Abstract
Gout is usually thought of as a peripheral joint disease. However, case reports are available describing gouty lesions in the spine. We report a case of a 51 year old African American woman with no previous history of gout who presented with lower back pain and fever and was found to have multiple small fluid collections in the paraspinal muscles at the L3 to L5 levels on the MRI. She was empirically treated with antibiotics, since the fluid was not accessible for drainage initially. Unsuccessful antibiotic therapy and an episode of peripheral gout during this hospitalization prompted the diagnosis of axial gout as the cause for the paraspinal lesions in this patient. CT guided aspiration of the paraspinal lesions confirmed monosodium urate (gout) crystals under polarized microscopy.
Keywords: Axial gout, spinal lesions, paraspinal abscess, uric acid
CASE REPORT
A 51 year old African American woman with no previous history of gout presented with lower back pain and fever. Lumbar spine radiograph views were negative (Figure 1a and 1b). However MRI showed multiple small fluid collections in the paraspinal muscles at the L3 to L5 levels, the largest of which was at the L4 level on the right measuring approximately 11 × 7 mm in size (Figure 2). She also had increased T2 weighted signal as well as enhancement in the soft tissues posterior to the spine extending from L1 to L5 suggestive of abscess. Interventional Radiology was consulted however drainage could not be done because the fluid collections were considered too small. Because of concern that the patient had abscesses, she was empirically started on piperacillin/tazobactam and vancomycin, and was later changed to vancomycin and ciprofloxacin. Blood cultures were negative and neither transthoracic nor transesophageal echocardiogram revealed vegetations.
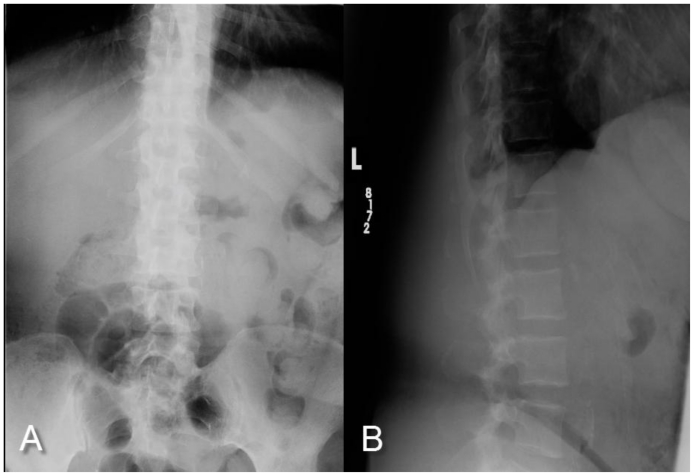
Figure 1.
Radiograph of the lumbar spine AP (A) and Lateral View (B) of 51 year old African American woman with Axial Gouty Arthropathy. There is normal alignment of the lumbar spine. There is no fracture or dislocation seen. The vertebral body heights are normal.
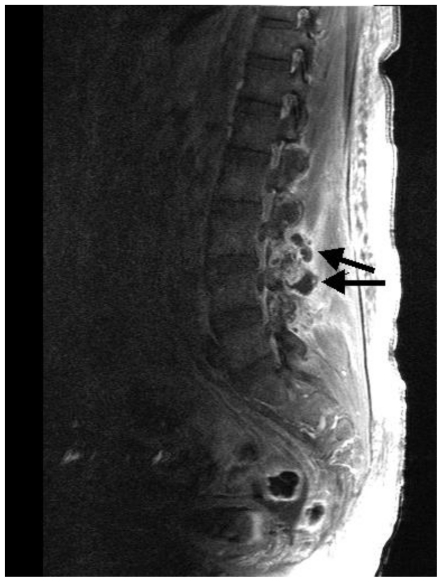
Figure 2.
