Abstract
Calcific tendinosis (tendonosis/tendonitis) is a condition which results from the deposition of calcium hydroxyapatite crystals in any tendon of the body. Calcific tendonitis usually presents with pain, which can be exacerbated by prolonged use of the affected tendon. We report a case of calcific tendinosis in the posterior tibialis tendon at the navicular insertion. The pathology is rare in the foot, and extremely rare in the tibialis posterior tendon, indeed there are only 2 reported in the published literature. This case report highlights the need to consider calcific tendinosis in the foot despite its rarity. If this diagnosis is considered early, appropriate investigations can then be requested and unnecessary biopsies, use of antibiotics and surgery can be avoided. We also discuss possible causes of calcific tendinosis in the tibialis posterior tendon, the role of imaging modalities and review treatment methods.
Keywords: Calcific Tendonosis, Tendonitis, Tendinosis, Posterior Navicular Tendon, navicular attachment, navicular insertion, calcium hydroxyapatite, navicular tuberosity, tibialis posterior tendon
CASE REPORT
The patient was a 42 year old female, employed as an administration assistant. She presented to the Accident and Emergency department complaining of discomfort in the medial foot/ankle, which had caused a disturbed night’s sleep; it had started approximately 2 hours after finishing a usual day’s work the previous day. The patient’s past medical history included Asthma, for which she was being treated with Ventolin and Becotide inhalers, and lower back pain, for which she was taking analgesics: Tramadol, Codeine, Diazepam and Amitriptyline. The only other recorded medical problem was an allergy to lanolin. The patient had no significant history of prior foot trauma, although she had noted mild discomfort in the affected area intermittently during the previous year, however not sufficient enough to cause her to visit her GP.
On examination she had a pink, hypersensitive, hot, area of swelling over the region of the navicular tuberosity. The patient was non weight bearing on her right foot. She complained of pain on resisted inversion and plantar flexion. The active range of movements was restricted in all directions due to pain. The patient was systematically well, with a temperature of 36.7 degrees C and no other symptoms. Palpitation was impossible due to the acute and highly sensitive nature of the pain.
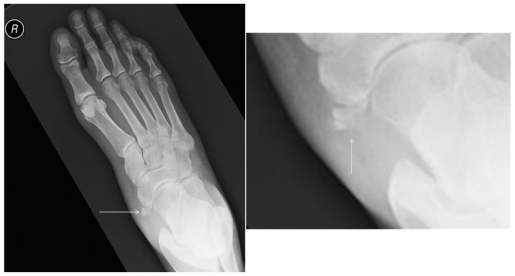
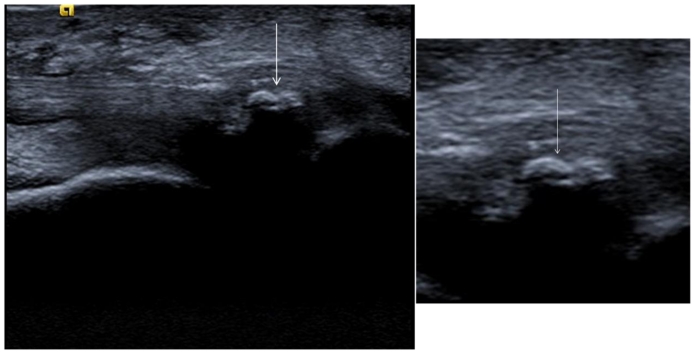
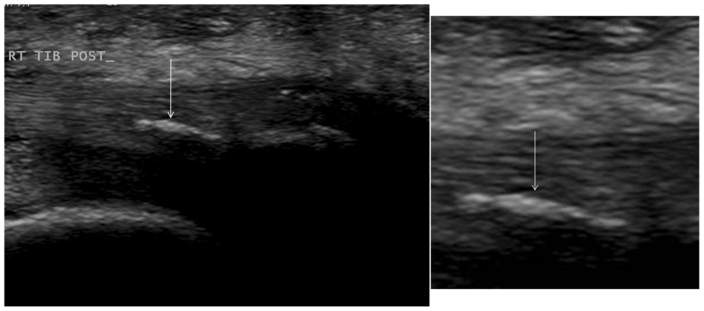
Investigations included plain radiographs (figure 1) which showed swelling of soft tissues overlying the right navicular, associated with amorphous calcification adjacent to the navicular tuberosity. The ultrasound (figures 2 and 3) demonstrated calcific tendinosis of the tibialis posterior tendon close to its insertion on the navicular bone, there was also oedema within the subcutaneous soft tissues around the tibialis posterior tendon. Under ultrasound guidance an injection of triamcinolone acetate (1 ml of 40 mg per ml) and bupivacaine (1 ml of 0.5%) was carried out in the area of maximal tenderness and around the distal tibialis posterior tendon.
