Abstract
Sinistral portal hypertension occurs when a pathological process causes occlusion of the splenic vein. The resultant elevated splenic bed venous pressure causes formation of gastric varices which can lead to hematemesis as a common presentation for this disease process. We present a case of sinistral portal hypertension in a patient with acute hematemesis as the primary presentation. Despite the challenging diagnosis process, the patient underwent splenectomy and was managed appropriately according to previously published literature.
Keywords: Sinistral hypertension, left-sided portal hypertension, pancreatitis, upper gastro intestinal bleeding, UGI bleed
CASE REPORT
A 34-year-old Caucasian male with a 2 year history of HIV/AIDS presented with one episode of severe hematemesis to the Emergency Department at our institution. The patient also suffered from recurrent episodes of shingles and had been compliantly taking Atripla anti-viral therapy to control his viral load and oral amphotericin for a recent fungal infection. There was no prior history of liver disease at the time of presentation.
Physical examination was normal. Subsequently, the patient underwent an emergency upper GI endoscopy which identified actively bleeding gastric varices. Upon further investigation, contrast abdominal CT demonstrated mild hepatosplenomegaly and spleno-gastric varices. No liver cirrhosis or its sequelae were seen and the varices were only observed in the gastric fundus. To differentiate between esophageal varices and simple thickening of esophageal wall, special attention was paid to detection of often multiple nodular, enhancing, intraluminally protruding lesions within the esophageal wall in the portal phase of axial MDCT images. Such lesions would indicate presence of esophageal varices. No suspicious esophageal varices on portal phase of contrast enhanced CT-scan was found in our patient. Initially, portal and splenic veins did not illustrate an obvious stenosis or other abnormalities. However, closer examination suggested the possibility of an occlusion in the region of pancreatic tail/splenic bed (Fig. 1).
Figure 1.
34 year old male with acute onset of hematemesis due to sinistral portal hypertension. Relevant CT scan findings in Portal Venous Phase: Varices (arrow) (a). Soft tissue thickening in splenic hilum (arrow) (b). Splenic vein incomplete filling (arrow) (c, d) on coronal view. Areas of suspected pathology magnified in insert of each corresponding image. (Protocol: Siemens Sensation 64, 3mm slice thickness, 120 kVp 369 mA, Omnipaque 350, 120 cc)
Results of relevant haematological workup are illustrated in table 1.
Table 1.
Relevant haematological workup at the time of presentation
| Measured | Normal | |
|---|---|---|
| AST | 13 U/L | 7–36 |
| ALT | 23 U/L | 4–45 |
| AP | 167 U/L | 31–103 |
| TBIL | 0.3 mg/dL | 0.2–1.1 |
| INR | 1.1 | |
| Creatinine | 0.8 mg/dL | 0.5–1.3 |
| Urea Nitrogen | 16 mg/dL | 7–23 |
A subsequent gastro endoscopy confirmed the isolated gastric varices with no esophageal varices detected. To ensure the absence of any underlying liver pathology, percutaneous liver biopsy was performed which revealed non-specific portal and lobular inflammation without fibrosis. To investigate the splenic vein for possible placement of gastro-venous shunt for the patient’s symptomatic relief from further upper GI bleeding episodes, a splenic arteriogram was performed. This revealed a normal splenic artery with absence of splenic vein filling (Fig. 2).
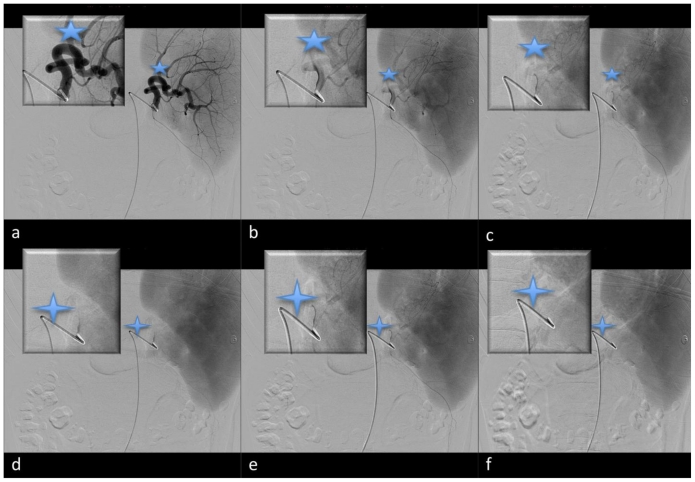
Figure 2.
