Abstract
Most pancreatic arteriovenous malformations (PAVM) present due to gastrointestinal bleeding or abdominal pain, but these patients may be asymptomatic. Increased portal vein flow from these malformations can lead to portal hypertension and gastrointestinal bleeding. Diagnosis is often made by imaging, and early diagnosis has led to successful surgical resection or percutaneous embolization. We report a patient with PAVM, diagnosed by CT and angiography, who has remained asymptomatic for 2 years without treatment.
Keywords: arteriovenous malformation, AVM, pancreas
CASE REPORT
An asymptomatic 52-year-old man underwent upper abdominal CT for a 2 cm lesion of the right lobe of the liver identified by sonography. Numerous foci of pancreatic hyperenhancement with early portal venous opacification were demonstrated (Fig. 1). There was also duplication of the inferior vena cava with azygos continuation (Fig. 2). Subsequent angiography including superselective injections confirmed the diagnosis of pancreatic arteriovenous malformation (PAVM) and provided details of the vascular supply and drainage of the anomaly (Fig. 3). The malformation was supplied by branches of the gastroduodenal, splenic and middle colic arteries with immediate shunting to the portal vein. An octreotide scan was negative. The patient had no bleeding, abdominal pain, or abnormal liver function studies to suggest cirrhosis or portal hypertension. Therefore, no treatment was undertaken. Follow up CT four months later showed the lesion to be stable. At 2 year follow-up, the patient remains asymptomatic.
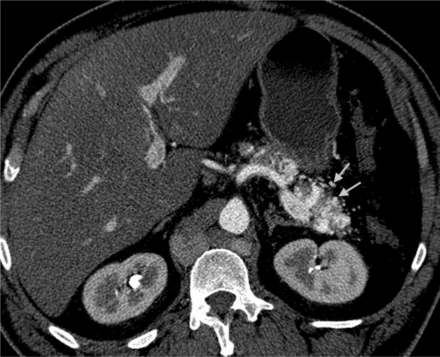
Figure 1.
Upper abdominal computed tomography. 52 year old male with pancreatic arteriovenous malformation. Early axial arterial image shows multiple irregular pancreatic body and tail arteries (arrows). (Protocol: kVp-140, mA-376, slice thickness 2.5 mm, iohexol 300 mgi/ml, 100 ml)
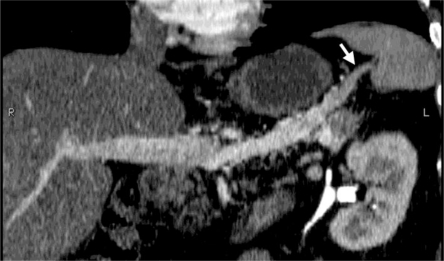
Figure 2.
Upper abdominal computed tomography. 52 year old male with pancreatic arteriovenous malformation. Curved reformatted coronal image shows opacification of the splenic vein along the pancreas but not at the splenic hilum (arrow) indicating that opacification is not from the spleen. (Protocol: kVp-140, mA-376, slice thickness 2.5 mm, iohexol 300 mgi/ml, 100 ml)
Figure 3.
Upper abdominal computed tomography. 52 year old male with pancreatic arteriovenous malformation. Portal venous phase axial image shows uniform pancreatic enhancement (arrows). The arteries of the vascular malformation are not visible. (Protocol: kVp-140, mA-376, slice thickness 2.5 mm, iohexol 300 mgi/ml, 100 ml)
DISCUSSION
Pancreatic arteriovenous malformations are rare, with fewer than 100 reported cases (1). PAVMs can be congenital or acquired. As many as 15% of patients with hereditary hemorrhagic telangiectasia (HHT) studied with CT have PAVMs, but the lesions have been small incidental findings (2). The patient reported here had duplication of the inferior vena cava with azygos continuation, but associated congenital anomalies other than hereditary telangiectasia have not been reported. The relationship of these two anomalies in this patient is unknown. Acquired etiologies of PAVM have included neoplasms, inflammation, trauma and complication of pancreatic transplant (3). It has been hypothesized that patients with no other hereditary disease or primary condition may have a congenital PAVM that is a persistent remnant of the fetal pancreatic vascular network.
