Abstract
Vertebro-vertebral arteriovenous fistulae occur infrequently. We report on such a case with delayed presentation following penetrating neck injury. This was successfully treated via coil embolisation. A 40-year-old woman presented with a subjective tinnitus that was abolished by turning her head to the right. She had sustained penetrating neck trauma 6 months earlier. Doppler Ultrasound and magnetic resonance angiogram confirmed the presence of a vertebral arterio-venous fistula. Using a trans-femoral arterial approach, the left vertebral artery was embolised by deployment of multiple coils. The patient had no return of symptoms at 3 months follow up. Radiological diagnosis and endovascular management of this condition is discussed.
Keywords: Interventional radiology, vertebral arterio-venous fistula, coil embolisation, endovascular
CASE REPORT
Introduction
Traumatic injury of the vertebral artery is rare, but can result in laceration, occlusion, dissection, pseudoaneurysm formation or more rarely arteriovenous fistula formation (1). One report suggests that sixty eight per cent of vertebral arterio-venous fistulae are traumatic in aetiology, the remainder spontaneous (2).
Diagnosis relies on confirmation using catheter angiography. However, the diagnosis can be suggested through use of Doppler ultrasound and increasingly Magnetic Resonance Angiography (MRA) and Computed Tomography Angiography (CTA) are used as part of the diagnostic work-up. The relative merits of each modality are discussed.
Lesions of the vertebral artery are difficult to treat through open surgical repair owing to the vessel’s anatomical position in close association to the brachiocephalic vessels, mandible and cervical spine. This makes adequate exposure and vessel control challenging. In recent years, endovascular strategies have therefore been employed. Mechanisms include embolisation through coil deployment (3,4), detachable balloon occlusion (5,4) and covered stent grafting of the artery (4, 6, 7, 8, 9).
Management of traumatic arteriovenous fistulae of the vertebral artery and vein are occasionally described within the literature (3, 4, 5, 6, 7, 8). We describe a case of penetrating cervical trauma that resulted in the formation of a vertebro-vertebral arterio-venous fistula with distally occluded vertebral artery. This was managed endovascularly through coil embolisation of the vertebral artery.
Case Report
A 40-year-old woman began to suffer from a series of seizures. These were later attributed to epilepsy by the Neurology team. On the occasion of her first seizure, her appearance led her husband to believe that she was choking on her food and therefore suffocating. Despite no previous medical training, he attempted to perform an emergency tracheostomy using a sharp carving knife. An incision was made slightly to the left of the midline in the anterior neck. His attempt failed, but the seizure settled.
The patient was admitted to hospital with the knife wound and a CT of the neck was performed. This demonstrated superior mediastinal gas and an anterior left-sided haematoma, likely secondary to disruption of the left anterior jugular vein but all other structures including the left vertebral artery at this time appeared intact (see figure 1 and 2). She was managed conservatively and discharged after a period of observation.
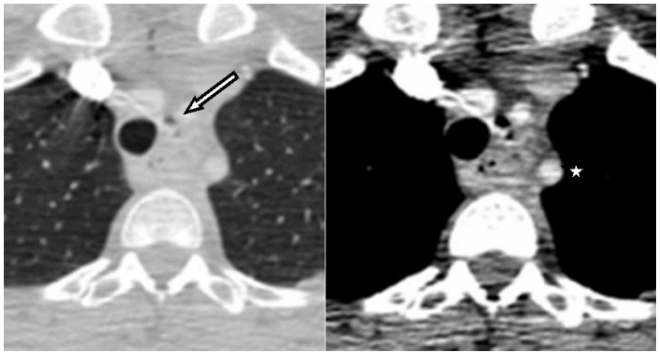
Figure 1.
40 year old women with vertebral arterio-venous fistula secondary to penetrating cervical trauma. Axial Contrast- Enhanced Computed Tomography of the upper chest and neck, (right, lung windows) and (left, mediastinal windows): air in the superior mediastinum (arrows) close to the left subclavian artery (star).
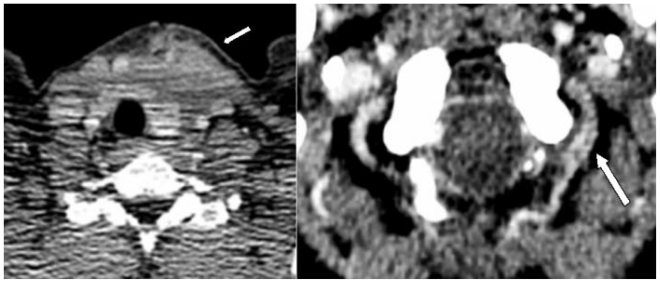
Figure 2.
