Abstract
Esophageal Actinomycosis is a rare disease with only two previous reports in the Radiology literature. We present a 27 year-old African American male with a past medical history of a renal transplant for renal disease secondary to lupus who presented with odynophagia. The computed tomography and barium swallow findings are presented as well as a differential diagnosis of infectious esophageal diseases.
Keywords: Esophagus, actinomycosis
CASE REPORT
A 27 year old African American male with a past medical history significant for end stage renal disease secondary to lupus seven months status post cadaveric kidney transplant presented with a chief complaint of odynophagia. His immunosuppressive regimen included Prograf, prednisone, and plaquenil. He initially presented to his primary care physician with a chief complaint of two months of odynophagia. At that time the patient described his pain as sharp, non-radiating epigastric pain associated with swallowing, more severe with ingestion of solid foods. The patient failed a trial of Omeprazole 20 mg PO twice daily, during which time his symptoms progressed to a constant, epigastric pain with an associated 15 pound weight loss. Physical examination at the time of patient presentation was remarkable for bilateral perimolar ulcerations. The patient was subsequently referred to gastroenterology and radiology for further evaluation.
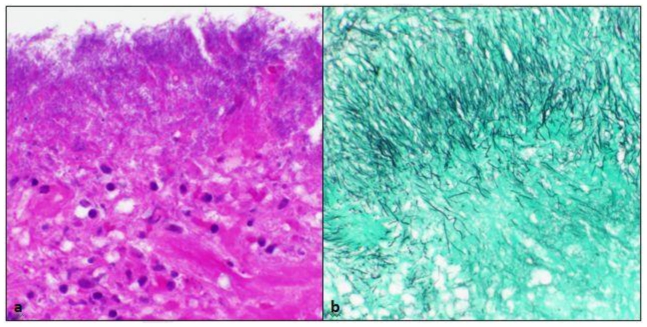
Esophagogastroduodenoscopy (Fig 1) identified an ulcerated lesion in the esophagus, approximately 27–32 cm from the incisors. A biopsy was taken of this lesion with histologic examination demonstrating ulcerated squamous mucosa with numerous branching filamentous bacterial organisms invading the granulation tissue. These bacteria were weakly gram positive and formed characteristic sulfur granules, consistent with Actinomyces species (Fig 2a,b).
Figure 1.
27 year old male with esophageal actinomycosis. Esophagogastro-duodenoscopy demonstrates an ulcerated lesion in the esophagus, approximately 27–32 cm from the incisors.
Figure 2.
27 year old male with esophageal actinomycosis. a. Biopsy specimen demonstrates ulcerated mucosa with extensive granulation tissue being infiltrated by filamentous bacteria, consistent with Actinomyces species (H&E, 200x). b. The filamentous nature of these bacteria is highlighted with the Gomori methamine silver stain (200x). No fungal hyphal elements or yeast forms were seen. A modified acid fast bacilli stain was negative, excluding the possibility of Nocardia. Additionally, immunohistochemistry for cytomegalovirus, adenovirus, and herpes simplex virus were all negative.
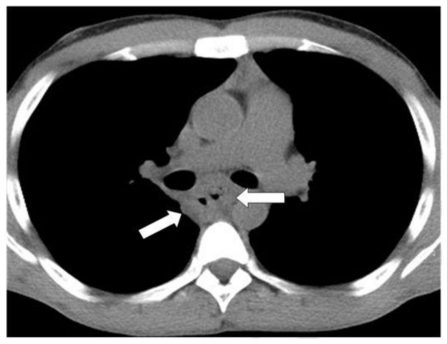
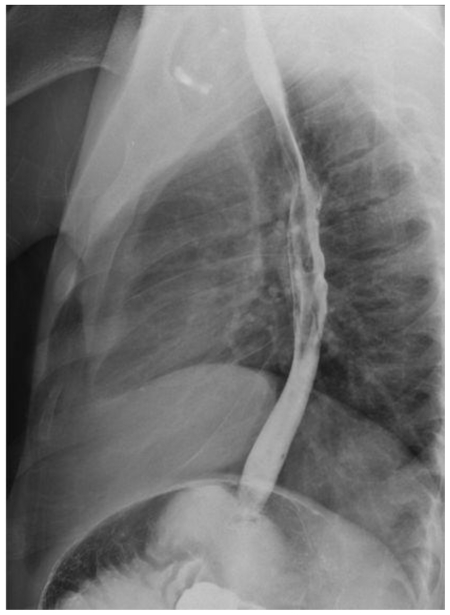
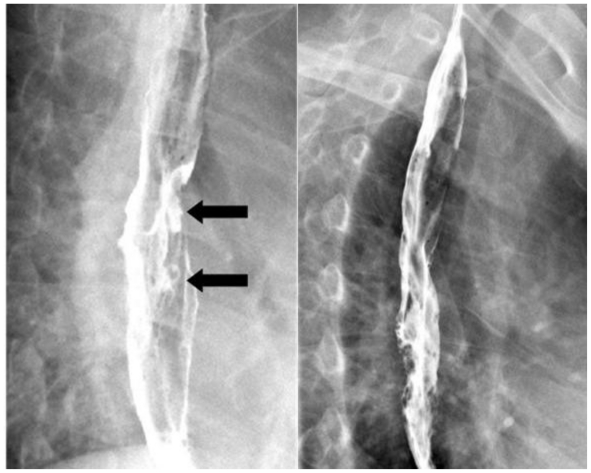
Subsequent computed tomography of the chest demonstrated esophageal wall thickening, most notable in the subcarinal region, out of proportion to what would be expected for simple underdistension (Fig. 3). In addition, scattered mediastinal and axillary lymph nodes were noted, most prominent in the anterior mediastinum, likely secondary to reactive adenopathy. However, there was no evidence of extraesophageal extension of the primary infectious process. To definitively exclude mediastinal actinomycotic extension, a barium swallow was performed which demonstrated esophageal ulcerations and mucosal irregularity in the middle third of the esophagus, consistent with the pathologic diagnosis of esophageal actinomycosis (Fig. 4 and 5).
