Abstract
A 36-year-old female presented with constant, worsening left lower quadrant pain without associated fever or vaginal discharge. Pelvic and transvaginal ultrasound examinations were performed which demonstrated a large complex cystic structure in the left adnexa with peripheral flow on color Doppler imaging. Given the sonographic appearance and patient symptoms, possibilities included endometrioma or hemorrhagic cyst. Tubo-ovarian abscess (TOA) and other cystic ovarian masses were considered less likely. Two days later, the patient returned with severe pelvic pain as well as fever and leukocytosis. Follow-up ultrasound showed enlargement of the mass and a tubo-ovarian abscess (TOA) was suspected. Ultrasound-guided transvaginal abscess drainage was performed with removal of purulent fluid. The case demonstrates that the radiological features of TOA may mimic those of adnexal cystic masses such as an endometrioma or hemorrhagic cyst. A complementary case is also included which demonstrates similar sonographic findings in a patient with endometrioma. In addition to sonographic imaging, a thorough clinical and laboratory evaluation is important in differentiating these entities. Furthermore, we provide a comprehensive discussion about imaging features of cystic ovarian mass on different imaging modalities.
Keywords: Tubo-ovarian, abscess, sebaceous dermoid, endometrioma
CASE REPORT
We present the case of a 36-year-old African American female, gravida 0, para 0, with no significant medical or surgical history who presented to the outpatient clinic due to constant, worsening left lower quadrant pain that started several days before presentation. The patient was afebrile and did not get any blood test at that time, but was referred for diagnostic ultrasound examination of the pelvis.
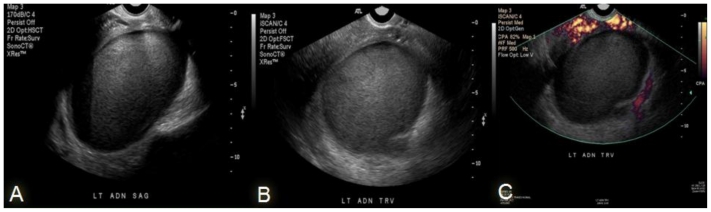
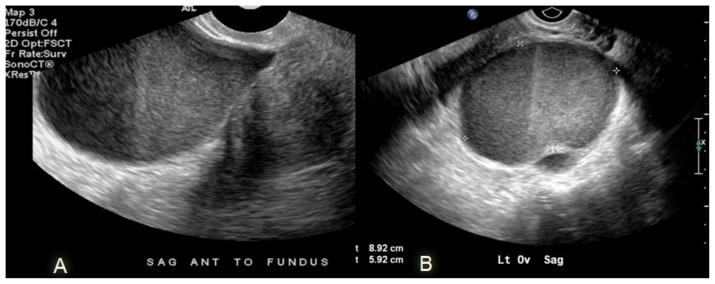
Initial pelvic and transvaginal sonographic evaluation showed a large unilocular complex cystic structure within the left adnexa measuring 8.9 × 8.0 × 5.9 cm that demonstrated homogenous low-level internal echoes, a fluid-fluid level and smooth walls. Color Doppler imaging demonstrated vascular flow in the periphery of the cystic mass, therefore ovarian torsion with internal hemorrhage was felt to be unlikely. There was no evidence of internal echogenic focus or calcifications (Fig. 1).
Figure 1.
36-year-old female with tubo-ovarian abscess, initial visit. The transvaginal ultrasound images (Philips C 8-4 MHZ transducer) showing a complex left adnexal cystic structure demonstrating homogenous internal debris and fluid-fluid level (a), without significant hyperemia on color Doppler. This was thought to represent an endometrioma or a dermoid cyst (b).
Given the sonographic appearance listed above and the patient s symptoms, possibilities included endometrioma, hemorrhagic cyst or dermoid cyst. Tubo-ovarian abscess (TOA) and other cystic ovarian masses were considered less likely.
The patient was given pain medication and was advised to return if the pain persisted or increased. The patient did experience severe increasing pelvic pain and presented to the emergency department (ED) for reevaluation two days later. At this time she was noted to have fever of 103 degrees F and an elevated white blood count of 25,000 cells/mcL.
