Abstract
Isolated cortical vein thrombosis is an uncommon condition and often difficult to diagnose, both clinically and radiologically. We report a case of a 38 years old man who presented with headache of new onset and clinical examination was unremarkable. The unenhanced brain CT did not reveal any abnormality. In view of unrelenting headache and partial seizures, we performed magnetic resonance imaging (with axial T1, T2 and gradient echo sequences, coronal FLAIR, diffusion weighted imaging as well as Gadolinium contrast-enhanced images) and magnetic resonance venography of the brain that revealed an isolated parietal cortical vein thrombosis with the rarely reported 'cord sign'. We report the clinical and radiological findings in our patient with isolated parietal cortical vein thrombosis.
Keywords: Cortical vein thrombosis, cord sign
CASE REPORT
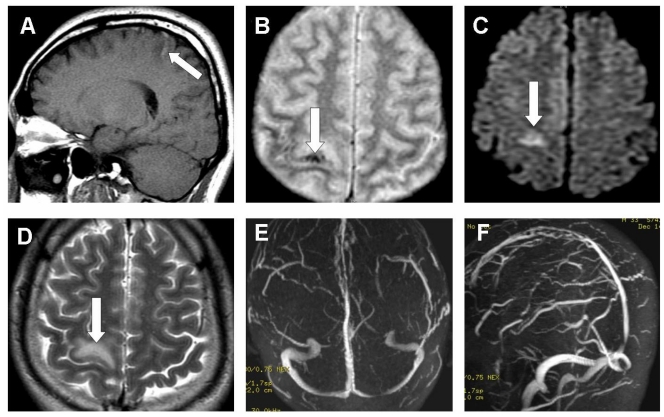
A 38-years-old Chinese male presented with history of right occipital sharp and continuous headache of new onset for 5 days. Headache was unrelenting and only partially relieved by analgesics. He did not have fever, nausea, vomiting, photophobia or phonophobia. He had two short episodes of jerking of left upper extremity without any generalization or change in his level of consciousness. There was no previous history of frequent headaches, diabetes mellitus, hypertension, autoimmune or connective tissue disorders. On clinical examination, he was found to be fully conscious, normotensive and afebrile. Neurological examination was unremarkable. Routine laboratory tests, unenhanced CT scan of the brain (Fig. 1) and electroencephalography were unremarkable. In view of the new onset localized headache and partial seizures, magnetic resonance imaging (MRI) of the brain was performed. MRI of the brain included axial T1, T2 and gradient echo sequences, coronal FLAIR, diffusion weighted imaging as well as Gadolinium contrast-enhanced images. A small high parietal cortical hemorrhagic infarction was noted on the right side (Fig. 2A, 2B, 2C) with a prominent hyperintense signal on the cerebral surface in sagital T1-weighted sequence (Fig. 2D), suggesting an acutely thrombosed isolated cortical vein. Magnetic resonance angiography of the brain was unremarkable. On magnetic resonance venography (MRV) of the brain, all major venous sinuses were patent and did not show any abnormal signals (Fig. 2E, 2F). Investigations for hypercoagulable states as well as connective tissue markers were unremarkable. He was treated with anti-epileptic medications and anticoagulated, initially with heparin and later with oral coumadin. Headache subsided by day 3 and he didn’t have any focal seizures. He has remained asymptomatic and without any neurological deficits, when seen in the outpatient clinic 2 months after discharge from the hospital.
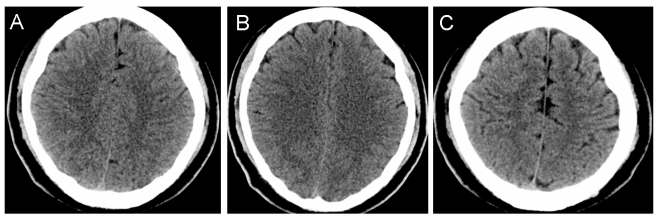
Figure 1.
A non-contrast enhanced CT scan of the brain in a 38 years old man presenting with right parietal cortical vein thrombosis, showing no abnormality.
Figure 2.
38 years old man with right parietal cortical vein thrombosis. Magnetic resonance imaging of the brain: Sagittal T1 (A) sequence shows a hyperintense signal in the right parietal region, axial gradient echo (B) sequence demonstrates the hemorrhagic component as susceptibility artifact, diffusion weighted (C) imaging shows a bright signal in the right parietal region with a corresponding hyperintense signal on axial T2 weighted (D) imaging. Normal patency of the major cerebral venous sinuses is seen on magnetic resonance venography (E and F).