Figure 3.
27 year old male with esophageal actinomycosis. Selected axial image from a noncontrast CT of the chest demonstrates diffuse esophageal wall thickening, most notable in the subcarinal region (arrows). There was no evidence of extraesophageal extension.
Figure 4.
27 year old male with esophageal actinomycosis. Overhead radiograph from a double-contrast esophagogram demonstrates mucosal irregularity in the middle third of the esophagus.
Figure 5.
27 year old male with esophageal actinomycosis. Two upright LPO spot images from a double-contrast esophagography demonstrate esophageal ulcerations in the middle third of the esophagus (arrows) with associated mucosal irregularity.
Following an infectious disease consult, the patient was initiated on a four week regimen of penicillin G, 3 million units intravenously every four hours, with a plan for transition to oral antibiotics. Following therapy, the patient subsequently recovered and as such no additional invasive testing or imaging was required.
DISCUSSION
Many different causes of infectious esophagitis have been reported in both immunocompetent and immunocompromised patient. Candida is the most common cause of infectious esophagitis (1). Candida esophagitis classically manifests on double-contrast studies as discrete plaque-like lesions, seen as linear or irregular filling defects, that tend to be oriented longitudinally and are separated by normal mucosa (2). However, a more fulminant form of candidiasis has been encountered in severely immunocompromised patients, with radiographic findings demonstrating a grossly irregular or "shaggy" esophagus caused by coalescent pseudomembranes and plaques, with trapping of barium between the lesions (3–4). Herpes simplex virus (HSV) is another common cause of infectious esophagitis. HSV esophagitis may manifest on double-contrast studies as small superficial ulcers against a background of normal mucosa (5). Cytomegalovirus (CMV) is a less common infectious cause of esophagitis, typified on double-contrast studies as multiple small ulcers or, more commonly, as one or more giant flat ulcers that are two to three centimeters or more in length (6). Human immunodeficiency virus (HIV) infection of the esophagus can lead to the development of giant esophageal ulcers which may be indistinguishable from those caused by CMV esophagitis (1). Double-contrast esophagography typically reveals one or more large ovoid or diamond-shaped ulcers surrounded by a radiolucent rim of edema, sometimes associated with a cluster of small satellite ulcers (7). Other reported causes of infectious esophagitis include tuberculosis and varicella (8–9). A much rarer cause of esophagitis, as reported in this case discussion, is actinomycosis. Based on a recent literature review (10), only 15 cases of esophageal actinomycosis have been reported since 1970. Such reported cases are understandably rare within the radiology literature, with only two reported cases (11, 12).
