Abstract
Metallosis and metal-induced synovitis are well-recognized complications of metal-backed polyethylene joint prostheses and have been frequently described in the orthopedic surgery literature; however, relatively fewer articles discussing the radiologic aspects of this complication have been published. To illustrate the importance of radiologic findings in the diagnosis and management of these patients, we present a case of metallosis and metal-induced synovitis complicating two revisions of a total knee arthroplasty, caused by polyethylene liner wear and dissociation of the polyethylene liner from the metal-backed patellar prosthesis. Specific attention is given to reviewing signs that aid in diagnosis, such as the “bubble sign,” “cloud sign,” and “metal-line signs.”
Keywords: Metallosis, metal-induced synovitis, total knee arthroplasty complications, polyethylene liner failure, periprosthetic osteolysis, bubble sign, metal-line sign, cloud sign
CASE REPORT
A 74 year-old man with rheumatoid arthritis was followed in the outpatient orthopedic clinic for a long history of left knee pain. The patient had undergone a left total knee arthroplasty (TKA) approximately 18 years earlier (performed at an outside institution with unknown specific hardware type), which remained functional for about 12 years, at which time a patellar polyethylene exchange revision was performed (in 1996). He did fairly well until 2006, when he developed worsening left knee pain and a sensation of left knee instability. Plain radiographs were obtained to evaluate his new complaints. These showed evidence of loosening of the tibial component with fracturing of the tibial plateau, as well as amorphous cloudy densities posterior to the knee and large areas of periprosthetic lucency (Fig. 1). For preoperative planning of a potential arthroplasty revision, a computed tomography (CT) was ordered by the orthopedic surgeon. This nicely demonstrated the lytic areas in close proximity to the tibial component, and their internal characteristics (Fig. 2). Scattered metallic debris fragments were also present (Figs. 1 and 2). The patient went on to undergo a TKA revision. Because the patellar component showed minimal wear of the polyethelyene surface intra-operatively, it was not replaced at that time. Despite the lack of wear on the patellar component, significant metal-on-metal wear of the tibial and femoral components and periprosthetic metallic debris was found. The revision was performed using implants from a Legion Revision Knee System (Smith and Nephew Inc., Memphis, TN). Specifically, a Legion Oxinium constrained femoral component with a straight cemented stem, a Legion Oxinium revision tibial base plate with a cemented stem, and a constrained Genesis II articular polyethylene insert were used. Oxinium is a trademark of Smith and Nephew and consists of oxidized zirconium, without detectable nickel elements. Histologic examination of the periprosthetic tissues demonstrated an extensive benign foreign-body type reaction in a background of chronic synovitis. Many large multi-nucleated giant cells contained abundant gray-black particulate material and crystalline material consistent with metallic debris and cement fragments. Follow-up radiographs obtained approximately one month after the revision (Fig. 3) showed no complications, and the prosthesis remained radiographically stable at both the six-month and one-year follow-up evaluations.
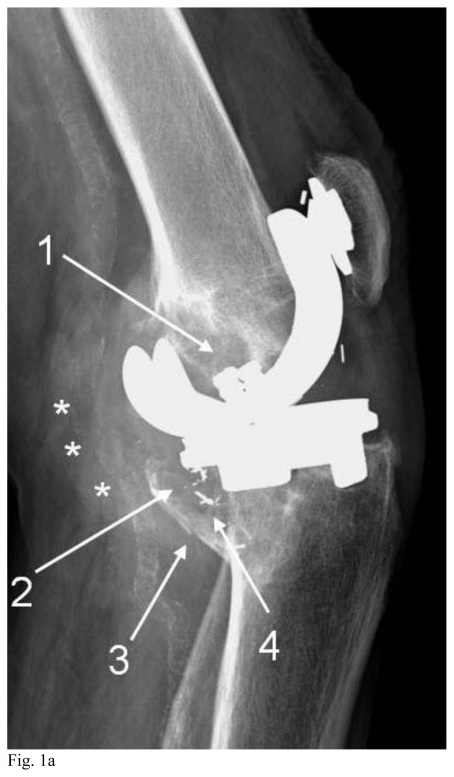
Figure 1.
74 year-old man with prior left total knee arthroplasty and patellar revision with increasing pain, now with periprosthetic osteolysis and manifestations of metallosis. Lateral (Fig. 1a) and AP (Fig. 1b) radiographs of the left knee show areas of osteolysis (arrows #1 and #2 in both projections) with associated fracturing of the tibial plateau (arrow #3, lateral view). Several metallic debris fragments are evident (arrow #4, lateral view). Amorphous increased density is present posterior to the knee on the lateral view (*). Similar findings seen at the hip have been referred to as the “cloud sign” of metallosis. A joint effusion is present. Vascular calcifications are noted.
