Abstract
Isomerism or Heterotaxy syndromes are rare multifaceted congenital anomalies with multi-system involvement. Grouped under the broad category of Situs Ambiguous defects, these often pose diagnostic difficulties due to their varied and confusing anatomy. Since patients rarely survive into adulthood due to cardiovascular complications, the etiology and natural history of such conditions are not fully understood. Imaging provides the most accurate non invasive method for diagnosis and thereby, prognosis in such cases. We present a case of right sided Isomerism with complex cardiac anomalies in a 17 year old adolescent, who presented with dysphagia as one of the main complaints. Multi modality imaging demonstrated the intricate abnormalities in vital systems.
Keywords: Ivemark Syndrome, Isomerism syndrome, asplenia, polysplenia, bilateral right sidedness
CASE REPORT
A 17 year old male was referred with complaints of dysphagia, cough since 4–5 days with one episode of blood in sputum, and episodic exertional breathlessness.
Dysphagia was mainly of insidious onset, progressive and mainly for solids. There was no history of vomiting. Cough was gradual in onset, progressive in nature and increased in the night time. There was one episode of associated blood in sputum which was frank red in colour and of minimal amount. Patient had exertional breathlessness, relieved on resting. On further enquiry, the patient's mother gave positive history of episodes of breathlessness through childhood. History suggestive of cyanotic spells was also present, which apparently would get relieved on squatting. The patient had normal siblings, and normal general developmental milestones.
On examination, tachycardia with pallor, central cyanosis and digital clubbing were present. Systemic examination revealed pre-cordial bulge, right sided apex beat, right sided cardiac dullness, pan-systolic murmur in right 3–5 intercostal space, and ejection systolic murmur in right second intercostals space. A provisional diagnosis of congenital heart disease with dextrocardia was made. Laboratory investigations showed reduced haemoglobin.
Plain radiograph of chest in posterior-anterior view revealed the cardiac silhouette on the right side of thorax with left sided aortic arch. Mid-thoracic scoliosis with convexity towards right side was also noted (Fig. 1).
Figure 1.
A 17 year old male with right Isomerism presenting with dysphagia. Plain radiograph chest in PA view demonstrates dextrocardia (black arrow) with left sided aortic arch (arrowhead) and mid-thoracic scoliosis (white arrow).
Upper GI barium series with diluted barium sulphate suspension revealed partial narrowing of a short segment of thoracic esophagus at the level of aortic arch. Mild proximal dilation of the esophagus was seen. This suggested compression by the aortic arch causing partial mechanical obstruction to the esophagus (Fig. 2).
Figure 2.
A 17 year old male with right Isomerism presenting with dysphagia. Upper GI Barium series with Barium sulphate suspension shows partial smooth narrowing of thoracic esophagus (arrow) due to compression by aortic arch.
Barium filled gastric shadow was seen inferior to the right lobe of the liver and lower down in the right side of abdomen. Duodenal loop was crossing the midline and duodeno-jejunal junction was in the left paravertebral region at L-3 level. Jejunal loops were seen mainly on the left side of the abdomen apparently pushed lower down by a large structure of soft tissue density in the left upper abdomen (Fig. 3). The ileo-colic junction was normally placed in the right iliac region (Fig. 4). Distal gut anatomy was normal. These findings indicated Fore-gut malrotation.
Figure 3.
A 17 year old male with right Isomerism presenting with dysphagia. Upper GI Barium series with Barium sulphate suspension shows stomach placed in the left sub-hepatic region (arrow). The duodeno-jejunal junction is seen slightly to the left of the midline (arrowhead) indicating foregut malrotation.
Figure 4.
A 17 year old male with right Isomerism presenting with dysphagia. Barium meal follow through with Barium sulphate suspension shows normally positioned ileo-colic junction (curved arrow) indicating normal position of hind gut. Jejunal loops are seen predominantly on the left side of the abdomen (straight arrow).