Actinomycetes, the causative organism in esophageal actinomycosis, are facultatively anaerobic, Gram-positive bacilli which are present as saprophytes in the soil. In addition, actinomycetes are often found in vaginal mucosa and in the normal intestinal tract, most commonly with in the oral cavity (10, 13). Although the species A. israelii is the most common Actinomyces found in humans, four other species (A. naeslundii, A. viscosus, A. A odontolyticus, and A. bovis) are known to exist (8). These organisms have a low degree of pathogenicity but can lead to severe infections, most commonly chronic cervicofacial suppurative infections. Less commonly, Actinomyces infections can occur in the abdominopelvic and pulmonothoracic areas (14). Actinomycosis of the central nervous system is rare, with brain abscess being the most common manifestation (15). However, infection with these organisms can occur in nearly any part of the body. When infections do occur, they are generally found in immunocompromised patients, though reports in immunocompetent patients are known (16–17). Generally, actinomyces infections are preceded by some known insult to the native mucosa (18), for example prior dental or surgical procedures, trauma, infection, or, in the case of pelvic actinomycotic infection, intrauterine device placement (19). In our case, the patient had no prior instrumentation to the esophagus, with actinomycotic infection likely occurring secondary to initial esophageal mucosal insult of unknown etiology.
Radiologic findings in Actinomycosis infection are not specific and depend greatly on the location of the disease. In general, the findings on imaging studies are consistent with the tendency of actinomycosis infection to spread through tissue planes. With regard to esophageal actinomycosis, barium esophograms may demonstrate deep ulcers with fistulas and multiple sinus tracts (11, 17). Alternatively, as in our case, barium esophogram may demonstrate only nonspecific shallow mucosal irregularities, ulcers, or potentially short segment strictures (findings which can be seen in much more common causes of infectious esophagitis, including Candida, herpes simplex virus, and cytomegalovirus) (1). CT demonstrates a thickened esophageal wall in the early stages of actinomycosis infection, with potential development of sinus tracts (11). PET imaging is also non-specific, and if performed may show increased FDG activity in the affected region secondary to the inflammatory process (12). In all cases, regardless of radiologic findings, definitive diagnosis must be made by bacterial culture or histologic examination of a biopsy specimen showing filamentous bacteria and classic sulfur granules.
Suggested treatment for thoracic and/or abdominal forms of actinomycosis is 4–6 weeks of intravenous penicillin, 3–4 million units intravenously every four hours, followed by oral pencillin or amoxicillin for 6–12 months (20, 21), as was prescribed for our patient, with a positive therapeutic outcome, and complete resolution of symptoms after 3 months. Tetracycline is the preferred antibiotic for individuals with penicillin allergy (22), although minocycline, erythromycin, clindamycin, ceftriaxone, and imipenem are also viable alternative treatments.
TEACHING POINT
Esophageal actinomycosis is a rare but important cause of esophageal pathology, particularly in the immunocompromised patient. Radiologic findings in Actinomycosis infection, including esophageal wall thickening on CT and mucosal irregularity/ulceration on double-contrast esophogram, can be suggestive of the entity but are nonspecific.
ABBREVIATIONS
- HSV
Herpes simplex virus
- CMV
Cytomegalovirus
- HIV
Human Immunodeficiency Virus
- CT
Computed Tomography
- EGD
esophagogastroduodenoscopy
REFERENCES
- 1.Levine MS, Rubenstein SE. Diseases of the esophagus: diagnosis with esophagography. Radiology. 2005;237:414–427. doi: 10.1148/radiol.2372050199. [DOI] [PubMed] [Google Scholar]
- 2.Levine MS, Macones AJ, Laufer I. Candida esophagitis: accuracy of radiographic diagnosis. Radiology. 1985;154:581–587. doi: 10.1148/radiology.154.3.3969456. [DOI] [PubMed] [Google Scholar]
