Abstract
Osteoblastoma is a rare benign bone tumor that usually arises in the vertebral column and long bones of young adults. Craniofacial involvement is extremely rare. To date, osteoblastoma of the frontal sinus has not been reported in the English literature. We report an osteoblastoma of both frontal sinuses in a 23-year-old male who presented with headache and blurry vision in the left eye. Computed tomography (CT) demonstrated an expansile lesion involving both frontal sinuses with sclerotic and fibrous components, eroding into the roof of the left orbit. On magnetic resonance imaging (MRI) the dense portion of the lesion showed signal void on all sequences, while the fibrous matrix was isointense to grey matter on T1-weighted and T2-weighted images and showed avid enhancement following intravenous contrast administration. Surgical resection was performed and histology was consistent with osteoblastoma.
Keywords: Frontal sinus, exophthalmos, osteoblastoma
INTRODUCTION
Osteoblastoma is an osteobalstic bone tumor that usually involves the vertebrae and long bones (1). It is an uncommon osseous lesion accounting for less than 1 percent of excised primary osseous tumors and about 3 percent of benign osseous tumors (1). Craniofacial involvement is extremely rare, usually seen in the paranasal sinuses and orbits (2). To our knowledge, this is the first case of craniofacial osteoblastoma arising in the frontal sinuses, reported in the English literature.
CASE REPORT
A 23-year-old white male patient presented to the emergency department of our institution following the onset of blurred vision in the left eye, worsening over the past 48 hours. He also described bilateral frontal headache over the past month associated with frontal fullness. The patient had a personal history of hypertension requiring medical treatment. On physical examination he had swelling and tenderness over the left facial area. There was minimal exophthalmos of the left eye but the movement of the extraocular muscles was intact. Visual field examination showed field cut in left lower quadrant. The physical exam was otherwise unremarkable. Results of routine laboratory tests were within normal limits.
Given the patient’s history and physical examination, non-contrast CT scan of the brain was ordered, and demonstrated an expansile mass involving both frontal sinuses, with most involvement in the left frontal sinus. The lesion had sclerotic and fibrous components, the former along its anterior aspect and the latter along its supero-posterior aspect; it measured 5.4 × 4.0 × 4.0 cm (maximum transverse, anteroposterior, and craniocaudal dimensions respectively) (Fig 1). The fibrous component caused thinning, and in some regions erosion of the posterior cortex of the left frontal sinus wall (Fig 1) and extended inferiorly into the ipsilateral frontoethmoid recess (Fig 2). The dense component scalloped the anterior frontal sinus cortex (Fig 1) and eroded through the left orbital roof (Fig 2). The portion of the frontal sinuses not occupied by the described lesion was completely opacified by a homogenous soft tissue density (Fig 1). MRI showed signal void corresponding to the dense component on all sequences without enhancement following intravenous contrast administration (Fig 3). The fibrous component was iso-intense to grey matter on T1-weighted (T1W), T2-weighted (T2W) and Fluid-Attenuated Inversion Recovery (FLAIR) sequences and showed strong enhancement following intravenous contrast administration (Fig 3). The soft tissue density in the frontal sinuses seen on CT had high T2W and intermediate T1W signal intensity and showed peripheral enhancement (Fig 3). Coronal images confirmed erosion of the orbital roof and demonstrated impingement on superior rectus muscle (Fig 4) resulting in minimal secondary proptosis (Fig 5). The leading radiological differential diagnosis was fibrous dysplasia and osteoma.
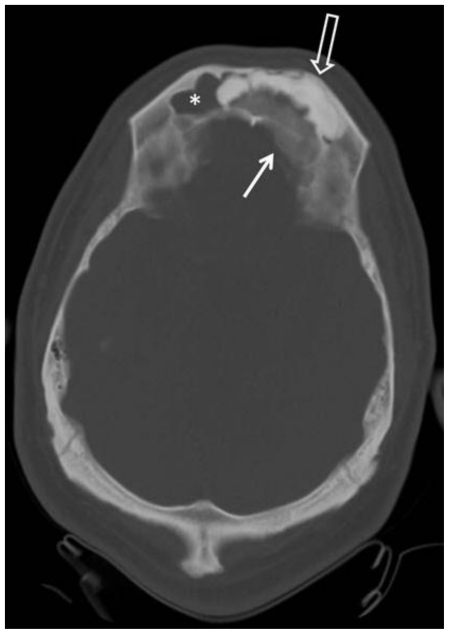
Figure 1.
