Abstract
Fibro-osseous lesions of the face and paranasal sinuses are relatively uncommon. These lesions have overlapping clinical, radiologic and pathologic features causing difficulty in diagnosis. Neoplastic fibro-osseous paranasal sinus lesions can be benign or malignant. The benign fibro-osseous lesions described are: ossifying fibroma (and its histologic variants) and fibrous dysplasia. The variants of ossifying fibroma differ in the nature of calcified material (i.e. cementum versus bone), in the location of the lesion (oral versus paranasal sinus or orbital), other morphologic variations (presence of psammomatoid concretions) and biologic behavior (aggressive versus stable). Presence of cementum or bone classifies the lesion as cementifying fibroma or ossifying fibroma respectively while lesions with mixture of both cementum and bone are called cemento-ossifying fibroma. We describe a case of a young adult male with cemento-ossifying fibroma of paranasal sinus presenting acutely as left orbital cellulitis with proptosis.
Keywords: Cemento-ossifying fibroma, Paranasal sinus, CT, MRI
CASE REPORT
A 25 year old male patient presented to the emergency department with left periorbital swelling and redness of two days duration. He had a cold and nasal congestion for last five days. He subsequently noticed swelling around the left eye with redness which had progressed. There was no history of reduction of vision, headache, fever or nasal bleeding. No history of any chronic illness was present.
Physical examination was unremarkable. Ophthalmic examination revealed left periorbital swelling with lid redness and oedema, conjunctival chemosis and diminished eye movement in lateral and superior gaze. Vision and color vision was normal. Cornea was clear. Pupil, anterior chamber and optic disc were normal.
LABORATORY INVESTIGATIONS
Total WBC count was normal but there was mild neutrophilia. ESR was elevated. Nasal swab showed no polymorphonuclear cells, epithelial cells or organisms. Culture revealed scanty growth of Klebsiella pneumoniae. Blood glucose levels and renal function tests were normal.
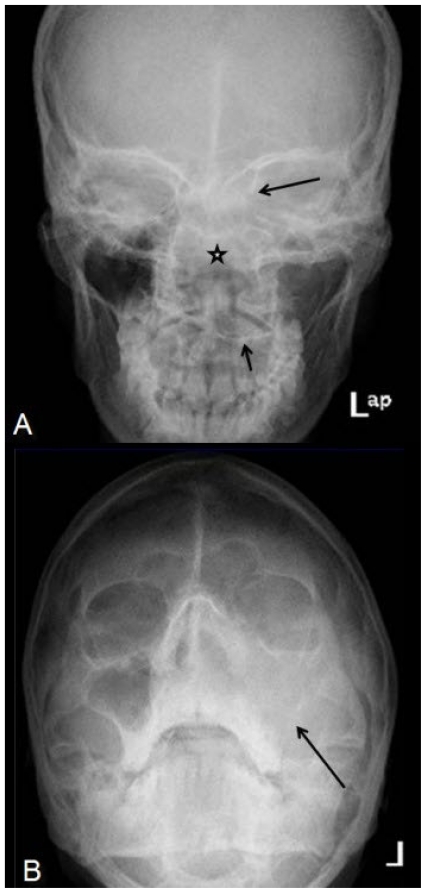
A diagnosis of left orbital cellulitis was made clinically and radiograph of the skull and paranasal sinuses were performed. The AP skull radiograph revealed expanded nasal cavity with non visualized ethmoid sinus trabeculae, depressed left half of the hard palate and ill defined left medial orbital wall (Fig 1a). Occipito-mental view showed soft tissue opacity occupying the left nasal cavity and left maxillary sinus region with non visualized maxillary sinus walls (Fig 1b).
Figure 1.
25-year-old male patient with cemento-ossifying fibroma of the paranasal sinuses presenting with left orbital and periorbital redness and swelling. A: AP Skull radiograph (upper image) shows expanded nasal cavity (asterix) with depressed left half of hard palate (short black arrow) and ill-defined left medial orbital wall (black arrow). The ethmoid sinus trabeculae are not delineated. B: Occipitomental view (lower image) shows soft tissue opacity occupying the left nasal cavity and left maxillary sinus region with nonvisualized maxillary sinus walls (long black arrow).