MRI of lumbar spine of 51 year old African American woman with Axial Gouty Arthropathy- T1 post-contrast (gadolinium) image with fat suppression (sagittal plane) showing multiple small fluid collections in the paraspinal muscles at the L3 to L5 level (Arrows). Technique: Magnet Strength: 1.2 Tesla; Plane: Transverse; with contrast; TR- 588.0; TE 14.0
During this hospitalization, the patient developed acute swelling, warmth and pain in the right shoulder and elbow. An arthrocentesis of the affected elbow joint was performed and gout crystals were seen on synovial fluid analysis. It contained 23,000 white cells with 99% neutrophils. The gram stain and culture were both negative. Serum uric acid was elevated at 13.1. Prednisone 40 mg daily was initiated to treat the peripheral gout since she had chronic renal insufficiency with Creatinine around 1.8 and thus colchicine or NSAIDS were avoided. Prednisone dose was gradually reduced over 2–3 weeks and then stopped.
The patient had a repeat MRI after 4 weeks of the initiation of intravenous antibiotics which still showed the same fluid collections and associated soft tissue involvement. However the lesions appeared to be centered around the facet joints (Figure 3) which prompted the radiologist to suggest the possibility of spinal gout as an etiology given the patient's recent history of peripheral gout and elevated uric acid level.
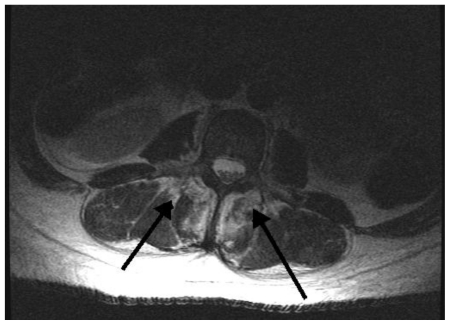
Figure 3.
MRI of lumbar spine of 51 year old African American woman with Axial Gouty Arthropathy- T2 Axial image showing fluid collections (Arrows) and inflammatory changes appear to be centered over the facet joints. Technique: Magnet Strength: 1.2 Tesla; Plane: Transverse; with contrast; TR- 5116.7; TE 104.9
A decision was made to biopsy the lesion under CT guidance (Figure 4). The drained fluid showed uric acid crystals under microscopic analysis and cultures were negative. The pathologic study of the biopsy showed only clotting material. At this point, Allopurinol was started. Unfortunately, the patient was non-compliant with the medication and lost follow-up.
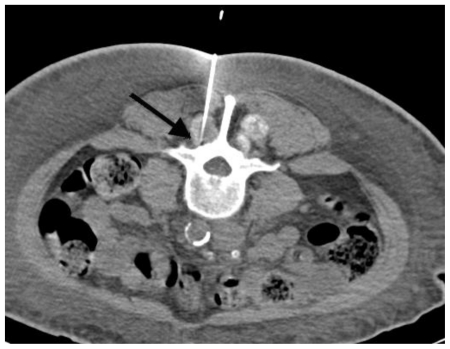
Figure 4.
51-year-old African American woman with Axial Gouty Arthropathy. Non-contrast computed tomographic biopsy (arrow) of the lumbar paraspinal lesion. Technique: 110.0 kV 200.0mA
DISCUSSION
Gout is monosodium urate crystal-induced inflammatory arthritis associated with hyperuricemia. (1). Predisposing factors for an acute attack include trauma, surgery, increasing alcohol intake, high levels of intake of meat and fish and medications including diuretics and cyclosporine. Metabolic syndrome and impaired renal function are common co-morbidities in gout patients. Gout is more common in men with a male to female ratio of 4:1 below the age of 65 and 3:1 above the age of 65 (2).
Gout classically involves the peripheral joints. In 50% of gout cases, the first joint to be involved is the first metatarsophalangeal joint. There are about 125 cases reported in the English literature describing a variety of gouty lesions in the axial spine(3).
In a retrospective review of records of gout patients, approximately 48% of the axial gout patients had involvement of the lumbar vertebrae, 29% the cervical vertebrae and 20% the thoracic vertebrae and 8.7% the sacro-iliac joints (4). The common symptoms of patients with axial gout are back pain with features suggestive of radiculopathy or weakness(5).
It takes years to develop radiographic bony changes secondary to gout. Radiography and CT scan might show paraarticular "punched out" bone erosions often with a thin sclerotic margin which are typical of chronic tophaceous gout. Periosteal new bone formation with classic overhanging edge sign is also seen in tophaceous bone lesions. Bony ankylosis can also occur rarely. Soft-tissue swelling around the involved joints is usually found. Joint space narrowing is not usually seen in gout (3). In MRI of axial gout, low to intermediate signal intensity may be noted in T1 sequence and intermediate to high signal on T2 sequences (3). Lesions are usually enhanced with gadolinium (5). Facet joint erosions in lumbar spine in a patient with gout should raise suspicion for Axial Gouty Arthropathy (3). It is also important to note that urate crystals are not usually radiologically opaque unless they get calcified (3).
