Abstract
Background:
Reports of series of central jaw tumours in children are rare hence predicting their biological behaviour as well as treatment, prognosis have not been documented from this part of the world.
Aim:
To study retrospectively, the paediatric central jaw tumours, reported to our institute with relation to site of occurrence, presentation and biological behaviour.
Materials and Methods:
All consecutive patients (<18 years), between 2004-2010, histologically diagnosed as having an intraosseous tumour or tumour-like lesions formed the study population. Patients fulfilling the inclusion criteria were only considered for further study. The entire study material was analyzed and grouped into various categories for logical conclusions. The data accumulated were grouped, entered and analyzed.
Results:
Sixty-one cases fulfilled the criteria. Gender distribution was equal, with mandible predominance (2.2:1) and a predominance of non-odontogenic lesions (2:1). There were 4 malignant and 57 benign conditions. Anterior jaw lesions were 23 while 38 were present in the posterior region of jaws (1:1:6).
Conclusions:
The pattern of central jaw tumours presentation in children from this part of India has been documented. In this study, paediatric jaw tumours are less common compared to those in adults with non-odontogenic tumours being common. The finding of the present study indicates that an impacted tooth, beyond the eruption time deserves more attention for the reason of associated pathologies in children.
Keywords: Central jaw tumors, children, odontogenic and nonodontogenic lesions, odontogenic
INTRODUCTION
Central jaw tumors (intraosseous) in children occur infrequently and few oral pathologists have had the opportunity or experience in diagnosing these lesions and predicting their biological behavior. Some children are not diagnosed correctly at the initial stages as having a neoplasm and are wrongly treated for infections by antibiotic administration. Subsequent to an unresponsive antibiotic therapy radiographs are taken to reveal a radiolucent or radiodense lesion in the jaws. Finally a tissue diagnosis becomes necessary in order to diagnose and initiate proper therapy. Unfortunately the number of organized courses available to the clinician, radiologist, and pathologist discussing the various aspects of tumor and tumor-like lesions of the jaws in the pediatric age group is relatively small. These limitations prompted us to undertake a study on pediatric jaw tumors as reported in our Institute. The collected data were broadly classified into odontogenic and nonodontogenic groups and the commonly occurring tumors in children were identified. A comparison with adult jaw tumors in their incidence, prevalence, site of occurrence with a plausible explanation for their etiology, and pathogenesis has been attempted.
MATERIALS AND METHODS
All patients below the age of 18 years who were histologically diagnosed as having an intraosseous tumor or tumor-like lesions were included in the study group. The material was collected from the year 2004 to 2010. The criteria for inclusion were:
All lesions with radiological changes in bone were included.
Soft tissue tumors showing bone erosion were excluded.
Aggressive cysts like OKC, CEOC, and aneurysmal bone cyst were included.
The entire study material was analyzed and grouped into various categories for logical conclusions.
RESULTS
The study sample comprised a total of 61 pediatric tumors as reported in the Department of Oral Pathology and Microbiology at Subharti Dental College, Meerut, India, over a period of 6 years (2004–2010).
Sex distribution was males – 30 and females – 31 which was almost equal. The site of occurrence was found to be more in the mandible compared to maxilla (mandible: maxilla 42:19, i.e., 2.2:1). There were 40 nonodontogenic tumors compared [Table 1] to 21 odontogenic tumors (2:1). There were altogether 57 benign conditions [Table 2] while malignant were only 4 (16:1). Anterior jaw lesions were 23 cases while 38 were present in the posterior region of jaws (1:1:6).
Table 1.
Distribution of cases: Pediatric tumors
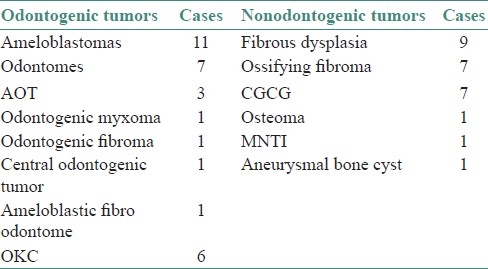
Table 2.
