Abstract
A hydrocele is a collection of fluid in the space surrounding the testicle between the layers of the tunica vaginalis. Occasionally the scrotal hydrocele may extend through the inguinal canal, deep inguinal ring, and into the abdomen as an abdominoscrotal hydrocele. Traditionally, abdominoscrotal hydrocele have been evaluated and diagnosed with US. However if a relationship between the abdominal mass and the hydrocele is not clearly defined by sonography, the traditional modality for imaging the abdomen and the scrotum such as CT or MRI, should be considered because it can be difficult to clearly delineate the anatomy and the full extent of the abnormality. We present a rare case of a giant hemorrhagic abdominoscrotal hydrocele in a 24 year old man that required an elective operative laparotomy for complete excision of the abdominolscrotal mass.
Keywords: Abdominolscrotal mass, haemorragic hydrocele, scrotal MRI
CASE REPORT
A 24 year old male was referred to our Institution with a history of an asymptomatic palpable mass in the left testis growing into the inguinal region since early childhood. A testicular ultrasound performed in another hospital demonstrated a hetererogeneus component in the left testis, a suspected tumour. Physical examination of the patient revealed a left non tender scrotal mass, the upper limits of which could not be palpated, along the homolateral inguinoscrotal region. Testicular tumour markers were unremarkable (Beta HCG, AFP, LDH). To better characterize the lesion, MRI was performed using axial T2-weighted axial T1-weighted and sagittal images before and after gadolinium enhancement. It showed an hourglass shaped heterogeneous mixed intensity mass in the left scrotum, extending towards the abdomen through the homolateral inguinal canal, measuring 23 cm in length, 9 cm in width and 6 cm in height with the presence of a normal left testis, smaller (9 cm3, normal range in adult 15–20 cm3) in size that was surrounded by the mass (Fig. 1,2). The right testis was normal except for the presence of a simple hydrocele in the ipsialateral scrotal bursa (Fig. 3). The left iliac vessels and the lateral wall of the bladder were partly compressed but not infiltrated by the mass (Fig. 4). These findings were compatible with abdominal-scrotal hematoma. T1-weighted MRI with gadolinium showed no tumour-like enhancement (5–6).
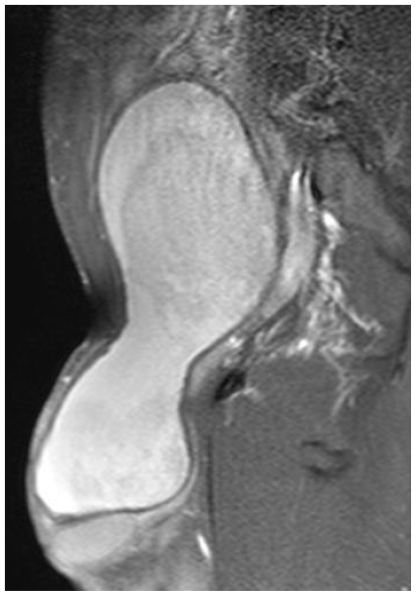
Figure 1.
24 Year old male with large hemorrhagic abdominolscrotal hydrocele: TSE T2-weighted sagittal plane. The caudal-cranial mass (about 23 cm) extends in the abdomen through the right inguinal canal to the top of L5. Since the mass can not expand in the right inguinal ring, on this view the lesion appears "hourglass" shaped. Posteriorly to the mass it is possible to recognize the bladder (i.e.: hyperintense structure). Just below the mass on the right side, there is a hydrocele with fluid signal intensity.
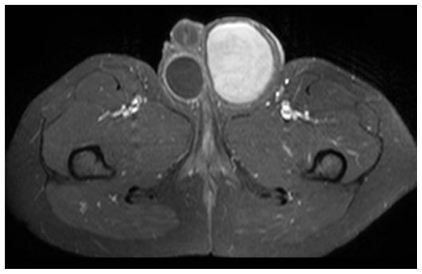
Figure 2.
24 Year old male with large hemorrhagic abdominolscrotal hydrocele: TSE T1-weighted axial plane. The left scrotal wall appears thickened, particularly on the left side and on the back. The content is heterogeneously hyperintense, possibly due to blood.
Figure 3.
24 Year old male with large hemorrhagic abdominolscrotal hydrocele: Gadolinium-enhanced T1-weighted axial image with fat suppression. Compared to the baseline, there is no Gadolinium enhancement apart from the right bursale-scrotal wall. On the ipsilateral side there is no enhancement of the bursal content. There is some Gad-enhancement at the level of the contralateral bursal wall (hyperintense for the blood). The absence of hyperaemia in the right scrotal bursa suggests a simple hydrocele. Also there is a shift towards right of the corpora cavernosa.