23-year-old male patient with frontal sinus osteoblastoma who presented with headache and blurry vision in left eye. Axial non enhanced CT image through the frontal sinuses shows a relatively well defined expansile lesion in both frontal sinuses with sclerotic and fibrous components. There is scalloping of the anterior frontal sinus cortex by the sclerotic component (open arrow) and erosion of the posterior cortex by the fibrous component (arrow). The remaining part of the frontal sinus is occupied by a soft tissue density (asterisk) that was found to represent entrapped secretions during surgery (Technique: KVp = 120; mA = 37; Slice Thickness = 5.00 mm).
Figure 2.
23-year-old male patient with frontal sinus osteoblastoma who presented with headache and blurry vision in left eye. Axial non enhanced CT image through the frontoethmoid recess and orbital roof shows extension of the fibrous component of the lesion into the left frontoethmoid recess (asterisk) and the sclerotic lesion into the left orbital roof (arrow). (Technique: KVp = 120; mA = 37; Slice Thickness = 5.00 mm).
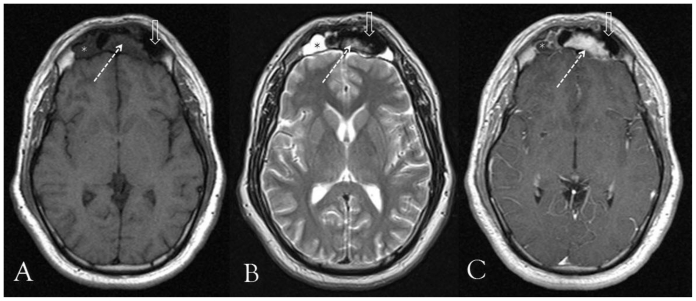
Figure 3.
23-year-old male patient with frontal sinus osteoblastoma who presented with headache and blurry vision in left eye. Axial MRI images through the frontal sinuses, at same level of the displayed CT image in figure 1. a: Axial noncontrast spin echo T1W image [1.5 Tesla (TR/TE = 437 msec./14 msec.) Slice Thickness = 5.00 mm]. b: Axial noncontrast fast spin echo T2W image [1.5 Tesla (TR/TE = 4000 msec./112 msec.) Slice Thickness = 5.00 mm]. c: Axial post contrast spin echo T1W image [1.5 Tesla (TR/TE = 500 msec./14 msec.) Slice Thickness = 5.00 mm, 15 cc Gadobenate Dimeglumine, Multihance]. The sclerotic component on CT scan shows low signal intensity (open arrow) on T1W and T2W images and no enhancement. The fibrous component (dashed arrow) on the other hand is of intermediate signal intensity on both unenhanced sequences and shows avid enhancement following intravenous contrast administration. The soft tissue component seen on CT (Fig. 1) consistent with secretions, has intermediate T1W and bright T2W signal intensity and shows faint peripheral enhancement (asterisks).
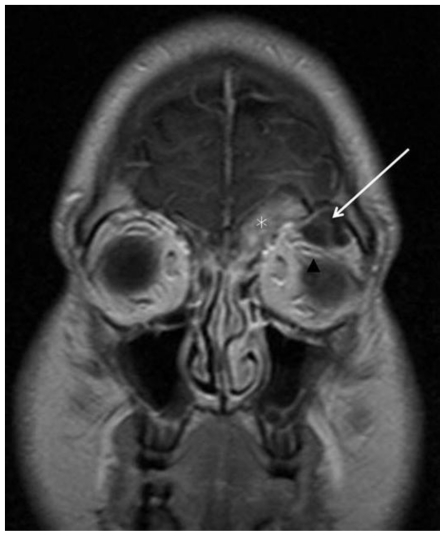
Figure 4.
