Abstract
Unilateral pulmonary artery agenesis is commonly seen associated with other congenital cardiovascular defects, when it is detected early in life, but isolated absence of the pulmonary artery is a rare entity, usually detected in adulthood. The latter patients are usually asymptomatic or might present with varied non-specific manifestations such as respiratory tract infections and hemoptysis. This report describes the imaging findings of a 67 year old female with absence of the right pulmonary artery. The embryology and clinical manifestations of the condition are reviewed.
Keywords: Pulmonary artery agenesis, embryology, contracted hyperlucent hemithorax
CASE REPORT
A 67 year old female presented to the out-patient department with non-exertional and intermittent chest pain for two months. Clinical examination of the respiratory and cardiovascular systems was normal. Electrocardiography was normal. Chest radiograph (Fig 1) showed a contracted right hemithorax with ipsilaterally shifted mediastinal structures and elevated right hemidiaphragm. The left pulmonary artery appeared prominent. With the differential diagnosis including lobar collapse, Swyer-James syndrome and right pulmonary artery hypoplasia/agenesis, computed tomography (CT) of the thorax with CT pulmonary angiography and Magnetic Resonance imaging (MRI) were performed. The right pulmonary artery was found to be absent, with the main pulmonary artery continuing as the left pulmonary artery (Fig 2) and the right heart chambers were seen to be of normal size (Fig 3), suggesting absence of pulmonary hypertension. Findings were confirmed on coronal reformats (Fig 4) and volume rendered images (Fig 5, 6). The pulmonary vasculature on the right side was grossly reduced while the left pulmonary veins and arteries were enlarged (Fig 5, 6). The right lung was hypoplastic with compensatory hyperinflation of the left lung (Fig 7, 8, 9). Prominent collaterals were seen in both modalities to arise from the descending thoracic aorta and supply the right lung (Fig 10). Transthoracic echocardiography confirmed absence of pulmonary hypertension, intracardiac shunts or structural heart defects. This is, as far as the authors’ knowledge, the oldest patient in whom this condition has been described. The patient’s symptoms resolved without treatment and she is presently healthy and on follow up.
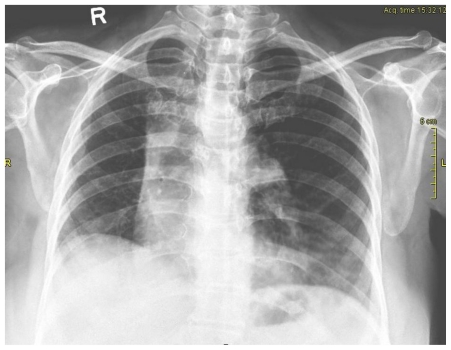
Figure 1.
67 year old female with absent right pulmonary artery. Chest radiograph shows a contracted right hemithorax with diminished vasculature, mediastinum shifted to the right and an elevated right hemidiaphragm.
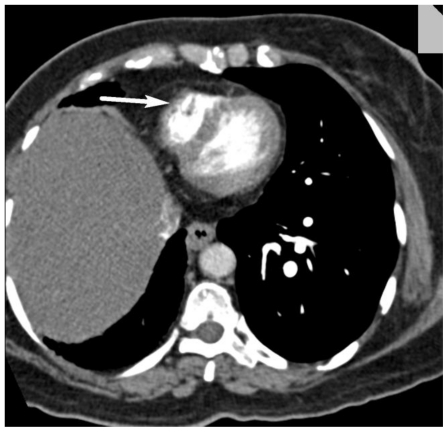
Figure 2.
67 year old female with absent right pulmonary artery. Axial section of a CT angiogram shows continuation of the main pulmonary artery as the left pulmonary artery (arrow) without a right pulmonary artery. (120 kV, 250 mAs, 5mm sections, 70ml of iohexol contrast agent).