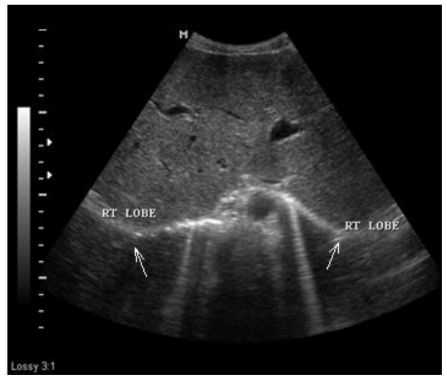
Abdominal Ultrasonography (USG) (MEDISON, SA8000, 3–7 MHz, curvilinear probe) showed midline liver with two morphological right lobes and absent anatomical left lobe. Gall bladder was contracted and in the midline. Spleen was absent (Fig. 5). Right kidney was lower down in the abdomen. Midline portal vein was seen dividing into two right branches to supply bilateral right lobes of liver (Fig. 6). Supra renal inferior vena cava was situated left antero-lateral to the abdominal aorta. Caeliac trunk was not visualised. A large superior mesenteric artery was seen. The foregut arterial supply probably originated from the superior mesenteric artery. Head and part of body of pancreas were present suggestive of truncated pancreas.
Figure 5.
A 17 year old male with right Isomerism presenting with dysphagia. Abdominal USG in axial plane demonstrates midline liver with two right lobes (arrows). (Protocol: Medison, SA8000, 3–7 MHz, curvilinear probe)
Figure 6.
A 17 year old male with right Isomerism presenting with dysphagia. Abdominal USG in axial plane demonstrates midline portal vein branching into two morphological right branches (arrow). (Protocol: Medison SA8000, 3–7 MHz, curvilinear probe).
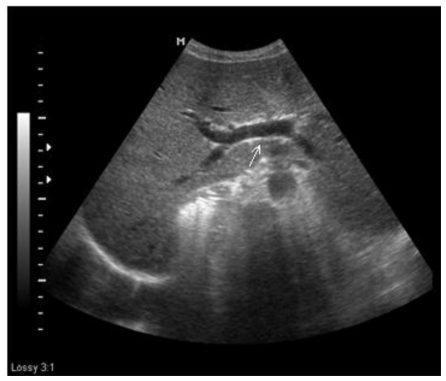
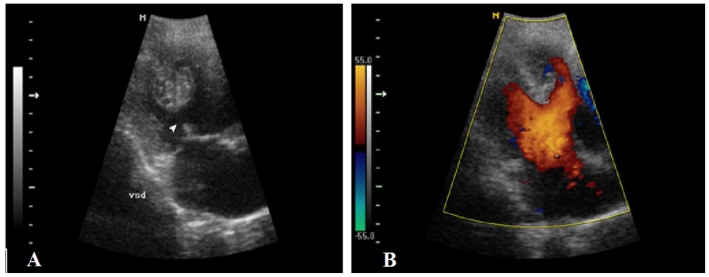
2D Echo (MEDISON, SA8000, 3–7 MHz, curvilinear probe in cardiac mode) demonstrated right sided cardia two morphologically similar right atria with atrial septal defect, a single atrioventricular valve(Fig. 7), a large ventricular septal defect with rudimentary interventricular septum (Fig. 8A and B), double outlet right ventricle, Transposition of great arteries (L type) and pulmonary stenosis.
Figure 7.
A 17 year old male with right Isomerism presenting with dysphagia. 2D Echo demonstrates mono atrioventricular valve (open) (curved arrow). (Protocol: Medison SA8000, 3–7 MHz, curvilinear probe in cardiac mode)
Figure 8.