Figure 4.
24 Year old male with large hemorrhagic abdominolscrotal hydrocele: TSE T2-weighted axial plane. There is slight compression of the left iliac vessels and the bladder without evidence of infiltration.
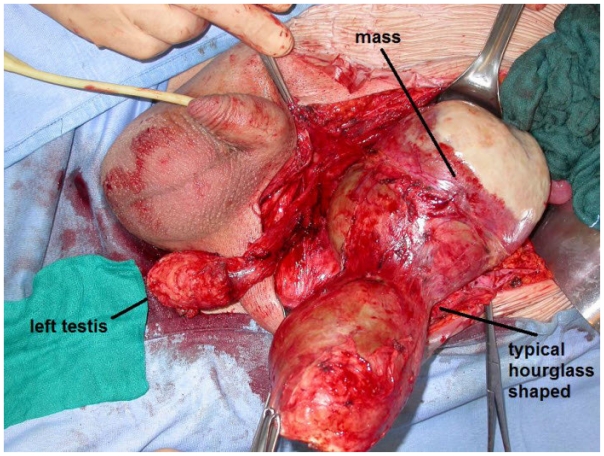
After the diagnostic MRI, the patient was scheduled for elective operative laparotomy with a left para rectal line incision extended to the pubic bone. On entering the abdomen, an intraperitoneal mass extending through the left internal inguinal ring into the left scrotum was encountered. The surrounding peritoneal layer was dissected from the solid mass and complete excision of the abdominal sac with its closure distally to the left internal inguinal ring was performed (Fig. 7). The postoperative course was uneventful. Pathologic examination of the specimens showed no malignancy.
Figure 7.
24 Year old male with large hemorrhagic abdominolscrotal hydrocele. Surgical procedure: left pararectal line incision extended to the pubic bone. On entering the abdomen, an intraperitoneal mass extending through the left internal inguinal ring into the left scrotum was encountered. Complete excision of the left abdominolscrotal sac with particular attention to the vessels of the left testis was performed. The final diagnosis (proved with histological examination) was hemorrhagic hydrocele.
DISCUSSION
Embryologically, a part of peritoneum called “processus vaginalis” precedes the testis through the deep inguinal ring. This communication between the peritoneum and the scrotum should obliterate after birth, but occasionally remains patent. A hydrocele is a collection of fluid in the space surrounding the testicle between the layers of the tunica vaginalis. Occasionally the scrotal hydrocele may extend through the inguinal canal, deep inguinal ring, and into the abdomen as an abdominoscrotal hydrocele. ASH is a rare form of hydrocele originally described by Dupuytren in 1834 (1). Several papers have been written about the pathogenesis, complications and surgical approach to repair this condition but we can find three theories of pathogenesis. The first theory showed by Dupuytren (1) says that an excessive distention of the tunica vaginalis displaces the hydrocele superiorly through the inguinal canal into the abdomen to form the abdominal component. A second theory proposes that the scrotal hydrocele extends into the abdomen through a valve-like action of the processus vaginalis when intrascrotal pressure becomes high (2–5). The third theory postulates the presence of a preformed congenital peritoneal diverticulum with an underlying anatomic abnormality of the pre-existing abdominal sac (6–8).
Traditionally, abdominoscrotal hydroceles have been evaluated and diagnosed with US. However, if a relationship between the abdominal mass and the hydrocele is not clearly defined by sonography, the traditional modality for imaging the abdomen and the scrotum such as CT or MRI, should be considered because it can be difficult to clearly delineate the anatomy and the full extent of the abnormality.
Also there were not clear causes of bleeding (example: trauma) in the patient history to correlate the mass with a giant hemorrhagic hydrocele. In our case MRI was helpful, particularly by demonstrating the typical hourglass shape and the intensity, thus excluding other possible diagnoses such as testicular tumor, vas deferens cyst, multicystic hydrocele or lymphangioma. It is also useful in demonstrating the mass effect on neighboring vessels, urinary tract and the homolateral testis. To date, the only reported management is by surgical excision. Spontaneous resolution has not been documented in the literature. However surgery is not easy when the anatomy is distorted and as it is an uncommon condition, fewer than 200 cases have been reported, the majority of which are in adults. Surgeons may not be able to build up a large experience. Traditional risks of damage to the spermatic cord and vessels are increased because of the nature of the surgery and the condition. The spermatic cord transection and intestinal obstruction have been mentioned as complications. The operative approach to resection of an abdominoscrotal hydrocele depends on the size of the abdominal component of the sac and include: inguinal (9–10), peritoneal (11) or even scrotal (12) approaches.