Differential diagnosis includes infectious or metastatic process(6) in the spine. Contrast enhancement occurs in gout as well as epidural or paraspinal abscesses. It is difficult to differentiate spinal gout from infectious pathology like epidural abscess (7), paraspinal abscess or osteomyelitis based on imaging modality. History of intravenous drug abuse or immuno-compromised state are more common in epidural abscess than gout. Prior history of positivity to PPD, pulmonary tuberculosis or exposure to a TB patient may be present in a case of Tuberculosis of the spine. Also, thoracic spine is more commonly involved than lumbar spine in Tuberculosis. Destructive changes of two contiguous vertebral bodies with collapse of the intervening disc space is a typical finding in vertebral osteomyelitis (8). CT guided needle biopsy of the lesion with microscopy, gram stain, aerobic, anerobic, mycobacterial and fungal culture of the lesion is needed for final diagnosis.
The medical management of spinal gout is not different from that of acute gout of any other joint. However aggressive lowering of uric acid is essential in the treatment of such patients (9,10). In addition, the spinal gout might need surgical intervention especially if cord compression is an issue (9). Symptoms suggestive of spinal cord compression include radiculopathy, paresthesias, paresis and bladder/bowel dysfunction.
In conclusion, gout should be considered in the differential diagnosis of spine lesions in a patient with risk factors or prior history of gout. This is important clinically, as the treatment and prognosis would obviously be different in gout versus an infectious cause. Early diagnosis would also help avoid unnecessary use of long-term antibiotics.
TEACHING POINT
Gout needs to be considered as one of the differential diagnoses in patients with spinal lesions and risk factors for gout. Lumbar spine is most commonly involved and axial gouty arthropathy typically have facet joint erosions.
Table 1.
Differential diagnoses of axial gouty arthropathy
| DIFFERENTIAL DIAGNOSIS | HISTORY AND CLINICAL FINDINGS | XRAY/CT | MRI |
|---|---|---|---|
| Axial Gouty Athropathy | H/o peripheral gout, tophi, hyperuricemia | Radiography and CT might show paraarticular “punched out” bone erosions often with a thin sclerotic margin which are typical of chronic tophaceous gout. Periosteal new bone formation with classic overhanging edge sign is also seen in tophaceous bone lesions. CT guided aspiration will reveal urate crystals. | Low to intermediate signal intensity may be noted in T1 sequence and intermediate to high signal in T2 sequence. Lesions are usually enhanced with gadolinium. Facet joint erosions in lumbar spine should raise suspicion for axial gout. |
| Infectious process (eg. Epidural abscess, paraspinal abscess, osteomyelitis) | H/O IV drug abuse, immunocompromised state, bacteremia should raise suspicion of infectious process. | Narrowing of disk space and bone lysis are commonly seen in epidural abscess. CT guided aspiration may be gram stain and culture positive for organisms. | MRI delineates both the longitudinal and paraspinal extension of the abscess. Destructive changes of two contiguous vertebral bodies with collapse of the intervening disc space is typical for vertebral osteomyelitis. |
| Tuberculosis spine | Thoracic spine is more commonly involved in TB. PPD + and h/o exposure to TB. | TB involves anterior end plates and results in kyphosis. | Contrast enhanced MRI defines intraspinal extension, focal myelopathy or cord compression. |
| Spinal metastasis | H/o loss of weight, loss of appetite or h/o known primary cancer. | Osteoblastic and osteolytic lesions and pathologic fracture- dislocation. The disk margins usually are spared in contrast to marked disk destruction seen in infectious processes. | Contrast enhanced MRI will delineate the lesions. |
Table 2.