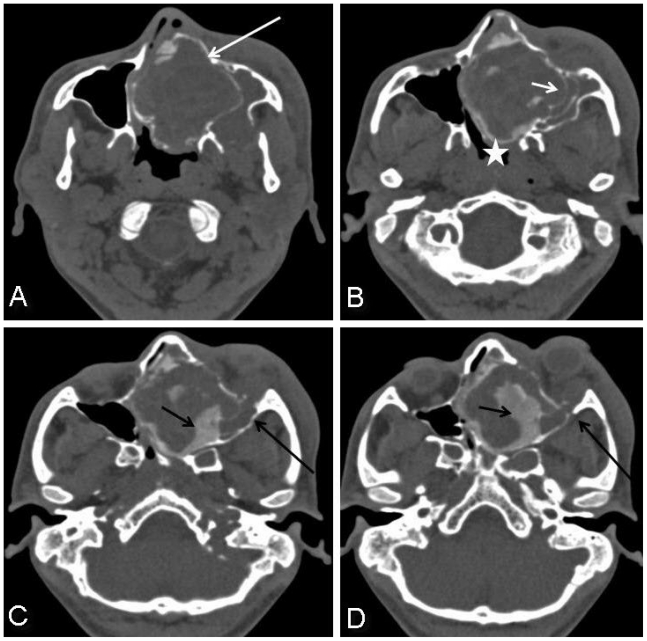
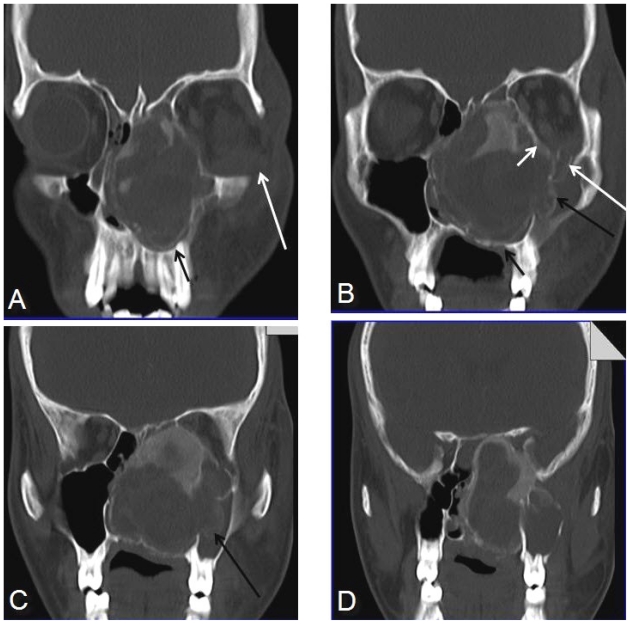
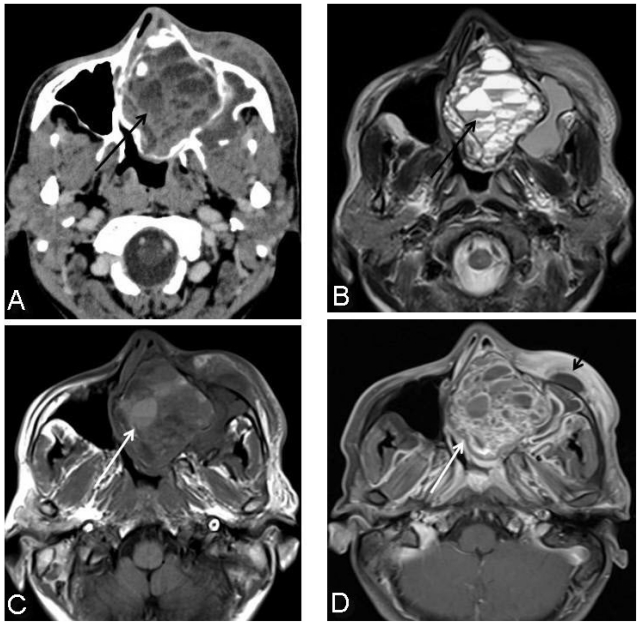
Subsequently a CT orbit and paranasal sinuses was requested. Plain and contrast enhanced CT paranasal sinus showed a large expansile well circumscribed corticated left sinonasal mass involving left ethmoid and maxillary sinuses and left nasal cavity eroding the left maxillary sinus and medial left orbital walls (Fig. 2a, 2b, 3b, 3c). There were plaque like areas of high density within the lesion (180–220 HU) suggesting calcification or ossification (Fig. 2c, 2d). The lesion showed extension into left orbit via inferior orbital fissure causing left orbital proptosis (Fig. 2c, 2d, 3a, 3b). The mass was seen remodelling the alveolar process of left maxilla (Fig. 3a, 3b). No intracranial extension was noted. The postcontrast images revealed multiple small pockets of hypodense areas with fluid-fluid levels within the lesion (Fig. 4a).