DISCUSSION
Cerebral sino-venous thrombosis is a relatively uncommon but a potentially life-threatening condition, accounting for 1% to 2% of strokes in young adults. Compared to dural venous sinus thrombosis, isolated cortical vein thrombosis is an uncommon condition and often difficult to diagnose, both clinically as well as radiologically (1). The clinical presentations are non-specific and the typically described ‘cord sign’ is seen rarely (2). MRI is the most appropriate diagnostic tool as it may enable direct visualization of the thrombus in the affected superficial cortical vein as well as the secondary changes of venous outflow obstruction, seen in the form of swollen gyri as a result of venous congestion. In our patient, an area of T2 hyperintensity was noted surrounding the thrombosed cortical vein, suggestive of a small infarct. However, we did not perform the ADC mapping and this area could also represent a T2-shine-through phenomenon. Many patients with isolated cortical venous thrombosis have underlying coagulation abnormalities or chronic inflammatory conditions such as inflammatory bowel disease (3). Our patient did not suffer from any illness predisposing him for venous thrombosis and no coagulation abnormalities were noted on the laboratory testing.
The neuroimaging features of isolated cortical venous thrombosis include direct visualization of the thrombus, localized hemorrhage or venous infarction. Visualization of the clot within a thrombosed cortical vein on CT scans is often described as the ‘cord sign’ (4). MRI equivalent of the cord sign can be difficult to identify, especially during the early phase as the clot tends to be isointense with brain on T1-weighted images and hypointense on T2-weighted images, appearing as flow void. From 3 to 7 days after thrombosis, the clot becomes hyperintense on both T1- and T2-weighted images and is thus easier to identify.
Certain other conditions can present with focal intracerebral hemorrhage and include intracranial vascular malformations, hemorrhage transformation in ischemic infarctions, bleeding into a tumor, cerebral arteritis, aneurysm rupture, systemic hypertension, trauma and various coagulation disorders. MRI and MR angiography can differentiate most of these pathological conditions. Conventional catheter angiography may be required at time, particularly when looking for subtle vasculitic changes, small arteriovenous malformations, and some dural arteriovenous shunts. In conclusion, we describe the clinical and imaging findings in a patient with isolated cortical vein thrombosis. A high index of clinical suspicion is often required for the diagnosis of isolated cortical vein thrombosis, especially in patients presenting with headache and focal seizures of new-onset.
TEACHING POINT
Isolated cortical vein thrombosis is an uncommon diagnosis. A high index of suspicion for isolated cortical vein thrombosis is needed in patients presenting with headache and focal seizures of new-onset with a normal brain CT and MRI brain (with Axial T1 and T2 weighted, FLAIR, Gradient-echo, diffusion-weighted as well as MR venography of the brain) should be performed for a definitive diagnosis.
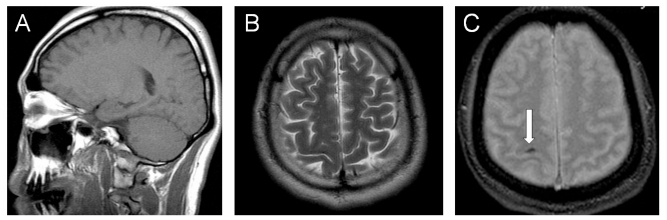
Figure 3.
38 years old man with right parietal cortical vein thrombosis. MRI of the brain repeated about 5 months later. Sagittal T1-weighted (A) and axial T2-wieghted (B) images show disappearance of the hyperintense signals noted in the previous study (Figure 2). Axial gradient-echo imaging (C) demonstrates in the right parietal region susceptibility artifact due to hemosiderin, representing old hemorrhage.
ABBREVIATIONS
- MRI
Magnetic Resonance Imaging
- MRV
Magnetic resonance venography
- FLAIR
Fluid attenuated inversion recovery
REFERENCES
- 1.Jacobs K, Moulin T, Bogousslavsky J, Woimant F, Dehaene I, Tatu L, Besson G, Assouline E, Casselman J. The stroke syndrome of cortical vein thrombosis. Neurology. 1996;47:376–382. doi: 10.1212/wnl.47.2.376. [DOI] [PubMed] [Google Scholar]
- 2.Leach JL, Bulas RV, Ernst RJ, Cornelius RS. MR imaging of isolated cortical vein thrombosis: the hyperintense vein sign. J Neurovasc Dis. 1996;1:1–7. [Google Scholar]
- 3.Derdeyn CP, Powers WJ. Isolated cortical venous thrombosis and ulcerative colitis. AJNR Am J Neuroradiol. 1998;19:488–490. [PMC free article] [PubMed] [Google Scholar]
- 4.Ahn TB, Roh JK. Cerebral venous thrombosis in adults: the role of imaging evaluation and management. Arch Neurol. 2003;60:1314–1316. [Google Scholar]