Coronal T1W spin echo post contrast [1.5 Tesla (TR/TE = 500 msec./14 msec.) Slice Thickness = 6.00 mm, 15 cc, Gadobenate Dimeglumine, Multihance) clearly shows the enhancing fibrous component extending into the left frontoethmoid recess (asterisk) while the sclerotic non enhancing component extends through the left orbital roof (arrow) and causes mass effect on the superior rectus muscle (arrow head).
Figure 5.
23-year-old male patient with frontal sinus osteoblastoma who presented with headache and blurry vision in left eye. a: Axial non enhanced CT images through the orbits, performed on presentation shows that the posterior wall of the left globe (arrow) is at the level of the interzygomatic line (white line), while the normal right counterpart is slightly more posterior. Findings are those of proptosis of the left globe.(Technique: KVp = 120; mA = 37; Slice Thickness = 5.00 mm). b: Axial non enhanced CT image through the orbits (same level as in “a”) done 2 months post operatively shows resolution of proptosis. The posterior wall of the left globe (arrow) is now posterior to the interzygomatic line and is now symmetric to the right counterpart. (Technique: KVp = 120; mA = 350; Slice Thickness = 5.00 mm)
A bicoronal craniotomy, tumor resection and cranioplasty were subsequently done under general anesthesia. Multiple fragments of fibrotic, membranous and bony tissue measuring 7.0 × 6.0 × 3.0 cm in aggregate were resected and submitted for microscopic examination. The tumor consisted of anastomosing, irregular, sclerotic bony trabeculae rimmed with osteoblasts. The intertrabecular spaces were occupied by hypocellular stroma made up of innocuous appearing spindle cells and capillaries. The morphologic features were indistinguishable from osteoid osteoma. A diagnosis of osteoblastoma was made solely on the basis of tumor size (Fig 6). Post operative imaging showed complete resection of tumor and gradual decrease in proptosis that completely resolved on the two-month follow-up CT examination (Fig 5).
Figure 6.
23-year-old male patient with frontal sinus osteoblastoma who presented with headache and blurry vision in left eye. Hematoxylin and Eosin stained section of the surgically resected frontal sinus tumor showing sclerotic lamellar bony trabeculae rimmed with osteoblasts (arrows) and intertrabecular loose fibrovascular stroma. (Original magnification x 400).
DISCUSSION
Osteoblastoma was recognized as a separate pathologic entity, independently by Jaffe (3) and Lichtenstein (4) in 1956. It is an uncommon primary osseous tumor involving predominantly the vertebral column and the long bones (1). Unlike fibrous dysplasias, which may have a similar radiological appearance, craniofacial osteoblastoma is extremely rare with only twenty four cases of nasal cavity and paranasal sinus osteoblastomas reported (2,5–27) (Table 1). These included eight ethmoid sinus, seven maxillary sinus, five nasal cavity, and four frontal sinus lesions; none of the frontal sinus lesions was reported in the English literature (5,6,8,26). The affected population ages ranged between 3 and 69 years with only two patients older than 30 years (age is not available from one case (5)). This is similar to the reported age distribution of osteoblastoma elsewhere in the body (28). There was no sex predilection, however, (gender is not available from two cases (5,11)), in contradistinction to the reported male predominance of two to one in the vertebra and long bones (28). The reported presenting symptoms were headache, facial swelling, as well as nasal obstruction and epistaxis when the nasal cavity was involved, and signs and symptoms related to orbital involvement such as exophthalmos, epiphoria, and orbital pain. Our patient had in addition to headache, acutely blurred vision in the left eye, a previously unreported presentation. This may be due to the mass effect on the orbital structures, although the extraocular muscle movement was reported to be within normal on physical exam.
Table 1.