- 3.Levine MS. Esophagus: Differential Diagnosis. In: Gore RM, Levine MS, editors. Textbook of Gastrointestinal Radiology. 2nd edition. Philadelphia: WB Saunders; 2000. p. 523. [Google Scholar]
- 4.Levine MS, Woldenburg R, Herlinger H, Laufer I. Opportunistic esophagitis in AIDS: radiographic diagnosis. Radiology. 1987;165:815–820. doi: 10.1148/radiology.165.3.2825235. [DOI] [PubMed] [Google Scholar]
- 5.Levine MS, Laufer I, Kressel HY, Friedman HM. Herpes esophagitis. Am J Roentgenol. 1981;136:863–866. doi: 10.2214/ajr.136.5.863. [DOI] [PubMed] [Google Scholar]
- 6.Balthazar EJ, Megibow AJ, Hulnick D, Cho KC, Beranbaum E. Cytomegalovirus esophagitis in AIDS: radiographic features in 16 patients. Am J Roentgenol. 1987;149:919–923. doi: 10.2214/ajr.149.5.919. [DOI] [PubMed] [Google Scholar]
- 7.Sor S, Levine MS, Kowalski TE, Laufer I, Rubesin SE, Herlinger H. Giant ulcers of the esophagus in patients with immunodeficiency virus: clinical, radiographic, and pathologic findings. Radiology. 1995;194:447–451. doi: 10.1148/radiology.194.2.7824725. [DOI] [PubMed] [Google Scholar]
- 8.Semaan GK, Dittus K, Nassour DN, Shaikh MA, Young MF. Actinomycosis esophagitis in a patient with persistent dysphagia. Southern Medical Association. 2005:662–664. doi: 10.1097/01.SMJ.0000163312.19136.47. [DOI] [PubMed] [Google Scholar]
- 9.Mandell GL, Bennett JE, Dolin R, editors. Principles and practice of infectious disease. 4th edition. New York: Churchill Livingston Inc.; 1995. p. 2286. [Google Scholar]
- 10.Abdall J, Myers J, Moorman J. Actinomycotic infection of the oesophagus. Journal of Infection. 2005;51:39–43. doi: 10.1016/j.jinf.2004.08.011. [DOI] [PubMed] [Google Scholar]
- 11.Spencer GM, Roach D, Skucas J. Actinomycosis of the esophagus in a patient with AIDS: findings on barium esophograms. Am J Roentgenol. 1993;161:795–796. doi: 10.2214/ajr.161.4.8372761. [DOI] [PubMed] [Google Scholar]
- 12.Ho L, Seto J, Jadvar H. Actinomycosis mimicking anastamotic anastamotic recurrent esophageal cancer on PET-CT. Clin Nucl Med. 2006;31( 10):646–647. doi: 10.1097/01.rlu.0000238193.34543.b9. [DOI] [PubMed] [Google Scholar]
- 13.Weese EC, Smith IM. A study of 57 cases of actinomycosis over a 36 year period: a diagnostic 'failure' with good prognosis after treatment. Arch Intern Med. 1975;135:1562–1568. [PubMed] [Google Scholar]
- 14.Manfredi R, Mazzoni A, Cavicchi O, et al. Invasive mycotic and actinomycotic oropharyngeal and craniofacial infection in two patients with AIDS. Mycoses. 1994;37:209–215. doi: 10.1111/j.1439-0507.1994.tb00302.x. [DOI] [PubMed] [Google Scholar]
- 15.Russo TA. Agents of Actinomycosis. In: Mandell GL, Bennett JE, Dolin R, editors. Mandell, Douglas, and Bennett's Prinicples and Practice of Infectious Disease. 5th ed. Philadelphia: Churchill Livingstone; 2000. pp. 2645–2654. [Google Scholar]
- 16.Mpilo Hospital Rounds: Actinomycosis of the esophagus. Cent Afr J Med. 1970;16:216–218. [PubMed] [Google Scholar]
- 17.Ng FH, Wong SY, Chang SM, Lai ST, Chau KY. Esophageal actinomycosis: a case report. Endoscopy. 1997;29:133. doi: 10.1055/s-2007-1004092. [DOI] [PubMed] [Google Scholar]
- 18.Burden P. Actinomycosis. J Infect. 1989;19:95–99. doi: 10.1016/s0163-4453(89)91739-8. [DOI] [PubMed] [Google Scholar]
- 19.Russo TA. Actinomycosis. In: Fauci AS, Braunwald E, Isselbacher KJ, et al., editors. Harrison's Principles of Internal Medicine. 14th ed. New York: McGraw-Hill; 1998. pp. 989–991. [Google Scholar]
- 20.Poles MA, McMeeking AA, Scholes JV, Dietrich DT. Actinomyces infection of a cytomegalovirus esophageal ulcer in two patients with acquired immunodeficiency syndrome. Am J Gastroenterology. 1994;89:1569–1572. [PubMed] [Google Scholar]
- 21.Chou FT, Cheng KS, Chiang I-P. Esophageal Actinomycosis. Advances in Therapy. 2006;23:623–626. doi: 10.1007/BF02850050. [DOI] [PubMed] [Google Scholar]
- 22.Arora AK, Nord J, Olofinlade O, Javors B. Esophageal Actinomycosis: A case report and review of the literature. Dysphagia. 2003;18:27–31. doi: 10.1007/s00455-002-0080-5. [DOI] [PubMed] [Google Scholar]