40 year old women with vertebral arterio-venous fistula secondary to penetrating cervical trauma. Axial Contrast- Enhanced Computed Tomography of the neck demonstrating left anterior neck haematoma (arrow, left) and enhancement of the left vertebral artery at the atlanto-occipital level (arrow, right).
Six months later she re-presented with symptoms of hearing a repetitive left-sided “whooshing” noise or tinnitus. She was able to obliterate this by turning her head to the right. Her neurological examination was unremarkable, however she exhibited a machinery murmur on auscultation of the left side of her upper chest and this was obliterated with a head turn to the right.
The patient was investigated with carotid and vertebral artery Doppler ultrasound. This demonstrated abnormal flow within the left vertebral vein that appeared arterialised. Subsequent 2D time-of-flight (figure 3 and 4) plus 3D contrast-enhanced magnetic resonance angiogram (MRA) (figure 5) helped to confirm the diagnosis, with occlusion of the left vertebral artery beyond its origin with early filling of the vertebral vein. The appearances were consistent with a left verterbro-vertebal arterio-venous fistula, thought secondary to the traumatic event 6 months earlier.
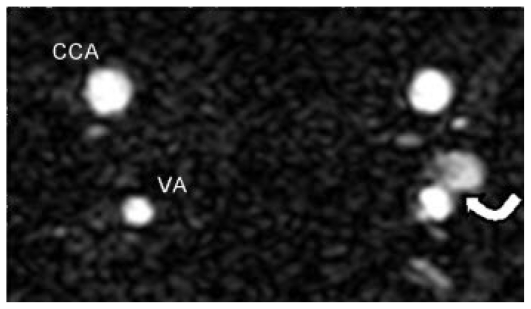
Figure 3.
40 year old women with vertebral arterio-venous fistula secondary to penetrating cervical trauma. Axial time-of-flight MRA demonstrating a “blush” (arrow) from the left vertebral artery at the origin of the fistulous connection. The contralateral neck vessels are annotated (CCA = Common carotid artery, VA = Vertebral artery).
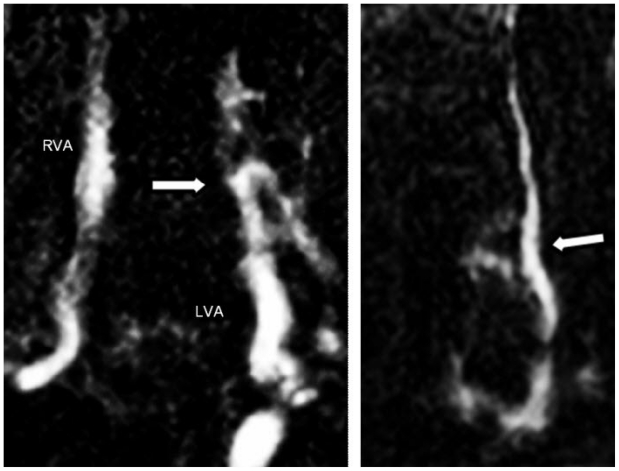
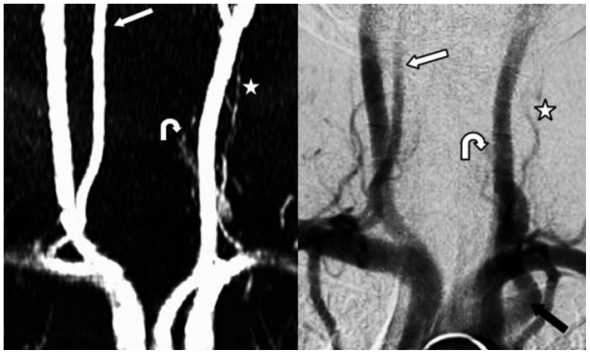
Figure 4.
40 year old women with vertebral arterio-venous fistula secondary to penetrating cervical trauma. Coronal 2D time of flight MRA demonstrating (left) early occlusion of the left vertebral artery (white arrow) with fistulous connection. A further coronal image (right) shows fistulous connection and arterial flow in a left vertebral vein (white arrow). RVA = Right vertebral artery, LVA = Left vertebral artery.
