Abstract
Spontaneous visceral artery dissection is an uncommon event with an unpredictable natural history with superior mesenteric artery being the most common affected artery. It is most often asymptomatic and usually diagnosed at autopsy. Pre-disposing factors are not specific but have been suggested to be pre-existing vascular disease, hypertension and pregnancy. Spontaneous resolution, definitive occlusion of the artery, and formation of an aneurysm with associated complications are some other possible outcomes. Isolated dissection of the celiac artery (CA) is rare and there are only a few cases reported in the literature. We present a case of a 65 year old male with spontaneous celiac artery dissection and provide a review of the current literature about imaging findings and management of this entity.
Keywords: Celiac artery, dissection
CASE REPORT
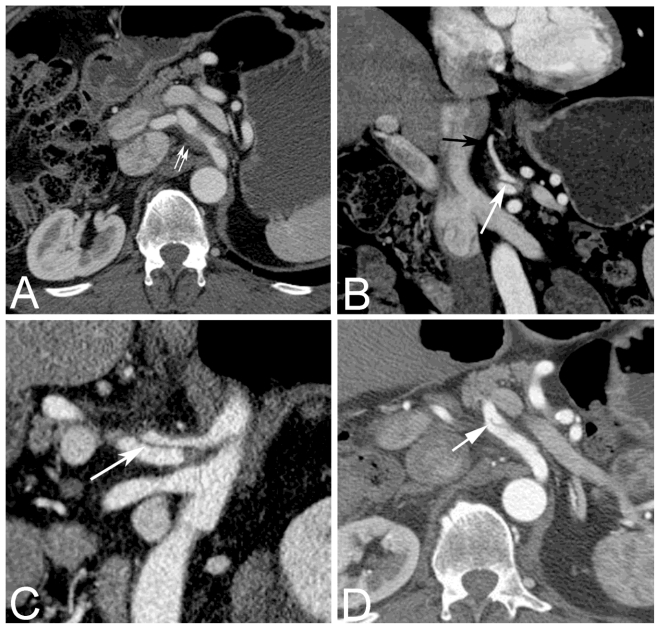
A 65-year-old previously healthy man had sudden onset of sharp burning epigastric abdominal pain, three days prior to presentation, which was non-radiating and intermittent in intensity ranging from mild to severe. The patient also developed some anorexia. He denied any vomiting, diarrhea, fevers, bright red blood per rectum, melena or rigors. The patient had no history of hypertension and his blood pressure was normal at presentation. On physical examination he was mildly tender to palpation in the epigastric region without guarding or rebound. His vital parameters were normal with a blood pressure of 126/70mmHg and heart rate of 76 bpm. A helical CT scan of the abdomen and pelvis with contrast (378mAs, 120 kVp, slice thickness 2.5 mm, 150 cc of Visipaque) in the portal venous phase (Figure 1) was performed which showed a focal dissection in the celiac artery, approximately 2.5 cm in length. There was associated fat stranding around the celiac artery and its proximal branches. The dissection began approximately 1.5 cm distal to the origin of the celiac artery, extended past the origin of the left gastric artery and into the bifurcation of the artery into the splenic and common hepatic artery. A small intramural thrombus was seen in the proximal part of the dissection. Both the false and true lumens were patent with contrast seen in the hepatic, left gastric and splenic arteries. The left gastric originated from the false lumen, the splenic artery from the true lumen and the hepatic artery from both. The aorta, superior mesenteric artery and its branches and inferior mesenteric artery and its branches were all normal. There were no vascular calcifications in the region of the celiac artery or its branches. The patient was treated conservatively with aspirin and follow up CT angiograms performed at six and 12 months (392 mAs, 120 kVp, slice thickness 1.25 mm, 150 cc of Visipaque) showed no change in the celiac artery dissection (Figure 1d); however the fatty infiltration around the celiac artery had decreased.
Figure 1.