Pelvic examination was performed revealing a palpable left adnexal mass with tenderness to palpation. Minimal cervical discharge was noted. The patient denied sexually transmitted disease or prior pelvic inflammatory diseases and reported being in a monogamous relationship. Cultures from the cervix for gonorrhea and chlamydia were negative.
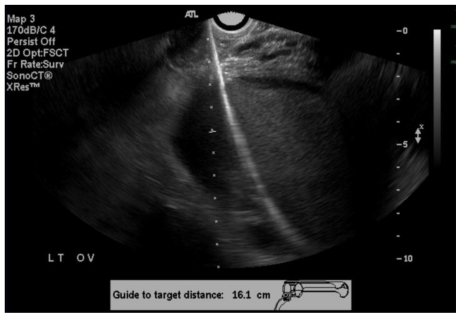
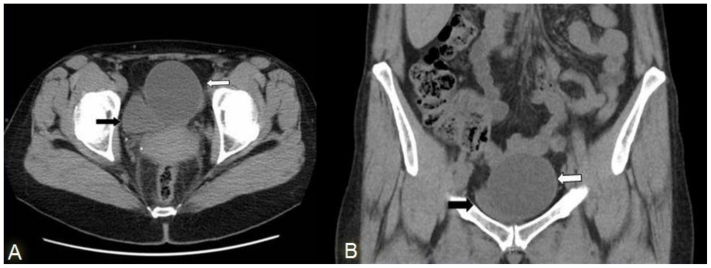
Follow up pelvic and transvaginal ultrasound examinations revealed an increase in the size of the complex adnexal cystic structure with internal debris, fluid-fluid level, hyperechoic thick walls and increased posterior acoustic enhancement, measuring 12.0 × 7.0 × 9.9 cm overall (Fig. 2). In view of the fever, worsening pain and leukocytosis, the adnexal cystic mass was now considered highly suspicious for a TOA. A contrast-enhanced computed tomography scan (CT) was performed to exclude additional underlying pathology and to evaluate the extend of the disease. Contrast-enhanced CT demonstrated a large, thick-walled left adnexal mass with central low attenuation as well as several adjacent tubular structures with central low attenuation. Soft tissue density stranding was also seen in the adjacent left hemipelvis. The mass was slightly displacing several loops of bowel laterally and the uterus inferiorly and to the right (Fig. 3). As no suspicious underlying pathology was identified, the TOA was considered primary.
Figure 2.
36-year-old female with left adnexa cystic mass, follow-up visit. The transvaginal ultrasound (HDI 5000 C 8-4 MHZ transducer) showing increase in the size of the previously noted complex left adnexal cystic structure demonstrating internal debris, fluid-fluid level (a+b) and the Doppler interrogations reveling hyperemic thick walls (c). These findings are consistent with left tubo-ovarian abscess.
Figure 3.
36-year-old female with left TOA, follow-up visit. A coronal CT reconstruction of the abdomen and pelvis with oral and IV contrast during arterial phase shows a large left adnexal cystic mass (white arrow) with thickened enhancing walls and several low-density tubular appearing structures (curved white arrow) with surrounding soft tissue density in the left hemipelvis adjacent to the large mass, likely focal pyosalpingitis. The mass was displacing the uterus (curved black arrow) inferiorly and to the right. Black arrow = urinary bladder.
The patient was admitted and started on triple intravenous antibiotics therapy of ampicillin, gentamicin, and clindamycin.
Interventional radiology was consulted and ultrasound-guided drainage of the left adnexal collection was performed utilizing a transvaginal approach. Aspiration of approximately 300cc of purulent fluid was accomplished through the catheter, which was subsequently locked in place and connected to gravity drainage (Fig. 4).
Figure 4.
36-year-old female with left tubo-ovarian abscess. The ultrasound-guided drainage of the left adnexal fluid collection was undertaken utilizing a transvaginal approach. Aspiration of approximately 300 cc of a purulent fluid was accomplished. The catheter was locked in place and connected to gravity drainage.