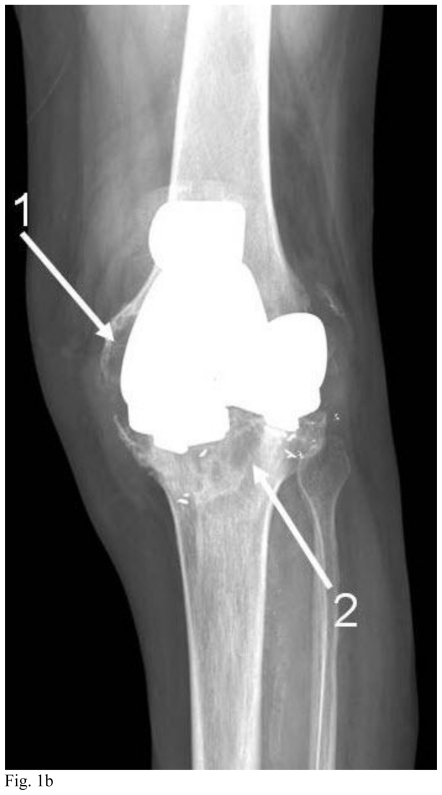
Figure 2.
74 year-old man with prior left total knee arthroplasty and periprosthetic osteolysis. Noncontrast axial CT of the left lower extremity at the level of the proximal tibia with bone algorithm (Fig. 2a) and soft tissue algorithm (Fig. 2b). (GE Lightspeed 16 CT scanner; kVp 120; mA 80; slice thickness 2.5 mm).
Fig. 2a shows several rounded lucencies (*) in the proximal tibia consistent with osteolysis. The differential diagnosis for periprosthetic osteolysis would include small particle disease, infection, and hardware loosening. Note is made of two metallic debris fragments (solid arrows). Atherosclerotic calcifications are also present.
Fig 2b (CT image with soft tissue algorithm) better shows the internal characteristics and complexity of the lytic foci. Curvilinear and nearly circular intermediate attenuation structures with central lower attenuation are seen within the more medial lytic lesion (dashed arrow). The Hounsfield units of the largest lytic area measured 48 (solid arrow).
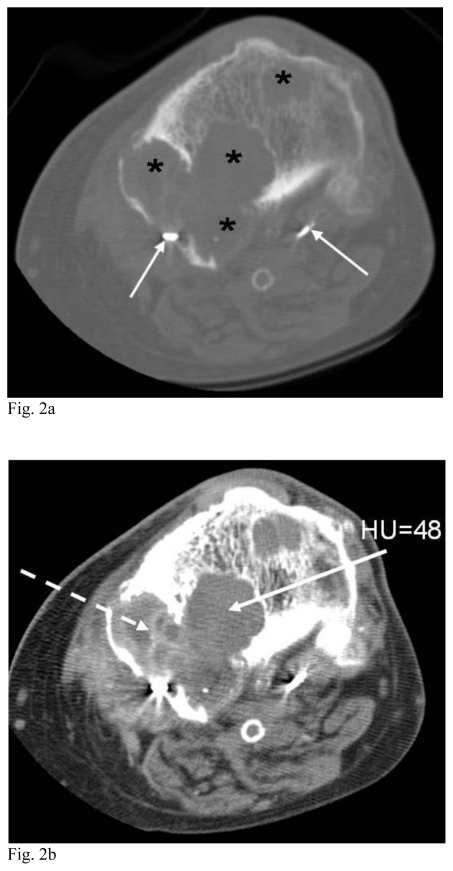
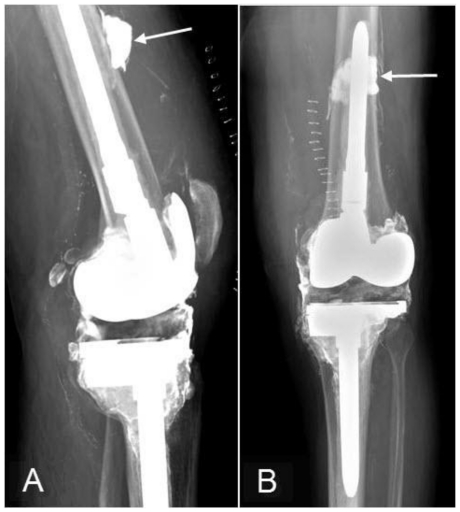
Figure 3.
74 year-old man with left total knee arthroplasty hardware failure and metallosis. Lateral (Fig. 3a) and AP (Fig. 3b) radiographs of the left knee were obtained after TKA revision (refer to Figs. 1a and 1b for preoperative radiographs), showing postoperative cutaneous staples. The lateral view demonstrates a small linear metallic density of the patellar polyethylene liner (arrow) in appropriate position. Notice there is now a tibial rod component in place. A joint effusion is also present.
