Abstract
Fusion is the union of two tooth buds that are normally separated. Fusion is more frequent in deciduous teeth, particularly in the anterior region. The etiology of fusion is not known. It has been suggested that the pressure of adjacent dental follicles produces their contact and fusion before calcification. There is no difference between men and women in incidence. The term paradental cyst means that such type of cysts that are close proximity with the root of a tooth. A history of recurrent pericoronitis is reported usually and there is often the presence of a communication between the periodontal pocket and the cyst. We present a rare case report where in partially erupted mandibular third molar is fused horizontally with a supernumerary tooth with paradental cyst.
Keywords: Cyst, fusion, impaction
INTRODUCTION
Fusion is the joining of two tooth buds during development. It leads to a reduced number of teeth in the dental arch when it does not involve supernumerary tooth. Fusion is infrequently seen in permanent teeth. Fusion of the mandibular third molar and supernumerary tooth with paradental cyst occurring together is extremely rare.[1–3] In this article, we report a case of fusion of the mandibular third molar with a supernumerary tooth along with paradental cyst.
The term paradental cyst means cysts that have relationships or proximity with the root of a tooth.[4] Shear defined paradental cyst as an inflammatory cyst arising on the lateral aspect of a vital tooth as a result of an inflammatory process in the periodontal pocket. The etiology of these cysts is still debated, but is believed that they originate from the reduced enamel epithelium or from the inflammatory proliferation of epithelial rests of malassez, which come from the superficial mucosa of a tooth in eruption (pericoronitis). The major clinical features of the paradental cyst are the presence of a recurring inflammatory periodontal process, usually a pericoronitis.[4,5]
CASE REPORT
A 28-year-old female patient was referred to the outpatient department with pain in the left lower region since 1 year. Clinical examination of the oral cavity revealed a partially impacted left third mandibular molar, with pericoronitis distal to it associated with pain. OPG revealed mesio-angular partially impacted third molar with radiopaque mass attached to the crown of the molar distally. A well-defined radiolucency was also noticed in association with impacted tooth. The supernumerary tooth was fused with the partially impacted mandibular left third molar horizontally with distinct crown, which was pushing the roots of the third molar, but separated with a radiolucent line in few areas [Figure 1].
Figure 1.

OPG showing mandibular third molar fused with supernumerary tooth
Radiographically, the anomaly appeared as unilocular radiolucency at the apical portion of the supernumerary tooth. The pulp chamber of both teeth appeared separate. Differential diagnoses for the radiopacity considered were supernumerary tooth and odontoma, and for the radiolucency the paradental cyst was considered. The partially impacted tooth along with the supernumerary tooth was removed surgically under LA and the healing was uneventful. Examination of the gross specimen showed that the supernumerary tooth was horizontally fused with the third molar [Figure 2a] and when viewed apically the enamel of the supernumerary tooth was clearly seen [Figure 2b]. Intra oral periapical radiograph was taken of the gross specimen [Figure 3]. The gross specimen was cut into equal halves and seen under stereo microscope. The dentin was continuous of both the impacted third molar and the horizontal supernumerary tooth in one area and confirmed the diagnosis of fusion [Figure 4]. When the soft tissue surrounding the supernumerary tooth seen histologically, the epithelial lining was made up of 2–4 layers resembling reduced enamel epithelium [Figure 5]. Few areas there were hyperplastic nonkeratinized squamous epithelium. A heavy inflammatory infiltrate of mononuclear and polymorphonuclear cells was observed in the epithelium and connective tissue wall [Figure 6]. The fibrous wall showed multinucleated giant cells associated with the thickness of the blood vessel walls. The histopathology associated with macroscopic and radiographic examinations permitted the definitive diagnosis of a paradental cyst of the partially impacted mandibular left third molar fused to supernumerary tooth.
Figure 2.