Figure 2.
25-year-old male with cemento-ossifying fibroma of paranasal sinus presenting acutely as orbital cellulitis. Axial noncontrast CT paranasal sinus images in bone window reveal a large, expansile, well-circumscribed, corticated left sinonasal mass involving the left ethmoid sinus, nasal cavity and left maxillary sinus (2a, white arrow). The mass is remodelling the left maxillary sinus medial wall (2b, small arrow) and bulging into the left side of nasopharynx (2b, asterix). There are plaque-like areas of high density (180 – 220 HU) within the lesion suggestive of calcification or ossification (2c, small black arrow and 2d). The lesion extends into the left orbit via inferior orbital fissure causing left orbital proptosis (2c, long black arrow and 2d).
Figure 3.
25-year-old male with cemento-ossifying fibroma of paranasal sinus presenting acutely as orbital cellulitis. Coronal; CT paranasal sinus images in bone window show supero-inferior extent of the lesion (the mass seen extending from roof of the nasal cavity to the maxilla). The mass is remodeling the alveolar process of left maxilla (3a, 3b, small black arrows) with erosion of medial maxillary sinus wall (3b, 3c, long black arrows), medial wall and floor of left orbit (3b, short white arrow) with intraorbital extension (3a, 3b, long white arrows). The medial wall of right maxillary sinus is also deviated. No erosion of crista galli or floor of anterior cranial fossa noted.
Figure 4.
25-year-old male with cemento-ossifying fibroma of paranasal sinus presenting acutely as orbital cellulitis. Axial post contrast CT paranasal sinus reveals multiple pockets of nonenhancing areas of hypodensity with likely fluid-fluid levels (4a, black arrow). Axial T2 weighted image at the same level confirms multiple fluid-fluid levels (4b, black arrow). Few of these areas are showing T1 hyperintense signal also representing thick secretions or blood-blood levels (4c, white arrow). Post contrast axial T1 fat suppressed image shows irregular rim and solid areas of enhancement (4d, white arrow) with associated premaxillary soft tissue thickening and collection (4d, short black arrow).
Patient was admitted and followed by ophthalmology and ENT departments. He was put on intravenous morepenem and MRI was performed.
Noncontrast and contrast enhanced MRI confirmed the presence of multiple small pockets of fluid collections with fluid-fluid levels (Fig. 4b). Some of these pockets revealed bright signal on T1W images also suggestive of blood-blood levels or complex secretions (Fig. 4c). Post contrast images revealed multiple irregular pockets of rim and solid enhancing areas within the mass ( Fig. 4d).
Radiological possibility of Ossifying fibroma was made. In view of areas of multiple fluid-fluid or blood levels, a rare diagnosis of associated aneurysmal bone cyst was also considered
Patient subsequently underwent endoscopic examination under general anesthesia followed by resection of the mass.
The endoscopic examination revealed a large expansile sinonasal mass pushing the nasal septum to the right side and medial wall of left maxillary sinus towards left. Posteriorly, the mass was encroaching upon the nasopharynx and superiorly up to lamina papyracea. The mass was hard on probing with the endoscope.
Macroscopic examination of the specimen consisted of multiple grey brown fragments of tissue measuring 8.0 × 7.0 × 2.5 cm in aggregate. Cartilaginous and bony tissue fragments were seen. Cut section showed focal cystic areas filled with thick mucoid material.