34 year old male with acute onset of hematemesis due to sinistral portal hypertension. Splenic angiography. Arterial phase (a,c) (five point star) illustrates patent splenic artery. There is an absence of splenic vein filling following splenic artery injection with contrast as depicted by (d-f) (four point star). Corresponding magnified image of the hilum provided in each image insert. (Protocol: Flouroscopy, Philips, Visipaque, 130cc, fluoro time 34.6 minutes, access made through Right femoral artery, selective splenic artery catheterization with a 4Fr Glide Catheter (Terumo, Japan), rate of injection 5 cc/sec, total volume 30 cc, contrast injection made in distal splenic artery proximal to splenic hilum)
Figure 2 findings were supportive of splenic vein occlusion. Closer examination of axial views of the initial CT examination (Fig. 3), in light of the findings on mesenteric angiography made proximal splenic vein occlusion/thrombosis the most likely etiology of this patient’s presentation with acute upper GI bleed. Reviewing the patient’s clinical presentation and radiological findings in light of his near normal liver function tests, lack of physical signs of liver cirrhosis, and non-specific liver biopsy findings made the diagnosis of sinistral/left sided portal hypertension the most likely possibility. While being scheduled for elective splenectomy, the patient experienced a second episode of severe hematemesis, lasting approximately 45 minutes, and underwent an emergent splenectomy and variceal resection. Exploratory laparotomy was performed during which the left gastroepiploic vein was found to be dilated. Furthermore, the pancreatic tail was found to be firm, supporting the hypothesis of silent episodes of pancreatitis as a possible cause, with normal texture in the remainder of the organ. The pathological pancreatic tail extended into splenic hilum and cardia of the stomach. Intra-operative examination revealed a normal appearing liver and mesenteric veins suggesting normal portal vein. Splenectomy combined with partial pancreatomy and gastrotomy was performed. Splenic vein was also removed and was found to be occluded proximally. No abnormality was observed in the splenic vein. Following the surgery, the patient did not experience any further hematemesis while recovering in the hospital. The patient recovered fully from this procedure with no further bleeding episodes and is doing well 90 days post operation.
Figure 3.
34 year old male with acute onset of hematemesis due to sinistral portal hypertension. Soft tissue stranding of splenic hilum suggestive of possible silent chronic pancreatitis (arrow) (a). Splenic vein filling defect (Portal Venous phase shown), initially inconclusive, supported distal splenic vein thrombosis following splenic angiogram illustrated above (arrow) (b,c,d). Areas of suspected pathology magnified in insert of each corresponding image. (Protocol: Siemens Sensation 64, 3mm slice thickness, 120 kVp, 369 mA, Omnipaque 350, 120 cc)
DISCUSSION
Sinistral portal hypertension is a rare, less than 1%, but life threatening cause of upper gastric bleeding [1, 2,3]. It is commonly caused by an occlusive thrombus in the splenic vein which could lead to formation of lieno(spleno)-gastric varices in order to decompress increased pressure in the splenic vein [1]. Due to its low incidence, it is likely that most cases of sinistral hypertension are initially misdiagnosed as a generalized portal hypertension. In fact, the name sinistral portal hypertension is a misnomer since portal pressure is usually within the normal range in these cases [1,3]. Other synonymous terminologies referring to sisnistral portal hypertension are left sided portal hypertension, segmental, regional, localized, compartmental, lineal, or splenoportal hypertension [3].