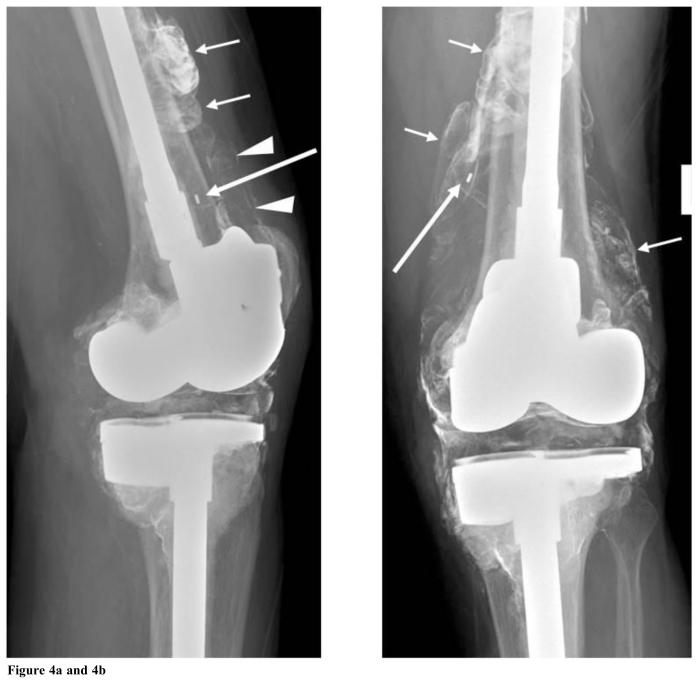
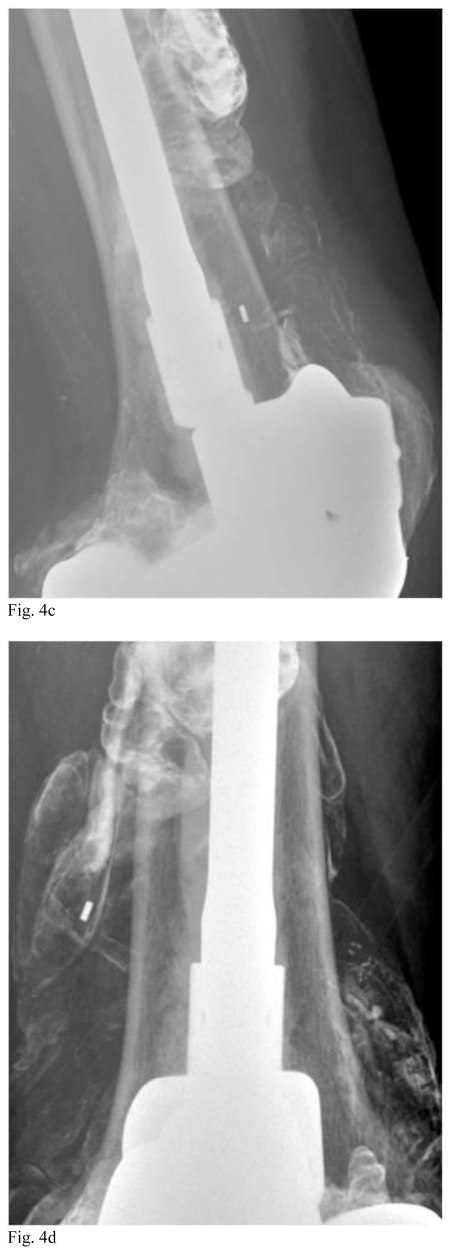
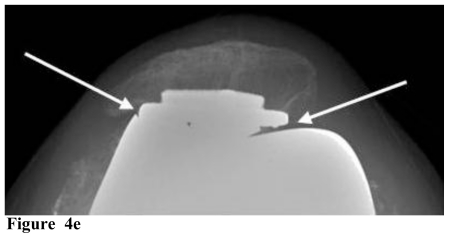
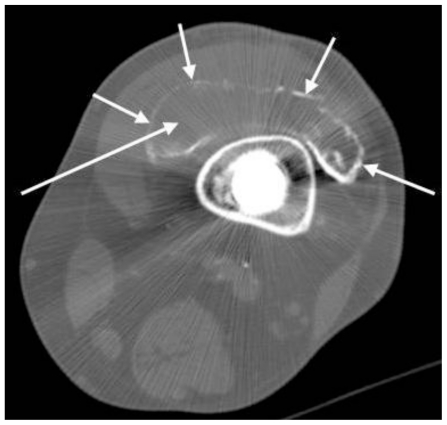
Approximately 18 months after the TKA revision discussed above, the patient developed progressive left knee swelling, crepitus, and pain, greatest near the patella and distal femur. Radiographs of the left knee were obtained for evaluation, and demonstrated new bubbly and curvilinear radio-densities around the knee, most evident adjacent to the distal femur, particularly in the suprapatellar pouch region (Figs. 4a-d). Additionally, a small linear metallic density had migrated away from the patella, thought to represent a dissociated patellar polyethylene liner (Figs. 4a-d). Close apposition of the patellar and anterior femoral components was present on the sunrise view radiograph (Fig. 4e), also suspicious for patellar liner wear and dissociation. A CT was ordered to evaluate the left knee and to better delineate the joint space. This confirmed extensive linear densities outlining a distended joint capsule (Fig. 5).