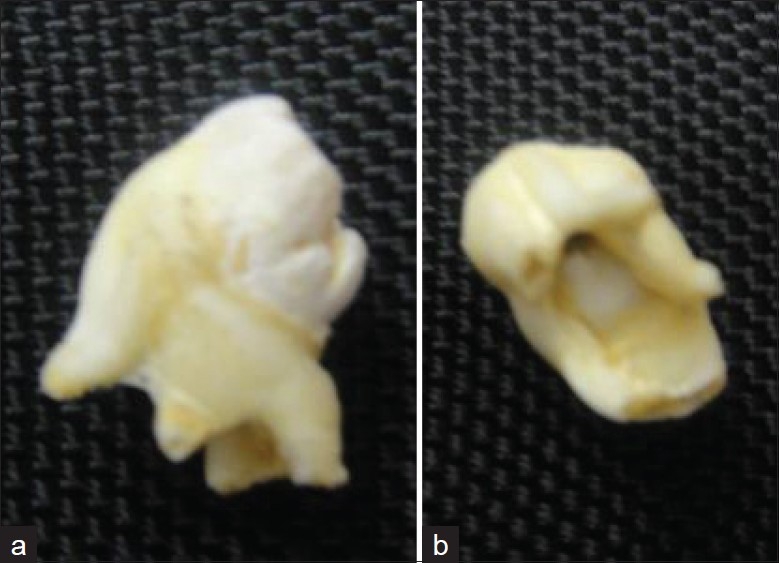
(a and b) Gross specimen showing fusion of the third molar and supernumerary tooth and enamel displayed from the apical aspect
Figure 3.
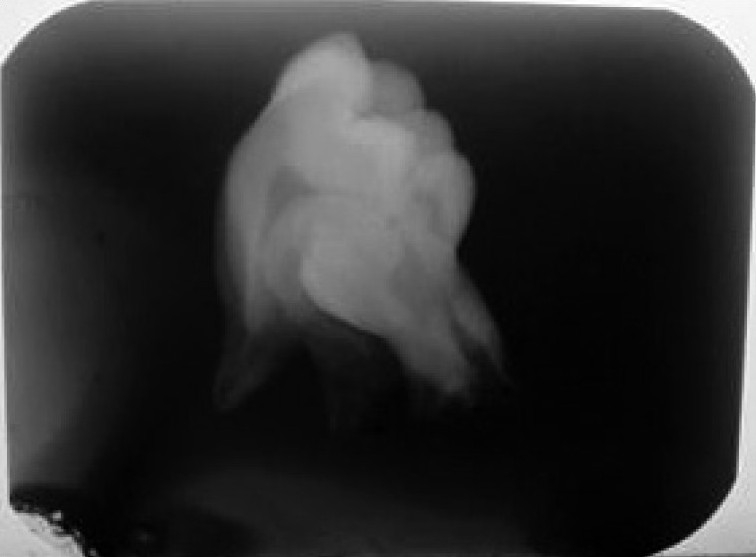
Intra oral periapical radiograph of the gross specimen showing third molar fused with supernumerary tooth
Figure 4.

Stereo microscopic view showing continuous dentin between third molar and supernumerary tooth
Figure 5.
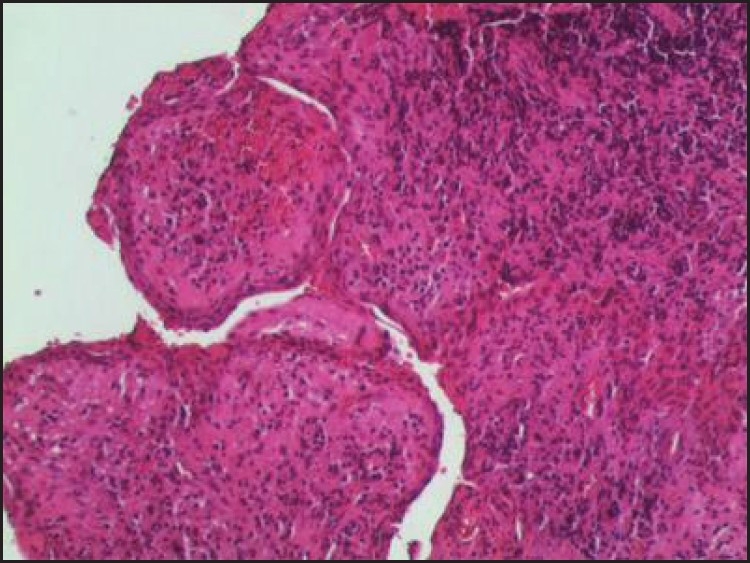
2–4 layered epithelium seen resembling reduced enamel epithelium (H and E, 10×)
Figure 6.