Figure 1.
A 42 year old female was diagnosed with calcific tendinosis of the posterior tibialis tendon. AP radiograph of the right foot shows ‘cloudy’ calcium hydroxyapatite crystals adjacent to the navicular tuberosity due to calcific tendinosis of the tibialis posterior tendon. White arrow indicates location of pathology.
Figure 2.
A 42 year old female was diagnosed with calcific tendinosis of the posterior tibialis tendon. Ultrasound scan of the tibialis posterior tendon carried out using an 8–12 MHz linear array ultrasound probe in the longitudinal plane showed calcific tendinosis within the tendon distally, close to its insertion into the navicular bone. The rest of the tibialis posterior tendon was intact and of normal echo texture. White arrow indicates location of pathology.
Figure 3.
A 42 year old female was diagnosed with calcific tendinosis of the posterior tibialis tendon. Ultrasound scan of the tibialis posterior tendon carried out using an 8–12 MHz linear array ultrasound probe in the longitudinal plane (slightly different angle than seen on figure 2) showed calcific tendinosis within the tendon distally, close to its insertion into the navicular bone. The rest of the tibialis posterior tendon was intact and of normal echo texture. White arrow indicates location of pathology.
The patient was initially treated conservatively with rest, elevation of the affected foot, crutches, and use of the already prescribed Tramadol, Codeine and Diazepam. In addition she was given Diclofenac 50 mg TDS. A local steroid injection (triamcinolone acetate) under ultrasound guidance was carried out 2 weeks later. The Patient showed significant improvement, and no further treatment was deemed necessary.
DISCUSSION
Calcific tendinosis most commonly affects the tendons of the shoulder, being seen in approximately 3% of adults [1]. However it has also been reported in many other parts of the body. It tends to affect men and women equally in the 4th to 6th decades with a slight predominance in premenopausal women [2]. The pathology is rare in the foot, and accounts for only 1% of reported cases [3], it has been reported most commonly in the flexors of the forefoot [3, 4]. There are, however, only two reported cases of calcific tendinosis in the tibialis posterior tendon [5, 6] in English language literature.
The tibialis posterior muscle originates from lateral part of posterior surface of tibia and the medial 2/3 of fibula. The major insertion site for the tibialis posterior tendon is the navicular bone. Posterior tendon slips of the tibialis posterior tendon pass to the sustenaculum talus of calcaneus, the plantar surface of all 3 cuneforms, the cuboid and to base of 2nd, 3rd, and 4th metatarsals.
Calcific tendinosis has been variously described in literature under the synonyms of calcific peritendinitis, calcific bursitis, periarthritis calcarea and hydroxyapatite rheumatism [3]. It is a relatively common problem in a number of areas in the body. These include the tendons of the Longus colli muscle [6], Pectoralis major and the Rotator cuff muscles [1], in fact approximately 50% of shoulder pain problems [1] are caused by calcific tendinosis. However in the foot it is not commonly seen, particularly not over the navicular tuberosity, hence is often not considered in a clinical situation. This could potentially result in missed diagnosis and possibly lead to inappropriate treatment with antibiotics or even surgery. Such differential diagnoses include local infection, fracture, and in more unusual cases possibly Gout or CPPD (calcium pyrophosphate dihydrate deposition disease).
A more common pathology for which calcific tendinosis could be mistaken is the presence of an accessory navicular bone (os navicularum or os tibiale externum). This is an extra bone or piece of cartilage that can be present on the inner side of the foot just above the arch. It is incorporated within the posterior tibial tendon, and can give almost identical symptoms to calcific tendinosis of the posterior tibialis tendon. This possibility should be considered, although coincidently the treatment is almost the same.
In terms of development, four distinct phases have been identified in calcific tendinosis: formative, calcific, resorptive and reparative [6], however the mechanism of development of calcium hydroxyapatite crystals is poorly understood. It has been postulated that it may occur as response to local hypoxia [6], or sub lethal trauma, however there is no consistently seen or reported cause. There are numerous competing theories, Harvie et al [7] describe an association between calcific tendinosis and disorders of thyroid and oestrogen metabolism. Gohr et al [8] postulated that extracellular organelles called matrix vesicles may be the origin of the pathologic calcification.
