Abstract
We report a case of a 50-year-old male who presented to the Emergency Department and was diagnosed with epididymo-orchitis. Sonographic evaluation of the testicle initially showed a normal, low resistance color Doppler waveform. The patient was admitted to the hospital. A follow up sonogram two days later demonstrated reversal of diastolic arterial flow on Pulse-Wave color Doppler imaging. Reversal of diastolic blood flow in testicular color Doppler sonography is a sign of impending infarction. On hospital day 6, the patient had a follow up ultrasound which demonstrated infarction of the testicle. Pathology confirmed the diagnosis and the tissue culture grew E. coli and Candida Albicans. This case documents the rapid progression of epididymo-orchitis with a normal spectral waveform to testicular infarction with reversal of diastolic blood flow on color Doppler imaging as a sign of impending infarction.
Keywords: Testicular infarction, epididymo-orchitis, reversal of diastolic flow
CASE REPORT
A 50-year-old male with no significant past medical history presented to the Emergency Department with right testicular pain. Ultrasound was obtained to rule out testicular torsion. It showed an enlarged and hyperemic right testicle and epididymis with normal arterial and venous waveforms (Figures 1–5). The patient had a white blood cell count (WBC) of 26,000 and a grossly positive urinalysis which grew out E. coli on culture. The patient was admitted with a diagnosis of right sided epididymo-orchitis and was treated with IV antibiotics. Over the next two days, the patient’s condition worsened with continued pain and no significant decrease in his WBC, so a second ultrasound was ordered on hospital day 2 to rule out an abscess. The second ultrasound again demonstrated an enlarged and hyperemic right epididymis with development of a complex right hydrocele likely representing a pyocele (Figure 6). However, the arterial blood flow at this time demonstrated a high resistive index pattern on Pulse-Wave color Doppler imaging with reversal of diastolic blood flow (Figures 7). These findings were discussed with the Urologist, as reversal of diastolic blood flow can be a sign of impending infarction. Over the course of the next few days, the patient’s condition worsened. He became septic and developed multi-system failure. On hospital day 6, the patient, who was experiencing continued testicular pain, underwent a third ultrasound evaluation. It demonstrated no arterial flow in the right testicle, consistent with testicular infarction (Figures 8–10). The patient eventually underwent a right orchiectomy. Pathology confirmed the diagnosis of acute and chronic epididymo-orchitis with hemorrhage and necrosis (Figures 11–13). On pathology review, fungal elements were noted in the testicle and tunica vaginalis that was identified as Candida Albicans on culture. After surgery, the patient’s status improved and he was eventually discharged on antibiotics and antifungals.
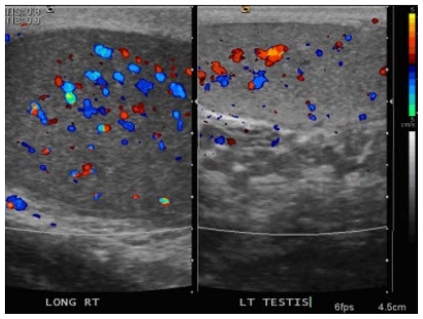
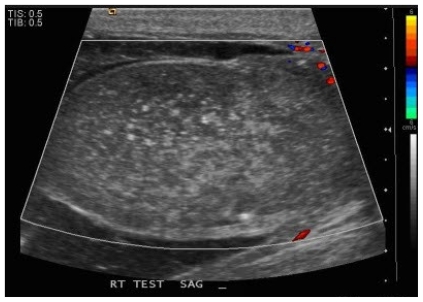
Figure 1.
50-year-old male with right sided epididymo-orchitis. Side by side longitudinal ultrasound image on day of admission demonstrates an enlarged right testicle (measuring 5.0 cm × 3.1 cm × 2.8 cm) that is slightly hypoechoic when compared to the left testicle (measuring 4.0 cm × 2.5 cm × 2.0 cm). The right testicle also demonstrates subtle hyperemia compared to the left. These findings are consistent with right sided orchitis.
Figure 5.
50-year-old male with right sided epididymo-orchitis. Side by side color Doppler image of the right and left epididymis on day of admission demonstrates an enlarged and hypervascular right epididymis (measuring 1.4 cm × 1.6 cm) compared to the left (measuring 1.1 cm × 0.7 cm) consistent with right sided epididymitis.
