Abstract
Cleidocranial dysplasia (CCD), also known as Scheuthauer Marie-Sainton Syndrome, is a rare autosomal dominant inherited disorder, characterized by general retardation in bone ossification, hypoplastic clavicles and various craniofacial and dental abnormalities. Early diagnosis of CCD can be difficult, because the majority of craniofacial abnormalities become obvious only during adolescence. We present a rare case of CCD with neonatal manifestation and would like to promote the awareness of this rare disorder and the importance of early diagnosis.
Keywords: Cleidocranial dysplasia, CCD, Scheuthauer Marie-Sainton Syndrome, hypoplastic clavicle
CASE REPORT
A premature infant (36th week gestational age) was born to a 40-year-old mother (9 gravida, 8 para) who suffered from adiposity and insulin-dependent diabetes mellitus. The family history was otherwise unobtrusive. Initially after birth the child suffered from respiratory distress syndrome and continuous positive airway pressure (CPAP) breathing had to be applied. The first clinical examination revealed small cranial bones, big fontanelles and wide sutures upon palpation. The conventional radiograph of the thorax showed hypoplastic clavicles. The distance between the proximal metaphysis of the humerus and the ossified part of the socket of the scapula was extended on both sides. The transversal processes in the thoracic spine as well as parts of the vertebral bodies and laminae in the cervical spine weren’t ossified appropriately. The upper ribs showed an uprising course (figure 1). Ultrasound examination the following day confirmed the diagnosis of cleidocranial dysplasia (CCD). No clavicles were visible and there were large ossification defects in the skull (figure 2). The metaphyses and the socket of the shoulder and hip joints seemed to be far apart due to widening of the cartilaginous part (figure 3). A plain radiograph of the left hand revealed incomplete ossification of the distal phalanges, brachytelephalangy and deformed middle and distal phalanges (figure 4).
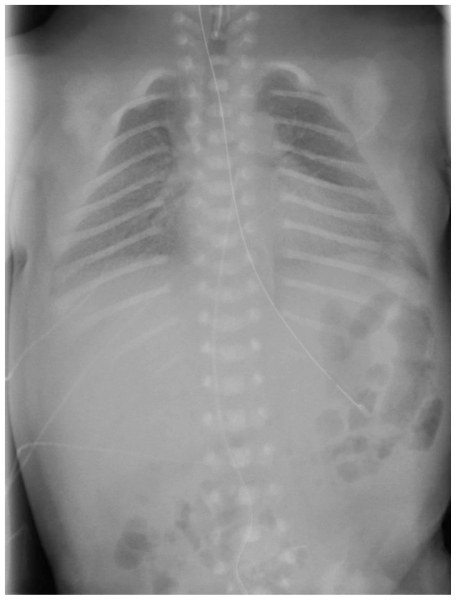
Figure 1.
Newborn infant with cleidocranial dysplasia causing respiratory distress syndrome. Anterior-posterior chest radiograph obtained 6 hours after birth. Bilateral lung opacities of reticulogranular texture and partial effacement of the cardiac and diaphragmatic contours, consistent with respiratory distress syndrome. Skeletal conspicuities include hypoplastic clavicles and an uprising course of the ribs.
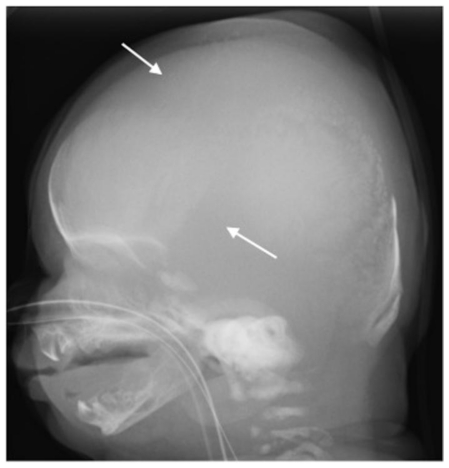
Figure 2.
Newborn infant with cleidocranial dysplasia causing respiratory distress syndrome. Lateral radiograph of the skull reveals large ossification defects (arrows).
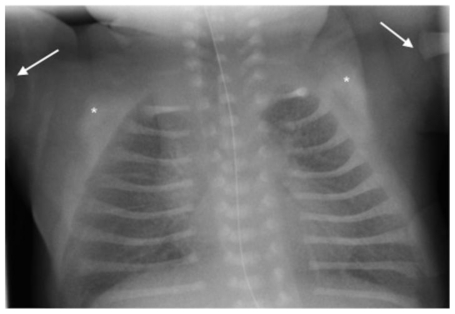
Figure 3.
Newborn infant with cleidocranial dysplasia causing respiratory distress syndrome. Magnified view of an anterior-posterior chest radiograph obtained approximately 8 hours after birth demonstrates an extended distance between the proximal metaphysis of the humerus (arrows) and the ossified part of the socket of the scapula (*) on both sides.
Figure 4.
Newborn infant with cleidocranial dysplasia causing respiratory distress syndrome. Plain dorso-palmar radiograph of the left hand shows incomplete ossification of the distal phalanges, brachytelephalangy and deformation of the middle and distal phalanges.
After symptomatic medical treatment for respiratory distress syndrome the child was released two weeks after birth in a good state of health. In the following course the mother presented the child again to the hospital about two months after birth and reported that the patient was choking on ingestion and suffered from episodes of apnea. Fluoroscopy was unobtrusive and revealed no reflux. Clinical examination revealed retrognathy, which could possibly be accounted for the eating and drinking problems.