The use of conservative treatment is reported to be effective with Accessory Navicular Syndrome [9], although local steroid injections may have a more prominent effect on patients with calcifying tendonitis [10]. As a result clinical vigilance for this pathology may prevent unnecessary surgical intervention. If the possibility of calcific tendinosis is considered, then radiographic diagnosis is usually straightforward. The calcific concretions are found in a classic location, with a characteristic comet tail appearance [6]. Plain radiographs are usually sufficient to diagnose the pathology, and even the extent, delineation and density of calcification [6]. Symptomatic patients tend to have ill-defined hazy calcification with fluffy appearance, whereas less symptomatic patients tend to have well defined calcifications [6].
Computed tomography can be used to assess the extent of damage caused in aggressive cases, and ultrasound shows calcifications as hyperechoic structures which may or may not have posterior acoustic shadowing. Ultrasound can be used to good effect to accurately identify the involved tendon, the best resolution and visualisation of the tendon at ultrasound is obtained using a high frequency (10–15 MHz) linear array probe. Ultrasound guidance can also be used for aspiration of soft calcifications and injection of steroids. Magnetic resonance imaging (MRI) may show calcifications as low intensity foci, however is of little use compared to the aforementioned techniques due to lack of specificity for identifying calcification which is of the same or similar low signal intensity as the rest of the tendon. On extensive literature research we could not find evidence of increased uptake on bone scintigraphy with calcific tendonosis. However one paper suggested increased uptake on bone scintigraphy when there is osseous involvement (which is not the case in our patient) [11].
When calcific tendinosis of the tibialis posterior tendon is diagnosed there are several treatment options, however due to the scarcity of reported cases, the best option remains uncertain [12]. We would suggest a similar sequence of treatment to calcific tendinosis in other locations; primarily the patient should be treated conservatively, potentially with bracing, taping, foot orthotics, and stretching. Secondary treatment may include extra corporeal shockwave lithotripsy, needle aspiration and steroid injection. If these techniques fail then surgical removal of the calcification is an option. In operations on calcific tendinosis of the rotator cuff, preoperative ultrasonic mapping of calcium deposits significantly aids location and removal of the problematic calcific deposits [13]. This technique could be equally beneficial when operating on patients with calcific tendinosis on the tibialis posterior tendon.
TEACHING POINT
Calcific tendinosis of the tibialis posterior tendon should be considered as a diagnosis in cases where a patient presents with discomfort in the medial foot/ankle, and swelling over the region of the navicular tuberosity. Plain radiographs are sufficient to confirm this diagnosis; however ultrasound is useful to ascertain more information regarding the location and extent of calcification, and may aid intervention if conservative treatment fails.
Table 1.
Summary table for calcific tendonitis of the tibialis posterior tendon.
| Etiology | Unknown, though possible explanations include: Local hypoxia; sub lethal trauma; disorders of thyroid and oestrogen metabolism; or extracellular organelles called matrix vesicles |
| Incidence | Unknown |
| Gender ratio | Calcific tendinosis tends to affect men and women equally with a slight predominance in premenopausal women; however incidence in the tibialis posterior tendon is too rarely reported to construct a gender ratio. |
| Age predilection | 4th to 6th decades |
| Risk factors | Older than 40, female |
| Treatment | Conservative treatment with rest, bracing, taping, foot orthotics, and stretching. Secondary treatment may include extra corporeal shockwave lithotripsy, needle aspiration and steroid injection. If these techniques fail then surgical removal of the calcification is an option |
| Prognosis | Good prognosis, full recovery possible |
| Findings on imaging | Calcific tendinosis within the tibialis posterior tendon distally, close to its insertion into the navicular bone. calcific concretions are found in a classic location, with a characteristic comet tail appearance |
Table 2.
Differential diagnosis table for calcific tendinosis of the posterior navicular tendon and corresponding imaging findings.