Distribution of cases: Pediatric tumors
Observations
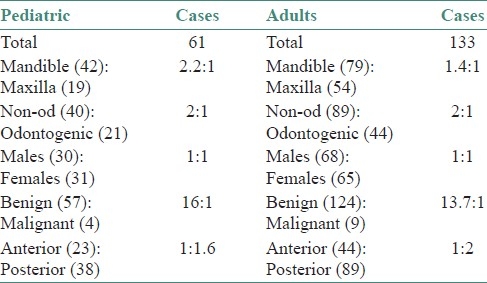
It was observed that the reported number of cases of pediatric jaw tumors over a period of 6 years was much less compared to the total number of adult jaw tumors (61:133) [Table 3]. Intraosseous tumors have shown preponderance toward occurring more in mandible compared to maxilla. This was seen in both pediatric and adult tumors. It was observed that the incidence of nonodontogenic tumors was almost twice that of odontogenic tumors in both children and adults. Cases of malignant jaw tumors were much less compared to benign tumors. This was seen to be 16:1 in children below 18 years and 13.7:1 in adults above 18 years of age. Tumors affecting the posterior region of the jaws were more common than those affecting the anterior region as seen in both pediatric and adult cases.
Table 3.
Comparison between pediatric and adult tumors
DISCUSSION
Primary jaw tumors are broadly classified into odontogenic and nonodontogenic groups. Odontogenic tumors are considered to be common in children,[1] of which ameloblastomas are found extremely rarely. However in the present survey there were reportedly more ameloblastomas in the sample of odontogenic tumors. Out of 9 cases 5 were follicular, 3 plexiform, and 1 acanthomatous [Graph 1].
Graph 1.
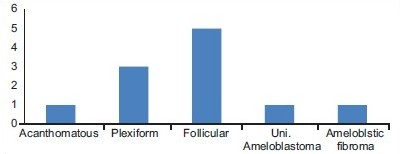
Distribution of cases in ameloblastomas
One case of unicystic ameloblastoma (mural proliferation) was seen among the pediatric group. According to Ord et al.,[2] it is impossible to estimate the true incidence of childhood ameloblastoma because different authors have defined the pediatric population upper age limit at differing time periods as less than 20 years, 18 years, 16 years, and 15 years.[3] In the present study the male-female ratio for ameloblastomas was almost equal with five cases in males and six in females. This was in contrast to that of 21 males and 9 females in adults, the ratio being about 2:1 with a male predilection.
The two ameloblastic lesions that are commonly found in childhood are the ameloblastic fibroma and the unicystic ameloblastoma.[4] In the present study the comparative frequency of occurrence of ameloblastomas may be because the upper age limit taken is 18 years unlike studies where pediatric group is restricted to 12 years of age.[3] Seven cases of odontomes were reported which was the next most commonly occurring odontogenic tumor or hamartomatous malformation seen in children.
Seven (7) cases of central giant cell lesions were reported in the Department of Oral Pathology in children out of a total of 61 cases, while in adults there were 12 CGCG out of a total of 133 tumors. So the relative percentage of occurrence of CGCG in children is quite high compared to the adults. The reactive nature of these lesions may be emphasized upon which is more exuberant in children, thus leading to tumorous proliferations.
Jaffe was the first to raise the possibility that these lesions were non-neoplastic but rather reactive in nature.[5] One pediatric CGCG was diagnosed as the Brown tumor of hyperparathyroidism which regressed after institution of therapy in the present study.