A 17 year old male with right Isomerism presenting with dysphagia. 2D Echo demonstrates a large VSD (arrowhead) (A), and biventricular flow from the atria (B). (Protocol: Medison SA8000, 3–7 MHz, curvilinear probe in cardiac mode)
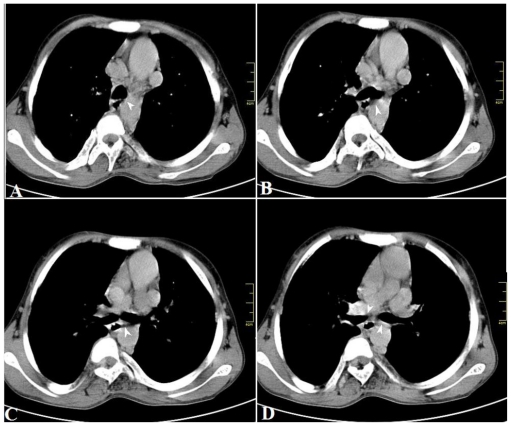
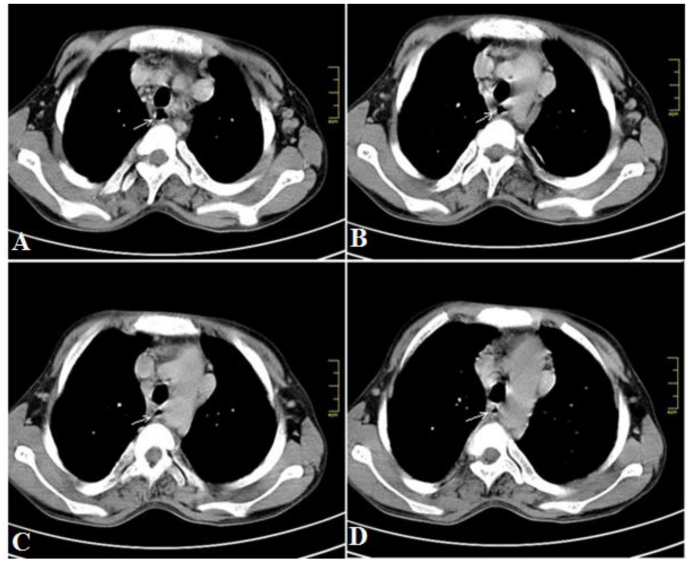
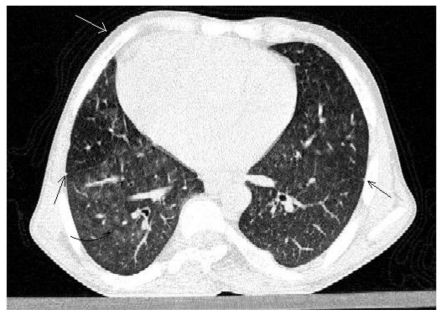
Computed tomography (CT) (SIEMENS, SOMATOM, dual slice CT) chest and abdomen were done. Non contrast CT thorax in mediastinal window demonstrated the heart predominantly in the right hemi thorax and bilateral eparterial bronchi (Fig. 9). Bilateral superior vena cavae draining into the two atria were also seen. Progressive esophageal narrowing is seen at the level of aortic arch (Fig. 10). HRCT Lung demonstrated symmetrical fissures on both sides (Fig. 11). Right lung fields showed features of cotton wool spots suggesting alveolar haemorrhage which could explain the patient's haemoptysis (Fig. 11).
Figure 9.
A 17 year old male with right Isomerism presenting with dysphagia. Non contrast axial CT scan of thorax in mediastinal window, at the level of tracheal bifurcation(A, B) demonstrate main bronchi (C, D) branching from trachea (arrowheads). At no level are the pulmonary arteries seen crossing superior to the main bronchi, thus indicating eparterial bronchi on both sides. (Protocol: Siemens Somatom, dual slice CT at 90 mAs and 130 kV, 5 mm slice thickness, non contrast).
Figure 10.
A 17 year old male with right Isomerism presenting with dysphagia. Non contrast axial CT of the thorax in mediastinal window. Serial axial sections at the level of aortic arch demonstrate the progressive narrowing of esophagus (arrow). (Protocol: Siemens Somatom, dual slice CT at 90 mAs and 130 kV, 5 mm slice thickness, non contrast).
Figure 11.