Figure 4a.
and 4b. These “off lateral (a = left)” and AP (b = right) radiographs of the left knee were obtained about 18 months after the Fig. 3 images. There are new lobulated and somewhat bubbly densities around the distal femur (short white arrows in Figs. 4a and b) similar to the “bubble sign” that has been described after total hip arthroplasty. Linear densities are also seen in the suprapatellar region on the lateral view (arrowheads in Fig. 4a), similar to the “metal-line sign” of metal-induced synovitis. Both the “bubble sign” and “metal-line sign” represent metallic debris outlining the joint space, effectively demonstrating the joint cavity. Also, note that the small metallic density associated with the patellar polyethylene marker has dissociated superomedially (long arrow in Figs. 4a and 4b), compared to Fig. 3. This is an uncommon but important finding of hardware failure.
Figures 4c and 4d.
are magnification views of the “off-lateral” and AP views in Figs. 4a and 4b, respectively, better demonstrating the findings.
Figure 4e.
The sunrise view of the left knee shows close apposition of the metal backing of the patellar component with the trochlear groove of the femoral component (arrows). This finding can be a sign of abnormal position of the polyethylene liner, but the differential for patellofemoral narrowing would also include liner wear and technical factors due to projection.
Figure 5.
74 year-old man after left total knee arthroplasty revision with metallosis and metal-induced synovitis. Noncontrast axial CT of the left lower extremity at the level of the distal femur (GE Lightspeed 16 CT scanner; kVp 120; mA 310; 2.5 mm slice thickness) demonstrates linear radiodensities outlining the suprapatellar joint space (short arrows). The joint cavity is distended and outlined by increased density. This finding corresponds with the “metalline sign” seen on plain radiographs (see Fig. 4a), consistent with metal-induced synovitis. There is relatively low attenuation within the joint space. The Hounsfield unit measurement in this region is limited by streak artifact from the adjacent hardware, but the area that the long arrow points to in this image measured 100 Hounsfield units.
The patient was again taken to surgery in June, 2008 (approximately 20 years after the initial TKA, approximately 12 years after the patellar revision, and approximately 2 years after the tibial and femoral implant revision described in detail above). Intra-operatively, the polyethylene liner of the patellar component had fragmented into large pieces which were removed. The metal backing of the patellar component was worn, but remained well-fixed. The patient was not deemed to be a candidate for patellar revision (due to wear on the trocheal groove area of the femoral component from contact with the metal-backed portion of the patellar component), and thus the metal patellar component was also removed. The femoral and tibial components were left in place. There was extensive gray-black discoloration of the periprosthetic soft tissue and a large effusion. A subtotal synovectomy was performed and the debrided synovial tissue consisted of diffusely gray-black, rubbery tissue fragments which could not grossly be identified as synovium. Histologically, the tissue demonstrated reactive synovial hyperplasia and diffuse deposition of finely granular, black metallic debris (Fig. 6). Many large multinucleated giant cells containing black granular debris and refractile material were scattered throughout the synovial lining (Fig. 7). Radiographs performed three weeks after surgery showed no acute complications. Much of the bubbly and linear radio-densities had been removed, particularly in the suprapatellar region, and with evidence of removal of the patellar component (Fig. 8). Radiographs performed at six-month follow up remained stable; the patient’s pain has continued to improve and he is currently able to participate in physical therapy.
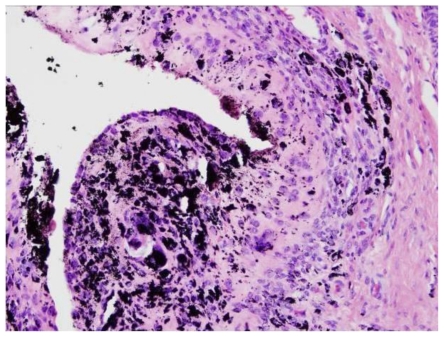
Figure 6.
74 year-old man with periprosthetic metallosis and metal-induced synovitis. Left knee synovium (H&E, 200x magnification). The synovium is reactive and appears loaded with fine black metallic debris.
