Abstract
Ameloblastoma is a slow growing odontogenic epithelial tumor of jaw. It accounts for 1% of all tumors and cysts arising in maxilla and mandible. Although it is locally invasive and has a marked tendency to recur, metastasis is rare. Of the various histological patterns of ameloblastoma, the granular cell type is extremely rare accounting for 4% of ameloblastomas. We report a case of granular cell ameloblastoma with metastasis to the cervical lymph node presenting in a 40-year-old Indian female.
Keywords: Ameloblastoma, granular cell change, lymph node, metastasis
INTRODUCTION
Ameloblastoma is seen to have a benign appearance on histology, irrespective of its variable clinical behavior. Microscopically various patterns have been described (follicular, plexiform, acanthomatous, papilliferous-keratotic, granular cell type, desmoplastic, vascular, and dentinoameloblastoma).[1–3] Majority of patients present in the fourth decade.[4] Men are affected slightly more often than female, with a particularly elevated incidence in eastern Africa. More than 80% of ameloblastomas arise in the mandible (mostly angle or ramus).[5] Clinically, ameloblastomas are separated into solid or multicystic, unicystic, and peripheral. Unicystic ameloblastomas are believed to be less aggressive.[6] Peripheral ameloblastomas are rare.[7] They are either primary or secondary soft tissue tumors, the latter appearing after operations. Radiologically, ameloblastomas present as unilocular or multilocular translucencies.
Malignancy in the ameloblastoma has been divided into two distant lesions. A malignant (metastasizing) ameloblastoma is diagnosed when a seemingly histologically benign ameloblastoma produces a metastasis resembling the original lesion. Both lesions are microscopically well differentiated. Ameloblastic carcinoma is an odontogenic tumor having the overall microscopic architectural features of ameloblastoma but in addition having malignant cytological features such as marked nuclear atypia and numerous mitotic figures.[8,9]
In the year 1965, Tsukada et al. reported a case of granular cell ameloblastoma with metastasis to the lung.[10] Two years later, a case of granular cell ameloblastoma with metastasis to cervical vertebrae was reported.[11] We reviewed the literature for any cases of granular cell ameloblastoma with metastasis, which might have been reported from year 1967 until now. To the best of our knowledge this is probably the third case of a metastasizing granular cell ameloblastoma.
CASE REPORT
A 40-year-old female first reported to the surgery department of Safdarjung hospital, New Delhi, India. She presented with a disfiguring swelling on the right side of neck of approximately two years duration [Figure 1]. Swelling was associated with pain and difficulty in chewing. Cervical lymph nodes were palpable and nontender. Roentgenogram of the mandible showed swollen translucent cystic structures reaching from corpus to ramus of the right mandible. A biopsy was taken and sent for histopathological examination. Diagnosis of ameloblastoma of the granular cell type was made. The patient was admitted for surgery. Right extended radical neck dissection with right hemi mandibulectomy was performed. Excision of zygomatic arch and surrounding soft tissue, masseter muscle, and temporalis muscle along with right parotid, was done. Reconstruction was performed using right pectoralis major myofacial flap for buccal mucosal reconstruction and delto pectoral flap with split skin graft for skin defect. The surgical specimens were sent to our Institute for histopathological examination. Two years following surgery, patient's follow up with x-rays, have not revealed any new lesions.
Figure 1.

Patient with a large abnormal swelling on the right side of face
Pathological findings
Gross examination of the excised specimen showed a well circumscribed large pink tan growth measuring 7.5 × 5 × 4 cm in the region of the mandible. Masseter and temporalis muscles along with the parotid gland were identified and sections taken. Thirteen lymph nodes were isolated from the specimen of radical neck dissection.
Microscopic examination of the sections showed an encapsulated tumor of odontogenic origin. Tumor cells formed nests supported by fibrous connective tissue stroma [Figure 2]. At the periphery of the nests, there were columnar cells organized in a pallisaded fashion [Figure 3]. The inner cell mass showed round to polygonal cells with abundant granular cytoplasm and small pyknotic nuclei [Figure 4]. Parotid gland and muscle fibers were free from tumor cell infiltration. One lymph node showed tumor metastasis characterized by the presence of granular cells [Figure 5].
Figure 2.