The fluid culture showed many colonies of beta hemolytic streptococci. Blood cultures and urine cultures were all negative. The patient was hospitalized for 7 days with her pain subsiding gradually. The patient remained afebrile and her white count slowly normalized. The drainage output diminished significantly. In such cases we follow up patient with a pelvic and transvaginal ultrasound. However, knowing that the prior CT of the pelvis gave us better information of the structures surrounding the TOA such was the pyosalpinx, a post drainage noncontrast CT scan of pelvis was performed for evaluation of catheter position and also to re-evaluate for remaining fluid collection. The CT scan showed no significant remaining fluid collection in the left adnexal region. The catheter was removed and she was discharged to home on oral antibiotics of amoxacillin clavulonate and metronidazole. Complementary case:
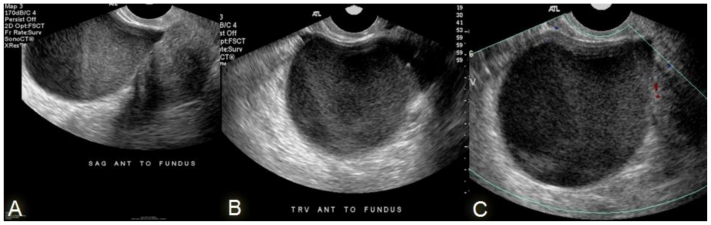
A 47 year-old female presented to ED with acute onset of left flank pain that was felt to be suspicious for a renal stone. The patient was afebrile and had a normal white blood count. A non-contrast CT scan of abdomen and pelvis using renal stone protocol was performed which showed a left renal calculus as well as an incidental low-attenuation left adnexal mass (Fig. 5 and Fig. 6). To better evaluate the pelvic mass dedicated pelvic and transvaginal ultrasound examinations were performed. These examinations demonstrated a cystic structure in the left adnexal region with smooth walls filled with homogenous debris that showed fluid-fluid level. Based on the above sonographic findings and the patient s known history of endometriosis, the mass was most consistent with an endometrioma (Fig. 7). Comparing this adnexal mass side by side with the previously described mass/TOA, it seems they share similar sonographic findings (Fig. 8).
Figure 5.
Complementary case. 47 year-old female comes to the ED with left flank pain. An axial and a reconstructed coronal image from a noncontrast CT image of the pelvis demonstrating a rounded hypodense structure in the left adnexal region (white arrow) displacing the bladder laterally (black arrow), with attenuation values greater than simple fluid and smooth thin walls. This finding was suspicious for an endometrioma versus a hemorrhagic ovarian cyst and turned out to be an endometrioma.
Figure 6.
Complementary case. 47 year-old female comes to the ED with left flank pain. A reconstructed sagital image from a noncontrast CT image demonstrating a rounded hypodense structure in the left adnexal region (white arrow) displacing the bladder inferiorly (black arrow), with attenuation values greater than simple fluid and smooth thin walls. The curved arrow demonstrated the uterus. The finding was suspicious for an endometrioma versus a hemorrhagic ovarian cyst and turned out to be an endometrioma.
Figure 7.
Complementary case. 47 years old female presented with incidental cystic adnexal mass identified on renal stone protocol CT. The transvaginal ultrasound demonstrated a large left adnexal cystic structure with smooth walls filled with debris and a fluid-fluid level and without hyperemia in the walls, favoring an endometrioma, which correlated with patient’s known history of endometriosis.
Figure 8.
Transvaginal sagital image (HDI 5000 C 8-4 MHZ transducer) of the complementary case (left) representing endometrioma and the transvaginal sagital image of the case report (right) representing an tubo-ovarian abscess. Both these structures demonstrate similar findings on gray scale ultrasound such as fluid-fluid level and homogenous internal echoes.
DISCUSSION
A Tubo-ovarian abscess (TOA) usually results as a complication of untreated or inadequately treated acute pelvic inflammatory disease. Though in our case the cultured organism was beta-hemolytic streptococcus, the causative infection is usually polymicrobial with a predominance of anaerobes (1).
The predominant theory on TOA formation relates to infections ascending in the fallopian tubes causing loss of normal mucosal configuration and peristalsis and swelling of the tubal wall. As inflammatory exudates such as pus and cellular debris accumulate within the tube, the patient can present with pyosalpingitis. The purulent secretions can “slide” out of the tube adjacent to the ovary, eventually creating a walled-off complex fluid collection known as a primary TOA (2).
