one-third of all chordomas and most often originate from the spheno-occipital synchondrosis.
Radical surgery with free surgical margins is the most accurate curative treatment. The combination with proton beam radiation therapy achieves the best results (1).
In particular, in chordomas of the clivus, CT scans generally show a centrally located, well-circumscribed, soft-tissue mass with moderate enhancement following administration of iodinated contrast material and with associated extensive lytic bone destruction and irregular intratumoral calcification.
Classic findings of MRI in intracranial chordoma include intermediate to low signal intensity on T1-weighted images and high signal intensity on T2-weighted images. Enhancement is marked and often heterogeneous.
To our knowledge, there are no cases of multifocal chordomas reported in literature.
FDG-PET/CT is a hybrid diagnostic technique used for characterization of metabolically active masses, tumour staging and treatment response evaluation and radiotherapy treatment planning. In fact, it allows a combination of both anatomical and physiological co-registered images acquired in the same session, with a dual gain in diagnostic accuracy. At present there is no literature regarding the optimal use of FDG-PET for detection of both primary and recurrent chordoma (4).
Multiple Myeloma (MM) is a clonal neoplasm of terminally differentiated plasmacells. The solitary form (Plasmacytoma), typically presents as a lytic lesion that affects the spine, pelvis, skull, ribs, sternum, and proximal appendages. The mass can mimic intracranial chordoma when the skull base is involved. Important advances in the therapeutic management of this disease have resulted in higher rates of durable complete remission, prolonged event-free survival and improved overall survival.
CT scan findings in MM consist of punched-out lytic lesion, expansive lesions with soft-tissue mass, diffuse osteopenia, fractures and osteosclerosis rarely (5).
In MRI T1-weighted spin-echo images generally depict a focal plasmacytoma as a hypointense area. On T2-weighted spin-echo, gradient-echo, STIR images and gadolinium-enhanced images the focal lesions are hyperintense relative to the hypointense marrow background.
In skeletal scintigraphy the detection of bone involvement with technetium 99-m (99mTc) based bone scanning agents relies on an osteoblastic response of the skeleton. As MM is primarily an osteolytic neoplasm, bone scans obtained with 99mTc MDP usually underestimate the extent of the disease (6–7). The FDG-PET/CT shows focal uptake in the metabolically active lesion and may help in the detection of other unsuspected sites. FDG PET has improved the detection of tumoral lesions in patients with MM. In a recent study (8), in a series of 43 patients with MM and solitary plasmacytoma, Shirrmeister et al reported focal tracer uptake on FDG PET scans in 38 of 41 lesions (sensitivity, 93%) with known osteolytic pattern; FDG PET depicted 71 additional lesions undetected by radiographs in 14 patients. False-negative results, however, were reported with FDG PET in early disease. In advanced disease, differentiation of active from inactive myeloma with this technique may be difficult (9).
Another recent study (10) on a group of patients with solitary plasmacytoma of bone (SPB) (local disease) suggests that FDG PET/CT may detect further unsuspected sites of bone involvement, upstaging the extent of the disease. In these cases, SPB may be a local manifestation of multiple myeloma where other sites of involvement have eluded detection by other less sensitive imaging modalities (i.e. skeletal surveys) or anatomically restricted imaging (i.e., less than total body MRI or CT). Detecting other sites of involvement has significant implications for appropriate treatment of myeloma.
This case report underlines the role of FDG-PET/CT in the assessment of extra-cranial lesion masses arising from the clivus, with the definition of their metabolic activity, and especially for the possibility of a total body evaluation. This is important in defining the most effective and radical therapeutic and surgical approach according to the type of lesion, because the clivus contains critical neural structures which should be preserved. FDG-PET/CT shows different pattern of Fluorodeoxyglucose uptake in metabolically different lesions. In fact the plasmacytoma shows mild-intense signal (as confirmed in our case) while there is still no literature about the use of FDG-PET in chordoma.