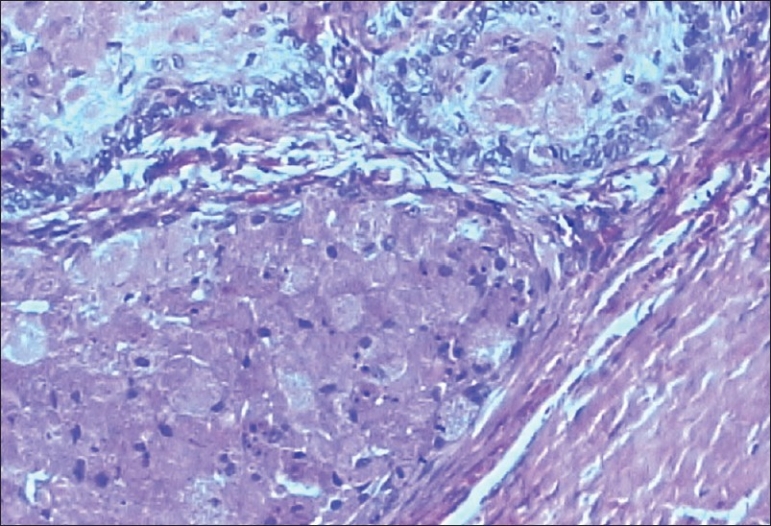
Tumor nests in a fibrous stroma. (H and E, ×100)
Figure 3.
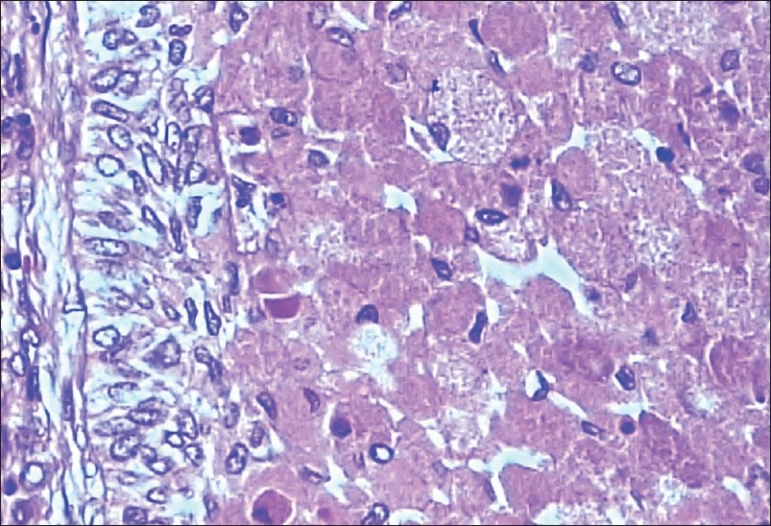
Periphery of tumor nests having pallisaded cells. (H and E, ×200)
Figure 4.
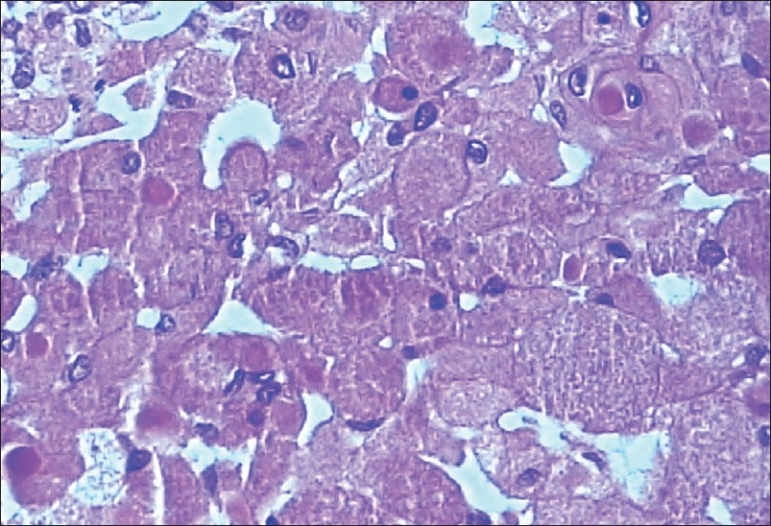
Cells displaying cytoplasmic granularity with pyknotic nuclei, some of which are eccentric. (H and E, ×400)
Figure 5.