Summary of the reported cases of paranasal sinus and nasal cavity osteoblastomas Cases listed by date of publication starting with the oldest M:Male. F:Female. ?:Not Available
| Osteoblastoma Epicenter | Gender | Age (yrs) | Presenting Sign/Symptom | Authors reference |
|---|---|---|---|---|
| Frontal sinus | ? | ? | ? | Vensi 5 |
| Frontal sinus | M | 21 | Headache | Korytowski et al. 6 |
| Ethmoid sinus | F | 12 | Exopthalmos | Fu et al.7 |
| Frontal sinus | M | 11 | Headache | Szlezak et al.8 |
| Ethmoid sinus | M | 13 | Epiphora | Freeman 9 |
| Maxillary sinus | M | 15 | Facial Swelling | Labayle et al. 10 |
| Nasal Cavity | ? | 7 | Nasal obstruction | Goberna Burguera et al. 11 |
| Maxillary Sinus | F | 30 | Facial Swelling | Chatterji et al. 12 |
| Maxillary Sinus | M | 23 | Epiphora | Bilaniuk et al. 13 |
| Ethmoid Sinus | F | 69 | Proptosis | Som et al. 14 |
| Maxillary Sinus | M | 22 | Facial Swelling | Tom et al.15 |
| Maxillary Sinus | F | 15 | Facial Swelling | Osguthorpe et al.16 |
| Maxillary Sinus | F | 25 | Expothalmos | Ikawa et al.17 |
| Nasal Cavity | F | 12 | Epistaxis | Ducastelle et al. 18 |
| Ethmoid Sinus | M | 18 | Proptosis | Coscina et al.19 |
| Ethmoid Sinus | M | 14 | Facial Swelling | Sooknundun et al20 |
| Maxillary Sinus | F | 22 | Facial Swelling | Bettinger et al.21 |
| Nasal Cavity | M | 19 | Epistaxis | Chen et al.22 |
| Ethmoid Sinus | M | 9 | Exopthalmos | Ungkanont et al.23 |
| Nasal Cavity | F | 3 | Bulging of nose | Imai et al.24 |
| Ethmoid Sinus | F | 22 | Epistaxis | Velegrakis et al.25 |
| Frontal sinus | F | 16 | Headache | Garstecka et al.26 |
| Ethmoid Sinus | M | 66 | Exopthalmos | Lee et al.27 |
| Ethmoid Sinus | M | 13 | Exopthalmos | Park et al2 |
| Frontal Sinus | M | 23 | Blury vision | Present case |
On imaging, osteoblastomas tend to be expansile and tend to remodel adjacent bone. The reported lesions of the nasal cavity and paranasal sinuses remained fairly well circumscribed without causing significant bone destruction like elsewhere in the skeleton (27). However due to its anatomic proximity to vital structures, paranasal osteoblastomas, when large, tend to be symptomatic. Lesions tend to have mixed components with a dense sclerotic portion and a fibrous portion (27). The main differential diagnosis includes fibrous dysplasia, which, due to its relatively higher incidence, is considered first radiologically when a similar such lesion is encountered. The entities may be difficult to differentiate on CT but the mixed osseous and fibrous appearance of an osteoblastoma tends to be more nodular and coarsely organized than that of most fibrous dysplasias (29). On MR imaging the sclerotic component of the lesion will demonstrate signal void and no enhancement (2). The fibrous component, on the other hand, will demonstrate low to intermediate signal intensity on both T1W and T2W images and intense enhancement following the administration of intravenous contrast (2). The enhancement pattern also helps differentiate osteoblastoma from fibrous dysplasia which generally enhances along the margin of the lesion (29). The major role of MRI is to carefully evaluate the involvement of the adjacent vital structures mainly the intra-orbital structures as part of pre-operative assessment.
Histologically, osteoblastoma resembles an osteoid osteoma, from which it is separated purely on the basis of size. Arbitrarily, a lesion that is smaller than 1.5 cm is considered an osteoid osteoma, and a lesion that is larger than 1.5 cm is considered an osteoblastoma. Both lesions are well circumscribed and associated with sclerosis.
TEACHING POINT
Osteoblastoma is a rare benign bone tumor arising predominantly in the vertebrae or long tubular bones, but can be rarely seen in craniofacial bones. We reported the first case in the English literature, arising in both frontal sinuses in a 23-year-old male patient. This entity may have similar radiologic appearance to fibrous dysplasia and histologic appearance to osteoid osteoma and should be included in the differential of a mixed sclerotic and fibrous lesion of the paranasal sinuses.