65 year old male with celiac artery dissection. CT contrast enhanced images acquired on GE Lightspeed VCT, Milwaukee, (378 mAs, 120 kVp, 2.5mm slice thickness, 150 cc of Visipaque) A. axial, B. coronal reformat (slice thickness 5 mm) and C. sagittal oblique reformat reformat (slice thickness 5 mm) shows the dissection extending into the celiac artery (white arrow) best seen on the coronal and sagittal oblique reformats. Note the fat stranding around the celiac artery with a small intramural thrombus at the proximal aspect of the dissection (double arrows), and the left gastric artery is patent seen on the coronal reformat (black arrow). D. Image from an axial contrast enhanced CT (392 mAs, 120 kVp, slice thickness 1.25 mm, 150 cc of Visipaque)performed 12 months after the first CT with the same parameters shows decrease in the fat stranding around the celiac artery but stable appearance of the dissection (arrow).
DISCUSSION
Spontaneous dissection of visceral arteries was first described by Baurersfeld in 1947 (1). Spontaneous renal artery dissection has been reported in the literature more often than celiac artery dissection. Even with the larger number of cases of renal artery dissection reported, there are only about 200 cases reported in the literature (2). Isolated spontaneous celiac artery dissection is a rare entity with only 19 cases described in the literature on our search. Most of these cases were seen as spontaneous occurrence in young patients and were managed either surgically or by medical management. As per Fenoglio et al, isolated spontaneous celiac artery dissection is usually iatrogenic or secondary to atherosclerosis, trauma, pregnancy, fibromuscular dysplasia, inflammatory or infectious diseases, or congenital disorder of the vascular wall (3). Histology has shown that the dissection occurs between the intima and the external elastic layer, whereas in dissection of the aorta the cleavage plane is between the first and the second part of the intima (1).
Spontaneous arterial dissection is more common in males (5:1) with an average age of patients being approximately 55 years (4). The predisposing factors include hypertension, pre-existing vascular disease and pregnancy leading to weakening of the arterial wall (5). Other precipitating events are mechanical stretching and microtrauma caused by exertion or sudden abdominal hyperpressure (e.g., sneezing, lifting). Other reported risk factors include cystic medial necrosis, abdominal aortic aneurysm, fibromuscular dysplasia, trauma and connective tissue disorders (6). Most patients with celiac artery dissection are asymptomatic possibly due to the lack of small bowel involvement. Some patients may present with abdominal pain which may be due to simultaneous involvement of the splenic, renal or superior mesenteric arteries causing infarction and bowel ischemia. Patients with ruptured aneurysms present acutely with bleeding. Chronic dissection can present with symptoms of intestinal angina i.e. post-prandial abdominal pain and weight loss (6).
Contrast-enhanced CT/CTA is considered the primary technique for diagnosing celiac artery dissection; however, MR angiography, sonography, and conventional angiography also can be used (6). Celiac artery dissection can be accompanied by celiac artery aneurysm formation (7). Diagnostic imaging findings on CT according to Kim et al include an intimal flap, which is pathognomonic or eccentric mural thrombus in the celiac lumen, which should raise suspicion for dissection (8). Because the intimal flap is not always visible, mural thrombus may be the only clue to the presence of dissection (4, 8). Infiltration of the fat surrounding the celiac axis may be seen in acute spontaneous celiac artery dissection. This finding may be predictive of the acuity of dissection and predisposition toward extension of dissection into adjacent vessels as suggested by D’Ambrosio et al (4).
Treatment strategy for dissection includes limiting progression of the dissecting hematoma, controlling hypertension and administering anticoagulants to prevent thromboembolic complications. In addition, secondary antiplatelet therapy is advisable in patients with stenotic lesions to prevent thrombosis. Surgical treatment of celiac artery dissection is performed to prevent acute complications like aneurysm rupture, intestinal ischemia or to prevent chronic complications like stenosis. Surgical treatment options include resection of the dissected segment with anastomosis or bypass creation. In addition, surgery allows for biopsy of the affected artery which may be necessary to exclude vasculitis as the cause of dissection (6). The risk of bowel ischemia associated with celiac artery dissection is less than that associated with SMA dissection. According to Schievink et al, surgery and endovascular procedures maybe considered when a patient is hemodynamically unstable, has persistent abdominal pain, when medical therapy fails to control blood pressure, and when dissection is progressing (9). This can be assessed by follow up with imaging and since there are no set standards, in our case imaging was repeated by CT scan at 6 and 12 months. Endovascular management of celiac artery dissection has been infrequently reported, however endovascular stent placement or fenestration has been reported in spontaneous superior mesenteric artery dissection (10). To prevent thromboembolic complications, therapy with anticoagulant or antiplatelet agents for 3–6 months with a target INR of 2.0–3.0 with strict blood pressure control (3, 9) has been suggested. Medical treatment also may include antihypertensive drugs, anti-inflammatory drugs, steroids, in-addition to anticoagulants (4).