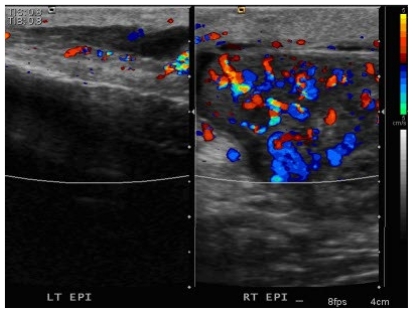
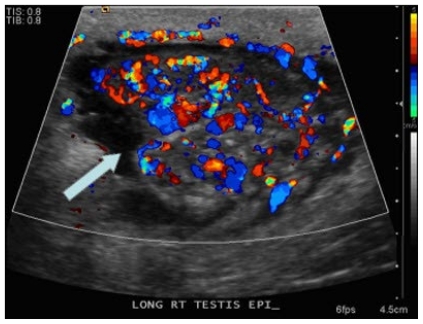
Figure 6.
50-year-old with right sided epididymo-orchitis. Color Doppler sonogram of the right testicle and epididymis 2 days after admission demonstrates an enlarged (measuring 1.6 cm × 1.0 cm), hyperemic right epididymis (arrow) consistent with epididymitis. There has been development of a complex right hydrocele (arrowhead) without internal blood flow representing a pyocele.
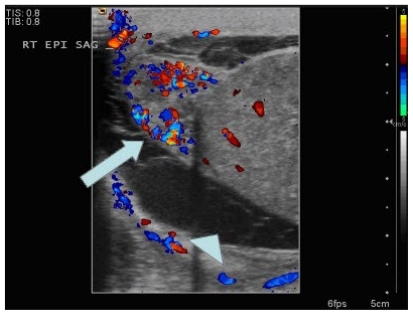
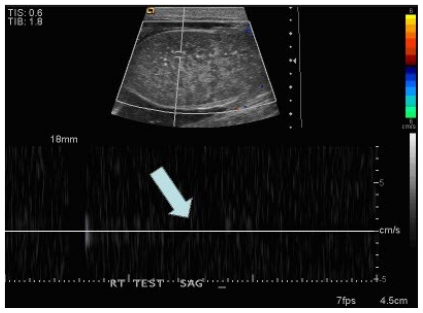
Figure 7.
50-year-old with right sided epididymo-orchitis. Spectral waveform on color Doppler imaging 2 days after admission demonstrates reversal of diastolic blood flow. The peak systolic flow is elevated (arrow), and the peak diastolic flow is reversed (arrowhead). Incidentally noted is aliasing artifact (curved arrow). In the setting of infection, this type of waveform is concerning for impending infarction. Also demonstrated is the previously described complex right hydrocele, representing a pyocele.
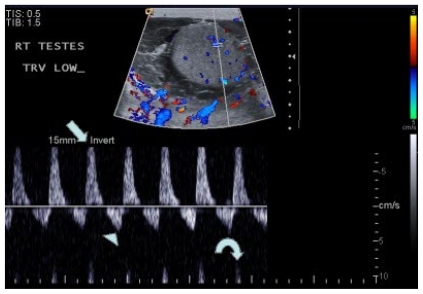
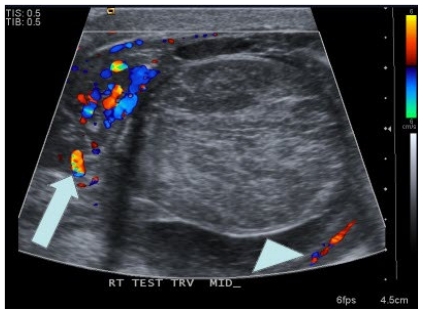
Figure 8.
50-year-old male with right sided epididymo-orchitis. Color Doppler sonogram of the right testicle 6 days after admission demonstrates no appreciable color flow within the right testicle which appears more heterogeneous in echotexture. These findings are consistent with testicular infarction.
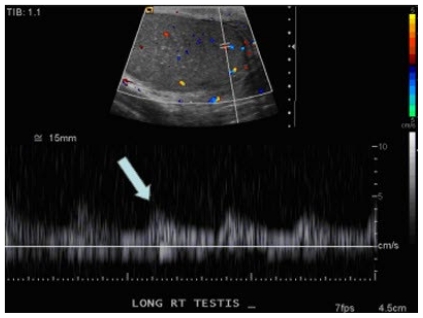
Figure 10.
50-year-old male with right sided epididymo-orchitis. Spectral waveform image on color Doppler imaging 6 days after admission demonstrates no appreciable spectral waveform (arrow) in the right testicle confirming testicular infarction.
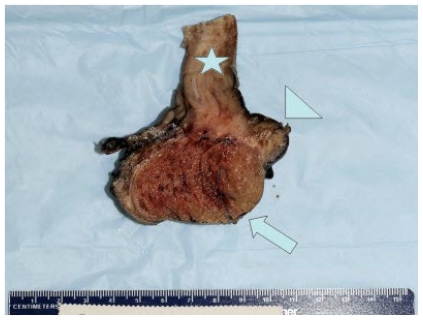
Figure 11.