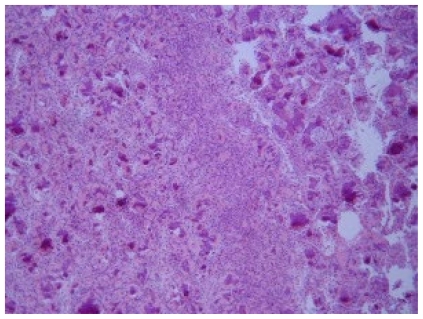
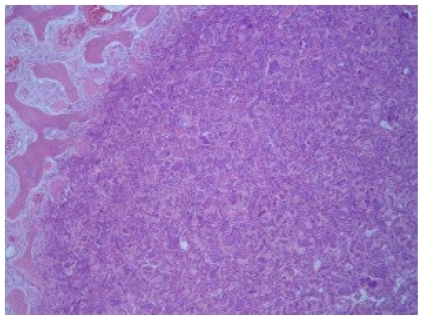
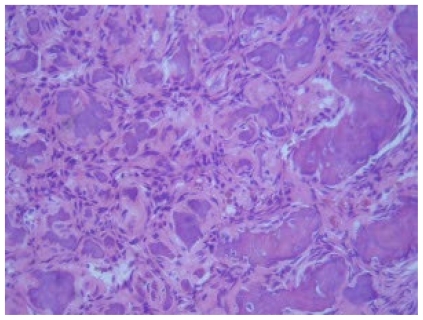
Microscopic examination of the specimen mid power view (magnification X10) showed fibrous stroma with bone trabeculae and associated variable mineralized material that resembled dental cementum. These features were consistent with fibro-osseous nature of the lesion (Fig. 5). Low power view (magnification X4) showed well circumscribed margins of the lesion (Fig. 6). High power view (magnification X40) showed hypercellularity (Fig. 7).
Figure 5.
25-year-old male with cemento-ossifying fibroma of paranasal sinus. Histologic examination reveals fibrous stroma with bone trabeculae and associated variable mineralized material that resembled dental cementum consistent with fibro- osseous nature of the lesion. (H & E stain, magnification X10).
Figure 6.
25-year-old male with cemento-ossifying fibroma of paranasal sinus. Low power view (H & E stain, magnification X4) showing well circumscribed margins of the lesion.
Figure 7.
25-year-old male with cemento-ossifying fibroma of paranasal sinus. High power view (H & E stain, magnification X40) showed hypercellularity.
Final diagnosis of fibro-osseous lesion consistent with cemento-ossifying fibroma was made.
DISCUSSION
Fibro-osseous lesions of face and paranasal sinuses are relatively uncommon. The benign fibro-osseous lesions described are ossifying fibroma (and its histologic variants) and fibrous dysplasia. Craniofacial benign fibro-osseous lesions may not be distinguished from histopathological findings alone and need radiographic correlation for differentiation (1).
Ossifying fibroma is most commonly seen in 3rd and 4th decades with marked female preponderance (M: F = 1:2) (2). It has been suggested that ossifying fibroma arises from the mesenchyma of the periodontal membrane (a layer of fibrous connective tissue surrounding the roots of teeth) and is related to the cementifying fibroma and cemento-ossifying fibroma (3).
Variants of ossifying fibroma differ in the nature of calcification (cementum or bone), according to the location (oral, paranasal or orbital), morphological differences (presence or absence of psammomatoid component) and in behavior (aggressive or static) (1). When the lesion contains cementum it is known as cementifying fibroma while presence of bone within the lesion makes it ossifying fibroma. Lesions with a mixture of both cementum and bone matrix are known as cemento-ossifying fibroma. The location of these lesions in areas not associated with periodontal ligament (like paranasal sinus and orbit), has been hypothesized to be due to displaced periodontal ligamentous tissues during embryogenesis or from cells capable of differentiating into cementum, bone and fibrous tissue (4).
Cemento-ossifying fibromas commonly involve the mandible and are unusual in the maxilla (5). The lesion is generally asymptomatic. Persistent growth of the lesion can cause noticeable swelling and facial asymmetry. Displacement of teeth may be an early feature. Orbital and para-orbital involvement is usually asymptomatic and it is usually an incidental finding on radiographic examinations.
In the early stages, cemento-ossifying fibroma appears as radiolucent lesion with no internal radiopacities. With maturity of the lesion there is increasing calcific flecks progressing ultimately to an extremely radiopaque mass. The growth pattern of the mass is centrifugal so grows equally in all directions presenting therefore as a well circumscribed mass (6).
70 % of cemento-ossifying fibromas involve the mandible; about 22 % can be found involving the molar region of maxilla, ethmoidal and orbital regions and is seen exceptionally in petrous bone (4, 7, 8).
Three radiographic patterns have been described depending on radiographic borders: (1) defined lesion without sclerotic border (40%), (2) defined lesion with sclerotic border (45%) and (3) lesion with ill-defined border (15%) (9).
CT shows a well demarcated soft tissue mass with areas of relatively high density or areas of low and fluid densities, with scattered calcifications. Sinus wall may be destroyed or fragmented while orbital floor is displaced. Medial orbital wall and frontal skull base maybe eroded (7, 10, 11).