A 17 year old male with right Isomerism presenting with dysphagia. HRCT thorax demonstrates dextrocardia (white arrow) and symmetrical fissures in both lungs indicating bilateral right lungs (black straight arrows). Cotton wool spots of alveolar haemorrhage were noted in the right lung fields (black curved arrow). (Protocol: Siemens Somatom, dual slice CT at 90 mAs, 130 kV and 5 mm slice thickness).
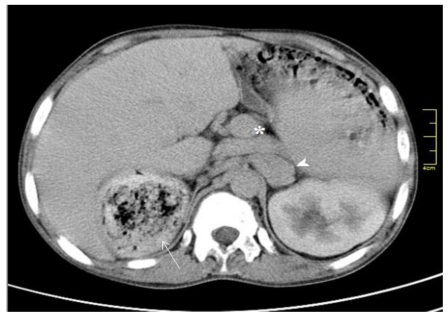
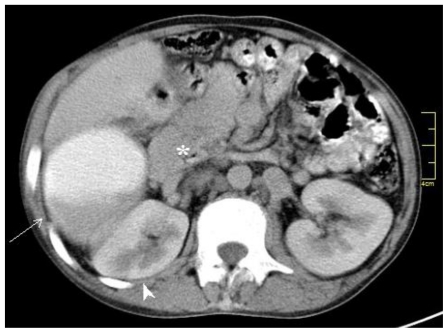
Contrast enhanced CT Abdomen with 60ml i.v contrast (OMNIPAQUE, GE Healthcare, Ireland) confirmed the USG findings viz, large liver, crossing over to contralateral side of abdomen, appearing as bilateral right lobes. USG findings of absent spleen, stomach on the right side of abdomen and midline portal vein were confirmed on CT. Inferior vena cava was left anterolateral to the aorta and both vessels were on left side of spine (piggy-back IVC) (Fig. 12). Celiac trunk was again not visualised. A large Superior mesenteric arterial trunk was noted. Truncated pancreas was present in which only head and part of body were seen (Fig. 13). The right Kidney was much lower than the left, being displaced inferiorly by the stomach and liver. Consequently the right renal vein was seen to drain with an elongated trunk into the IVC as was noted on coronal reconstructed image of CT abdomen (Fig. 14).
Figure 12.
A 17 year old male with right Isomerism presenting with dysphagia. Contrast enhanced CT abdomen demonstrates stomach on the right side of abdomen (white arrow), midline portal vein (*), piggy back IVC (arrowhead). (Protocol: Siemens Somatom, dual slice CT at 96 mAs and 136 kV, 5 mm slice thickness, contrast enhanced with 60 ml of intravenous Omnipaque).
Figure 13.
A 17 year old male with right Isomerism presenting with dysphagia. Contrast enhanced axial CT abdomen demonstrates stomach on the right side of abdomen (white arrow), right kidney inferior to the stomach (arrowhead), and truncated pancreas (*). (Protocol: Siemens Somatom, dual slice CT at 96 mAs and 136 kV, 5 mm slice thickness, contrast enhanced with oral contrast 500 ml 2% diluted Omnipaque, and intravenous 60 ml Omnipaque).
Figure 14.
A 17 year old male with right Isomerism presenting with dysphagia. Coronal reconstructed CT abdomen shows stomach in right subhepatic region (arrowhead), an inferiorly pushed right kidney(*) with long right renal vein (arrow). (Protocol: Siemens Somatom, dual slice CT at 96 mAs and 136 kV, 5 mm slice thickness, coronal reconstruction)
Coronal T2 weighted FSE Magnetic Resonance (GE SIGNA PROFILE 0.2T MRI) images of chest in coronal plane showed dextrocardia with bilateral superior vena cava entering into the atria and a large atrial septal defect (Fig. 15). The right ventricular wall was hypertrophied and the systemic aorta was seen emerging from it (Fig. 16).