A TOA can also arise from infectious or inflammatory processes of the adjacent pelvic structures such as the appendix, colon, and bladder or in association with a pelvic malignancy. When a TOA arises secondary to these processes, the term secondary TOA is used. These abscesses may demonstrate a thicker wall and are usually located further away from the adnexa (3). The management of primary and secondary TOA can be the same, except that the initiating disease process must also be addressed in the latter (4, 5).
Lower abdominal or pelvic pain is the most common presenting symptom and may be present for variable periods of time prior to diagnosis. The pelvic pain from TOA is usually constant and often worsening (as was seen in our patient), in contrast to that from endometriosis which is often cyclical and corresponds to the patient’s menstrual cycle. Additional symptoms of TOA include vaginal discharge (55%), irregular vaginal bleeding (36%), urinary symptoms (19%), nausea and vomiting (10%), and proctitis symptoms (7%) (6). About 20% of patients with TOA may be afebrile or have a normal leukocyte count, which represents a significant minority (7). On physical examination patients may show tenderness over the adnexal region with or without guarding or rebound.
Early recognition of a TOA is important in order to prevent the associated morbidity and mortality (8). Several imaging methods have been shown to be helpful in differentiating between a TOA and an endometrioma. These include contrast enhanced CT, magnetic resonance imaging (MR) and ultrasonography. In the end, a thorough history and physical examination is also a key in this challenging diagnosis.
Ultrasound (US) is the most commonly utilized imaging modality in cases of PID/TOA. Ultrasound examination of TOA usually will show a complex adnexal structure with thick walls and internal echoes likely pus with cellular debris. During the transvaginal examination patients may exhibit tenderness over the area of the fluid collection. The presence of air foci within adnexal mass has also been reported (9).
Although the sonographic appearance of an adnexal mass can be highly suggestive of a TOA, there is often an overlap of appearances with other entities including endometriosis, hemorrhagic cysts, dermoid cysts or other cystic ovarian masses. In our case the TOA presented initially as a large unilocular cystic mass with homogenous internal echoes and a fluid-fluid level. Comparing the index case with the subsequent companion case, the TOA demonstrated slightly thicker walls with increased vascular flow compared to the endometrioma. Even though there were minimal sonographic differences in these cases, such findings are often nonspecific. A diagnosis of TOA is difficult to make by sonography alone, and clinical and laboratory findings can play a key role in diagnosis. Despite this, about 20% of patients with TOA may be afebrile or have a normal leukocyte count (10, 11). Pain can also be vague or even absent in the chronic stage, which can further confound the diagnosis.
Endometriomas can have a variety of ultrasound appearances. While the “classic” endometrioma has been described as a homogeneous, hypoechoic focal lesion within the ovary, the majority of the endometriomas exhibit diffuse low-level internal echoes, multilocularity and hyperechoic foci in the wall (12).
Occasionally CT may be employed for further evaluation of an adnexal mass, however CT imaging is not specific in diagnosing TOA or endometriosis. Some CT characteristics that may be suggestive of TOA are that of a peripherally enhancing low-density pelvic mass with thick or irregular walls, anterior displacement of the round ligament, and especially satellite lesions adjacent to main mass, which may represent an adjacent fluid-filled fallopian tube or pyosalpinx (13). While non-specific, CT may be utilized for the evaluation of possible underlying inflammatory processes of the adjacent pelvic structures such as those involving the appendix, colon, and bladder or in association with a pelvic malignancy.
The MR appearance of TOA is described as a thick-walled adnexal mass with low signal intensity contents on T1-weighted images and high signal intensity on T2-weighted images. This appearance is variable however, and there are cases of TOA demonstrating intense or increased signal intensity on T1-weighted images, and some have heterogeneous signal intensity on T2-weighted images (14).
The signal intensity of content of the abscess can vary depending on its viscosity or protein concentration. A thin rim of high signal intensity in the innermost portion of the abscess on T1-weighted images is frequently found and represents a layer of granulation tissue with microscopic hemorrhage. The variable appearance of these lesions is thought to reflect the concentration of blood products (10).
The MR appearance of endometriosis is somewhat more specific with endometriomas typically demonstrating high signal intensity on T1-weighted images and “shading” or decrease of signal intensity within the mass on T2-weighted images (12).