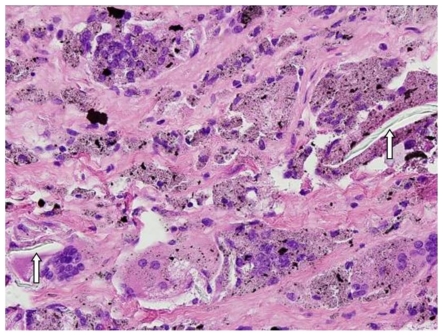
Figure 7.
74 year-old man with periprosthetic metallosis and metal-induced synovitis. Left knee synovium (H&E, 400x magnification). High power magnification demonstrates the presence of black metallic debris within multinucleated giant cells in the synovial lining. Polyethylene fragments are seen as refractile material within the giant cells (white arrows).
Figure 8.
74 year-old man with metallosis. Lateral (Fig. 8a) and AP (Fig. 8b) radiographs of the left knee show interval removal of the metal-backed patellar component and dissociated liner (reference Figs. 4a-d). A subtotal synovectomy and metallosis debridement were also performed with removal of the bubbly and linear radiodensities that were seen around the distal femur (reference Figs. 4a-d). Dense residual debris and/or calcification is noted in the highest portion of the suprapatellar joint cavity (arrows), and a joint effusion and skin staples are present.
DISCUSSION
Metallosis is a complication of total joint replacement. It refers to deposition of metallic debris into the periprosthetic soft tissues from abrasion of metallic components. This process can involve the joint capsule or cavity, and the extra-articular tissues. Small particles also get abraded from the surface of the polyethylene liner. Deposition of debris from the prosthesis into the periarticular soft tissues can cause pain, formation of a mass with occasional cystic change, osteolysis and systemic effects related to metal hypersensitivity [1–4].
Metallosis is most commonly described at the knee and hip joints, but has been reported in other locations such as the shoulder, wrist and elbow [1–5]. In a series by Rader et al., metallosis was present in 7 of 30 (23%) patients with total knee replacements using metal-backed patellar components [6]. Metal-backed patellar components are no longer in frequent use, however, but patients with this implant are still common [7]. The overall incidence of metallosis as a result of total hip arthroplasty failure has been reported at approximately 5.3% [8]. The implant material likely relates to the rate of its wear, and how the body reacts to the presence of the debris. Titanium components appear to have increased association with metallosis when compared to chromium-cobalt [9]. For example, in a series by Weissman et al. of 18 patients with metallosis following TKA, the worn component had titanium metal backing in 11 patients, and a chromium-cobalt backing in 5 patients [9]. Newer materials have been produced in efforts to decrease component wear, for example, Oxinium (oxidized zirconium) by Smith and Nephew Inc.
Pathophysiologically, there are thought to be three primary mechanisms for the development of a chronic inflammatory arthritis following joint replacement. These mechanisms include metal hypersensitivity, direct toxic effects of the ionic metal particles, and particle induced synovitis [10].
The presence of microscopic debris particles in the soft tissues incites a foreign body inflammatory reaction with a histiocytic infiltrate and mulinucleated giant cells (Fig. 7). A fibrotic response ensues in an attempt to encapsulate the immunogen, and the histiocytes that engulf the particles release inflammatory cytokines, such as interleukin-1 [11]. These cytokines may cause the periprosthetic osteolysis (as demonstrated in Figs. 1 and 2) that is associated with implant loosening. Inflammatory cells infiltrate the synovium in response to the debris, which causes synovial hyperplasia and there is histopathologic evidence of black material in the synovium (Fig. 6). This is usually associated with an acutely painful effusion [9]. Metal and polyethylene particles can also be taken up by the lymphatic system and carried away from the joint replacement site [12]. Inguinal lymphadenopthay has been reported due to metallic debris from loosening of a knee prosthesis in a 19 year old patient [12], although this was not present in our case. Elevated metal levels have been found in blood and urine of patients with metallosis [13], but were not evaluated for in our patient.
The most common cause of fine metallic debris after total knee replacement is wear of a metal-backed polyethylene patellar prosthesis [14,15]. Early wear of the polyethylene liner leads to deposition of small particles of polyethylene into adjacent tissues with associated giant cell reaction and synovitis [6]. Further wear can lead to metal-on-metal contact, and thus shedding of metal debris. Dissociation of the polyethylene liner from the metal-backed patellar component similarly leads to metallosis by allowing friction between the patellar metal plate and the anterior femoral component, which sloughs debris into the joint capsule [16]. In one series, dissociation of the polyethylene from the metal-backing was present in 4 of 30 patients with TKA [6]. One of the main reasons for failure of the metal-backed polyethylene liner (failure defined as excess wear and/or dissociation of the liner), is thought to be undue high biomechanical stresses on the insert [6]. Reported mechanisms that lead to this undesirable stress are patellar tracking abnormalities, trauma, and soft tissue imbalance [16]. Patellar tracking refers to the motion of the patella relative to the femoral groove with knee flexion and extension. This is predominately central with normal biomechanical alignment. With regard to TKA and TKA revisions, patellar tracking is assessed prior to reaming of the patellar component. Notably, subluxation of the patellar component is one of the most common causes of failed total knee replacement. Radiographically, abnormal position of the patellar polyethylene liner might be suggested by an aberrant location of the small, linear metallic density associated with the liner (Figs. 4a-d). Close apposition of the patellar component with the anterior aspect of the femoral component (Fig. 4e) can also be a sign of liner wear or abnormal liner position. Early revision to an all-polyethylene patellar prosthesis seems to be the best solution to prevent progressive destruction of the joint [6].