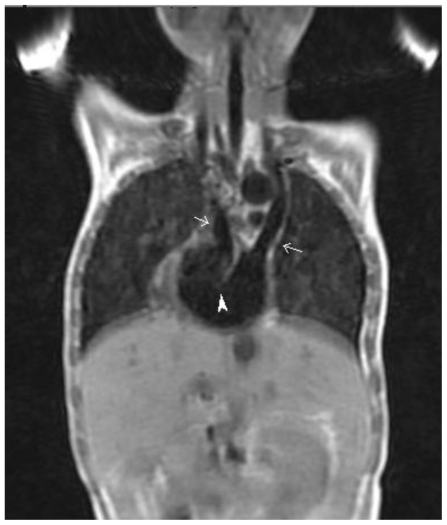
Figure 15.
A 17 year old male with right Isomerism presenting with dysphagia. Coronal T1 weighted MR scan demonstrates bilateral superior vena cava (arrows) draining into both atria. A large atrial septal defect (arrowhead) is also demonstrated. (Protocol: GE SIGNA PROFILE 0.2T MRI at TE 16 ms, TR 520 ms, non contrast).
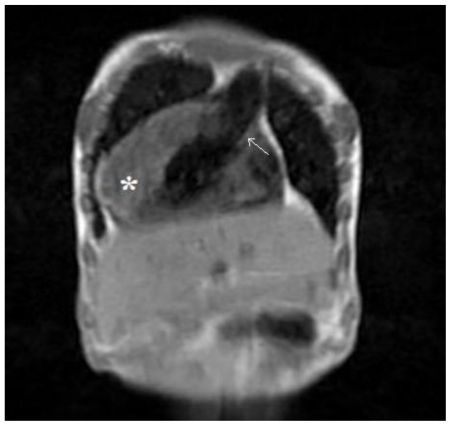
Figure 16.
A 17 year old male with right Isomerism presenting with dysphagia. Coronal T1 weighted MR scan demonstrates thickened myocardial wall of right ventricle (*) from which systemic aorta is seen arising (arrow). (Protocol: GE SIGNA PROFILE 0.2T MRI at TE 16 ms, TR 520 ms, non contrast).
DISCUSSION
The normal arrangement of internal organs in the body is called Situs Solitus [1]. Abnormality in this arrangement classified into Situs inversus and Situs ambiguous varieties. Situs inversus totalis is a mirror image of the normal situs where all internal organs occupy the corresponding contralateral side and are otherwise normal. These individuals are incidentally discovered. Situs ambiguous are the intermediate presentations between Situs solitus and situs inversus. Due to the varied nature of anomalies in situs ambiguous, they are known by various names viz, Heterotaxy, Isomerism syndromes, Asplenia syndrome, Polysplenia syndrome and so on [2]. These laterality disorders are probably due to disturbances in midline primary developmental field [3].
Two major categories in the Heterotaxy syndromes are the left isomerism (Polysplenia syndrome) and right isomerism (Asplenia syndromes or Ivemark syndrome). Left isomerism is seen more in females and mostly present with acyanotic congenital heart disease. Their anatomy are characterized by only major fissures in both lungs, bilateral hyparterial bronchi, congenital cardiac anomalies such as ASD and VSD, interrupted IVC with azygous continuation into thorax (the Double-vessel sign)[4], multiple spleens, gut malrotation, and biliary atresia. Most patients survive up to mid adolescence [5,6].
Right isomerism (Ivemark syndrome) is seen more in males, presents mostly with cyanotic heart disease and patients are immunocompromised due to absent spleen. Majority are characterised by bilateral superior vena cava draining into bilateral atria, both lungs with major and minor fissures, bilateral eparterial bronchi, complex cardiovascular anomalies such as TAPVC, TGA, common AV valve etc., absent spleen, midline symmetrical liver with midline gall bladder, gut malrotation, piggy-back IVC [7], and truncated pancreas. Most patients with right isomerism succumb within the first year of life due to cardiovascular compromise [5,7]. Survival into adulthood can be explained by less severe pulmonary stenosis, absence of arrhythmias or overwhelming infections [8]. However, to the best of our knowledge, there is no convincing literature yet to explain the exact cause of survival in patients that do survive.