Sinistral portal hypertension can prove difficult to distinguish from generalized portal hypertension as the presence of varices is commonly suggestive of a liver etiology. However, it is important to differentiate between sinistral and generalized/mesenteric portal hypertension since the optimal management of each disease process is quite different. Treatment options for refractory haemorrhage from varices in cirrhotic patients, specifically endoscopic clipping or TIPS, will have no benefit in sinistral hypertension [1,4]. There are several causes of sinistral portal hypertension presented in the literature with the majority of such cases due to a pathology in the pancreas [1,2]. While chronic pancreatitis is the most common cause, pancreatic pseudocysts, and various pancreatic neoplasms have all been reported as possible causes [1,2]. The relationship of the splenic vein to the pancreas makes it susceptible to occlusion/thrombosis in cases of pancreatic inflammation. Such occlusion causes back-pressure in the gastroepiploic veins which eventually leads to the formation of gastric varices. While gastric varices are common in both sinistral and mesenteric portal hypertension, one should suspect sinistral portal hypertension when such varices are only found in the gastric fundus, in absence of any evidence of liver function abnormalities or signs of liver cirrhosis, in conjunction with splenomegaly [1,2]. Iatrogenic splenic vein injury, ectopic spleen, colonic tumor infiltration, peri-renal abscess, post liver transplantation, Hodgkin’s disease, retropertoneal fibrosis, pancreatic transplantation, and spontaneous thrombus formation are among the less common causes of splenic vein thrombosis that can lead to left sided hypertension [1,2]. Although bleeding is the most severe and life-treating sequelae of sinistral portal hypertension, only a small proportion of people with splenic vein thrombosis experience variceal bleeding [5]. In a prospective study, 8% of patients with chronic pancreatitis experienced splenic vein thrombosis, the majority of whom did not experience any form of symptomatic GI bleeding [6]. Moreover, as evident in our patient, the incidence of sinistral portal hypertension does not correlate to the severity of pancreatitis and may be a result of a mild/subclinical episode of pancreatitis [7,8].
While diagnosis is mainly clinical and often made by exclusion of systemic portal hypertension, diagnostic imaging plays an important role in confirming the diagnosis in the majority of cases [3]. Although trans-abdominal ultrasonography (US) is often the initial imaging modality utilized, it is more helpful in excluding presence of systemic portal hypertension and its primary etiologies such as liver cirrhosis. The accuracy of trans-abdominal US is limited in detecting splenic vein thromboses which are smaller and more subtle than those of portal veins [9]. While endoscopic ultrasound (EUS), high resolution multi-detector contrast CT scan, magnetic resonance angiography (MRA) are all gaining popularity, angiography of splenic vein remains the gold standard in diagnosing sinistral portal hypertension [10–16]
The most common and recommended treatment option for symptomatic sinistral portal hypertension has been surgical correction of the primary cause in combination with splenectomy [7,17]. Less invasive endovascular treatments such as splenic artery embolization [1, 4] and trans hepatic splenic vein stent placement [4] have shown benefit in selective cases. Specifically, splenic artery embolization should be reserved in actively bleeding patients who are not medically fit for a splenectomy procedure [18,19]. While surgery has its well-known risks involved in any laparotomy, reported complications of the endovascular procedures have included partial gastric and/or pancreatic infarctions, and splenic abscess to name a few [4]. It is important to remember that the goal of splenic artery embolization is to achieve partial embolization with the objective of decreasing blood flow to the spleen while maintaining its immunological functionality [3]. If successful, partial embolization has been shown to reduce post-procedural complications of endovascular therapy [3].
Not all patients with sinistral portal hypertension would experience bleeding complications. Agarwal et al. reported that although 22% of patients with chronic pancreatitis, in their study, had imaging evidence of splenic vein thrombosis, only 15% of those presented with gastrointestinal bleeding [5]. Management of asymptomatic patients is more controversial than the symptomatic ones: splenectomy has been suggested as a prophylactic measure by some while others have not shown any significant benefit of this procedure in survival [3,5]. However, more evidence suggests that watchful waiting as acceptable course of management in asymptomatic individuals [20,21]. Although endovascular stenting of the portal vein has been used as a treatment for generalized portal hypertension, there has not been enough data to support the stenting of the splenic vein as a viable management of sinistral portal hypertension [3].