Radiography is the primary imaging method for evaluation of TKA, and can diagnose metallosis and metal-induced synovitis. Metallosis can lead to amorphous, fluffy increased densities in the periprosthetic soft tissues. In our case, this is best seen in the soft tissues posterior to the left knee joint on Fig. 1. This finding was initially described as a complication of total hip arthroplasty, and was referred to as the “cloud sign” on plain radiographs [17]. Additionally, bubbly appearing radiodensities have been described complicating total hip arthroplasty [18]. These represent metal deposition outlining the synovium and joint capsule, and are known as the “bubble sign” on plain radiographs. In our patient, the bubbly densities are best demonstrated on Figs. 4a-d. Distinction of the “cloud sign” from the “bubble sign” can be made by recognizing that the cloudy densities are seen as an area of fairly uniform, amorphous increased density, as opposed to the curvilinear densities of the “bubble sign.” While the “bubble sign” and “cloud sign” were first described after total hip replacement, they have been adapted to our patient with a TKA. A radiographic finding previously described after TKA is the “metal-line sign [9].” This sign, which is thought to be specific for metal-induced synovitis [9], is seen as a thin rim of linear increased density outlining a portion of the joint capsule. It is usually seen in the suprapatellar pouch region. Similar in pathophysiology to the “bubble sign,” the appearance is caused by metal debris deposition into the joint capsule with resultant uptake of the microscopic particles by multinucleated giant cells in the synovial lining (refer to Fig. 4 for the radiographic appearance of the “metal-line sign,” to Fig. 5 for its corresponding CT appearance, and to Figs. 6 and 7 for the histological appearance). Weissman et al. found this sign to be present in 11 of 18 patients with proven metal-induced synovitis, and the sign was identified from 19 months to 6 years after the time of arthroplasty [9]. An associated joint effusion is usually present. Diffusely increased density in the joint cavity may also be present, indicating abnormally dense synovial fluid.
One role of CT in evaluation of metallosis is to better evaluate the dense metal outlining the affected joint (Fig. 5) [5]. CT can also help confirm the presence of questionable areas of osteolysis seen on radiographs, and allows more accurate quantification of periprosthetic bone loss (Fig. 2a). CT may also better delineate the internal architecture of areas of osteolysis (Fig. 2b). MRI is not routinely used in the evaluation of metallosis, and was not utilized in our case. If performed, MRI should show susceptibility artifact to confirm the presence of metal within the soft tissues [5].
Early recognition of the radiographic changes associated with metallosis is important. In our case involving total knee arthroplasty, we saw similar radiographic findings of metallosis that have been described after total hip arthroplasty, including the “cloud sign” and the “bubble sign.” Also demonstrated was the “metal-line sign,” which is considered essentially diagnostic of metal-induced synovitis [9]. Prompt diagnosis of the radiographic changes associated with metallosis will alert the orthopedist to the extent of metallic debris deposition, and the need for intervention to prevent progressive joint destruction.
TEACHING POINT
Metallosis can result from metal-on-metal wear in patients with total knee arthroplasty. Metallosis can be recognized on radiographs as the “metal-line sign,” which is seen as a thin rim of linear increased density outlining a portion of the joint capsule, and usually in the suprapatellar pouch region. More curvilinear and circular radiodensities are referred to as the “bubble sign,” and also outline the joint space. Visualization of amorphous, cloudy, periprosthetic soft tissue densities is referred to as the “cloud sign.” Other associated findings of metallosis include periprosthetic osteolysis, a joint effusion, and metallic fragmentation.