In a 2007 literature review of 90 patients, the mean age of patients with PAVM was 52.5 years (7 mo-73years), M:F;73:17. 14/90 (16%) were asymptomatic. 48/90 (54%) presented with gastrointestinal bleeding, 29/90(32%) with abdominal pain or discomfort, and 4/90 (5%) with jaundice (1).
The etiology of gastrointestinal hemorrhage, the most common presentation, can be due to direct hemorrhage from PAVM into the pancreatic duct or a bile duct, hemorrhage from an AVM involving the bowel wall, an associated duodenal ulcer or the result of varices due to portal hypertension. Portal hypertension with varices of the esophagus, stomach or duodenum is a late complication of PAVM. The incidence of gastrointestinal bleeding due to varices has ranged from 12–23% (4,5). In a 2006 literature review of 51 patients, 6/51 (12%) presented with pancreatitis (4). Pancreatitis has been attributed to bleeding into the pancreatic duct (6) or PAVM with vascular steal leading to ischemia (7).
PAVM has been diagnosed by CT, MR imaging, sonography, and angiography. CT findings include multiple discrete intrapancreatic vessels, best demonstrated on early arterial scanning. Multiple feeding vessels are often associated with early portal vein opacification. (Fig. 2) Reformatted MIP (maximum intensity projection) and volume rendered images may be useful. If scanning is only done in the portal venous phase however, the diagnosis may difficult due to dense pancreatic parenchymal enhancement coupled with less conspicuous feeding vessel enhancement.
The diagnostic findings can also be demonstrated by MR imaging. On sonography, the abnormal vessels appear as nonspecific hypoechoic nodules, but Doppler ultrasound can demonstrate a mosaic pancreatic color flow pattern and pulsatile portal vein waveforms. Angiography is invasive, but can provide detailed depiction of all supplying vessels. This information can be used to determine if treatment by embolization is feasible and also provide a road map for interventional procedures or surgical planning. Multiple feeding vessels may preclude embolization.
The differential diagnosis for pancreatic arteriovenous malformation is primarily hypervascular tumors such as islet cell tumors, and hypervascular metastases. These entities can generally be differentiated from pancreatic arteriovenous malformation by their discrete nature. Rarely, an atypical appearance of chronic pancreatitis, or an intrapancreatic accessory spleen may mimick pancreatic arteriovenous malformation.
Treatment of symptomatic patients, including patients with varices and gastrointestinal bleeding has included arterial embolization, transjugular intrahepatic portosystemic shunting (TIPS), vascular ligation and pancreatic resection. A literature review reported that 22/90 (24%) patients were treated conservatively while 60/90 (67%) had interventions, most often pancreatic resection 35/90 (39%) and arterial embolization 15/90 (17%) (1).
PAVM is rare cause of gastrointestinal hemorrhage, but is in the differential diagnosis when the common etiologies have been excluded. In some patients, as with the patient presented here, the diagnosis is made by serendipity. These asymptomatic patients have been treated conservatively and followed. However, if patients develop symptoms or have evidence of portal hypertension, consideration of intervention is warranted.
TEACHING POINT
Pancreatic arteriovenous malformations are a rare cause of gastrointestinal bleeding. CT findings include multiple discrete intrapancreatic vessels best demonstrated on early arterial scanning and multiple feeding vessels associated with early portal vein opacification.
Figure 4.
