Abstract
Guillain-Barré syndrome is a relatively common, acute, and rapidly progressive, inflammatory demyelinating polyneuropathy. The diagnosis is usually established on the basis of symptoms and signs, aided by cerebrospinal fluid findings and electrophysiologic criteria. Previously, radiologic examinations have been used only to rule out other spinal abnormalities. We report a case of systemic lupus erythematosus associated with Guillain-Barré syndrome with marked enhancement of nerve roots of the conus medullaris and cauda equina on MR imaging. These MR observations may help confirm the diagnosis of Guillain-Barré syndrome.
Keywords: Guillain-Barré syndrome, spinal MRI
CASE REPORT
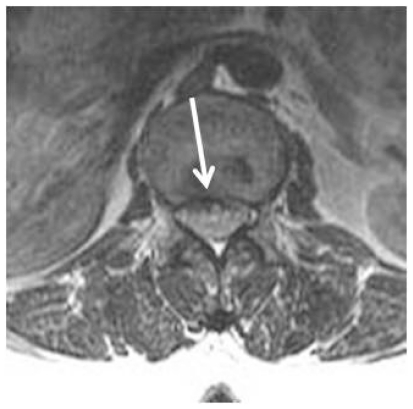
A 39-year-old woman with systemic lupus erythematosus presented with bilateral lower extremity weakness. Neurologic examination revealed absent deep tendon reflexes. Cerebrospinal fluid examination revealed a normal cell count and elevated protein concentration. Antinuclear antibodies were positive in the blood. Electrodiagnostic studies revealed prolonged distal latencies and slowed motor conduction velocities, confirming the diagnosis of polyradiculoneuropathy. The patient underwent thoracic and lumbar spine MR imaging. Spine MR examination was performed using a 1.5-Tesla MR scanner (Siemens Symphony, Erlangen, Germany). Imaging studies included axial and sagittal spin echo T1- weighted image, sagittal and axial turbo spin echo T2-weighted images, and post-contrast axial and sagittal fat suppressed spin echo T1-weighted images. Precontrast MRI of spine imaging showed disc herniation at T12-L1 level. Spinal cord and dural sac was normal (Fig 1-5). Contrast-enhanced T1-weighted MR imaging revealed marked enhancement of the anterior and posterior nerve roots in the conus medullaris and cauda equina (Fig 6,7). The patient underwent plasmapheresis, with near complete resolution of symptoms by 6 weeks. A follow-up MR was not obtained.
Figure 1.
39 year-old female with Guillain-Barré syndrome secondary to systemic lupus erythematosus. She presented with progressive bilateral lower extremity weakness. Sagittal TSE T2-weighted MR image demonstrates disc herniation at T12-L1 level (arrow). The herniated disk is seen to cause minimally conus medullaris compression.
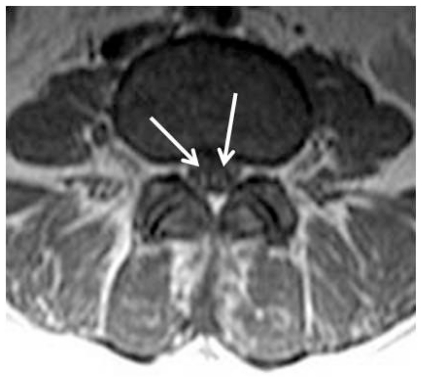
Figure 5.
39 year-old female with Guillain-Barré syndrome secondary to systemic lupus erythematosus. There are no abnormalities on the precontrast axial SE T1-weighted MR image at the level of the L4 vertebrae.
Figure 6.
39 year-old female with Guillain-Barré syndrome secondary to systemic lupus erythematosus. Contrast – enhanced fat suppressed sagittal T1-weighted MR imaging shows marked contrast enhancement of thickened nerve roots of cauda equina and conus medullaris (arrows).
Figure 7.
39 year-old female with Guillain-Barré syndrome secondary to systemic lupus erythematosus. Contrast – enhanced axial T1-weighted MR imaging shows marked enhancement of the nerve roots in the conus medullaris and cauda equina (arrows).
DISCUSSION
Guillain-Barré syndrome is characterized as an acute, symmetrically progressive, inflammatory demyelinating polyneuropathy. Clinical presentation is usually characterized by progressive ascending and symmetric paralysis of the extremities and marked hyporeflexia or areflexia (1, 2). It is the most frequent cause of acute flaccid paralysis throughout the world. In approximately two thirds of cases, a mild respiratory or gastrointestinal tract infection precedes the onset of symptoms. Surgical procedures, lymphoma, and systemic lupus erythematosus are other predisposing factors. Cerebro-spinal fluid analysis typically reveals elevated protein concentrations without pleocytosis (3). Because the diagnosis of Guillain-Barré syndrome is determined mainly on the basis of clinical findings and CSF analysis, most imaging studies are realized to exclude other conditions. There are several reports on the MR imaging findings of Guillain-Barré syndrome. These reports note that there was marked enhancement of the thickened nerve roots in the conus medullaris and cauda equina, although there are no abnormalities on precontrast images (1, 5). Byun et al suggested that enhancement solely of the anterior roots was strongly suggestive of Guillain-Barré syndrome (1). In our case, while precontrast images were normal, postcontrast images showed marked enhancement of the thickened anterior and posterior nerve roots in the conus medullaris and cauda equina.