Dermoid cyst, an adnexal cystic tumor, is composed of well -differentiated derivation from at least two of the three germ cell layers. It is considered the most common benign ovarian tumor of a female younger than 45 years of age (16).
The dermoid appearance may vary. Commonly, it would represent as a complex cystic structure with densely echogenic shadowing nodule, fluid-fluid level with the sebaceous/fat content layering above the fluid. In addition, calcified structure which resembles bone or tooth and/or multiple thin echogenic lines which are caused by the presence of hair in the cyst cavity are also seen.
Cases of predominately echogenic mass with intense posterior shadowing which obscures the posterior border known as the “tip of iceberg” sign are commonly reported.
The best diagnostic clue on CT and MR scan is the presence of the internal fat content which demonstrates increased signal intensity on TIW images and variable signal intensity on T2W. The drop of fat signal intensity on the TIW fat-suppressed images is diagnostic (16).
Furthermore, TOA and especially multiloculated TOA may also mimic an ovarian neoplasm which may represent on ultrasound as a complex cystic structure containing internal septations, debris and/or mural nodularities. CT images, in addition may show preservation of fat planes without inflammatory changes (Table 1).
Table 1.
Differential diagnosis of cystic ovarian masses.
| Clinical presentation | Lab | US | CT | MRI | |
|---|---|---|---|---|---|
| Hemorrhagic Cyst. | About 40%-acute pelvic pain which resolves within hours/days. | NL |
|
Vary.
|
|
| Endometriosis. | Cyclic pelvic pain which correspond with the menstrual cycle, Dispareunia. | NL |
|
Non specific
|
T1WFS-homogenous high signal T2WI- Loss of signal intensity (+shading). May show pelvic anatomical distortion. |
| TOA | Pelvic pain Fever, Leucocytosis | WBC increased |
|
|
|
| Dermoid | Pelvic pain/discomphort. | Normal. |
|
|
|
| Serous cyst Adenoma/adenocarcinoma | Pelvic pain/discomphort | CA125 may be increased but not specific* |
|
|
|
| Mucinous cyst Adenoma/adenocarcinoma | Pelvic pain/discomphort Or-incidental on pelvic exam. Abdominal distention secondary to metastatic spread of the disease. | CA125 may be increased but not specific* |
|
|
|
There is no diagnostic laboratory test for ovarian cystic masses such as mucinous/serous adenoma/adenocarcinoma. The CA 125 is an ovarian cell membrane antigen which is expressed by normal ovarian tissue and ovarian neoplasm. CA 125 is a non specific test and it is seen increased in different ovarian masses, non-ovarian conditions and even on a small percentage on a healthy population. Combinations of increased levels of CA 125 with suspicious sonographic findings are considered useful/nearly diagnostic in evaluating ovarian cystic masses.
Several cystic adnexal masses share the same sonographic characteristic that makes the ultrasound alone difficult to fully diagnose and differentiate these masses.
Tubo-ovarian abscess (TOA) is a complication of pelvic inflammatory disease requiring prompt diagnosis, admission, intravenous antibiotics and, possibly aspiration or surgery (15).
The radiological features of TOA may mimic those of benign ovarian tumors such as an endometrioma, hemorrhagic cyst, sebaceous dermoid or some malignant ovarian neoplases. In addition to sonographic imaging, a thorough history and clinical examination, as well as laboratory studies and other imaging modalities can play an important role in differentiating these entities.
In our index case the patient had an isolated pelvic ultrasound examination. Had she received additional clinical screening including CBC and possibly CT imaging, the diagnosis of the TOA might have been made earlier and would likely have made a difference in patient morbidity.
TEACHING POINT
The sonographic appearance of a tubo-ovarian abscess (TOA) can resemble and be mistaken for other cystic ovarian masses including an endometrioma or dermoid cyst. Ultrasound should be considered as a complementary examination technique used in conjunction with clinical and laboratory findings.
