Abstract
Transcatheter embolization is increasingly accepted as a safe and effective therapy for acute lower gastrointestinal hemorrhage, but the fate of the coils used for treatment is not entirely known. We report a patient with massive descending colonic bleeding, successfully treated with microcoil occlusion, in whom partially extruded coils were later visualized colonoscopically, but initially misidentified as ingested jewelry. The incidence of this endoscopically enigmatic (but in this case clinically inconsequential) finding is unknown.
Keywords: Colonic hemorrhage, Transcatheter embolization, Coil extrusion, Unrecognized endoscopic abnormalities
CASE REPORT
A 64 year old female with a mechanical aortic valve, necessitating chronic warfarin anticoagulation, presented with one day of increasing rectal bleeding. Her systolic blood pressure in the emergency department was below 50 mm Hg. Hematocrit, platelet count, and international normalized ratio were 17%, 203 K/μL, and 2.92, respectively. With hemorrhagic shock refractory to pressor support, she was emergently referred to interventional radiology for visceral angiography with plans for endovascular therapy.
Selective inferior mesenteric arteriography demonstrated marked vasoconstriction, presumably related to profound hypotension, with extravasation from a descending colonic arterial branch (Figure 1). Superselective marginal arteriography demonstrated massive active bleeding into the colon (Figure 2). Although targeted bleeding branch embolization was initially planned, this vessel could not be readily catheterized, and given her deteriorating clinical status, platinum microcoil (Tornado®, Cook Medical, Bloomington, IN) embolization was performed in the marginal artery just cephalad and caudad to the bleeding vessel (Figure 3). Complete hemostasis was not immediately achieved, presumably due to profound coagulopathy, but her hemodynamic status nonetheless improved rapidly and dramatically, with systolic blood pressure quickly rising to 100 mm Hg. Inferior mesenteric angiography several minutes later demonstrated cessation of bleeding, with no further target vessel filling, and dramatic improvement in previously noted vasoconstriction (Figure 4).
Figure 1.
Inferior mesenteric arteriography from a right transfemoral approach in a 64 year old female with massive lower gastrointestinal bleeding using a Sos Omni® Selective Catheter (AngioDynamics, Latham, NY) reveals marked vasospasm, probably related to hypotension, with a small focus of extravasation (arrow) in the mid-descending colon.
Figure 2.
Sequential images of a superselective angiography using a RenegadeTM Hi-Flo Microcatheter (Boston Scientific, Natick, MA), with coaxial catheter positioned in the marginal artery of the left colon, demonstrates progressive intra-luminal hemorrhage from a small distal branch (arrows).
Figure 3.
Immediately after Tornado® microcoil (Cook Medical, Bloomington, IN) embolization of the marginal artery both cephalad and caudad to the bleeding vessel (arrows) in this coagulopathic patient, extravasation persists (open arrow). Angiography is performed through a Renegade Hi-FloTM microcatheter positioned above the embolization site in the left colonic marginal artery.
Figure 4.
Several minutes after embolization, inferior mesenteric arteriography demonstrates non-filling of the target vessel, with otherwise intact marginal artery flow via the left colic and sigmoid arteries. Vasospasm has already improved. Angiography is performed through the Sos Omni® Selective Catheter (AngioDynamics, Latham, NY) positioned at the origin of the inferior mesenteric artery.
Over the next several days, with aggressive blood product replacement and coagulopathy correction, her gastrointestinal bleeding clinically ceased, and hematocrit stabilized.
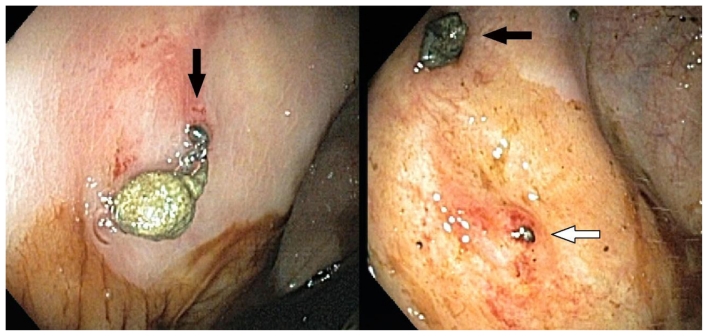
Colonoscopy was performed six days later to better evaluate the site and source of bleeding. Extensive diverticular disease was noted, without evidence for ischemia or ulceration in the embolization field. Unexpected to the endoscopist were two metallic foreign bodies. Protruding through the wall of the mid descending colon was a “medium size metal object” (Figure 5a). Approximately 3 cm cephalad, a second metallic object was identified, just barely protruding through the mucosa (Figure 5b).