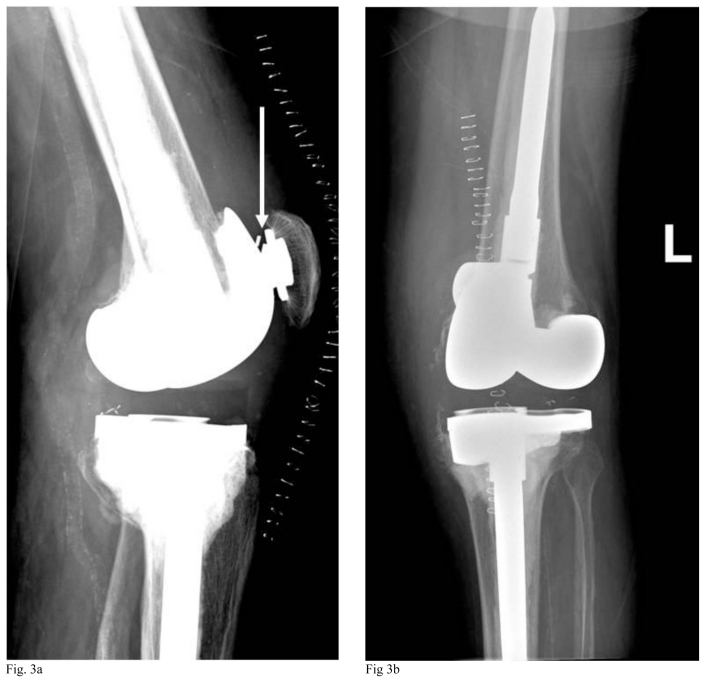
Table 1.
Differential diagnosis table for metallosis following total knee arthroplasty
| Differential diagnosis | X-ray | CT | MRI T1 | MRI T2 | Pattern of contrast enhancement | Scintigraphy |
|---|---|---|---|---|---|---|
| Metallosis | First line of diagnosis; metal-line sign; bubble sign; cloud sign (see discussion for details of signs); joint effusion often present; periprosthetic osteolysis, may see malposition of polyethylene liner | Radiodense rim outlining joint cavity, joint effusion, sometime with increased density within the joint fluid, periprosthetic osteolysis, soft tissue masses and complex fluid collections can be seen [5] | Not routinely used but may see low signal rim outlining joint capsule or in areas of metal deposition, low signal regions of lysis in bone | Not routinely used but may show signal rim outlining joint capsule or in areas of metal deposition *note: susceptibility artifact is seen on spin echo or gradient echo images [5] | Associated synovitis may enhance | Not routinely used |
| Small particle disease | First line of diagnosis; Periprosthetic osteolysis that is not loosening; may see evidence of component wear or malposition; no secondary bone response changes; progressive with eventual destruction and fracturing | Same as X-ray but with more accurate quantification of bone loss; look carefully for source of debris, particularly polyethylene wear; used for preoperative planning for extent and precise location of bone destruction | Low signal regions of synovitis and lysis of bone | May see high signal in osseous cysts | Associated synovitis may enhance | Not routinely used |
| Infected prosthesis | May be negative or indistinguishable from prosthetic loosening; lytic bone destruction; ill- defined bone resorption; periosteal reaction; occasional periprosthetic fluffy dystrophic bone formation | Same as X-rays | Not routinely used | Bone scan: cold defect associated with prosthesis and generalized increased activity around prosthesis, especially the stem; Indium 111 white blood cell scan shows activity around prosthesis, without corresponding marrow activity on sulfur colloid marrow scan. | ||
| Prosthesis loosening | First line of diagnosis; lucency at bone-prosthesis or bone-cement interface | Same as x-rays, with more accurate depiction | Not routinely used | Bone scan: cold defect associated with prosthesis, increased activity at site of loosening; Sulfur colloid scan shows uptake accumulation around stem of prosthesis | ||
| Metastatic periprosthetic lytic lesion | Lytic lesions and/or associated soft tissue masses may be seen | Same as X-rays with more accurate depiction | Lytic lesions often T1 dark | Lytic lesions may have variable T2 appearance | Usually associated with enhancement | May show increased uptake or cold defects on bone scan |
Table 2.