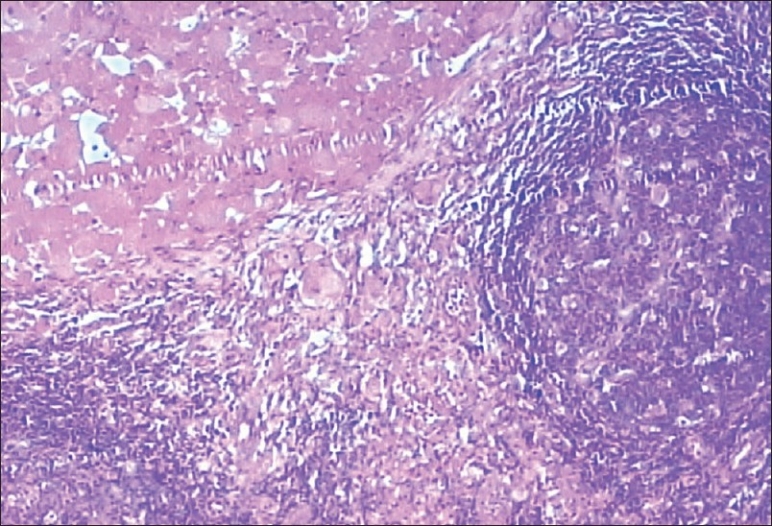
Metastasis in lymph node showing tumor cells with granular cytoplasm. (H and E, ×200)
DISCUSSION
Ameloblastoma is a locally invasive neoplasm derived from odontogenic epithelium. The tumor is made up of proliferating odontogenic epithelium especially of enamel organ-type tissue that has not undergone differentiation to the point of hard tissue formation. Characteristically, the tumor lacks enamel and dentin. It has been postulated that the epithelium of origin is derived from one of the following sources: (1) epithelial lining of odontogenic cyst, (2) dental lamina or enamel organ, (3) disturbances of developing enamel organ, (4) basal cells of surface epithelium, or (5) heterotopic epithelium of other parts of the body.[5,12]
Metastasis in ameloblastoma is extremely rare. Only 43 cases had been documented until 1987.[11] Mean interval between onset of tumor and metastasis was 16.4 years. Treatment for primary tumor prior to metastasis included surgery alone or with radiotherapy.[10] Two cases showed a granular cell change.[10,11] Our patient presented with a metastasis of granular cell ameloblastoma at the first instance, giving a brief history of 2 years. Metastasis was to the regional lymph node. Most common sites of metastasis are lung (76.7%), followed by regional lymphnodes (37.8%), pleura (16.2%), vertebrae (13.5%), skull (10.8%), diaphragm (8.1%), liver and parotid (5.4%) and even more rarely, the spleen and kidney.[13] Hematogenous[14,10] and lymphatic spread are thought to be the possible routes for metastasis. The best treatment is an initial extensive surgical excision. Ninety percent of cases treated conservatively, recur at some time.
Granular cell change in ameloblastoma is a rare histopathological entity. It was first seen by Krompecher[15] in 1918 and was called pseudoxanthomatous cells. Granular cells can appear in various odontogenic and nonodontogenic tumors. Granular cells of granular cell ameloblastoma are clearly of epithelial origin staining exclusively for cytokeratin. Granular cell tumors stain positive for vimentin and S-100. Only vimentin is positive in granular cells of granular ameloblastic fibroma. The term “granular cell ameloblastic fibroma” is a misnomer, as a number of these cases are probably central odontogenic fibromas exhibiting granular cell change. Ultrastructurally it has been revealed that it is the lysosomal overload in these cells that imparts the characteristic granularity.
Whether granular cell change in ameloblastoma is a degenerative process or a harbinger of a more aggressive course is a matter of debate. All three cases of granular cell ameloblastoma (our case included) have eventually produced metastasis. Add to this, our patient gave a short history of duration before tumor metastasis.