DISCUSSION
CCD, also known as Scheuthauer Marie-Sainton Syndrome, is a rare autosomal dominant inherited disorder, characterized primarily by general retardation in bone ossification, hypoplastic clavicles and various craniofacial and dental abnormalities. Its incidence has been estimated to be 0.5/100 000 live births (1). There are rare cases on record of possible autosomal recessive inheritance (2). CCD shows a wide variability in expression, although usually complete penetrance (3). Early diagnosis of CCD can be difficult, because the majority of craniofacial abnormalities become obvious only during adolescence (4).
Most cases of CCD are diagnosed during childhood or adolescence. So far, there have been few reports of an early diagnosis or even neonatal cases revealing the whole characteristic of this skeletal dysplasia (5,6). In case of a positive family history, prenatal ultrasound can help establishing an early diagnosis by showing an abnormal growth of the clavicles (3) or for example hypomineralization of the skull bones (7). The fontanelles may remain open until adulthood but the sutures often close with interposition of wormian bones. More than 100 additional anomalies have been reported and because of the variable clinical expression the diagnosis of CCD can be misjudged even after careful assessment (8). Hypoplastic clavicles in association with further skeletal abnormalities are suggestive of CCD, but still have to be reviewed in context with other findings. Differential diagnoses include hypophosphatasia (perinatal and infantile forms), congenital pseudarthrosis of the clavicle, osteogenesis imperfecta congenita (type 1) and Yunis-Varon syndrome (7).
Cases of CCD can occur sporadically, but most are inherited. In the present case report no chromosome analysis was performed so that a possible underlying genetic cause cannot be ruled out. As none of the patient's eight siblings suffered from comparable symptoms, a sporadic occurrence is likely. Early diagnosis of CCD is not only important in order to initiate an early and adequate interdisciplinary treatment, but also in order to prevent early complications as for example respiratory distress. As the lifespan is not markedly shortened and in most cases no cerebral deficits are reported, prognosis mainly depends on prevention and early treatment of such complications. There is an associated morbidity due to respiratory insufficiency including the development of respiratory distress syndrome needing intensive care unit treatment due to chest deformity as demonstrated by the current report.
Treatment options cut down to symptomatic measures such as corrective dental and orthopedic surgery, depending on the extent of accompanying abnormalities. Cooper et al. (9) stated that medical evaluation for consequences of delayed craniofacial development should further include evaluation for obstructive sleep apnea, medical and surgical therapy for upper airway obstruction, and medical and surgical therapy for recurrent and chronic sinusitis and otitis.
As most reports focus on accompanying craniofacial and dental abnormalities, we would like to point out the possibility of respiratory distress and the need for an adequate and early treatment in newborn infants presenting with CCD. Especially the obstetrician and the paediatrician looking after the newborn as well as the radiologist reading the first exams have to be aware of this possible condition.
TEACHING POINT
Cleidocranial dysplasia (CCD) is a rare autosomal dominant inherited disorder, characterized primarily by general retardation in bone ossification, hypoplastic clavicles and various craniofacial and dental abnormalities. Even though most cases are diagnosed during childhood or adolescence, newborn infants may present with symptoms of respiratory distress due to chest deformity, needing intensive care unit treatment.
ABBREVIATIONS
- CCD
cleidocranial dysplasia
- CPAP
continuous positive airway pressure
REFERENCES
- 1.Taybi H, Lachman RS, editors. Radiology of Syndromes, Metabolic Disorders, and Skeletal Dysplasias. St Louis: Mosby; 1996. [Google Scholar]
- 2.Goodman RM, Tadmor R, Zaritsky A, Becker SA. Evidence for an autosomal recessive form of cleidocranial dysostosis. Clin Genet. 1975;8:20–29. doi: 10.1111/j.1399-0004.1975.tb01950.x. [DOI] [PubMed] [Google Scholar]
- 3.Stewart PA, Wallerstein R, Moran E, Lee MJ. Early prenatal ultrasound diagnosis of cleidocranial dysplasia. Ultrasound Obstet Gynecol. 2000;15:154–156. doi: 10.1046/j.1469-0705.2000.00041.x. [DOI] [PubMed] [Google Scholar]
- 4.Suba Z, Balaton G, Gyulai-Gaal S, Balaton P, Barabas J, Tarkan I. Cleidocranial dysplasia: diagnostic criteria and combined treatment. J Craniofac Surg. 2005;16:1122–1126. doi: 10.1097/01.scs.0000179747.75918.58. [DOI] [PubMed] [Google Scholar]
- 5.Tokuc G, Boran P, Boran BO. Cleidocranial dysplasia in a mother and her daughter within the scope of neurosurgery. Report of two cases. J Neurosurg. 2006;104:290–292. doi: 10.3171/ped.2006.104.4.290. [DOI] [PubMed] [Google Scholar]
- 6.Tan KL, Tan LK. Cleidocranial dysostosis in infancy. Pediatr Radiol. 1981;11:114–116. doi: 10.1007/BF00971793. [DOI] [PubMed] [Google Scholar]
- 7.Soto E, Richani K, Goncalves LF, Devers P, Espinoza J, Lee W, Treadwell MC, Romero R. Three-dimensional ultrasound in the prenatal diagnosis of cleidocranial dysplasia associated with B-cell immunodeficiency. Ultrasound Obstet Gynecol. 2006;27:574–579. doi: 10.1002/uog.2770. [DOI] [PubMed] [Google Scholar]
- 8.Cavalli P, Santorelli FM, Bontardelli M, Tessa A, Bosi A, Poggiani C. Prenatal exclusion of cleidocranial dysplasia. Prenat Diagn. 2003;23:945–946. doi: 10.1002/pd.718. [DOI] [PubMed] [Google Scholar]
- 9.Cooper SC, Flaitz CM, Johnston DA, Lee B, Hecht JT. A natural history of cleidocranial dysplasia. Am J Med Genet. 2001;104:1–6. doi: 10.1002/ajmg.10024. [DOI] [PubMed] [Google Scholar]