Summary table for metallosis following total knee arthroplasty
| Etiology | Mechanical abrasion of metal surfaces causing microscopic debris with associated inflammatory response. |
| Incidence | Exact incidence is unknown [5], but has been reported at 23% after TKA with metal- backed patellar components [6] (which are no longer in common use). |
| Gender ratio | No known gender predilection. |
| Age predilection | Older patients (related to presence of arthroplasties in this population). |
| Risk factors | Biomechanical stresses on polyethylene liner insert that can lead to excess wear [6]. |
| Treatment | Surgical debridement, arthroplasty revision depending on extent of involvement |
| Prognosis | Good if early arthroplasty revision to prevent progressive joint destruction |
| Findings on imaging | Metal-line sign, bubble sign, cloud sign; periprosthetic osteolysis; often a joint effusion. |
ABBREVIATIONS
- CT
Computed tomography
- TKA
Total knee arthroplasty
REFERENCES
- 1.Cofield RH. Uncemented total shoulder arthroplasty - a review. Clin Orthop Relat Res. 1994:86–93. [PubMed] [Google Scholar]
- 2.Khan WS, Agarwal M, Malik AA, et al. Chromium, cobalt and titanium metallosis involving a Nottingham shoulder replacement. J Bone Joint Surg Br. 2008;90B:502–05. doi: 10.1302/0301-620X.90B4.20302. [DOI] [PubMed] [Google Scholar]
- 3.Groot D, Gosens T, van Leeuwen NCM, et al. Wear- induced osteolysis and synovial swelling in a patient with a metal-polyethylene wrist prosthesis. J Hand Surg Am. 2006;31A:1615–18. doi: 10.1016/j.jhsa.2006.09.009. [DOI] [PubMed] [Google Scholar]
- 4.Degreef I, Sciot R, De Smet L. Metallosis in revision total elbow arthroplasty. Complications and staging method. Acta Orthopaedica Belgica. 2008;74:753–760. [PubMed] [Google Scholar]
- 5.Heffernan EJ, Alkubaidan FO, Nielsen TO, Munk PL. The imaging appearances of metallosis. Skeletal Radiol. 2008;37:59–62. doi: 10.1007/s00256-007-0362-y. [DOI] [PubMed] [Google Scholar]
- 6.Rader CP, Lohr H, Whittmann R, Eulert J. Results of total knee arthroplasty with a metal-backed patellar component: a 6 year follow-up study. J Arthroplasty. 1996;11:923–30. doi: 10.1016/s0883-5403(96)80133-1. [DOI] [PubMed] [Google Scholar]
- 7.Chew FS, Ramsdell MG, Keel SB. Metallosis after total knee replacement. Radiologic-pathologic conferences of the Massachusetts General Hospital. AJR. 1998;170:1556. doi: 10.2214/ajr.170.6.9609173. [DOI] [PubMed] [Google Scholar]
- 8.Chang JD, Lee SS, Hur M, et al. Revision total hip arthroplasty in hip joints with metallosis: a single-center experience with 31 cases. J Arthroplasty. 2005;20(5):568–73. doi: 10.1016/j.arth.2005.04.001. [DOI] [PubMed] [Google Scholar]
- 9.Weissman BN, Scott RD, Brick GW, Corson JM. Radiographic detection of metal-induced synovitis as a complication of arthroplasty of the knee. J bone Joint Surg Am. 1991;73A:1002–7. [PubMed] [Google Scholar]
- 10.Niki Y, Matsumoto H, Otani T, et al. Five types of inflammatory arthritis following total knee arthroplasty. J Biomed Mat Res Part A. 2007;81A:1005–10. doi: 10.1002/jbm.a.31152. [DOI] [PubMed] [Google Scholar]
- 11.Al Saffar N, Revel PA. Interleukin-1 production by activated macropages surrounding loosened orthopaedic implants: a potential role in osteolysis. Br J Rheumatol. 1994;33:309–16. doi: 10.1093/rheumatology/33.4.309. [DOI] [PubMed] [Google Scholar]
- 12.Shinto Y, Uchida A, Yoshikawa H, et al. Inguinal lymphadenopathy due to metal release from a prosthesis: a case report. J Bone Joint Surg Br. 1993;75B:266–69. doi: 10.1302/0301-620X.75B2.8444948. [DOI] [PubMed] [Google Scholar]
- 13.Coleman RF, Herrington J, Scales JT. Concentration of wear products in hair, blood, and urine after total hip replacement. British Med J. 1973;1:527–29. doi: 10.1136/bmj.1.5852.527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bayley JC, Scott RD. Further observations on metal- backed patellar component failure. Clin Orthop. 1988;236:82–87. [PubMed] [Google Scholar]
- 15.Bayley JC, Scott RD, Ewald FC, Holmes GB., Jr Failure of the metal-backed patellar component after total knee replacement. J Bone and Joint Surg Am. 1988;70A:668–74. [PubMed] [Google Scholar]
- 16.Quale JL, Murphey MD, Huntrakoon M, et al. Titanium-induced arthropathy associated with polyethylene-metal separation after total joint replacement. Radiology. 1992;182:855–58. doi: 10.1148/radiology.182.3.1535907. [DOI] [PubMed] [Google Scholar]
- 17.Paydar A, Chew FS, Manner PA. Severe periprosthetic metallosis and polyethylene liner failure complicating total hip replacement: the cloud sign. Radiology case reports. 2007;2:1–6. doi: 10.2484/rcr.v2i4.115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Su EP, Callander PW, Salvati EA. The bubble sign: a new radiographic sign in total hip arthroplasty. J Arthroplasty. 2003;18:110–12. doi: 10.1054/arth.2003.50007. [DOI] [PubMed] [Google Scholar]