Figure 5.
40 year old women with vertebral arterio-venous fistula secondary to penetrating cervical trauma. Left: 3D Contrast-Enhanced Magnetic Resonance Angiogram demonstrating intact right vertebral artery (straight arrow), occluded left vertebral artery (curved arrow) and arterial flow in the left vertebral vein (star). Right: Comparative Digital Subtraction Angiogram demonstrating intact right vertebral artery (straight arrow), occluded left vertebral artery (curved arrow) arterial flow in a left vertebral vein (star) and flow within the left brachiocephalic vein (black arrow).
The patient was admitted for a formal angiogram, and endovascular intervention. This was performed under local anaesthesia. Angiography demonstrated an occluded distal left vertebral artery, normal right vertebral artery and early filling of the left vertebral and brachiocephalic veins (see figure 5 right and figure 6).
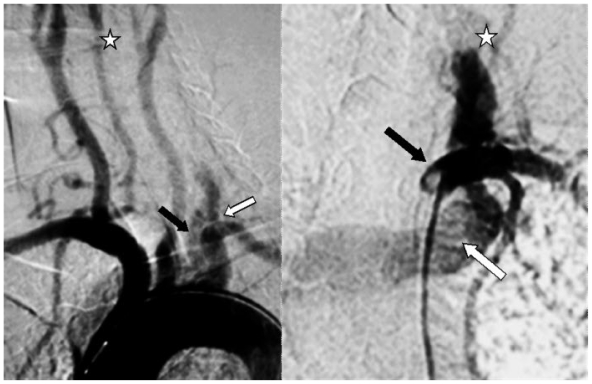
Figure 6.
40 year old women with vertebral arterio-venous fistula secondary to penetrating cervical trauma. Left: Arch Aortogram showing flow with early occlusion in the left vertebral artery (white arrow) with retrograde flow in the left brachiocephalic vein (black arrow). Right: Left Subclavian Angiogram showing catheter in the left subclavian artery (black arrow), an early occlusion of the left vertebral artery (star) and retrograde flow in the left brachiocephalic vein (white arrow).
Embolisation of the vertebral artery was selected as treatment because the distal vertebral artery was occluded. A 6F sheath with a haemostatic valve was introduced into the right common femoral artery and a 5 F head hunter catheter (Angiodynamics, Glenn Falls, NY, USA) was advanced into the proximal left vertebral artery (see figure 7). Multiple 3 mm coils (Complex helical fibered platinum coil, Boston Scientific, Fremont, USA) deployed in the proximal vertebral artery. This abolished flow into the vertebral vein.
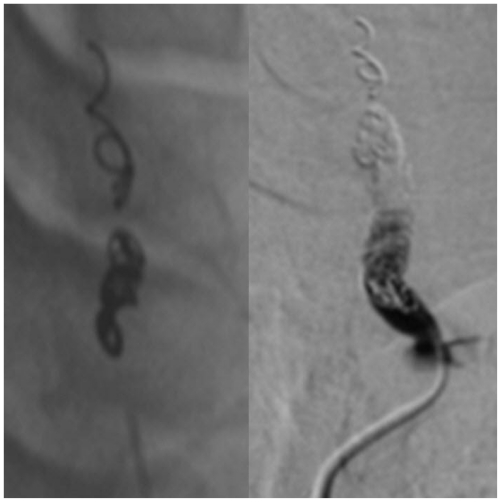
Figure 7.
40 year old women with vertebral arterio-venous fistula secondary to penetrating cervical trauma. Left: Fluoroscopy and Right: Left vertebral artery DSA demonstrating coil deployment and post-coiling occlusion of the left vertebral artery with absent flow in the left vertebral vein.
The patient’s symptoms were abolished using this technique. There was no return of symptoms at 3 months follow up. Follow-up Doppler ultrasound showed occluded left vertebral artery and normal flow in the vertebral vein. No neurological deficit developed during or after intervention.
DISCUSSION
Clinical features
Arteriovenous fistulae can present in a variety of ways including an audible bruit and/or subjective experience of tinnitus (1) as seen in this case. Other mechanisms include arterial steal (2), resulting in vertebrobasillar ischaemia: symptoms include diplopia, headaches and vertigo. More rarely cervical radiculopathy (3) can result leading to altered power and sensation.