Upper abdominal computed tomography. 52 year old male with pancreatic arteriovenous malformation. Coronal reformatted arterial phase image showing duplicated IVC with azygos continuation. Right (R) and left (L) IVC components lead to the azygos vein (A). (Protocol: kVp-140, mA-376, slice thickness 2.5 mm, iohexol 300 mgi/ml, 100 ml)
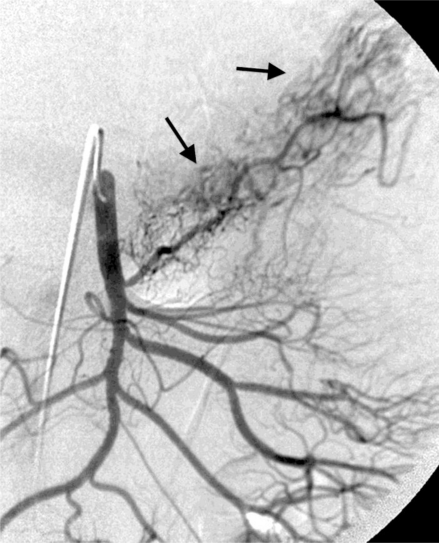
Figure 5.
Mesenteric angiogram. 52 year old male with pancreatic arteriovenous malformation. Frontal projection selective superior mesenteric artery injection shows a racemose vascular network in the body and tail of the pancreas. (Iohexol 300 mgi/ml)
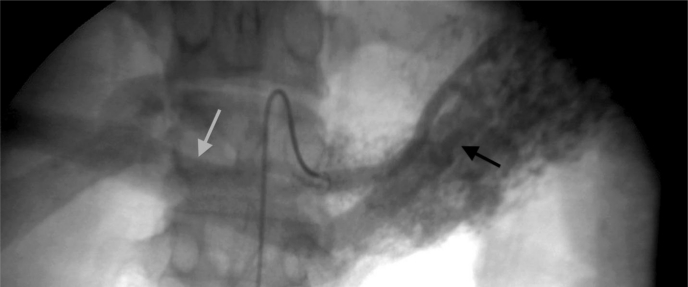
Figure 6.
Mesenteric angiogram. 52 year old male with pancreatic arteriovenous malformation. Frontal projection selective splenic artery injection early arterial phase shows multiple feeding arteries to the pancreatic lesion (black arrow) with immediate opacification of the portal vein (gray arrow). (Iohexol 300 mgi/ml)
Table 1:
Differential diagnoses for pancreatic arteriovenous malformation
| CT | MRI | Angiography | US | |
|---|---|---|---|---|
| Pancreatic arteriovenous malformation | Multiple discrete intrapancreatic vessels, best demonstrated on early arterial scanning; multiple feeding vessels associated with early portal vein opacification | Cluster of tubular structures demonstrating signal void on T2-weighted imaging | Lesion with racemose vascular network; multiple feeding arteries to the pancreatic lesion with immediate opacification of the portal vein | Nonspecific hypoechoic nodules; mosaic pancreatic color flow pattern; pulsatile portal vein waveforms on Doppler |
| Hypervascular pancreatic tumor (islet cell tumor) | Solitary hyperattenuating lesion in arterial and venous phase imaging; large lesions show ring-like enhancement | Discrete solitary lesion demonstrating high signal on T2; low signal on T1; variable enhancement, sometimes ring-like | Small to large densely opacified, well defined lesion | Solitary, well marginated, oval/round, homogeneous hypoechoic lesion |
| Hypervascular metastases | Solitary or multiple discrete masses with peripheral or homogeneous enhancement | Solitary or multiple discrete masses with variable signal intensity; peripheral or homogeneous enhancement | Solitary or multiple discrete hypervascular masses | Solitary or multiple well defined lesions |
| Intrapancreatic accessory spleen | Round mass with attenuation similar to spleen on all imaging sequences | Round mass with signal characteristics similar to spleen on all imaging sequences | Solitary lesion; may mimic islet cell tumor | Round or oval mass with similar echogenicity to spleen; posterior acoustic enhancement; vascular hilum |
| Chronic pancreatitis (rare appearance) | Hypervascularity and early arteriovenous shunting with portal vein filling; additional findings of chronic pancreatitis | Pancreas diffusely low in signal on T1 fat-suppressed sequences; decreased and delayed enhancement | Hypervascular mass with early visualization of the portal vein | Heterogeneous increased echogenicity; pancreatic enlargement; focal increased echogenicity; pseudocysts |
Table 2:
Summary table for pancreatic arteriovenous malformation