Summary table axial gouty arthropathy
| ETIOLOGY | Gout is monosodium urate crystal-induced inflammatory arthritis associated with hyperuricemia. |
| RISK FACTORS | Predisposing factors for an acute attack include trauma, surgery, increasing alcohol intake, high levels of intake of meat and fish and medications including diuretics and cyclosporine. |
| INCIDENCE | There are about 125 cases reported in the English literature regarding Axial Gouty Arthropathy |
| GENDER RATIO | Male to female ratio of 4:1 below the age of 65 and 3:1 above the age of 65 |
| AGE PREDILECTION | Prevalence increases with age majority being >65 years |
| TREATMENT | Similar to peripheral gout (NSAIDS/Colchicine/Steroid for acute attack; Uric acid lowering agents/uricosuric drugs for chronic gout) However if there are symptoms or signs suggestive of spinal cord compression, then surgery is indicated. |
| PROGNOSIS | Good if diagnosed and treated |
| FINDINGS ON IMAGING | Radiography and CT scan might show paraarticular “punched out” bone erosions often with a thin sclerotic margin which are typical of chronic tophaceous gout. Periosteal new bone formation with classic overhanging edge sign is also seen in tophaceous bone lesions. In MRI of axial gout, low to intermediate signal intensity may be noted in T1 sequence and intermediate to high signal in T2 sequence. Lesions are usually enhanced with gadolinium. Facet joint erosions in lumbar spine should raise suspicion for axial gout. |
ABBREVIATIONS
- CT
Computed Tomography
- MRI
Magnetic Resonance Imaging
- PPD
Purified Protein Derivative
- TB
Tuberculosis
REFERENCES
- 1.Doherty M. New insights into the epidemiology of gout. Rheumatology. 2009 May;48(Suppl 2):ii2–ii8. doi: 10.1093/rheumatology/kep086. [DOI] [PubMed] [Google Scholar]
- 2.Wallace KL, Riedel AA, Joseph-Ridge N, et al. Increasing prevalence of gout and hyperuricemia over 10 years among older adults in a managed care population. J Rheumatol. 2004 Aug;31(8):1582–7. [PubMed] [Google Scholar]
- 3.Saketkoo LA, Robertson HJ, Dyer HR, et al. Axial gouty arthropathy. Am J Med Sci. 2009 Aug;338(2):140–6. doi: 10.1097/MAJ.0b013e3181a3dc14. [DOI] [PubMed] [Google Scholar]
- 4.Konatalapalli RM, Demarco PJ, Jelinek JS, et al. Gout in the axial skeleton. J Rheumatol. 2009 Mar;36(3):609–13. doi: 10.3899/jrheum.080374. [DOI] [PubMed] [Google Scholar]
- 5.Yehia B, Flynn J, Sisson S. Crystal Clear. Am J Med. 2008 Jun;121(6):488–90. doi: 10.1016/j.amjmed.2007.12.013. [DOI] [PubMed] [Google Scholar]
- 6.Chan AT, Leung JL, Sy AN, Wong WW, Lau KY, Ngai WT, Tang VW. Thoracic spinal gout mimicking metastasis. Hong Kong Med J. 2009 Apr;15(2):143–5. [PubMed] [Google Scholar]
- 7.Yen PS, Lin JF, Chen SY, Lin SZ. Tophaceous gout of the lumbar spine mimicking infectious spondylodiscitis and epidural abscess: MR imaging findings. J Clin Neurosci. 2005 Jan;12(1):44–6. doi: 10.1016/j.jocn.2004.03.020. [DOI] [PubMed] [Google Scholar]
- 8.Lew DP, Waldvogel FA. Osteomyelitis. Lancet. 2004 Jul 24;364(9431):369–79. doi: 10.1016/S0140-6736(04)16727-5. [DOI] [PubMed] [Google Scholar]
- 9.Hou LC, Hsu AR. Spinal gout in a renal transplant patient: a case report and literature review. Surg Neurol. 2007 Jan;67(1):65–73. doi: 10.1016/j.surneu.2006.03.038. discussion 73. Epub 2006 Oct 6. [DOI] [PubMed] [Google Scholar]
- 10.Draganescu M, Leventhal L. Spinal Gout: Case Report and Review of the Literature. J Clin Rheumatol. 2004 Apr;10(2):74–79. doi: 10.1097/01.rhu.0000120898.82192.f4. [DOI] [PubMed] [Google Scholar]