Figure 5.
Left: Colonoscopy reveals a nest of microcoils protruding from the wall of the mid-descending colon (arrow), with a small focus of adherent stool. Right: A smaller shiny area of microcoil protrusion through the colonic mucosa is present just several centimeters cephalad (open arrow). The stool adherent to the former coil (arrow) is nearby, and noted for reference.
The etiology of the metallic structures was not recognized at the time of endoscopy, and the gastroenterologist speculated that these might reflect ingested jewelry that had perforated the colon, although no such history could be elicited. The larger protruding foreign body was removed with forceps at the time of colonoscopy, with only minimal associated bleeding, and sent to pathology. No attempts were made to remove the deeper and less conspicuous object. Only a gross examination was performed by the pathologist, who described a coiled wire, and offered a diagnosis only of “metallic foreign body” and commented, given the speculative history provided, that this might reflect part of an earring.
The specimen was soon discarded in pathology, and a photograph could thus not be obtained. After the radiographic appearance of constrained and unconstrained microcoils was shared with the endoscopist and pathologist, however, both agreed that the initially enigmatic removed foreign body in fact reflected an extruded embolization coil.
DISCUSSION
Although controversial in its infancy [1], transcatheter embolization is now widely accepted for the treatment of acute lower gastrointestinal bleeding [2,3,4,5,6,7]. Various embolic materials have been described, but microcoils have evolved over time as the preferred agents for many interventionalists [2,3].
After transcatheter embolization, coils have been infrequently reported at endoscopy protruding into duodenal ulcers [8,9], but to our knowledge, post-embolization coil extrusion through the colon has not been described. Herein we report a case of partial extrusion of embolization coils through the colonic wall after successful microcoil control of massive colonic bleeding.
Historically, mesenteric arterial vasopressin infusion served as primary transcatheter therapy for lower gastrointestinal bleeding [1]. Paralleling the development of microcatheters and microcoils, however, this technically simpler therapy has been rapidly replaced by superselective embolization [1]. While earlier embolization procedures resulted in ischemic complications in as many as one-third of cases [10,11], those complications are now uncommon [3], probably related to improvements in both devices and techniques, which together permit more controlled, targeted and therefore more effective occlusion. Microcoils, typically delivered through a coaxial microcatheter via a transfemoral route and positioned whenever possible to obtain both proximal and distal control when collateral vessels are present, are preferred in most circumstances to gelatin foam sponge or particulate matter, so as to minimize the risk of bowel infarction.
Recent articles outside of the interventional radiology domain, in the gastroenterology [6] and surgical [7] literature, attesting to the safety and efficacy of embolization are reflective, we believe, of increasing clinical awareness and acceptance of this minimally invasive therapy. Contraindications are few, and include renal insufficiency, contrast allergy, and uncontrollable coagulopathy. Transcatheter embolization is successful in as many as 83–100% of cases, obviating the need for bowel resection in many critically ill patients.
The visualization of errant medical devices at endoscopy is uncommon, and sufficiently unusual to have merited reporting in other settings. Gallbladder neck surgical clips migrating through the common bile duct were described as a “surprise finding” [12] in one publication, and two other groups have recently described gastroduodenal artery embolization coils protruding into duodenal ulcer craters [8,9]. Although post-embolization ulcers have previously been noted in the colon [2], we are unaware of any reports of transcolonic migration of embolization coils, particularly without associated ischemic ulceration, and believe that unawareness of this phenomenon likely contributed to the initial endoscopic misidentification in this case.