MRI of chest is particularly important in such syndromes as it can clearly delineate cardio-vascular anatomy due to superior soft tissue contrast and has an additional advantage of no radiation.
Management is mainly palliative. Surgical options include systemic-pulmonary shunting of de-oxygenated blood (bidirectional Glenn procedure), Blalock-Taussig shunt and TAPVC repair [9]. Prophylaxis against infection by capsulated organisms also may be needed.
In the present case, 17 year old adolescent male with right isomerism presented with dysphagia, cough and episodes of breathlessness, central cyanosis and clubbing.
Multi system abnormalities discussed under right isomerism were observed on imaging as previously mentioned. However dysphagia as a presenting symptom of right isomerism has not been reported in current literature.
TEACHING POINT
Right isomerism is a spectrum of rare congenital anomalies such as TEACHING POINTcomplex cardiac malformations, asplenia, gut malrotation etc. resulting from abnormal laterality orientation, wherein patients rarely survive into adulthood. Early diagnosis is possible by imaging, especially chest MRI, owing to its better depiction of cardiovascular anatomy.
Table 1.
Summary table for right isomerism
| Aetiology | Congenital with multi-factorial inheritance |
| Incidence | 1:1750 to 1:40000 live births |
| Gender ratio | Male> female |
| Age predilection | Infancy |
| Risk factors | Unknown |
| Treatment | Surgical correction ( Developmental stages) |
| Prognosis | Poor ( 80 % die within first year) |
| Findings on imaging | USG, CT and MRI show Bilateral superior vena cava draining into bilateral atria, both lungs with major and minor fissures, bilateral eparterial bronchi, complex cardiovascular anomalies such as TAPVC, TGA, common AV valve etc., absent spleen, midline symmetrical liver with midline gall bladder, gut malrotation, piggy-back IVC [7], and truncated pancreas. |
Table 2.
Differential diagnosis table for right isomerism (continued on next page)
| Disease | X-Ray | Echocardiography | USG | CT | MRI |
|---|---|---|---|---|---|
| Right Isomerism (asplenia syndrome) | Cardiac apex – right/left/midline, Aortic arch-right/left Major and minor fissures in both lungs Stomach-midline/right/left |
Cardiac apex-right/left/midline Both atrium has right atrium morphology with or without ASD Common atrioventricular valve Transposition of great arteries Pulmonary stenosis Bilateral SVC TAPVC IVC & aorta on same side of spine |
Absent spleen Symmetrical & midline liver & midline gall bladder Ipsilateral IVC & aorta Stomach-midline/right/left Gut malrotation Truncated pancreas |
Cardiac apex-right/left/midline Transposition of great arteries Bilateral SVC TAPVC Piggy backed IVC Aortic arch-right/left Bilateral eparterial bronchi Major and minor fissures in both lungs Absent spleen Symmetrical & midline liver & midline gall bladder, Gut malrotation Truncated pancreas |
Cardiac apex-right/left/midline Transposition of great arteries Bilateral SVC TAPVC Piggy backed IVC Aortic arch-right/left Bilateral eparterial bronchi Absent spleen Symmetrical & midline liver & midline gall bladder Gut malrotation Truncated pancreas |
| Left Isomerism (polysplenia syndrome) | Cardiac apex-right/left Aortic arch-right/left Bilateral hyparterial bronchi Absent bilateral minor fissure Stomach-right/left |
Cardiac apex-right/left ASD Normal atrioventricular valve in most cases VSD Normal relationship of great arteries IVC & aorta relationship is normal |
Multiple spleens Biliary atresia Liver-right/left/midline Interrupted IVC with double vessel sign Gut malrotation Truncated pancreas |