50-year-old male with right sided epididymo-orchitis that lead to testicular infarction. Gross surgical specimen demonstrates a gray-brown appearance to the right testicle (arrow), epididymis (arrowhead), and spermatic cord (star). These findings are consistent with acute and chronic epididymo-orchitis with hemorrhage and necrosis.
Figure 13.
50-year-old male with right sided epididymo-orchitis that lead to testicular infarction. Gross bivalved surgical specimen demonstrates a tan-red appearance to the right testicle (arrow) consistent with hemorrhage with a thin rim of normal apparent normal testicular parenchyma remaining. The epididymis (arrowhead) has surface hemorrhage and fibrosis throughout. The spermatic cord (star) is tan-white consistent with fibrosis with streak hemorrhages running throughout. These findings are consistent with acute and chronic epididymo-orchitis with hemorrhage and necrosis.
DISCUSSION
Epididymo-orchitis is an infectious/inflammatory process that occurs in approximately 1/1000 men per year (1). However, testicular infarction secondary to epididymo-orchitis is relatively rare and its true incidence is unknown. In cases of testicular infarction, greatly diminished and/or lack of blood flow is diagnostic. As seen in this case, reversal of diastolic flow in the affected testicle is an ominous sign of impending infarction and the ordering physician should be notified as this may prompt a change in the patient’s treatment plan and/or surgical exploration.
On scrotal sonography, spectral color Doppler imaging in a normal testicle will demonstrate a low resistive index pattern (Figure 4). Resistive index is defined as (S-D)/S where S is the height of the systolic peak and D is the height of the end diastolic peak (2). Normal resistive indices for a testicle are 0.48–0.75 with a mean of 0.62 (3). Reversal of diastolic flow in a testicle is a high resistive index pattern and indicates antegrade flow into the testicle during systole and retrograde flow during diastole, which causes resultant loss of tissue perfusion (4).
Figure 4.
50-year-old male with right sided epididymo-orchitis. Spectral waveform on color Doppler imaging on day of admission (arrow) demonstrates a normal, low resistance arterial waveform in the right testicle.
Testicular infarction in the setting of epididymo-orchitis has been postulated to be caused by epididymal or spermatic cord inflammation and edema causing compression of the testicular vein, testicular artery, and/or lymphatics. Also, endothelial damage secondary to bacterial toxins causing a vascular thrombus have also been postulated to cause infarction (1). Hydroceles have also been shown to cause high resistive index spectral flow patterns on color Doppler sonography (3). Thus, a complex hydrocele as seen in this case, in the setting of epididymo-orchitis, may contribute to the development of testicular infarction.
Reversal of diastolic flow on spectral waveform color Doppler imaging is also associated with other complications involving many other organ systems. In renal transplant patients, it is associated with hematoma, acute tubular necrosis, renal vein thrombosis, vascular kink, rejection, glomerulosclerosis, low cardiac output, and diabetic nephrosclerosis. The cause in renal transplant patients depends on the amount of time the patient is post operation. The sign in this patient population is non-specific (5). It is also associated with high grade carotid artery stenosis, intracranial vasospasm secondary to subarachnoid hemorrhage, and arterial vasospasm in liver transplant patients (6). In neonates with congenital heart disease, reversal of diastolic flow in abdominal aorta ultrasound is associated with an increased risk of necrotizing enterocolitis (7).
The most common organisms that cause epididymitis include Chlamydia and gonorrhea in patients less than 35 years of age and E. coli, enterococci, Pseudomonas, and Proteus in older men (1). However, cases that lead to infarction are usually associated with non-gonococcal organisms (8). The patient in this case grew out two organisms; E. coli and Candida Albicans, which was not deemed to be a contaminant. Epididymo-orchitis caused by Candida is extremely rare with only a few case reports existing in the literature (9). It was not known if the patient in this case presented initially with epididymo-orchitis caused by Candida Albicans and E. coli, or if the Candida infection developed secondary to the broad spectrum antibiotics he was initially given as treatment.
Obtaining spectral waveforms on color Doppler sonography of the scrotum should not be limited to examinations for torsion and epididymo-orchitis. For instance, obtaining spectral waveforms can help differentiate acute segmental testicular infarction from tumor as both can look similarly hypoechoic on gray scale imaging. However, tumor tends to be hypervascular and impending acute segmental testicular infarction can have a high resistant waveform if the testicle does not already demonstrate a lack of blood flow consistent with infarction (10).
There have been two previous case reports in the literature with true diastolic blood flow reversal in cases of testicular infarction caused by epdidymo-orchits (4; 6). This case documents and demonstrates how quickly a case of epdidymo-orchits with normal spectral waveforms can progress to reversal of diastolic blood flow and to infarction. The initial ultrasound evaluations in both prior case reports showed reversal of diastolic flow and only one study showed natural progression to infarction 3 weeks later.