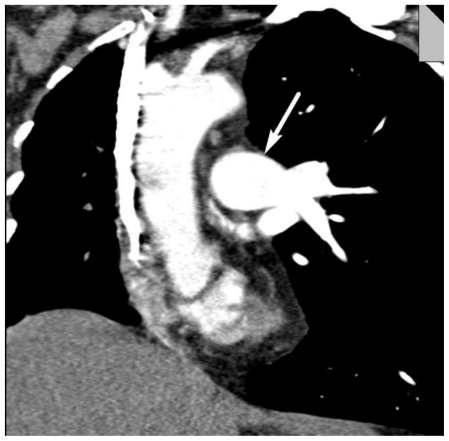
Figure 3.
67 year old female with absent right pulmonary artery. Axial section of a CT angiogram shows a normal-sized right ventricle (arrow) due to normal pulmonary arterial pressure (120 kV, 250 mAs, 5mm sections, 70ml of iohexol contrast agent).
Figure 4.
67 year old female with absent right pulmonary artery. Coronal reformatted section of a CT angiogram shows left pulmonary artery (arrow) without right pulmonary artery. (120 kV, 250 mAs, 5mm sections, 70ml of iohexol contrast agent).
Figure 5.
67 year old female with absent right pulmonary artery. Volume rendered image showing the main pulmonary artery continuing as the left pulmonary artery. An arrow marks the expected position of the absent right pulmonary artery. Large pulmonary vessels (arteries and veins) are seen in the left lung but none on the right.
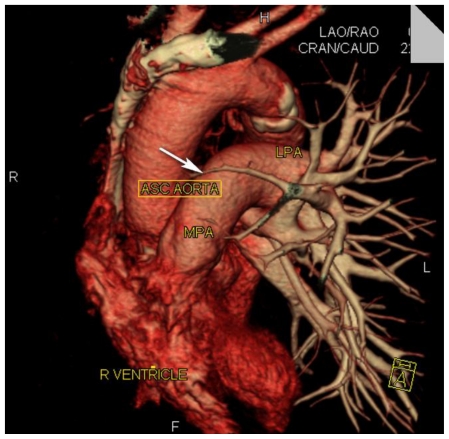
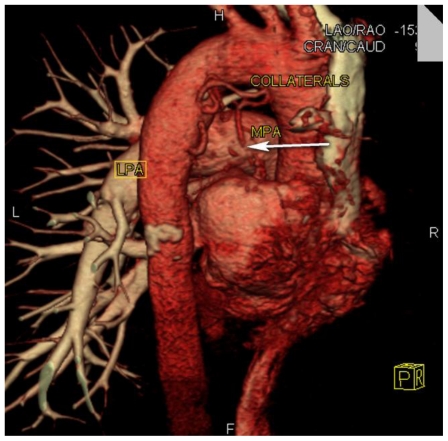
Figure 6.
67 year old female with absent right pulmonary artery. Volume rendered image (right posterior view) showing the main pulmonary artery (MPA) and left pulmonary artery (LPA) but no vessel at the expected site of the right pulmonary artery (arrow). Collaterals from the descending thoracic aorta are also marked.
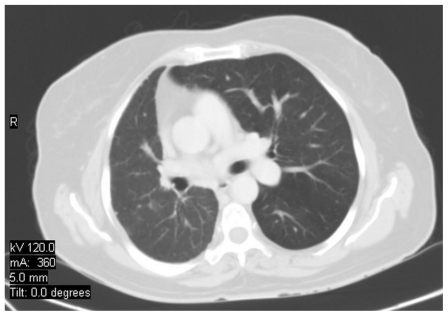
Figure 7.
67 year old female with absent right pulmonary artery. Axial section of a CT with lung windows shows a hypoplastic right lung with increased attenuation and smaller vasculature. (120 kV, 360 mAs, 5mm sections, 70ml of iohexol contrast agent).
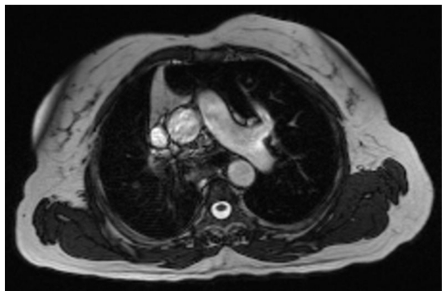
Figure 8.