ABBREVIATIONS
- CC
Craniocaudal
- CT
Computed tomography
- MRI
Magnetic resonance imaging
- FLAIR
Fluid-Attenuated Inversion Recovery
- Cm
Centimeters
- T1W
T1-weighted
- T2W
T2-weighted
- TR
Repetition Time
- TE
Echo time
- msec.
Millisecond
REFERENCES
- 1.Unni KK, Inwards CY, Bridge JA, Kindblom LG, Wold LE. AFIP Atlas of tumor pathology, Series 4. Washington DC: Armed Forces Institute of Pathology; 2005. Tumors of the bones and joints; pp. 126–35. [Google Scholar]
- 2.Park YK, Kim EJ, Kim SW. Osteoblastoma of the ethmoid sinus. Skeletal Radiol. 2007;36:463–467. doi: 10.1007/s00256-006-0269-z. [DOI] [PubMed] [Google Scholar]
- 3.Jafe HL. Benign osteoblastoma. Bull Hosp Joint Dis. 1956;17:141–51. [PubMed] [Google Scholar]
- 4.Lichtenstein L. Benign osteoblastoma: a category of osteoid- and bone-forming tumors other than classical osteoid osteoma, which may be mistaken for giant-cell tumor or osteogenic sarcoma. Cancer. 1956;9:1044–52. doi: 10.1002/1097-0142(195609/10)9:5<1044::aid-cncr2820090523>3.0.co;2-o. [DOI] [PubMed] [Google Scholar]
- 5.Vensi E. Multiple benign osteoblastoma of the femur and frontal sinus. Ann Laringol Otol Rinol Faringol. 1965;64(6):768–77. [PubMed] [Google Scholar]
- 6.Korytowski J, Dulczynski B, Przybora L. Case of frontal sinus osteoblastoma. Otolaryngol Pol. 1974;28:575–9. (Polish) [PubMed] [Google Scholar]
- 7.Fu YS, Perzin KH. Non-epithelial tumors of the nasal cavity, paranasal sinuses, and nasopharynx. A clinicopathologic study. II. Osseous and fibro-osseous lesions, including osteoma, ossifying fibroma, osteoblastoma, giant cell tumor, and osteosarcoma. Cancer. 1974;33:1289–305. doi: 10.1002/1097-0142(197405)33:5<1289::aid-cncr2820330514>3.0.co;2-p. [DOI] [PubMed] [Google Scholar]
- 8.Szlezak L, Przybora L, Markowska M. Benign osteoblastoma of the ethmoid labyrinth, frontal sinus, and orbit. Klin Oczna. 1975;45:247–51. [PubMed] [Google Scholar]
- 9.Freeman SR. Benign osteoblastoma of the ethmoid bone. Report of a case. Am J Clin Pathol. 1975;63:391–6. doi: 10.1093/ajcp/63.3.391. [DOI] [PubMed] [Google Scholar]
- 10.Labayle J, Bacular J, Chelloul D. Benign osteoblastoma. A propos of a case localized in the upper maxilla. Ann Otolaryngol Chir Cervicofac. 1976;93:661–8. [PubMed] [Google Scholar]
- 11.Goberna Burguera F, Hellin Meseguer D, Roig Riu M, Pastor Rosado J, Blaya Fernandez P, Noguera Moya A, et al. Osteoblastoma of the nasal cavity; a case report. An Esp Pediatr. 1997;46:83–4. [PubMed] [Google Scholar]
- 12.Chatterji P, Purohit GN, Ramdeo Bikaner IN. Benign osteoblastoma of the maxilla (periosteal) J Laryngol Otol. 1978;92:337–45. doi: 10.1017/s002221510008542x. [DOI] [PubMed] [Google Scholar]
- 13.Bilaniuk LT, Zimmerman RA. Computer-assisted tomography: sinus lesions with orbital involvement. Head Neck Surg. 1980;2:293–301. doi: 10.1002/hed.2890020407. [DOI] [PubMed] [Google Scholar]