| Disease | X-Ray | Ultrasound | MRI – T1 | MRI – T2 | Pattern of enhancement With GAD | Scintigraphy |
|---|---|---|---|---|---|---|
| Calcific tendonitis of tibialis posterior tendon | Calcification | Calcification in tendon | Low signal | Low signal | none | No uptake |
| Gout | Calcification in soft tissue and erosions | Calcification in soft tissues and erosions | Low signal in soft tissues. May have high signal marrow reactive changes | Low signal | Increased enhancement if active inflammation and marrow reaction | Increased uptake if active |
| Infection | Soft tissue swelling, may have gas in soft tissue and bone destruction | Soft tissue oedema and collections | Low signal | High signal | Increased enhancement in soft tissues and any affected bone | Increased uptake |
| Accessory navicular syndrome | Accessory bone. May be sclerotic | Soft tissue inflammation | Low signal or normal marrow signal | High signal marrow oedema or normal marrow signal | Increased enhancement if inflammation | Increased uptake if inflammation |
| Trauma with bruising | Soft tissue swelling | Oedema and soft tissue swelling | Low signal | High signal | Increased enhancement if recent trauma | Increased uptake if inflamed |
ABBREVIATIONS
- C
Celsius
- CPPD
Calcium Pyrophosphate Dihydrate Deposition Disease
- CT
Computerised tomography
- GP
General Practitioner
- MRI
Magnetic resonance imaging
REFERENCES
- 1.Holt PD, Keats TE. Calcific tendinitis: a review of the usual and unusual. USA Arthritis Rheum. 1989 Jun;32(6):741–7. doi: 10.1007/BF00191518. [DOI] [PubMed] [Google Scholar]
- 2.Fam AG, Rubenstein J. Hydroxyapatite pseudopodagra. A syndrome of young women. Arthritis Rheum. 1989 Jun;32(6):741–7. doi: 10.1002/anr.1780320612. [DOI] [PubMed] [Google Scholar]
- 3.Rhodes RA, Shelling CB. Calcific tendinitis of the flexors of the forefoot. Ann Emerg Med. 1986;15:751–753. doi: 10.1016/s0196-0644(86)80444-9. [DOI] [PubMed] [Google Scholar]
- 4.Gruneberg R. Calcifying tendinitis in the forefoot. Br J Radiol. 1963;36:378–9. doi: 10.1259/0007-1285-36-425-378. [DOI] [PubMed] [Google Scholar]
- 5.Kirschner S, Raab P, Krauspe R. Calcifying tendinitis of the tibialis posterior, case report. Foot Ankle Surg. 1998;4:233–236. [Google Scholar]
- 6.Jakhere SG, Yadav D, Bharambay HV. Acute calcific tendinitis of tibialis posterior tendon (TPT): A rare site of involvement. European Journal of Radiology Extra. 2011 Jan;77(1):e17–e20. [Google Scholar]
- 7.Harvie P, Pollard TCB, Carr AJ. Calcific tendinitis: Natural history and association with endocrine disorders. Journal of Shoulder and Elbow Surgery. 2007 Mar-Apr;16(2):169–173. doi: 10.1016/j.jse.2006.06.007. [DOI] [PubMed] [Google Scholar]
- 8.Gohr CM, Fahey M, Rosenthal AK. Calcific tendonitis: a model. Connect Tissue Res. 2007;48:286–291. doi: 10.1080/03008200701692362. [DOI] [PubMed] [Google Scholar]
- 9.Requejo SM, Kulig K, Thordarson DB. Management of foot pain associated with accessory bones of the foot: two clinical case reports. Clin Orthop Relat Res. 1999 Mar;(360):231–7. doi: 10.2519/jospt.2000.30.10.580. [DOI] [PubMed] [Google Scholar]
- 10.Glaser DL, Dormans JP, Stanton RP, Davidson RS. Surgical management of calcaneal unicameral bone cysts. Clin Orthop Relat Res. 1999 Mar;(360):231–7. doi: 10.1097/00003086-199903000-00027. [DOI] [PubMed] [Google Scholar]
- 11.Flemming DJ, Murphey MD, Shekitka KM, Temple HT, Jelinek JJ, Kransdorf MJ. Osseous Involvement in Calcific Tendinitis: A Retrospective Review of 50 Cases. AJR Am J Roentgenol. 2003 Oct;181(4):965–72. doi: 10.2214/ajr.181.4.1810965. [DOI] [PubMed] [Google Scholar]
- 12.Newmark H, 3rd, Forrester DM, Brown JC, Robinson A, Oiken SM, Bledsoe R. Calcific tendinitis of the neck. J Orthop Sports Phys Ther. 2000 Oct;30(10):580–91. doi: 10.1148/128.2.355. discussion 592–4. [DOI] [PubMed] [Google Scholar]
- 13.Rupp S, Seil R, Kohn D. Preoperative ultrasonographic mapping of calcium deposits facilitates localization during arthroscopic surgery for calcifying tendinitis of the rotator cuff. Arthroscopy. 1998 Jul-Aug;14(5):540–2. doi: 10.1016/s0749-8063(98)70088-x. [DOI] [PubMed] [Google Scholar]