67 year old female with absent right pulmonary artery. Axial trufisp MRI image obtained using a 1.5 Tesla magnet (TR 3.57, TE 1.51, 4 mm slices, no contrast) shows the left pulmonary artery and its branches, but no right pulmonary artery.
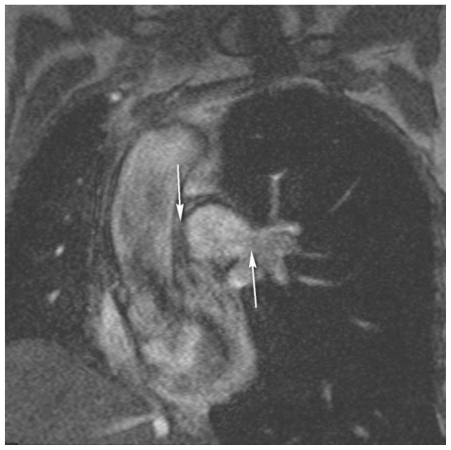
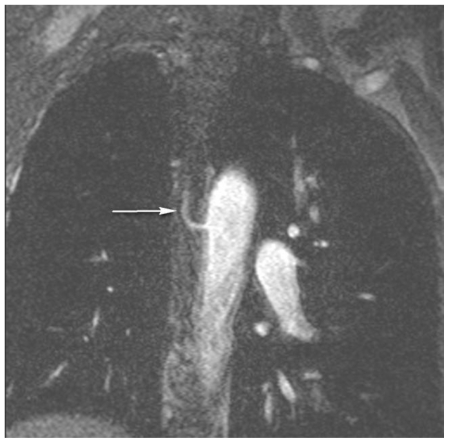
Figure 9.
67 year old female with absent right pulmonary artery. Coronal turboflash MRI image obtained using a 1.5 Tesla magnet (TR 3.35, TE 1460, 4.5 mm slices, no contrast) shows the left pulmonary artery and its branches (lower arrow), but no right pulmonary artery (upper arrow). Note also the reduced volume of the right lung and its diminished vasculature.
Figure 10.
67 year old female with absent right pulmonary artery. Coronal turboflash MRI image obtained using a 1.5 Tesla magnet (TR 3.47, TE 1460, 2.5 mm slices, no contrast) shows a large intercostal artery (arrow) which was arising from the descending thoracic aorta and was followed into the right lung hilum.
DISCUSSION
The first reported case of unilateral absence of the pulmonary artery (UPAA) was published in 1868 [1]. The prevalence of this disorder is estimated to be 1 in 300,000 [2]. The condition is commonly associated with congenital heart disease, when it is detected in infancy. The most common associations [3] include Tetralogy of Fallot and septal defects, and UPAA has also been reported with coarctation of aorta, subvalvular aortic stenosis, persistent ductus arteriosus, aortopulmonary window and transposition of the great arteries. When associated with these conditions, the left pulmonary artery is more often absent and the patient presents in infancy [4]. Isolated UPAA is much more uncommon [2], and about 110 cases of isolated UPAA have been reported so far. Patients present at a later age group with a median age of 14 years [3]. Common presentations include shortness of breath, recurrent pulmonary infections and hemoptysis [1,3], though several patients are asymptomatic. Most cases are detected on an abnormal chest radiograph. However, some patients with isolated UPAA have been known to present with severe pulmonary artery hypertension, pulmonary hemorrhage, heart failure and high altitude pulmonary edema (HAPE) [5]. Isolated UPAA more commonly affects the right pulmonary artery [2].
The embryologic explanation for the origin of the absent pulmonary artery is believed to be as follows [6]. The intrapulmonary pulmonary arteries arise from the lung buds and the extrapulmonary pulmonary arteries arise from the proximal portion of the sixth aortic arch. The main pulmonary artery is derived from the truncoaortic sac. The ductus arteriosus, which forms from the distal portion of the sixth arches, connects to the primitive dorsal aorta, which becomes the underside of the aortic arch ipsilateral to the arch or the base of the innominate artery contralateral to the arch. An absent pulmonary artery is caused by the involution of the proximal sixth aortic arch and persistence of the connection of the intrapulmonary pulmonary artery to the distal sixth aortic arch. It has been pointed out that all reported cases of absent pulmonary artery with satisfactory angiographic, surgical or autopsy documentation had a ductus arteriosus or ligamentum ipsilateral to the absent pulmonary artery [7]. The preferred terms for this condition have thus been suggested to be ‘pulmonary artery proximal interruption’ [5] or ‘nonconfluent pulmonary artery’ or ‘ductal origin of the distal pulmonary artery’ [8].