Spontaneous celiac artery dissection is rare, but the incidence may have been underestimated due to the varied presenting symptoms and outcomes. They are now more frequently reported as a result of the progress of imaging modalities, such as US, CT, and angiography. Clinicians must be aware of the possibility of spontaneous isolated dissection of the celiac artery in patients with postprandial abdominal pain. In most cases the cause of dissection is unknown (4). The optimal treatment has not been established but may involve simple surveillance, medical treatment and\or surgical\endovascular repair, depending on the clinical features.
TEACHING POINT
Spontaneous celiac artery dissection is rare, can present with intimal flap, mural thrombus or infiltration of fat around the artery and can be associated with complications like aneurysm formation or occlusion of the artery. Surgical or endovascular management is only necessary if patient is hemodynamically unstable, has persistent abdominal pain, when medical therapy fails to control blood pressure, and when dissection is progressing.
ABBREVIATIONS
- CA
celiac artery
- CT
computed tomography
- CTA
computed tomography angiography
- MR
magnetic resonance
- US
ultrasound
- SMA
superior mesenteric artery
REFERENCES
- 1.Bauersfeld S. Dissecting aneurysm of aorta: Presentation of 15 cases and review of current literature. Ann Intern Med. 1947;26:873–89. doi: 10.7326/0003-4819-26-6-873. [DOI] [PubMed] [Google Scholar]
- 2.Kanofsky J, Lepor H. Spontaneous renal artery dissection. Rev Urol. 2007;9(3):156–60. [PMC free article] [PubMed] [Google Scholar]
- 3.Fenoglio L, Allione A, Scalabrino E, et al. Spontaneous dissection of the celiac artery: a pitfall in the diagnosis of acute abdominal pain. Presentation of two cases. Dig Dis Sci. 2004;49(7–8):1223–7. doi: 10.1023/b:ddas.0000037816.57229.6f. [DOI] [PubMed] [Google Scholar]
- 4.D’Ambrosio N, Friedman B, Siegel D, Katz D, Newatia A, Hines J. Spontaneous isolated dissection of the celiac artery: CT findings in adults. AJR Am J Roentgenol. 2007;188(6):W506–11. doi: 10.2214/AJR.06.0315. [DOI] [PubMed] [Google Scholar]
- 5.Zeebregts CJ, Schepens MA, Hameeteman TM, Morshuis WJ, de la Riviere AB. Acute aortic dissection complicating pregnancy. Ann Thorac Surg. 1997;64(5):1345–8. doi: 10.1016/S0003-4975(97)00916-8. [DOI] [PubMed] [Google Scholar]
- 6.Glehen O, Feugier P, Aleksic Y, Delannoy P, Chevalier JM. Spontaneous dissection of the celiac artery. Ann Vasc Surg. 2001;15(6):687–92. doi: 10.1007/s10016-001-0012-0. [DOI] [PubMed] [Google Scholar]
- 7.Matsuo R, Ohta Y, Ohya Y, et al. Isolated dissection of the celiac artery--a case report. Angiology. 2000;51(7):603–7. doi: 10.1177/000331970005100710. [DOI] [PubMed] [Google Scholar]
- 8.Kim JH, Roh BS, Lee YH, Choi SS, So BJ. Isolated spontaneous dissection of the superior mesenteric artery: percutaneous stent placement in two patients. Korean J Radiol. 2004;5(2):134–8. doi: 10.3348/kjr.2004.5.2.134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Schievink WI. Spontaneous dissection of the carotid and vertebral arteries. N Engl J Med. 2001;344(12):898–906. doi: 10.1056/NEJM200103223441206. [DOI] [PubMed] [Google Scholar]
- 10.Gobble R, Brill E, Rockman C, et al. Endovascular treatment of spontaneous dissections of the superior mesenteric artery. J Vasc Surg. 2009;50(6):1326–32. doi: 10.1016/j.jvs.2009.07.019. [DOI] [PubMed] [Google Scholar]