Cardiac apex-right/left Aortic arch-right/left Normal relationship of great arteries IVC & aorta relationship is normal Bilateral hyparterial bronchi Absent bilateral minor fissure Multiple spleens Biliary atresia Liver-right/left/midline Interrupted IVC with double vessel sign Gut malrotation Truncated pancreas |
Cardiac apex-right/left Aortic arch-right/left Normal relationship of great arteries IVC & aorta relationship is normal Bilateral hyparterial bronchi Multiple spleens Biliary atresia Liver-right/left/midline Interrupted IVC with double vessel sign Gut malrotation Truncated pancreas |
| Situs Inversus Totalis | Cardiac apex-right Aortic arch-right Right hyparterial & left eparterial bronchus Minor fissure on left side Stomach-right side |
Cardiac apex-right Right atrium & ventricle on left side Left atrium & ventricle on right side Corrected transposition of great arteries Right side aorta & left side IVC |
Right side spleen Left side liver Left side gall bladder Right side stomach |
Cardiac apex-right Aortic arch-right Corrected transposition of great arteries Right side aorta & left side IVC Right hyparterial & left eparterial bronchus Minor fissure on left side Right side spleen Left side liver Left side gall bladder Right side stomach |
Cardiac apex-right Aortic arch-right Corrected transposition of great arteries Right side aorta & left side IVC Right hyparterial & left eparterial bronchus Right side spleen Left side liver Left side gall bladder Right side stomach |
ABBREVIATIONS
- USG
Ultrasonography
- CT
Computed Tomography
- MR
Magnetic Resonance
- HRCT
High Resolution CT
- ASD
Atrial Septal Defect
- VSD
Ventricular Septal Defect
- TAPVC
Total Anomalous Pulmonary Venous Drainage
- TGA
Transposition of Great Vessels
- IVC
Inferior Vena cava
- SVC
Superior vena cava
- GI
Gastro Intestinal
REFERENCES
- 1.Maldjian PD, Saric M. Approach to dextrocardia in adults: review. AJR Am J Roentgenol. 2007 Jun;188(6 suppl):S39–49. doi: 10.2214/AJR.06.1179. quiz S35–8. [DOI] [PubMed] [Google Scholar]
- 2.Casey B. Two rights make a wrong: human left-right malformations. Hum Mol Genet. 1998;7(10):1565–71. doi: 10.1093/hmg/7.10.1565. [DOI] [PubMed] [Google Scholar]
- 3.Martínez-Frías ML. Primary midline developmental field. I. Clinical and epidemiological characteristics. Am J Med Genet. 1995 May 8;56(4):374–81. doi: 10.1002/ajmg.1320560406. [DOI] [PubMed] [Google Scholar]
- 4.Sheley RC, Nyberg DA, Kapur R. Azygous continuation of the interrupted inferior vena cava: a clue to prenatal diagnosis of the cardiosplenic syndromes. J Ultrasound Med. 1995;14:381–7. doi: 10.7863/jum.1995.14.5.381. [DOI] [PubMed] [Google Scholar]
- 5.Applegate, et al. Situs Revisited: Imaging of the Heterotaxy Syndrome. Radiographics. 1999 Jul;19(4):837–852. doi: 10.1148/radiographics.19.4.g99jl31837. [DOI] [PubMed] [Google Scholar]
- 6.Ivemark BI. Implications of agenesis of the spleen on the pathogenesis of conotruncus anomalies in childhood: an analysis of the heart malformations in the splenic agenesis syndrome, with fourteen new cases. Acta Paediatr. 1955;44:7–110. [PubMed] [Google Scholar]
- 7.Tonkin IL, Tonkin AK. Visceroatrial situs abnormalities: sonographic and computed tomographic appearance. AJR Am J Roentgenol. 1982 Mar;138(3):509–15. doi: 10.2214/ajr.138.3.509. [DOI] [PubMed] [Google Scholar]
- 8.Matsuura K, et al. A case of right isomerism showing long survival without surgery. South Med J. 2007 Feb;100(2):218–21. doi: 10.1097/01.smj.0000242349.55168.a7. [DOI] [PubMed] [Google Scholar]
- 9.Takeuchi K, Murakami A, Hirata Y, et al. Surgical outcome of heterotaxy syndrome in a single institution. Asian Cardiovasc Thorac Ann. 2006 Dec;14(6):489–94. doi: 10.1177/021849230601400610. [DOI] [PubMed] [Google Scholar]