If the ductus arteriosus closes after birth, the ipsilateral intrapulmonary pulmonary artery will lose its source of blood supply, diminish in size, and thus not be visible with imaging [7]. Collaterals to the affected lung usually arise from bronchial arteries [2], but have also been documented to arise from intercostal, subdiaphragmatic, subclavian [3] and even coronary arteries [9]. The cases which present with hemoptysis are thought to be due to the high arterial pressure in the collaterals from bronchial arterioles and venules [10].
The isolated UPAA is often detected on a routine chest radiograph. Findings include a contracted hyperlucent hemithorax with a mediastinal shift to the affected side and elevation of the diaphragm, small hilum and pulmonary vasculature and contralateral hyperinflation [3]. The differentials include Swyer-James syndrome, lobar atelectasis, post lobectomy status, chronic pulmonary thromboembolism, pulmonary agenesis/hypoplasia complex and agenesis/hypoplasia of the pulmonary artery. Ventilation-perfusion scans show decreased ventilation and absent perfusion on the affected side. Other diagnostic tests include echocardiography, pulmonary angiography, CT and MRI. Pulmonary venous wedge angiography is particularly useful in delineating the presence of an ipsilateral hilar pulmonary artery and intrapulmonary vessels, which is required before revascularization [1]. Cases without pulmonary hypertension can be followed with echocardiography to detect early signs of the same.
There is no consensus regarding the treatment of isolated UPAA. While there are those that believe in treating only in the presence or symptoms or pulmonary arterial hypertension, others have advocated an early search for the occult pulmonary artery in all patients followed by a staged repair to restore the physiological pulmonary circulation and lung development and cause regression of pulmonary hypertension [1,7,11].
The surgical approaches [7] have been either the creation of an aortopulmonary shunt or connection of the affected pulmonary artery to the main pulmonary artery. Treatment options for massive hemoptysis and intractable life-threatening pulmonary infections include pneumonectomy and lobectomy; selective embolization of hypertrophied bronchial arteries may control hemoptysis successfully. Medical management includes treating pulmonary hypertension with diuretic agents, digoxin, intravenous prostacyclin or endothelin receptor antagonist bosentan [1].
In conclusion, it is important to be aware of the radiological appearances of UPAA, and have a high index of suspicion even in an asymptomatic patient as there is a risk of increasing pulmonary arterial hypertension, recurrent infections, hemoptysis and HAPE. When UPAA is suspected on a chest radiograph, performing a CT angiography would be the appropriate next step to confirm or rule out the diagnosis.
TEACHING POINT
Isolated absence of the pulmonary artery is a rare anomaly which is usually not detected till adulthood due to lack of or non-specific symptoms. This entity should be included in the differential of a chest radiograph with a contracted hyperlucent hemithorax.
Table 1.
Summary table for unilateral pulmonary artery agenesis
| Etiology | Involution of the proximal sixth aortic arch during embryogenesis. |
| Incidence | 1: 300,000. |
| Gender ratio | None. |
| Age predilection | Infancy (when other associated defects present). Adulthood (when isolated). |
| Risk factors | None known. |
| Treatment |
|
| Prognosis |
|
Table 2.