On MRI the lesion shows isointense signal in T1 weighted and has diffuse homogenous low signal on T2 weighted likely due to calcific and fibrous content of the tumour (12).
Our index case was unusual in many ways. First of all the history of our patient was very short and clinical presentation was simulating orbital cellulitis with exophthalmos. Such a clinical presentation has been reported in a small series of sinonasal osseous-fibroma in two children (13).
Secondly, the epicentre of the mass was located in the left ethmoid sinus, left nasal cavity with extension into left maxillary sinus eroding its walls. There are only few isolated case reports of ethmoidal cemento-ossifying fibroma presenting as exophthalmos (14,15). No reports of acute presentation of ethmoidal cemento-ossifying fibroma with exophthalmos and orbital cellulitis have been reported in adult patients to our knowledge.
Thirdly our case showed multiple fluid-fluid levels in MRI with intense peripheral and solid areas of enhancement, which could have been due to associated cysts, mucoceles or due to associated aneurysmal bone cyst. Similar MRI appearance has been reported in only a few case reports (16, 17).
Differential diagnosis of sinonasal fibro-osseous masses can be other lesions which have calcific or bone densities within a mass like:
Osteogenic sarcoma or chondrosarcoma.
Squamous cell carcinomas.
Well defined border of cemento-ossifying fibroma differentiates it from aggressive sarcomas or carcinomas (12).
3. Odontogenic cysts
4. Calcifying odontogenic cysts (Gorlin cyst).
5. Calcifying epithelial odontogenic tumour (Pindborg tumour).
Gorlin cysts or Pindborg tumor are not a differential in our case due to its non-odontogenic origin.
6. Fibrous dysplasia (FD) is the closest differential diagnosis of OF as OF can have pathologic areas resembling FD. Differentiating features can be unilocular appearance of osseous-fibroma with distinct boundaries having egg shell character (as seen in our index case), whereas borders of FD are diffuse and merge with normal bone (18, 19). On MRI FD is low signal in T2 weighted whereas it can have variable signal in OF (as in our case). Also, contrast enhancement in FD is seen only in expanded diffuse diploe of the involved bone unlike OF in which outer shell or septae enhance (20).
7. Aneurysmal bone cyst, though a rare location, classically shows multiple blood-blood levels. It can still be a differential in the index case due to the presence of multiple fluid-fluid levels showing heterogenous signal on MRI.
TEACHING POINT
Rarely sinonasal masses can present with acute orbital cellulitis. In a young patient with a well-defined sinonasal mass showing distinct boundaries and areas of speckled calcification, ossifying-fibroma should be considered.
ABBREVIATIONS
- WBC
White blood cell
- CT
Computed Tomography
- MRI
Magnetic resonance imaging
- N
Normal
- ESR
Erythrocyte sedimentation rate
- FD
Fibrous dysplasia
- OF
Ossifying fibroma
- H & E
Hematoxylin and eosin
- ENT
Ear-Nose-Throat
- HU
Hounsfield units
REFERENCES
- 1.Wenig Bruce M, Mafee Mahmood F, Ghosh Luna. Fibro-osseous, osseous, and cartilaginous lesions of the orbit and paraorbital region. Correlative clinicopathologic and radiographic features, including the diagnostic role of CT and MR imaging. RCNA. 1998;36(6):1241–59. doi: 10.1016/s0033-8389(05)70243-8. [DOI] [PubMed] [Google Scholar]
- 2.Waldron CA, Giansati JS. Benign fibro-osseous lesions of the jaws: A clinico-pathologic-histologic review of sixty-five cases. II. Benign fibro-osseous lesions of peridontal ligament origin. Oral Surg. 1973;35:340. doi: 10.1016/0030-4220(73)90072-8. [DOI] [PubMed] [Google Scholar]