TEACHING POINT
Sinistral portal hypertension is caused by splenic vein thrombosis which is usually due to a pancreatic pathology. It is a rare cause of upper gastric bleeding but it is important to differentiate it from generalized portal hypertension. The management options for sinistral portal hypertension are different from those of generalized portal hypertension. The 2 main forms are management of left-sided portal hypertension are the following: a. Surgical (more common): Treating primary pathology and splenectomy and b. Endovasucular: Splenic artery emboliztion or splenic vein stenting.
Table 2.
Summary table for acute upper gastrointestinal bleed
| Etiology | Thrombosis of splenic vein |
| Incidence | <1% of causes of upper GI bleeds |
| Gender Ratio | No gender difference has been reported |
| Age prediction | No age prediction, however older age is associated with increased incidence of risk factors |
| Risk Factors |
Common: Chronic pancreatitis, pancreatic pseudocyst, pancreatic carcinoma Uncommon: Iatrogenic splenic vein injury, ectopic spleen, colonic tumor infiltration, peri-renal abscess, post liver transplantation, Hodgkin’s disease, retroperitoneal fibrosis, pancreatic transplantation, and spontaneous thrombus formation |
| Treatment | Splenectomy, splenic vein embolization, splenic vein recanulization and stent placement |
| Prognosis | Good if diagnosed and treated |
| Findings on imaging | Spleno-gastric varices, hilar streaking of spleen, signs of pancreatitis in the tail of pancreas |
Table 3.
Differential diagnosis table for acute upper gastrointestinal bleed
| CT-Scan | Angiography | |
|---|---|---|
| Sinistral Portal Hypertension |
|
|
| Systemic Portal Hypertension |
|
|
| Mallory-Weiss Syndrome | No abnormality seen | Extravasation of contrast from esophageal vein |
| Peptic Ulcer Disease | No abnormality seen | No abnormality seen |
ABBREVIATIONS
- AIDS
Acquired Immune Deficiency Syndrome
- CT
Computed Tomography
- EUS
Endoscopic ultrasonography
- GI
Gastro Intestinal
- HIV
Human Immunodeficiency Virus
- MRA
Magnetic resonance angiography
- TIPS
Transjugular Intra-hepatic Porto-systemic Shunt
- US
Ultrasound
REFERENCES
- 1.Thompson R, Taylor M, McKie L, Diamond T. Sinistral Portal Hypertension. Ulster Med J. 2006;75:175–177. [PMC free article] [PubMed] [Google Scholar]
- 2.Singhal D, Kakodkar R, Soin A, Gupta S, Nundy S. Sinistral Portal Hypertension. A Case Report. JOP. 2006;7(6):670–67. [PubMed] [Google Scholar]
- 3.Koklu S, Coban S, Yuksel O, Arhan M. Left-Sided Portal Hypertension. Dig Dis Sci. 2007;52:1141–1149. doi: 10.1007/s10620-006-9307-x. [DOI] [PubMed] [Google Scholar]
- 4.Cakamak O, Parildar M, Oran I, Sever A, Memis A. Sinistral Portal Hypertension; imaging findings and endovascular therapy. Abdom Imaging. 2006;30:208–213. doi: 10.1007/s00261-004-0231-2. [DOI] [PubMed] [Google Scholar]
- 5.Agarwal A, Kumar R, Agarwal S, Sing S. Significane of Splenic Vein Thrombosis in Chroinc Pancreatitis. Am J Surg. 2008;196:149–154. doi: 10.1016/j.amjsurg.2007.07.039. [DOI] [PubMed] [Google Scholar]
- 6.Adams DB, Mauterer DJ, Vujic IJ, Anderson MD. Preoperative control of splenic artery inflow in patients with splenic venous occlusion. South Med J. 1990;83:1021–1024. doi: 10.1097/00007611-199009000-00010. [DOI] [PubMed] [Google Scholar]