| Etiology | Idiopathic, associated with hereditary hemorrhagic telangiectasia (HHT) |
| Incidence | Rare. Approximately 50% congenital, 5% acquired, 45% unknown |
| Gender ratio | Strong male predilection- approximately 88% |
| Age Predilection | 7 mos-73 yrs. Predominantly 50–60 years old |
| Risk factors | HHT, trauma, surgery, inflammation, tumor |
| Treatment | Arterial embolization, transjugular intrahepatic portosystemic shunt (TIPS), vascular ligation and pancreatic resection |
| Prognosis | Good in absence of portal venous hypertension |
| Findings on imaging | CT- multiple discrete intrapancreatic vessels, best demonstrated on early arterial scanning. Multiple feeding vessels associated with early portal vein opacification. US- nonspecific hypoechoic nodules, mosaic pancreatic color flow pattern and pulsatile portal vein waveforms on Doppler. Mesenteric Angiogram- Hypervascular mass with arteriovenous shunting |
ABBREVIATIONS
- CT =
Computed tomography
- HHT =
Hereditary hemorrhagic telangiectasia
- MIP =
maximum intensity projection
- MR =
Magnetic resonance
- PAVM =
Pancreatic arteriovenous malformation
- TIPS =
Transjugular intrahepatic portosystemic shunting
- US =
Ultrasound
Footnotes
Online access
This publication is online available at: www.radiologycases.com/index.php/radiologycases/article/view/742
REFERENCES
- 1.Takemoto I, Tsuda M, Yano Y, et al. Pancreatic arteriovenous malformation combined with portal thrombosis. Intern Med. 2007;46:233–236. doi: 10.2169/internalmedicine.46.1852. [DOI] [PubMed] [Google Scholar]
- 2.Siddiki H, Doherty MG, Fletcher JG, et al. Abdominal findings in hereditary hemorrhagic telangiectasia: Pictorial essay on 2D and 3D findings with isotropic multiphase CT. Radiographics. 2008;28:171–184. doi: 10.1148/rg.281075037. [DOI] [PubMed] [Google Scholar]
- 3.Barth MM, Khwaja K, Faintuch S, Rabkin D. Transarterial and transvenous embolotherapy of arteriovenous fistulas in the transplanted pancreas. J Vasc Interv Radiol. 2008;19:1231–1235. doi: 10.1016/j.jvir.2008.04.028. [DOI] [PubMed] [Google Scholar]
- 4.Kanno A, Satoh K, Kimura K, et al. Acute pancreatitis due to pancreatic arteriovenous malformation: 2 case reports and review of the literature. Pancreas. 2006;32:422–425. doi: 10.1097/01.mpa.0000220869.72411.39. [DOI] [PubMed] [Google Scholar]
- 5.Hosogi H, Ikai I, Hatano E, Taura K, Fujii H, Yamamoto Y, Shimahara Y. Pancreatic arteriovenous malformation with portal hypertension. J Hepatobiliary Pancreat Surg. 2006;13:344–346. doi: 10.1007/s00534-005-1068-y. [DOI] [PubMed] [Google Scholar]
- 6.Ohtani N, Kimoto K, Yoshida S, Tanaka T, Inokuchi H, Kawai K. Pancreatic arteriovenous malformation with pancreatitis involving a pancreatico-venous fistula. Gastroenterol Jpn. 1992;27:115–120. doi: 10.1007/BF02775073. [DOI] [PubMed] [Google Scholar]
- 7.Aida K, Nakamura H, Kihara Y, Abe S, Okamoto K, Otsuki M. Duodenal ulcer and pancreatitis associated with pancreatic arteriovenous malformation. Eur J Gastroenterol Hepatol. 2002;14:551–554. doi: 10.1097/00042737-200205000-00013. [DOI] [PubMed] [Google Scholar]
- 8.Malan E. Congenital angiodysplasias of the extremities. J Cardio-vasc Surg. 1964;5:87. [PubMed] [Google Scholar]