TEACHING POINT
The extension of a giant abdominoscrotal mass may be difficult to evaluate by Ultrasound alone, and sagittal MRI is helpful in demonstrating the extension of such a mass through the inguinal canal into the abdominal cavity and its contents. MRI images are particularly useful to plan the correct surgical approach and to reduce the need of radical orchifuniculectomy for tumor (especially in young men).
Figure 5.
24 Year old male with large hemorrhagic abdominolscrotal hydrocele: TSE T1-weighted axial plane at S2–S3 level. The lesion is hyperintense with isointense central spots. The hterogeneous signal of the lesion can be related to the presence of haemoglobin degradation products.
Figure 6.
24 Year old male with large hemorrhagic abdominolscrotal hydrocele: Gadolinium-enhanced T1-weighted with fat suppression sagittal image. Left medial view. There is no clear Gad-enhancement of the mass content. Posteriorly to the mass there is a moderate ectasia of the external left iliac vein.
ABBREVIATIONS
- ASH
Abdominoscrotal hydrocele
- MRI
Magnetic resonance imaging
- Beta HCG
Beta-human chorionic gonadotrophin
- AFP
Alfa alpha-fetoprotein
- LDH
Lactate dehydrogenase
REFERENCES
- 1.Dupuytren G. Lecons orales de clinique chirugicale. Balliere. 1834:444. [Google Scholar]
- 2.Saharia PC, Brunsther B, Abrams MW. Abdominoscrotal hydrocele. Case presentation and review of the literature. J Pediatr Surg. 1979;14:713–714. doi: 10.1016/s0022-3468(79)80251-1. [DOI] [PubMed] [Google Scholar]
- 3.Casolari E, Cacciari A, Federici S. Abdominoscrotal hydrocele in childhood. Case report and review of the literature. Z Kinderchir. 1983;38:353–355. doi: 10.1055/s-2008-1060005. [DOI] [PubMed] [Google Scholar]
- 4.Wlochynski T, Wassermann J, Generowicz Z. Abdominoscrotal hydrocele in childhood. J Pediatr Surg. 1993;28:248–250. doi: 10.1016/s0022-3468(05)80286-6. [DOI] [PubMed] [Google Scholar]
- 5.Luks FI, Yazbeck S, Honsy Y, et al. The abdominoscrotal hydrocele. Eur J Pediatr Surg. 1993;13:176–178. doi: 10.1055/s-2008-1063538. [DOI] [PubMed] [Google Scholar]
- 6.Cerrah CA, Akyuz H, Ciftlik A, Gürbüz A, Danismend N. Critical observation about the pathogenesis of abdominoscrotal hydrocele. J Pediatr Surg. 2001;36:1082–10848. doi: 10.1053/jpsu.2001.24760. [DOI] [PubMed] [Google Scholar]
- 7.Ferro F, Spagnoli A, Lucchetti MC, Marchetti P. Abdominoscrotal hydrocele: a reliable surgical technique. Urology. 2000;55:771–7739. doi: 10.1016/s0090-4295(00)00478-7. [DOI] [PubMed] [Google Scholar]
- 8.Serels S, Kogan S. Bilateral giant abdominoscrotal hydroceles in childhood. Urology. 1996;47:763–765. doi: 10.1016/s0090-4295(96)00022-2. [DOI] [PubMed] [Google Scholar]
- 9.Nagar H, Kessler A. Abdominoscrotal hydrocele in infancy: a study of 15 cases. Pediatr Surg Int. 1998;13:189–90. doi: 10.1007/s003830050286. [DOI] [PubMed] [Google Scholar]
- 10.Chamberlain SA, Kirsch AJ, Thall EH, Emanuel ER, Hensle TW. Testicular dysmorphism associated with abdominoscrotal hydroceles during infancy. Urology. 1995;46:881–2. doi: 10.1016/s0090-4295(99)80365-3. [DOI] [PubMed] [Google Scholar]
- 11.Luks FI, Yazbeck S, Collin PP. The abdominoscrotal hydrocele. Eur J Pediatr Surg. 1993;3:176–8. doi: 10.1055/s-2008-1063538. [DOI] [PubMed] [Google Scholar]
- 12.Belman AB. Abdominoscrotal hydrocele in infancy: a review and presentation of the scrotal approach for correction. J Urol. 2001;165:225–7. doi: 10.1097/00005392-200101000-00065. [DOI] [PubMed] [Google Scholar]