In conclusion, our case report shows that FDG-PET/CT scan technique can modify the diagnostic and therapeutic procedures in cases of myeloma, by evaluating the bone marrow involvement. The ability of FDG-PET/CT to assess the whole body in a single procedure is an important advantage over standard imaging techniques such as MRI, CT or radiographs because this allows a complete staging. Moreover, this technique could be useful in monitoring response to therapy and can be used in follow up.
TEACHING POINT
FDG-PET/CT scan technique can modify the diagnostic and therapeutic procedures in myeloma, by evaluating the bone marrow involvement. By evaluation of the whole body, it permits a complete staging with a single procedure. Moreover, this technique could be useful in monitoring response to the treatment and it can be used in follow up.
ACKNOWLEDGEMENTS
Special thanks to Mrs Meredith Buxton for the drawing-up of the article, Dr. O. Iannone of Modern Culture and Language Department, University of the Study of Calabria and Dr. Francesco Cerando of the Departement of Cell Biology, University of Calabria, Italy URS medical college, Kolar for their valuable contributions.
ABBREVIATIONS
- CT
Computed Tomography
- MRI
Magnetic Resonance Imaging
- FDG-PET/CT
Fluorodeoxyglucose Positron Emission Tomography/Computed Tomography
- MM
Multiple Myeloma
REFERENCES
- 1.Erdem E, Angtuaco E, Van Hemert R, et al. Comprehensive review of intracranial chordoma. Radiographics. 2003;23:995–1009. doi: 10.1148/rg.234025176. [DOI] [PubMed] [Google Scholar]
- 2.Jiang WH, Xie ZH, Zhang H, et al. Prevention and management of complications of endoscopic surgery for nasal-skull base neoplasms. Chinese J Otorhinolaringology Head and Neck Surgery. 2008 Feb;43( 2):84–8. [PubMed] [Google Scholar]
- 3.Fogelman I, Cook G, Israel O, Van der Wall H. Positron emission tomography and bone metastases. Semin Nucl Med. 2005 Apr;35( 2):135–42. doi: 10.1053/j.semnuclmed.2004.11.005. [DOI] [PubMed] [Google Scholar]
- 4.Miyazawa N, Ishigame K, Kato S, et al. Thoracic chordoma: review and role of FDG-PET. JNeurosurg Sci. 2008 Dec;52(4):117–21. [PubMed] [Google Scholar]
- 5.Angtuaco E, Fassas A, Walker R, et al. Multiple Myeloma: clinical review and diagnostic imaging. Radiology. 2004 Apr;231(1):11–23. doi: 10.1148/radiol.2311020452. [DOI] [PubMed] [Google Scholar]
- 6.Scutellari PN, Spanedda R, Feggi LM, Cervi PM. The value and limitations of total body scan in the diagnosis of multiple myeloma: a comparison with conventional skeletal radiography. Haematologica. 1985 Mar-Apr;70(2):136–142. [PubMed] [Google Scholar]
- 7.Woolfenden JM, Pitt MJ, Durie BJM, Moon TE. Comparison of bone scintigraphy and radiology in multiple myeloma. Radiology. 1980 Mar;134(3):723–728. doi: 10.1148/radiology.134.3.7355226. [DOI] [PubMed] [Google Scholar]
- 8.Schirrmeister H, Bommer M, Buck AK, et al. Initial results in the assessment of multiple myeloma using F-18 FDG PET. Eur J Nucl Med Mol Imaging. 2002 Mar 29;(3):361–366. doi: 10.1007/s00259-001-0711-3. [DOI] [PubMed] [Google Scholar]
- 9.Bredella MA, Steinbach L, Caputo G, Segall G, et al. Value of FDG PET in the assessment of patients with multiple myeloma. AJR Am J Roentgenol. 2005 Apr;184(4):1199–1204. doi: 10.2214/ajr.184.4.01841199. [DOI] [PubMed] [Google Scholar]
- 10.Nanni C, Rubello D, Zamagni E, et al. 18F-FDG PET/CT in myeloma with presumed solitary plasmocytoma of bone. In Vivo. 2008 Jul-Aug;22(4):513–7. [PubMed] [Google Scholar]