CONCLUSION
Granular cell ameloblastoma is an extremely rare entity. Although the exact implication of a granular cell change in ameloblastoma cannot be ascertained due to paucity of cases documented, yet reported cases must be followed closely in anticipation of metastasis.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
REFERENCES
- 1.Burkes EJ, Wallace DA. Granular cell ameloblastoma: Report of case. J Oral Surg. 1976;34:742–4. [PubMed] [Google Scholar]
- 2.Collini P, Zuchini N, Vessecchia G, Guzzo M. Papilliferous keratoameloblastoma of mandible: A papillary ameloblastic carcinoma: Report of a case with a 6-year follow-up and review of the literature. Int J SurgPathol. 2002;10:149–55. doi: 10.1177/106689690201000210. [DOI] [PubMed] [Google Scholar]
- 3.Nasu M, Takagi M, Yamamoto H. Ultrastructural and histochemical studies of granular cell ameloblastoma. J Oral Pathol. 1984;13:448–56. doi: 10.1111/j.1600-0714.1984.tb01445.x. [DOI] [PubMed] [Google Scholar]
- 4.Ladeinde AL, Ajayi OF, Ogunlewe MO, Adeyemo WL, Arotiba GT, Bamgbose BO, et al. Odontogenic tumors: A review of 319 cases in a Nigerian teaching hospital. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2005;99:191–5. doi: 10.1016/j.tripleo.2004.08.031. [DOI] [PubMed] [Google Scholar]
- 5.Ueno S, Namakura S, Mushimoto K, Shirasu R. A clinicopathologic study of ameloblastoma. J Oral Maxillofac Surg. 1986;44:361–5. doi: 10.1016/s0278-2391(86)80031-3. [DOI] [PubMed] [Google Scholar]
- 6.Olaitan AA, Adekeye EO. Unicystic ameloblastoma of the mandible: A long term follow up. J Oral Maxillofac Surg. 1997;55:345–8. doi: 10.1016/s0278-2391(97)90122-1. discussion 349-50. [DOI] [PubMed] [Google Scholar]
- 7.Gurol M, Burkes EJ., Jr Peripheral ameloblastoma. J Periodontol. 1995;66:1065–8. doi: 10.1902/jop.1995.66.12.1065. [DOI] [PubMed] [Google Scholar]
- 8.Eversole LR. Malignant epithelial odontogenic tumors. Semin Diagn Pathol. 1999;16:317–24. [PubMed] [Google Scholar]
- 9.McClatchey KD. Tumors of the dental lamina. A selective review. Semin Diagn Pathol. 1987;4:200–4. [PubMed] [Google Scholar]
- 10.Tsukada Y, Delapava S, Pickren JW. Granular cell ameloblastoma with metastasis to the lungs- report of a case and review of the literature. Cancer. 1965;18:916–25. doi: 10.1002/1097-0142(196507)18:7<916::aid-cncr2820180722>3.0.co;2-t. [DOI] [PubMed] [Google Scholar]
- 11.Hoke HF, Jr, Harrelson AB. Granular cell ameloblastoma with metastasis to the cervical vertebrae- observations on the origin of the granular cells. Cancer. 1967;20:991–9. doi: 10.1002/1097-0142(196706)20:6<991::aid-cncr2820200609>3.0.co;2-v. [DOI] [PubMed] [Google Scholar]
- 12.Shafer WG, Hine MK, Levy BM, Tomich CE. Ectodermal Tumours of odontogenic origin. Philadelphia: J. B. Saunders; 1983. pp. 276–92. [Google Scholar]
- 13.Inoue N, Shimojyo M, Iwai H, Ohtsuki H, Yasumizu R, Shintaku M, et al. Malignant ameloblastoma with pulmonary metastasis and hypercalcemia. Report of an autopsy case and review of the literature. Am J Clin Pathol. 1988;90:474–81. doi: 10.1093/ajcp/90.4.474. [DOI] [PubMed] [Google Scholar]
- 14.Byrne MP, Kosmala RL, Cunningham MP. Ameloblastoma with regional and distant metastases. Am J Surg. 1974;128:91–4. doi: 10.1016/0002-9610(74)90242-6. [DOI] [PubMed] [Google Scholar]
- 15.Krompecher E. The histogenesis and morphology of adamantinomas and other jaw tumors. Beitr Pathol Anat. 1918;64:165–97. [Google Scholar]