- 7.Sakorafas GH, Sarr MG, Farley DR, Farnell MB. The significance of sinistral portal hypertension complicating chronic pancreatitis. Am J Surg. 2000;179:129–133. doi: 10.1016/s0002-9610(00)00250-6. [DOI] [PubMed] [Google Scholar]
- 8.Little AG, Moossa AR. Gastrointestinal hemorrhage from left-sided portal hypertension. An unappreciated complication of pancreatitis. Am J Surg. 1981;141:153–158. doi: 10.1016/0002-9610(81)90029-5. [DOI] [PubMed] [Google Scholar]
- 9.Weber SM, Rikkers LF. Splenic vein thrombosis and gastrointestinal bleeding in chronic pancreatitis. World J Surg. 2003;27:1271–1274. doi: 10.1007/s00268-003-7247-6. [DOI] [PubMed] [Google Scholar]
- 10.Yale CE, Crummy AB. Splenic vein thrombosis and bleeding esophageal varices. JAMA. 1971;217:317–320. [PubMed] [Google Scholar]
- 11.Wiersema MJ, Kochman ML, Cramer HM, Tao LC, Wiersema LM. Endosonography-guided real-time fine needle aspiration biopsy. Gastrointest Endosc. 1994;40:700–707. [PubMed] [Google Scholar]
- 12.Lewis JD, Faigel DO, Morris JB, Siegelman ES, Kochman ML. Splenic vein thrombosis secondary to focal pancreatitis diagnosed by endoscopic sonography. J Clin Gastroenterol. 1998;26:54–56. doi: 10.1097/00004836-199801000-00014. [DOI] [PubMed] [Google Scholar]
- 13.Finn JP, Edelman RR, Jenkins RL, Lewis WD, Longmaid HE, Kane RA, Stokes KR, Mattle HP, Clouse ME. Liver transplantation: MR angiography with surgical validation. Radiology. 1991;179:265–269. doi: 10.1148/radiology.179.1.2006289. [DOI] [PubMed] [Google Scholar]
- 14.Erden A, Erden I, Yagmurlu B, Karayalçin S, Yurdaydin C, Karayalçin K. Portal venous system. Evaluation with contrast-enhanced 3D MR portography. J Clin Imag. 2003;27:101–105. doi: 10.1016/s0899-7071(02)00497-7. [DOI] [PubMed] [Google Scholar]
- 15.Lin J, Zhou KR, Chen ZW, Wang JH, Yan ZP, Wang YX. 3D contrast-enhanced MR portography and direct X-ray portography: a correlation study. Eur Radiol. 2003;13:1277–1285. doi: 10.1007/s00330-002-1645-2. [DOI] [PubMed] [Google Scholar]
- 16.Kreft B, Strunk H, Flacke S, Wolff M, Conrad R, Gieseke J, Pauleit D, Bachmann R, Hirner A, Schild HH. Detection of thrombosis in the portal venous system: comparison of contrast-enhanced MR angiography with intraarterial digital substraction angiography. Radiology. 2000;216:88–92. doi: 10.1148/radiology.216.1.r00jl2386. [DOI] [PubMed] [Google Scholar]
- 17.Thavanathan J, Heughan C, Cummings TM. Splenic vein thrombosis as a cause of variceal bleeding. Can J Surg. 1992;35:649–652. [PubMed] [Google Scholar]
- 18.Evans GRD, Yellin AE, Weaver FA, Stain SC. Sinistral (left-sided) portal hypertension. Am Surg. 1990;56:758–763. [PubMed] [Google Scholar]
- 19.Moossa AR, Gadd MA. Isolated splenic vein thrombosis. World J Surg. 1985;9:384–390. doi: 10.1007/BF01655272. [DOI] [PubMed] [Google Scholar]
- 20.Heider TR, Azeem S, Galanko JA, Behrns KE. The natural history of pancreatitis-induced splenic vein thrombosis. Ann Surg. 2004;239:876–882. doi: 10.1097/01.sla.0000128685.74686.1e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Loftus JP, Nagorney DM, Ilstrup D, Kunselman AR. Sinistral portal hypertension. Splenectomy or expectant management. Ann Surg. 1993;217:35–40. doi: 10.1097/00000658-199301000-00007. [DOI] [PMC free article] [PubMed] [Google Scholar]