Publications evaluating embolization in the gastrointestinal tract have focused on cessation of bleeding, recurrent hemorrhage, and ischemic complications when reporting outcomes [2,3]. The fate of embolic coils themselves, however, has received little attention, and thus the incidence of transmural migration is unknown. Although the use of abdominal computed tomography (CT) has increased markedly in recent years [13], and many of these patients likely undergo CT imaging at some later point, a retrospective analysis of the natural course of colonic microcoils from CT reports or actual images would be difficult. Coils are rarely the focus of interpretive attention at the time of cross sectional imaging, and even if they were, are so tiny they would likely be dwarfed in conspicuity by adjacent enteral contrast. Given the lack of associated symptoms in our patient, it is quite possible that microcoil extrusion occurs more frequently, unbeknownst to patients and physicians, as coils could easily pass completely undetected in stool. Endoscopic visualization in this case, then, may have been purely serendipitous, and related to the timing of colonoscopy.
Without previously published reports, the mechanism of transmural coil extrusion in the absence of ischemic ulceration is unknown, but may very well be as simple as that involved in the transcutaneous expulsion of splinters and resorbable sutures, both well familiar to physicians evaluating traumatic and surgical wounds, respectively. Transmural enteral extrusion of medical devices is considerably less common, but has been described in the setting of anastomotic staples [14], and reported to occur rarely with ventriculo-peritoneal shunts [15]. These events seem to occur without adverse sequelae, concordant with the benign course of spontaneous partial transmural colonic extrusion in our patient. Although extraction of the dominant protruding coil in this case resulted in no adverse consequences, such extraction could result in disruption of tenuous hemostasis, and as such we cannot advise routine removal of protruding coils, when identified.
In summary, we report a case of transmural colonic microcoil extrusion post embolization, which was clinically inconsequential, but initially enigmatic endoscopically. Increased awareness of this phenomenon by interventional radiologists and gastroenterologists may minimize clinical conundrums in the future, and help better elucidate the frequency with which this event occurs.
TEACHING POINT
Metallic embolization microcoils used for transcatheter treatment of gastrointestinal bleeding can extrude through the colonic wall, without adverse clinical sequelae. Recognition of this unusual phenomenon may minimize endoscopic and clinical confusion, and help physicians better identity the frequency with which this event occurs.
Table 1.
Embolic agents utilized for treatment of gastrointestinal bleeding
| Agent | Typical Setting | Comments |
|---|---|---|
| Gelatin foam sponge | Acute upper gastrointestinal bleeding. |
|
| Particles (e.g., polyvinyl alcohol, acrylic microspheres) | Uncommonly used for treatment of gastrointestinal bleeding; usually only in the setting of tumor. |
|
| Metallic coils | Acute upper or lower gastrointestinal bleeding. |
|
Table 2.
Summary table of transcatheter embolization for lower gastrointestinal bleeding
| Typical approach | Transfemoral arterial |
| Typical catheter | Coaxial microcatheter |
| Usual embolic agent | Metallic microcoils |
| Embolization target site | Usually as distal as possible, either at the level of the marginal artery or vasa recta |
| Risks | Puncture site complications, contrast nephropathy, bowel ischemia |
| Success | 83–100% |
| Contraindications | Vascular access limitations, prior adverse contrast reaction, renal insufficiency, coagulopathy (all relative) |