- 3.Huebner GR, Brenneise CV, Ballenger J. Central ossifying fibroma of anterior maxilla: Report of case. J Am Dent Assoc. 1998;116:507–10. doi: 10.14219/jada.archive.1988.0304. [DOI] [PubMed] [Google Scholar]
- 4.Fanibunda K, Reed MF. Cemento-ossifying fibroma of the mandible. Dentomaxillofacial Radiol. 1997;26:246–48. doi: 10.1038/sj.dmfr.4600245. [DOI] [PubMed] [Google Scholar]
- 5.Hamner JE, Scofield HH, Cornyn J. Benign fibro-osseous jaw lesions of peridontal membrane origin: An analysis of 249 cases. Cancer. 1968;22:861–78. doi: 10.1002/1097-0142(196810)22:4<861::aid-cncr2820220425>3.0.co;2-c. [DOI] [PubMed] [Google Scholar]
- 6.Montgomery AH. Ossifying fibroma of the jaw. Arch Surg. 1938;36:874–98. [Google Scholar]
- 7.Su L, Weathers DR, Waldrom CA. Distinguishing features of focal cemento-ossifying dyplasia and cemento-ossifying fibromas (II). A clinical and radiologic spectrum of 316 cases. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1997;84:540–49. doi: 10.1016/s1079-2104(97)90271-7. [DOI] [PubMed] [Google Scholar]
- 8.Brademann G, Werner JA, Jänig U, Mehdorn HM, Rudert H. Cemento-ossifying fibroma of the petromastoid region: case report and review of the literature. J Laryngol Otol. 1997;111:152–55. doi: 10.1017/s0022215100136709. [DOI] [PubMed] [Google Scholar]
- 9.Barberi A, Cappabianca S, Colella G. Bilateral cemento-ossifying fibroma of the maxillary sinus. BJR. 2003;76:279–80. doi: 10.1259/bjr.76.904.760279. [DOI] [PubMed] [Google Scholar]
- 10.Bendet E, Bakon M, Talmi YP, Tadmor R, Kronenberg J. Juvenile cemento ossifying fibroma of the maxilla. Ann Otol Rhinol Laryngol. 1997;106:75–8. doi: 10.1177/000348949710600113. [DOI] [PubMed] [Google Scholar]
- 11.Engelbrecht V, Preis S, Hassler W, Lenard HG. CT and MRI of congenital sinonasal ossifying fibroma. Neuroradiology. 1999;41:526–29. doi: 10.1007/s002340050798. [DOI] [PubMed] [Google Scholar]
- 12.Kuta John, Worley C MacDonald, Kaugars George E. Central Cementoossifying Fibroma of the Maxillary Sinus: A Review of Six Cases. AJNR. 1995;16:1282–86. [PMC free article] [PubMed] [Google Scholar]
- 13.Cruz AA, Alencar VM, Figueiredo AR, de Paula S, Eichenberger GC, Chahud F, Pedrosa MS. Ossifying fibroma: a rare cause of orbital inflammation. Ophthal Plast Reconstr Surg. 2008 Mar-Apr;24(2):107–12. doi: 10.1097/IOP.0b013e3181647cce. [DOI] [PubMed] [Google Scholar]
- 14.Apaydin M, Calli C, Yardim BG, Sarsilmaz A, Varer M, Uluç E. Kulak Burun Bogaz Ihtis Derg. 2008 May-Jun;18(3):185–87. [PubMed] [Google Scholar]
- 15.Yazgan C, Fitoz S, Atasoy P, Akyar S. Case report: Cemento-ossifying fibroma of the ethmoidal sinus presenting with exophthalmos.(Article in Turkish) Tani Girisim Radyol. 2003;9:192–94. [PubMed] [Google Scholar]
- 16.Kendi AT, Kara S, Altinok D, Keskil S. Sinonasal ossifying fibroma with fluid-fluid levels on MR images. AJNR Am J Neuroradiol. 2003;24:1639–41. [PMC free article] [PubMed] [Google Scholar]
- 17.Vaidya AM, Chow JM, Goldberg K, Stankiewicz JA. Juvenile aggressive ossifying fibroma presenting as an ethmoid mucocele. Otolaryngol Head Neck Surg. 1998;119:665–68. doi: 10.1016/S0194-5998(98)70031-2. [DOI] [PubMed] [Google Scholar]
- 18.Morris MR, Blakeslee DB, Zajtchuk JT. Aggressive paranasal sinus ossifying fibroma. Ear Nose Throat J. 1989;68:260–64. [PubMed] [Google Scholar]
- 19.Çakir B, Karaday N. Ossifying fibroma in the nasopharynx. Clin Imaging. 1991;15:290–92. doi: 10.1016/0899-7071(91)90122-c. [DOI] [PubMed] [Google Scholar]
- 20.Engelbrecht V, Preis S, Hassler W, Lenard HG. CT and MRI of congenital sinonasal ossifying fibroma. Neuroradiology. 1999:526–29. doi: 10.1007/s002340050798. [DOI] [PubMed] [Google Scholar]