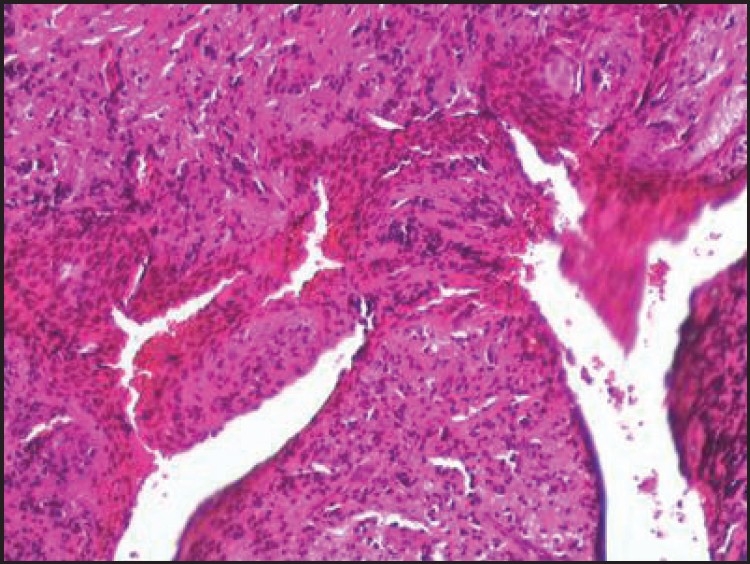
Epithelium showing hyperplasia with underlying connective tissue with inflammatory cells (H and E, 10×)
DISCUSSION
Fusion of the mandibular permanent teeth is a relatively uncommon dental anomaly. Fusion is more frequent in deciduous teeth, particularly in the anterior region; rarely have cases been reported with the permanent second and third molars.[2] The occurrence of paradental cyst along with the supernumerary tooth is extremely rare, as in our case, and we could not locate any similar case reported earlier in literature. The exact etiology of fusion is still not known.[2]
In this article, we present a case with similar radiological appearance with well-defined radiolucency associated with the roots of the partially impacted third molar fused with supernumerary tooth. The differential diagnosis included radicular cyst, lateral periodontal cyst, dental follicle, and dentigerous cyst.[4]
Histologic features of paradental cyst are similar to any other inflammatory odontogenic cysts. The walls of the connective tissue show chronic inflammatory cells and are lined by a nonkeratinized stratified squamous epithelium of varying thickness.[4] Our case was similar to the literature histologically. A clinicopathologic correlation, incorporating the surgical, radiographic, and histological findings is required to obtain the final diagnosis of paradental cysts.
Presence of impacted or partially impacted tooth in mandibular posterior region is common, and progressing into dentigerous cyst or paradental cyst is also usual finding. Presence of fused supernumerary tooth to third molar, which is associated with paradental cyst, may be a coincidence. However, in our case it appears like the presence of supernumerary tooth fused to the molar prevented its eruption and lead into cyst formation, as there was good space available for eruption of third molar as the opposing side third molar was erupted.
CONCLUSION
Fusion in posterior permanent dentition is a rare condition. If fusion occurs between a normal and a supernumerary tooth radiographs play an invaluable role in final diagnosis and the number of teeth, in such situations, might be normal. Paradental cyst with fusion occurring in permanent third molar with supernumerary tooth is extremely rare condition and perhaps might be the first case in literature.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
REFERENCES
- 1.Chen HS, Huang YL. Fusion of third and fourth mandibular molars? Oral Surg Oral Med Oral Pathol. 1992;73:767. doi: 10.1016/0030-4220(92)90027-n. [DOI] [PubMed] [Google Scholar]
- 2.Chen RJ, Yang JF, Lin CC, Chen CH, Lin LM. An unusual triad of dental anomalies-fusion, supernumerary and dens invaginatus of the mandibular third molar. Gaoxiong Yi Xue Ke Xue Za Zhi. 1986;2:353–9. [PubMed] [Google Scholar]
- 3.López-Carriches C, Leco-Berrocal I, Baca-Pérez-Bryan R. Fusion of mandibular third molar with supernumerary fourth molar. Rev Esp Cirug Oral Y Maxillofac. 2008;30:344–7. [Google Scholar]
- 4.de Sousa SO, Corrêa L, Deboni MC, de Araújo VC. Clinicopathologic features of 54 cases of paradental cyst. Quintessence Int. 2001;32:737–41. [PubMed] [Google Scholar]
- 5.Philepsen HP, Reichart PA, Ogawa I, Suei Y, Takata T. The inflammatory paradental cyst: A critical review of 342 cases from a literature survey, including 17 new cases from the author's files. J Oral Pathol Med. 2004;33:147–55. doi: 10.1111/j.0904-2512.2004.00139.x. [DOI] [PubMed] [Google Scholar]