ABBREVIATIONS
- mm Hg
millimeters of mercury
- CT
computed tomography
REFERENCES
- 1.Darcy M. Treatment of lower gastrointestinal bleeding: vasopressin infusion versus embolization. J Vasc Interv Radiol. 2003 May;14(5):535–43. doi: 10.1097/01.rvi.0000064862.65229.8a. [DOI] [PubMed] [Google Scholar]
- 2.Kuo WT, Lee DE, Saad WE, Patel N, Sahler LG, Waldman DL. Superselective microcoil embolization for the treatment of lower gastrointestinal hemorrhage. J Vasc Interv Radiol. 2003 Dec;14(12):1503–9. doi: 10.1097/01.rvi.0000099780.23569.e6. [DOI] [PubMed] [Google Scholar]
- 3.Kickuth R, Rattunde H, Gschossmann J, Inderbitzin D, Ludwig K, Triller J. Acute lower gastrointestinal hemorrhage: minimally invasive management with microcatheter embolization. J Vasc Interv Radiol. 2008 Sep;19(9):1289–96. doi: 10.1016/j.jvir.2008.06.003. [DOI] [PubMed] [Google Scholar]
- 4.Bandi R, Shetty PC, Sharma RP, Burke TH, Burke MW, Kastan D. Superselective arterial embolization for the treatment of lower gastrointestinal hemorrhage. J Vasc Interv Radiol. 2001 Dec;12(12):1399–405. doi: 10.1016/s1051-0443(07)61697-2. [DOI] [PubMed] [Google Scholar]
- 5.Peck DJ, McLoughlin RF, Hughson MN, Rankin RN. Percutaneous embolotherapy of lower gastrointestinal hemorrhage. J Vasc Interv Radiol. 1998 Sep-Oct;9(5):747–51. doi: 10.1016/s1051-0443(98)70386-0. [DOI] [PubMed] [Google Scholar]
- 6.Maleux G, Roeflaer F, Heye S, Vandersmissen J, Vliegen AS, Demedts I, Wilmer A. Long-term outcome of transcatheter embolotherapy for acute lower gastrointestinal hemorrhage. Am J Gastroenterol. 2009 Aug;104(8):2042–6. doi: 10.1038/ajg.2009.186. [DOI] [PubMed] [Google Scholar]
- 7.Koh DC, Luchtefeld MA, Kim DG, Knox MF, Fedeson BC, Vanerp JS, Mustert BR. Efficacy of transarterial embolization as definitive treatment in lower gastrointestinal bleeding. Colorectal Dis. 2009 Jan;11(1):53–9. doi: 10.1111/j.1463-1318.2008.01536.x. [DOI] [PubMed] [Google Scholar]
- 8.Singh G, Denyer M, Patel JV. Endoscopic visualization of embolization coil in a duodenal ulcer. Gastrointest Endosc. 2008 Feb;67(2):351–2. doi: 10.1016/j.gie.2007.08.022. [DOI] [PubMed] [Google Scholar]
- 9.Vardar R, Ozütemiz O, Parildar M. Endoscopic view of intravascular platinum coil after embolization of bleeding duodenal ulcer: report of two cases. Endoscopy. 2009;41( Suppl 2):E125–6. doi: 10.1055/s-0029-1214659. [DOI] [PubMed] [Google Scholar]
- 10.Bookstein JJ, Chlosta EM, Foley D, Walter JF. Transcatheter hemostasis of gastrointestinal bleeding using modified autogenous clot. Radiology. 1974 Nov;113(2):277–85. doi: 10.1148/113.2.277. [DOI] [PubMed] [Google Scholar]
- 11.Chuang VP, Wallace S, Zornoza J, Davis LJ. Transcatheter arterial occlusion in the management of rectosigmoidal bleeding. Radiology. 1979 Dec;133(3 Pt 1):605–9. doi: 10.1148/133.3.605. [DOI] [PubMed] [Google Scholar]
- 12.Taylor KM, Foxton M, McNair A. Surprise finding at endoscopic retrograde cholangiopancreatography. Clin Gastroenterol Hepatol. 2010 Mar;8(3):e24–5. doi: 10.1016/j.cgh.2009.09.028. [DOI] [PubMed] [Google Scholar]
- 13.Berrington de González A, Mahesh M, Kim KP, Bhargavan M, Lewis R, Mettler F, Land C. Projected cancer risks from computed tomographic scans performed in the United States in 2007. Arch Intern Med. 2009 Dec 14;169(22):2071–7. doi: 10.1001/archinternmed.2009.440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Schwarzbart G, Lubin J. Experience with auto suture surgical stapling instruments. Fate of enterically applied staples. Int Surg. 1978 Mar;63(3):146–51. [PubMed] [Google Scholar]
- 15.Gelabert González M. Extrusion of peritoneal catheter through the anus. Childs Nerv Syst. 1987;3(3):183–4. doi: 10.1007/BF00717899. [DOI] [PubMed] [Google Scholar]