While the majority are traumatic in aetiology (2), conditions including fibromuscular dysplasia and neurofibromatosis predispose to spontaneous fistula formation (10, 11), while a proportion may be congenital.
Imaging
Aids to diagnosis of the condition include doppler ultrasound, MRA, CTA and of course, catheter angiography. Doppler ultrasound is a cheap and minimally invasive test that is often used as a first line investigation, especially in the context of a bruit or murmur and is often useful as a follow-up tool. The diagnosis can certainly be suggested by this modality, with arterial flow seen in dilated adjacent veins, but it is often not possible to identify the exact site of involvement (12) and differentiation from other conditions such as vertebral artery stenosis or an arteriovenous malformation is difficult. Ultrasound is also limited by operator dependence and ability to image patients with difficult anatomy or with neck haematomas (14). A definitive examination is therefore needed.
Although conventional catheter angiography is the imaging technique of choice (it provides good anatomical detail and information regarding haemodynamics that is needed for treatment planning), MRA and CTA are increasingly used to help make the diagnosis. The use of MRA in imaging the vertebral artery is well described by Tay et al (12) where its potential in the diagnosis of vertebral AV fistula is suggested. Both 2D time-of-flight and 3D contrast enhanced MRA was useful in our case, demonstrating a fistulous connection to and arterial flow within paravertebral veins. MRA is, however, limited by several potential drawbacks that are not encountered using catheter angiography. These include inappropriate image coverage, subtraction misregistration artifacts, pseudodissection, and phase artifacts (13). Furthermore, MRA exhibits poor temporal resolution and slow scan times can, by scan completion, result in contrast filling of veins. Venous enhancement makes identification of the point of transition from artery to vein difficult (13). To the authors’ knowledge, the use of MRA in diagnosis of this condition is published only in case reports and no large series of comparison with catheter angiography is described.
Computed Tomography Angiography (CTA) is an alternative modality used in imaging of the vertebral artery. Stuhlfaut et al (14) have reported good correlation between catheter angiography and CTA in a series of cervical arterial injuries including several cases of vertebral arterio-venous fistula. CTA has the advantage of minimally invasive speed of acquisition that is vital in the acute setting. Use of 3D software packages now integrated within PACS systems also allows a detailed multiplanar analysis of the vasculature. The practical disadvantage of CTA is the confounding effect of vessel wall calcifications on image interpretation (14) as well as artefact caused by metal, (specifically bullet fragments), which may obscure vascular detail (15). In these cases, angiography is likely to be necessary for optimal assessment. Similarly, shoulder streak artifacts may limit the diagnostic information in some cases (15). Additional factors that should be considered include patient exposure to ionising radiation and the use of potentially nephrotoxic iodinated contrast media.
Management
Surgical management of vertebral AV fistulae is technically difficult owing to the vessel’s anatomical position that makes adequate exposure and vessel control challenging. We described endovascular management using vertebral artery embolisation. This method was employed as the vertebral artery was occluded distal to the fistula. This approach appears to be a safe method in the treatment of vertebral AV fistula when the vertebral artery is occluded distally.
Several other embolisation strategies for the treatment of arterio-venous fistulae involving the vertebral artery have been described. These include the use of balloon occlusion (5) or a combination of coil and balloon occlusion of the vertebral artery (4) particularly with acute high-flow fistulae to ensure immediate treatment of the lesion. In addition, coil deployment within the vertebral vein through cannulation of the orifice of the arteriovenous fistula with a microcatheter has been described (3) with success. This has the added advantage of maintaining flow within the vertebral artery.
In the presence of a patent artery, endovascular reconstruction of the artery using covered stents is also advocated (6, 7, 8, 9). Again, this conveys the theoretical advantage of maintaining flow within the vessel. Furthermore, in the case of a dilated vertebral vein it may limit the need to deposit a large amount of embolic material within this vessel close to the intervertebral foramen: potentially tightening the foramen and compressing the nerve root (9). Questions do remain regarding the long term patency of covered stents used in the vertebral artery, as it is subject to compression from external structures and early cases of stent occlusion have been described (8).
TEACHING POINT
Vertebral arterio-venous fistula should be considered in the presence of tinnitus or a murmur following penetrating neck trauma. The condition can be suggested by Doppler ultrasound and confirmed using non-invasive imaging techniques including MRA and CTA although both have pros and cons. Surgical management is challenging, however, safe treatment can be achieved using endovascular methods including coil embolisation and stenting.
