Abstract
This report describes a case of mesenchymal cystic hamartoma of the liver with diagnostic imaging work-up using only ultrasound and MRI. We demonstrate an approach starting from the pediatrician’s physical exam culminating in surgical resection and pathologic confirmation with an emphasis on MR imaging.
Keywords: Mesenchymal Cystic Hamartoma, Magnetic Resonance Imaging, MRI
CASE REPORT
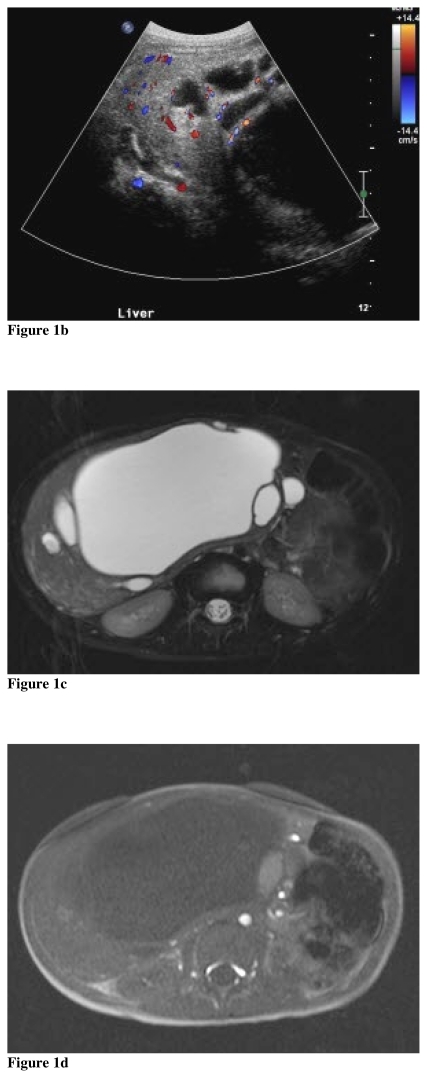
A 23-month-old male presented to his primary pediatrician with a six month history of increasing abdominal distention, progressively worsening vomiting, and weight loss. There was no history of fever or pain. On physical examination, hepatomegaly was present and the patient was referred for ultrasound (US). On songraphy, there was a large complex multilobulated cystic mass within the right liver. The largest cyst measured 16 × 10 × 12 cm. There were multiple smaller adjacent cysts with intervening internal septations measuring up to 5 mm in width (Fig. 1a). On color Doppler, vascularity was present in these septations (Fig. 1b). There was no vascularity within the cysts. To further assist in delineating the overall anatomy, magnetic resonance imaging (MRI) was performed.
Figure 1.
Mesenchymal cystic hamartoma in a 23-month-old male. (a) Transverse US image reveals a large complex cystic mass containing internal echos within the right liver lobe (b) transverse color US image at the inferior right liver demonstrates vascularity within septations (c) axial T2W MRI image with fat saturation (d) axial T1 pre and (e) post contrast demonstrates a multilobulated cystic mass within the right liver including one cyst - located just to the left of the dominant cyst - with internal hemorrhage. (f) gross pathological specimen. (g) disordered hepatic parenchyma with irregular bile ducts surrounded by immature mesenchyme, H&E 10X.
The patient was imaged on a 1.5T magnet (Siemens Magnetom SymphonyTM) utilizing the following sequences: 3 plane HASTE localizer sequences, axial T1 in and out of phase (TR 269/TE 4.7&2.3), coronal T1 gradient echo (TR 1676/TE 4.9), three plane T2 turbo spin echo (TR 5250/TE 154) with fat saturation, and three plane T1 (TR 884/TE 21) spin echo with fat saturation post contrast (Magnevist®, Bayer Healthcare). MRI demonstrated a very large complex cystic lesion occupying the entire right lobe of the liver resulting in mass effect on the adjacent organs including displacement of the left lobe of the liver. The mass measured 17 cm × 10 cm × 15 cm. The cystic areas were low in signal intensity on T1 and high signal intensity on T2 weighted sequences. There was a single cyst with high signal intensity on both T1 and T2 sequences located in the right anterior liver, highly suggestive of prior hemorrhage (Fig. 1c, 1d). The internal septations and rim of soft tissue surrounding the cysts enhanced post-contrast (Fig. 1e). There were no additional lesions identified in the liver. There was no adenopathy in the abdomen. The imaging findings were highly suggestive of benign mesenchymal cystic hamartoma. A right hepatic lobectomy was performed and this diagnosis was confirmed (Fig. 1f).