- 14.Som PM, Bellot P, Blitzer A, Som ML, Geller SA. Osteoblastoma of the ethmoid sinus: the fourth reported case. Arch Otolaryngol. 1979;105:623–5. doi: 10.1001/archotol.1979.00790220057013. [DOI] [PubMed] [Google Scholar]
- 15.Tom LW, Lowry LD, Quinn-Bogard A. Benign osteoblastoma of the maxillary sinus. Otolaryngol Head Neck Surg. 1980;88:397–402. doi: 10.1177/019459988008800414. [DOI] [PubMed] [Google Scholar]
- 16.Osguthorpe JD, Hungerford GD. Benign osteoblastoma of the maxillary sinus. Head Neck Surg. 1983;6:605–9. doi: 10.1002/hed.2890060112. [DOI] [PubMed] [Google Scholar]
- 17.Ikawa T, Kamizaki Y, Ishikawa T. Benign osteoblastoma of the maxillary sinus. Rhinology. 1983;21:373–5. [PubMed] [Google Scholar]
- 18.Ducastelle T, Dehesdin D, Hemet J. Benign subperiosteal osteoblastoma of the nasal cavity. Ann Pathol. 1985;5:131–6. [PubMed] [Google Scholar]
- 19.Coscina WF, Lee BC. Concurrent osteoblastoma and aneurysmal bone cyst of the ethmoid sinus: case report. J Comput Tomogr. 1985;9:347–50. doi: 10.1016/0149-936x(85)90031-1. [DOI] [PubMed] [Google Scholar]
- 20.Sooknundun M, Kacker SK, Kapila K. Benign osteoblastoma of the nasal bones. J Laryngol Otol. 1986;100:229–32. doi: 10.1017/s0022215100099035. [DOI] [PubMed] [Google Scholar]
- 21.Bettinger R, Loerz M. Osteoblastoma of the maxillary sinus. A rare bone lesion? Laryngorhinootologie. 1991;70:275–7. doi: 10.1055/s-2007-998037. [DOI] [PubMed] [Google Scholar]
- 22.Chen KTK, Weinberg RA, Simpson PR, Tschang TP. Osteoblastoma of the nasal cavity. J Laryngol Otol. 1993;107:737–9. doi: 10.1017/s0022215100124296. [DOI] [PubMed] [Google Scholar]
- 23.Ungkanont K, Chanyavanich V, Benjarasamerote S, Tantinikorn W, Vitavasiri A. Osteoblastoma of the ethmoid sinus in a nine-year-old child-an unusual occurrence. Int J Pediatr Otorhinolaryngol. 1996;38:89–95. doi: 10.1016/s0165-5876(96)01415-2. [DOI] [PubMed] [Google Scholar]
- 24.Imai K, Tsujiguchi K, Toda C, Sung KC, Tajima S, Sakamoto H, et al. Osteoblastoma of the nasal cavity invading the anterior skull base in a young child. J Neurosurg. 1997;87:625–8. doi: 10.3171/jns.1997.87.4.0625. [DOI] [PubMed] [Google Scholar]
- 25.Velegrakis GA, Prokopakis EP, Papadakis CE, Karampekios SK, Koutsoubi KG, Helidonis ES. Osteoblastoma of the nasal cavity arising from the perpendicular plate of the ethmoid bone. J Laryngol Otol. 1997;111:865–8. doi: 10.1017/s0022215100138836. [DOI] [PubMed] [Google Scholar]
- 26.Garstecka A, Mackiewicz-Nartowicz H, Szukalski J. Benign osteoblastoma of the frontal sinus. Otolaryngol Pol. 2004;58:649–52. (Polish) [PubMed] [Google Scholar]
- 27.Lee EJ, Park CS, Song SY, Park NH, Kim MS. Osteoblastoma arising from the ethmoid sinus. AJR Am J Roentgenol. 2004;182:1343–4. doi: 10.2214/ajr.182.5.1821343. [DOI] [PubMed] [Google Scholar]
- 28.Ronald G, Grainger David Allison, Adam Andreas, Dixon Adrian K. Grainger & Allison’s Diagnostic Radiology: A Textbook of Medical Imaging. 4th ed. pp. 1850–1852. [Google Scholar]
- 29.Some PM, Curtin HD. Head and neck imaging. 4th ed. St Louis, MO: Mosby; 2003. pp. 329–30. [Google Scholar]