Differential diagnosis table of unilateral pulmonary artery agenesis
| CXR | CT | MRI | V/Q Scan | Angiography | |
|---|---|---|---|---|---|
| Pulmonary artery agenesis |
|
|
|
|
|
| Swyer-James syndrome |
|
Air-trapping with reduced vascularity | ‘Pruned-tree’ appearance of ipsilateral pulmonary vasculature | Reduced or normal perfusion and markedly reduced ventilation in the affected segments |
|
| Chronic pulmonary thrombo embolism |
|
|
Findings and measurement of pulmonary hypertension | Abnormal perfusion scan with normal ventilation | Large central pulmonary arteries with marked peripheral tapering |
| Congenital pulmonary hypoplasia |
|
|
|
Perfusion defects and reduced or normal ventilation | Patent but hypoplastic pulmonary artery |
ABBREVIATIONS
- UPAA
Unilateral Pulmonary Artery Agenesis
- MRI
Magnetic Resonance Imaging
- CT
Computed Tomography
- HAPE
High Altitude Pulmonary Edema
REFERENCES
- 1.Shostak E, Sarwar A. A 50-year-old woman with dyspnea, lower extremity edema, and volume loss of the right hemithorax. Chest. 2009 Aug;136(2):628–32. doi: 10.1378/chest.09-0080. [DOI] [PubMed] [Google Scholar]
- 2.Kadir IS, Thekudan J, Dheodar A, Jones MT, Carroll KB. Congenital unilateral pulmonary artery agenesis and aspergilloma. Ann Thorac Surg. 2002 Dec;74(6):2169–71. doi: 10.1016/s0003-4975(02)03979-6. [DOI] [PubMed] [Google Scholar]
- 3.Ten Harkel AD, Blom NA, Ottenkamp J. Isolated unilateral absence of a pulmonary artery: a case report and review of the literature. Chest. 2002 Oct;122(4):1471–7. doi: 10.1378/chest.122.4.1471. [DOI] [PubMed] [Google Scholar]
- 4.Bouros D, Pare P, Panagou P, Tsintiris K, Siafakas N. The varied manifestation of pulmonary artery agenesis in adulthood. Chest. 1995 Sep;108(3):670–6. doi: 10.1378/chest.108.3.670. [DOI] [PubMed] [Google Scholar]
- 5.Nana-Sinkam P, Bost TW, Sippel JM. Unilateral pulmonary edema in a 29-year-old man visiting high altitude. Chest. 2002 Dec;122(6):2230–3. doi: 10.1378/chest.122.6.2230. [DOI] [PubMed] [Google Scholar]
- 6.Apostolopoulou SC, Kelekis NL, Brountzos EN, Rammos S, Kelekis DA. “Absent” pulmonary artery in one adult and five pediatric patients: imaging, embryology, and therapeutic implications”. AJR Am J Roentgenol. 2002 Nov;179(5):1253–60. doi: 10.2214/ajr.179.5.1791253. [DOI] [PubMed] [Google Scholar]
- 7.Welch K, Hanley F, Johnston T, Cailes C, Shah MJ. Isolated unilateral absence of right proximal pulmonary artery: surgical repair and follow-up. Ann Thorac Surg. 2005 Apr;79(4):1399–402. doi: 10.1016/j.athoracsur.2003.10.037. [DOI] [PubMed] [Google Scholar]
- 8.Turner DR, Vincent JA, Epstein ML. Isolated right pulmonary artery discontinuity. Images Paediatr Cardiol. 2000;4(4):24–30. [PMC free article] [PubMed] [Google Scholar]
- 9.Gupta K, Livesay JJ, Lufschanowski R. Absent right pulmonary artery with coronary collaterals supplying the affected lung. Circulation. 2001 Jul 24;104(4):E12–E13. doi: 10.1161/hc2901.093602. [DOI] [PubMed] [Google Scholar]
- 10.Rousou AJ, Tetenta S, Boffa DJ. Pulmonary artery agenesis and Kommerell’s diverticulum presenting with hemoptysis. Eur J Cardiothorac Surg. 2009 Feb;35(2):370–2. doi: 10.1016/j.ejcts.2008.10.053. [DOI] [PubMed] [Google Scholar]
- 11.Toews WH, Pappas G. Surgical management of absent right pulmonary artery with associated pulmonary hypertension. Chest. 1983 Oct;84(4):497–9. doi: 10.1378/chest.84.4.497. [DOI] [PubMed] [Google Scholar]