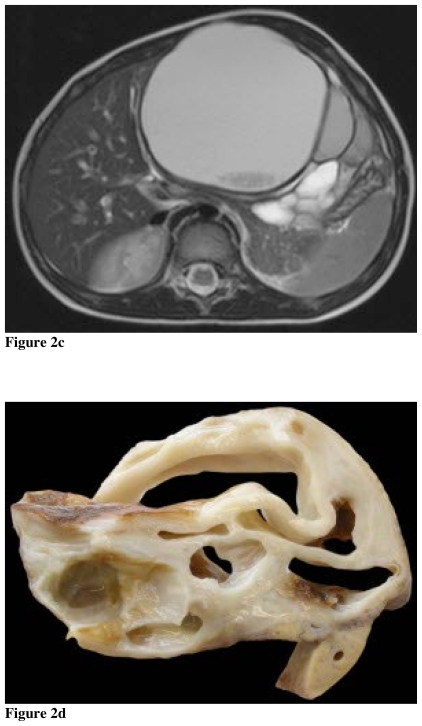
The gross pathologic specimen weighed 1,251 g and had a smooth, tan, dull surface. Sectioning revealed that the largest cyst measured 13 cm × 10.5 cm × 6 cm. Most of the cysts were filled with a yellowish green clear fluid. The internal cyst lining had a white appearance. The solid areas were white and tan-yellow, marbled appearance with a rubbery texture. On histology, there was no evidence of malignancy. The solid part was composed of a mixture of fibrous tissue, disordered bile ducts surrounded by loose mesenchyme, and islands of bland hepatocytes. The cystic structures were lined by attenuated epithelium (Fig. 1g).
DISCUSSION
Mesenchymal cystic hamartoma of the liver is a rare benign developmental malformation comprised of multiple cysts with internal septae (1). Cross sectional imaging of mesenchymal cystic hamartomas is often necessary to help facilitate planning of surgical resection. While CT has often been the preferred cross sectional imaging study, MRI is a feasible alternative with the benefit of avoiding ionizing radiation. We present a case which demonstrates an approach from clinical presentation to final pathology with an emphasis on MR imaging.
Mesenchymal hamartomas are composed of disorganized bile ducts, immature fluid filled mesenchymal tissue, and hepatocytes. This lesion likely originates as disturbances along the connective tissue of the portal tracts (1). Although mesenchymal hamartomas are benign lesions, there are rare occurrences of malignant degeneration to undifferentiated embroynal sarcoma (2). Mesenchymal hamartomas usually present in children less than four years old with either painless abdominal distention or abdominal mass. Since these lesions arise from mesenchymal rather than epithelial tissue, if laboratory evaluation is undertaken, tumor marker alpha fetal protein is normal in most, but not all, cases. Following clinical evaluation, imaging is crucial in determining the lesion location and suggesting the underlying pathology.
Although a rare entity, the radiographic appearance of mesenchymal hamartomas has been well described utilizing US and CT. Mesenchymal hamartomas may present as either cystic or stromal predominant lesions (3). Similar to the cases presented, mesenchymal hamartomas classically present as cystic lesions with multiple thin internal septations on US (1). The CT appearance demonstrates a spectrum of features ranging from a multiseptated macrocystic mass to a solid mass with enhancement of the septa and solid portions. There is correlation between the degree of solid components and the amount of hepatocytes on pathologic specimen (4). Calcification is very uncommon; however, a recent report demonstrated a unique presentation with calcification at the periphery of the lesions on CT (5). Although appearance on CT has been established, the clinical use of MRI in delineating this entity is emerging.
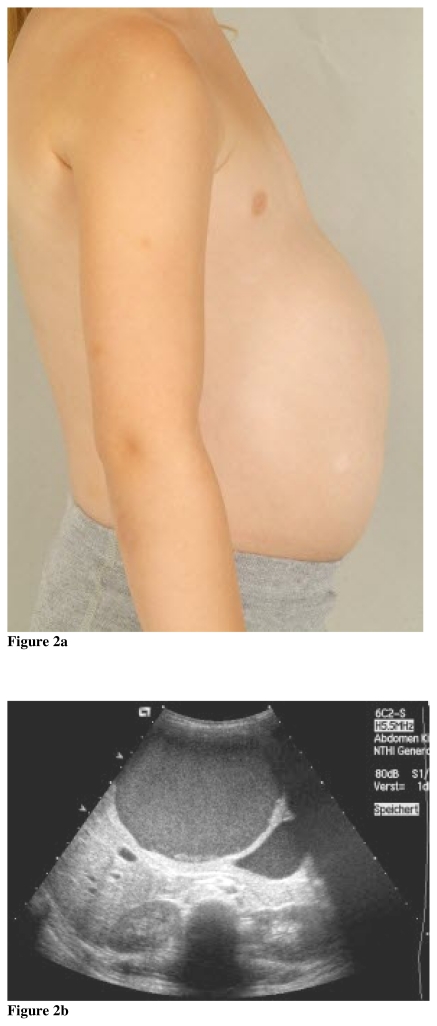
The MRI findings of mesenchymal hamartomas were reported for the first time in 1994 (6). In the interim, a series of twelve cases from the gastroenterology literature again demonstrated a spectrum of findings ranging from cystic to solid lesions. This series also depicted the relationship of lesion to the intrahepatic vessels (7). The MRI features reflect the underlying morphology of the lesion with cystic predominant lesions displaying high signal intensity on T2 weighted images, and variable intensity on T1 weighted images due to cyst contents. The intervening septations are of low signal intensity and display enhancement. These MRI findings are reflected in the case presented as well as an additional companion case of pathologically confirmed mesenchymal cystic hamartoma (Fig. 2). MRI is advantageous over other currently available imaging modalities because MRI has superb soft tissue characterization ability. Also, MRI with MRCP provides improved depiction of the biliary system which assists in surgical resection.