TEACHING POINT
This case stresses the importance of using color Doppler imaging and obtaining spectral waveforms when performing ultrasound examinations of the scrotum for epididymo-orchitis. When reversal of diastolic flow is identified, it is important to promptly alert the ordering physician of the sign concerning for impending testicular infarction as it may acutely alter their treatment plan.
Figure 2.
50-year-old male with right sided epididymo-orchitis. Sonogram of the right epididymis on day of admission (arrow) demonstrates an enlarged right epididymis (measuring 1.4 cm × 1.6 cm).
Figure 3.
50-year-old male with right sided epididymo-orchitis. Color Doppler sonogram of the right epididymis on day of admission (arrow) demonstrates increased vascularity throughout the epididymis consistent with epididymitis.
Figure 9.
50-year-old male with right sided epididymo-orchitis. Color Doppler image of the right epididymis (arrow) and right testicle (arrowhead) 6 days after admission demonstrate continued hyperemia of the right epididymis with no appreciable flow in the right testicle, consistent with infarction. Again noted is the complex right hydrocele, representing a pyocele.
Figure 12.
50-year-old male with right sided epididymo-orchitis that lead to testicular infarction. Gross surgical specimen demonstrates a tan-white to gray-brown appearance to the right testicle and epididymis. Noted in the distal portion of the right testicle are multiple purulent nodules measuring up to 0.3cm. These findings are consistent with acute and chronic epididymo-orchitis with hemorrhage and necrosis.
ABBREVIATIONS
- WBC
White blood cell count
- UA
Urinalysis
- IV
Intravenous
- ICU
Intensive care unit
REFERENCES
- 1.Sue SR, Pelucio M, Gibbs M. Testicular infarction in a patient with epididymitis. Acad Emerg Med. 1998 Nov;5(11):1128–30. doi: 10.1111/j.1553-2712.1998.tb02679.x. [DOI] [PubMed] [Google Scholar]
- 2.Bude RO, Rubin JM. Relationship between the resistive index and vascular compliance and resistance. Radiology. 1999 May;211(2):411–7. doi: 10.1148/radiology.211.2.r99ma48411. [DOI] [PubMed] [Google Scholar]
- 3.Mihmanli I, Kantarci F, Kulaksizoglu H, et al. Testicular size and vascular resistance before and after hydrocelectomy. AJR Am J Roentgenol. 2004 Nov;183(5):1379–85. doi: 10.2214/ajr.183.5.1831379. [DOI] [PubMed] [Google Scholar]
- 4.Sanders LM, Haber S, Dembner A, Aquino A. Significance of reversal of diastolic flow in the acute scrotum. J Ultrasound Med. 1994 Feb;13(2):137–9. doi: 10.7863/jum.1994.13.2.137. [DOI] [PubMed] [Google Scholar]
- 5.Lockhart ME, Wells CG, Morgan DE, Fineberg NS, Robbin ML. Reversed diastolic flow in the renal transplant: perioperative implications versus transplants older than 1 month. AJR Am J Roentgenol. 2008 Mar;190(3):650–5. doi: 10.2214/AJR.07.2666. [DOI] [PubMed] [Google Scholar]
- 6.Gerscovich EO, Bateni CP, Kazemaini MR, Gillen MA, Visis T. Reversal of diastolic blood flow in the testis of a patient with impending infarction due to epididymitis. J Ultrasound Med. 2008 Nov;27(11):1643–6. doi: 10.7863/jum.2008.27.11.1643. [DOI] [PubMed] [Google Scholar]
- 7.Carlo WF, Kimball TR, Michelfelder EC, Border WL. Persistent diastolic flow reversal in abdominal aortic Doppler-flow profiles is associated with an increased risk of necrotizing enterocolitis in term infants with congenital heart disease. Pediatrics. 2007 Feb;119(2):330–5. doi: 10.1542/peds.2006-2640. [DOI] [PubMed] [Google Scholar]
- 8.Bird K, Rosenfield AT. Testicular infarction secondary to acute inflammatory disease: demonstration by B-scan ultrasound. Radiology. 1984 Sep;152(3):785–8. doi: 10.1148/radiology.152.3.6463261. [DOI] [PubMed] [Google Scholar]
- 9.Jenks P, Brown J, Warnock D, Barnes N. Candida glabrata epididymo-orchitis: an unusual infection rapidly cured with surgical and antifungal treatment. J Infect. 1995 Jul;31(1):71–2. doi: 10.1016/s0163-4453(95)91612-1. [DOI] [PubMed] [Google Scholar]
- 10.Sriprasad S, Kooiman GG, Muir GH, Sidhu PS. Acute segmental testicular infarction: differentiation from tumour using high frequency colour Doppler ultrasound. Br J Radiol. 2001 Oct;74(886):965–7. doi: 10.1259/bjr.74.886.740965. [DOI] [PubMed] [Google Scholar]