On enhanced MR imaging, the spinal cord and nerve roots in the thecal sac generally do not take up much gadolinium because of the blood-nerve barrier or blood-brain barrier. Therefore, marked enhancement of nerve roots indicates a breakdown of the blood-nerve barrier. It is thought to correlate with the inflammatory infiltration of Guillain-Barré syndrome (6). However, enhancement of the spinal roots is a nonspecific finding that can be seen in neoplastic or other inflammatory processes, such as meningeal carcinomatosis, sarcoidosis, lymphoma, AIDS-related cytomegalovirus polyradiculopathy, Lyme disease, postoperative arachnoiditis and chronic inflammatory demyeinating polyneuropathy. Like Guillain-Barré syndrome, these intradural-extramedullary conditions are accompanied by an elevated level of protein in cerebrospinal fluid (5).
Some recent studies have suggested contrast-enhanced MR imaging in monitoring the response to therapy given (2, 4). Serial imaging may be useful in monitoring the response to therapy (1).
In conclusion, most patients with signs and symptoms strongly suggestive of Guillain-Barré syndrome don’t have to undergo MR imaging. Contrast-enhanced spinal MR imaging can be used as a supplementary diagnostic modality in the diagnosing of Guillain-Barré syndrome, especially when the clinical and electrophysiologic findings are equivocal
TEACHING POINT
The diagnosis of Guillain-Barré syndrome is determined mainly on the basis of clinical findings and CSF analysis. Most imaging studies are performed to exclude other conditions. However, contrast-enhanced spinal MR imaging can be used as a supplementary diagnostic modality in the diagnosing of Guillain-Barré syndrome and in monitoring response to theraphy.
Figure 2.
39 year-old female with Guillain-Barré syndrome secondary to systemic lupus erythematosus. Axial TSE T2-weighted MR image demonstrates disc herniation at T12-L1 level (arrow).
Figure 3.
39 year-old female with Guillain-Barré syndrome secondary to systemic lupus erythematosus. The nerve roots in the conus medullaris and cauda equina are normal on the axial TSE T2-weighted MR image at the level of the L4 vertebrae (arrow).
Figure 4.
39 year-old female with Guillain-Barré syndrome secondary to systemic lupus erythematosus. Precontrast sagittal SE T1-weighted MR image demonstrates disc herniation at T12-L1 level. Conus medullaris and dural sac demonstrate no abnormality.
ABBREVIATIONS
- MRI
Magnetic Resonance Imaging
REFERENCES
- 1.Byun WM, Park WK, Park BH, Ahn SH, Hwang MS, Chang JC. Guillain-Barré syndrome: MR imaging findings of the spine in eight patients. Radiology. 1998 Jul;208(1):137–41. doi: 10.1148/radiology.208.1.9646804. [DOI] [PubMed] [Google Scholar]
- 2.Coskun A, Kumandas S, Paç A, Karahan OI, Guleç M, Baykara M. Childhood Guillain-Barré syndrome. MR imaging in diagnosis and follow-up. Acta Radiol. 2003 Mar;44(2):230–5. doi: 10.1080/j.1600-0455.2003.00023.x. [DOI] [PubMed] [Google Scholar]
- 3.Fulbright RK, Erdum E, Sze G, Byrne T. Cranial nerve enhancement in the Guillain-Barré syndrome. AJNR Am J Neuroradiol. 1995 Apr;16(4):923–5. [PMC free article] [PubMed] [Google Scholar]
- 4.Iwata F, Utsumi Y. MR imaging in Guillain-Barré syndrome. Pediatr Radiol. 1997 Jan;27(1):36–8. doi: 10.1007/s002470050059. [DOI] [PubMed] [Google Scholar]
- 5.Baran GA, Sowell MK, Sharp GB, Glasier CM. MR findings in a child with Guillain-Barré syndrome. AJR Am J Roentgenol. 1993 Jul;161(1):161–3. doi: 10.2214/ajr.161.1.8517296. [DOI] [PubMed] [Google Scholar]
- 6.Matsuki M, Okada N, Matsuo M. Case report: MR findings of Guillain-Barré syndrome. Radiat Med. 1998 Mar-Apr;16(2):133–5. [PubMed] [Google Scholar]