Figure 2.
Mesenchymal cystic hamartoma in a 4-year-old female. (a) Clinical image demonstrating distended abdomen at presentation (b), transverse US image of the liver showing a cystic mass in the left liver containing internal debris (c) axial T2W MRI image reveals the complex nature of the cystic high signal lesion with internal low signal debris (d) correlative gross pathologic specimen with “swiss cheese” like cystic channels.
The clinical approach presented in this case report and accompanying companion case, specifically utilizing US followed by MRI, is crucial in providing optimal imaging without the use of radiation. Although the initial diagnosis of mesenchymal hamartoma (particularly the cystic predominant pattern) can be made on ultrasound, further anatomic delineation prior to surgical resection is necessary to minimize surgical complications (8). While CT provides this information, the use of ionizing radiation must be reconsidered given the known potentially deleterious effects. Image GentlyTM has reemphasized the need to use alternatives to ionizing radiation when clinically feasible (9). These cases demonstrate a clinical pathway of progression from pediatrician’s physical examination to surgical resection with pathologic confirmation without the use of ionizing radiation.
TEACHING POINT
MRI provides optimal imaging for diagnosis and surgical planning of mesenchymal cystic hamartomas of the liver with the additional benefit of avoiding ionizing radiation.
ABBREVIATIONS
- US
Ultrasound
- MRI
Magnetic Resonance Imaging
- CT
Computed Tomography
- MRCP
Magnetic resonance cholangiopancreatography
- TM
Trademark
REFERENCES
- 1.Ros P, Goodman Z, Ishak K, et al. Mesenchymal Hamartoma of the Liver: Radiologic-Pathologic Correlation. Radiology. 1986;158:619–624. doi: 10.1148/radiology.158.3.3511498. [DOI] [PubMed] [Google Scholar]
- 2.Stringer M, Alizai N. Mesenchymal hamartoma of the liver: A systematic review. J Pediatr Surg. 2005;40:1681–1690. doi: 10.1016/j.jpedsurg.2005.07.052. [DOI] [PubMed] [Google Scholar]
- 3.Powers C, Ros P, Stoupis C, Johnson W, Segel K. Primary Liver Neoplasms: MR imaging with Pathologic Correlation. RadioGraphics. 1994;14:459–482. doi: 10.1148/radiographics.14.3.8066263. [DOI] [PubMed] [Google Scholar]
- 4.Kim S, Kim W, Cheon J, et al. Radiological Spectrum of Hepatic Mesenchymal Hamartoma in Children. Korean J Radiol. 2007;8:498–505. doi: 10.3348/kjr.2007.8.6.498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Steiner M, Giles H. Mesenchymal hamartoma of the liver demonstrating peripheral calcifications in a 12-year-old boy. Pediatr Radiol. 2008;38:1232–1234. doi: 10.1007/s00247-008-0942-6. No open access version available. [DOI] [PubMed] [Google Scholar]
- 6.Wholey M, Wojno K. Pediatric hepatic mesenchymal hamartoma demonstrated on plain film, ultrasound and MRI, and correlated with pathology. Pediatr Radiol. 1994;24:143–144. doi: 10.1007/BF02020176. No open access version available. [DOI] [PubMed] [Google Scholar]
- 7.Ye B, Hu B, Wang L, et al. Mesenchymal Hamartoma of liver: Magnetic resonance imaging and histopathologic correlation. World J Gastroenterol. 2005;11:5807–5810. doi: 10.3748/wjg.v11.i37.5807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Karpelowsky J, Pansini A, Lazarus C, Rode H, Millar A. Difficulties in the management of mesenchymal hamartomas. Pediatr Surg Int. 2008;24:1171–1175. doi: 10.1007/s00383-008-2239-0. [DOI] [PubMed] [Google Scholar]
- 9.CT and Radiation Dose. [accessed Dec 2008]. http://www.imagegently.com/CT.