ABBREVIATIONS
- US
Ultrasound imaging
- CT
Computed Tomography
- MR
Magnetic Resonance
- PID
Pelvic Inflamatory Disease
- TOA
Tubo-ovarian abscess
- ED
Emergency Department
REFERENCES
- 1.Wilbur A, Aizenstein RI, Napp TE. CT findings in tuboovarian abscess. AJR Am J Roentgenol. 1992;158:575–579. doi: 10.2214/ajr.158.3.1738998. [DOI] [PubMed] [Google Scholar]
- 2.Callen PW. Ultrasound characteristics of pelvic inflammatory disease. Ultrasonography in obstetrics and genecology. (Fifth edition) 2008;30:974. [Google Scholar]
- 3.Potter AW, Chandrasekhar CA. US and CT Evaluation of Acute Pelvic Pain of Gynecologic Origin in Nonpregnant Premenopausal Patients. RadioGraphics. 2008;28:1645–1659. doi: 10.1148/rg.286085504. [DOI] [PubMed] [Google Scholar]
- 4.Protopapas AG, Diakomanolis ES, Milingos SD, et al. Tubo-ovarian abscesses in postmenopausal women: gynecological malignancy until proven otherwise? Eur J Obstet Gynecol Reprod Biol. 2004;114:203. doi: 10.1016/j.ejogrb.2003.10.032. [DOI] [PubMed] [Google Scholar]
- 5.Jackson SL, Soper DE. Pelvic inflammatory disease in the postmenopausal woman. Infect Dis Obstet Gynecol. 1999;7:248. doi: 10.1002/(SICI)1098-0997(1999)7:5<248::AID-IDOG8>3.0.CO;2-V. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Freij BJ. Acute pelvic inflammatory disease. Seminars in adolescent medicine. 1986 Jun;2(2):143–53. [PubMed] [Google Scholar]
- 7.Ha HK, Lim GY, Cha ES, et al. MR imaging of tubo-ovarian abscess. Acta Radiol. 1995;36:510–514. [PubMed] [Google Scholar]
- 8.Seshadri S, Kirwan J, Neal T. Perimenopausal pneumococcal tubo-ovarian abscess--a case report and review. Infect Dis Obstet Gynecol. 2004;12(1):27–30. doi: 10.1080/1064744042000210366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hochsztein JG, Koenigsberg M, Green DA. US case of the day. Actinomycotic pelvic abscess secondary to an IUD with involvement of the bladder, sigmoid colon, left ureter, liver, and upper abdominal wall. RadioGraphics. 1996;16:713–7. doi: 10.1148/radiographics.16.3.8897636. [DOI] [PubMed] [Google Scholar]
- 10.Kim SH, Kim SH, Yang DM, Kim KA. Unusual causes of tubo-ovarian abscess: CT and MR imaging findings. Radiographics. 2004 Nov-Dec;24(6):1575–89. doi: 10.1148/rg.246045016. [DOI] [PubMed] [Google Scholar]
- 11.Ha HK, Lim GY, Cha ES, et al. MR imaging of tubo-ovarian abscess. Acta Radiologica. 1995;36:510–514. [PubMed] [Google Scholar]
- 12.Woodward PJ, Sohaey R, Mezzetti TP., Jr Endometriosis: Radiologic-Pathologic Correlation. RadioGraphics. 2001;21:193–216. doi: 10.1148/radiographics.21.1.g01ja14193. [DOI] [PubMed] [Google Scholar]
- 13.Jeong WK, Kim Y, Song SY. Tubo-ovarian abscess: CT and pathological correlation. Clin Imaging. 2007 Nov-Dec;31(6):414–8. doi: 10.1016/j.clinimag.2007.04.024. [DOI] [PubMed] [Google Scholar]
- 14.Mudgil S. Pelvic Inflammatory Disease/Tubo-ovarian Abscess. EMedicine. Updated Aug 13, 2007. Available at: http://emedicine.medscape.com/article/404537-overview.
- 15.Adhikari S, Blaivas M, Lyon M. Role of bedside transvaginal ultrasonography in the diagnosis of tubo-ovarian abscess in the emergency department. Emerg Med. 2008 May;34(4):429–33. doi: 10.1016/j.jemermed.2007.05.057. [DOI] [PubMed] [Google Scholar]
- 16.Gynecology. Ovarian neoplasms. [Accessed January 6, 2010]. https://my.statdx.com/action/dx/master-outline-gyn-dx.