ABBREVIATIONS
- CTA
Computed Tomography Angiography
- MRA
Magnetic Resonance Angiography
REFERENCES
- 1.Amirijamshidi A, Abbassioun K, Rahmat H. Traumatic aneurysms and arteriovenous fistulas of the extracranial vessels in war injuries. Surg Neurol. 2000;53:136–145. doi: 10.1016/s0090-3019(99)00181-0. [DOI] [PubMed] [Google Scholar]
- 2.Gobin YP, Duckwiller GR, Vinuela F. Direct arteriovenous fistulas (carotid-cavernous and vertebral-venous) Neuroimaging Clin N Am. 1998;8:425–443. [PubMed] [Google Scholar]
- 3.Tenjin H, Kimura S, Sugawa N. Coil embolization of vertebro-vertebral arteriovenous fistula: a case report. Surg Neurol. 2005;63:80–83. doi: 10.1016/j.surneu.2004.01.026. [DOI] [PubMed] [Google Scholar]
- 4.Albuquerque F, Javedan S, McDougall C. Endovascular management of penetrating vertebral artery injuries. J Trauma. 2002;53:574–580. doi: 10.1097/00005373-200209000-00032. [DOI] [PubMed] [Google Scholar]
- 5.Halbach VV, Higashida RT, Heishima GB. Treatment of vertebral arteriovenous fistulas. Am J Roentgnol. 1988;150:405–12. doi: 10.2214/ajr.150.2.405. [DOI] [PubMed] [Google Scholar]
- 6.Gonzalez A, Mayol A, Gil-Peralta A, et al. Endovascular stent-graft treatment of an iatrogenic vertebral arteriovenous fistula. Neuroradiol. 2001;43:784–786. doi: 10.1007/s002340100586. [DOI] [PubMed] [Google Scholar]
- 7.Singer RJ, Dake MD, Norbash A, et al. Covered stent placement for neurovascular disease. Am J Neuroradiol. 1997;18:507–509. [PMC free article] [PubMed] [Google Scholar]
- 8.Huttl K, Sebestyen M, Entz L, et al. Covered stent placement in a traumatically injured vertebral artery. J Vasc Intervent Radiol. 2004;15:201–2. doi: 10.1097/01.rvi.0000109406.52762.98. [DOI] [PubMed] [Google Scholar]
- 9.Sadato A, Satow T, Ishii A, et al. Large vertebral arteriovenous fistula treated with stent-grafts--case report. Neurologia Medico-Chirurgica. 2003;43:250–254. doi: 10.2176/nmc.43.250. [DOI] [PubMed] [Google Scholar]
- 10.Bahar S, Chiras J, Carpena JP, et al. Spontaneous vertebro-vertebral arterio-venous fistula associated with fibro-muscular dysplasia. Report of two cases. Neuroradiol. 1984;26:45–49. doi: 10.1007/BF00328203. [DOI] [PubMed] [Google Scholar]
- 11.Deans WR, Bloch S, Leibrock L, et al. Arteriovenous fistula in patients with neurofibromatosis. Radiol. 1982;144:103–107. doi: 10.1148/radiology.144.1.6806851. [DOI] [PubMed] [Google Scholar]
- 12.Tay KY, U-King-Im JM, Trivedi RA, et al. Imaging the vertebral artery. Euro Rad. 2005;15:1329–1343. doi: 10.1007/s00330-005-2679-z. [DOI] [PubMed] [Google Scholar]
- 13.Sharma AK, Westesson P. Preoperative evaluation of spinal vascular malformation by MR angiography: How reliable is the technique: Case report and review of literature. Clin Neurol and Neurosurg. 2008;210:521–524. doi: 10.1016/j.clineuro.2008.02.005. [DOI] [PubMed] [Google Scholar]
- 14.Stuhlfaut JW, Glenn Barest G, Sakai O, et al. Impact of MDCT Angiography on the use of Catheter Angiography for the assessment of cervical arterial injury after blunt or penetrating trauma. Am J Roentgenol. 2005;185:1063–1068. doi: 10.2214/AJR.04.1217. [DOI] [PubMed] [Google Scholar]
- 15.Núñez DB, Torres-León M, Múnera F. Vascular injuries of the neck and thoracic inlet: Helical CT-Angiographic correlation. Radiographics. 2004;24:1087–1098. doi: 10.1148/rg.244035035. [DOI] [PubMed] [Google Scholar]