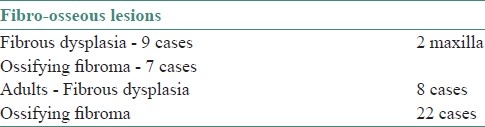
Though maxilla is said to be involved more often than mandible we had only two cases of fibrous dysplasia affecting maxilla while seven cases were reported in the mandible [Table 4]. Compared to adult cases it was much more frequent in pediatric patients which was observed in our study. No case of Cherubism was reported in the present survey. Ossifying fibromas were more commonly seen in adult patients which may be explained by the fact that the lesion forms mature lamellated bone and remains asymptomatic until an obvious swelling is manifested, so the time of diagnosis reaches adulthood.
Table 4.
Distribution of cases: Fibroosseous lesions
Aggressive cysts
Although cystic lesions are benign lesions, in children they may present clinical problems, namely a rapid increase in size, occasional recurrence (odontogenic keratocysts, or severe hemorrhage (aneurysmal bone cysts).[3]
Six cases of odontogenic keratocysts have been reported out of 61 cases of pediatric tumors while among 133 adult tumors 26 OKCs were seen. The relative percentage of occurrence in adults is 20% compared to 10% cases in children. Moreover it was noted that all the pediatric OKCs were reportedly around 17 or 18 years of age, or age approaching adulthood. No case was diagnosed in the first decade of life. This too may be because of the intramedullary growth of the cyst without obvious facial asymmetry and at times being diagnosed on routine radiographs in asymptomatic cases. Aneurysmal bone cyst which is considered under certain classifications as aggressive jaw cyst was reported in a single case of 15-year-old female patient in the parasymphysis area extending to the body of the mandible. One other case of aneurysmal bone cyst was reported in a 45-year-old female patient. From this small sample size the only conclusion drawn was that may be aneurysmal bone cyst is seen more commonly in females which is in accordance with some of the reported studies with larger sample sizes.[6,7] A history of trauma in both pediatric and adult cases was elicited.
Salivary gland lesions
Only one case of intraosseous salivary gland tumor was found to be reported in pediatric patient which was a case of Mucoepidermoid carcinoma of the minor salivary gland in posterior palate. The patient was an 18-year-old female while in adults intraosseous salivary gland tumors were seen in 13 cases. All were diagnosed as pleomorphic adenomas in palate or intraosseous mucoepidermoid carcinomas of the mandible. So the occurrence of an intraosseous salivary gland tumor in the pediatric age group is an unusual occurrence.[7] The possible pathogenesis of mucoepidermoid carcinoma as a complication of pre-existing dentigerous cyst can be considered in the given case though this could not be confirmed [Table 5].
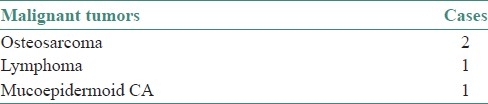
Table 5.
Distribution of malignant cases
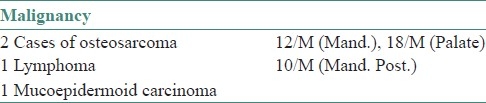
The malignant tumors reported in this study were two cases of osteogenic sarcoma, one lymphoma (round cell tumor) and one mucoepidermoid carcinoma of salivary glandular origin. One case of osteosarcoma was seen in mandible while the other was a more rare site of occurrence, namely the posterior region of the hard palate. In a study by Dehner et al.[8] of malignant jaw tumors in children osteosarcoma was found to be most frequently reported malignant tumor in their limited pediatric series. Though osteosarcomas are more commonly seen in long bones, the occurrence in jaw bones within the age group of 10-25 years is relatively common which is in accordance with the present findings. A dramatic increase of incidence in adolescence corresponds with the growth spurt. No history of trauma or any underlying bone disease could be elicited in these cases.
Others
One case of melanotic neuroectodermal tumor of infancy was reported in a female child of 4 months. No recurrence was reported after the tumor was surgically excised.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
REFERENCES
- 1.Kaban LB, Troulis MJ. Text book of Pediatric Oral and Maxillofacial surgery. 2nd ed. Philadelphia: Elsevier Saunders; 2004. pp. 212–45. [Google Scholar]
- 2.Ord RA, Blanchaert RH, Jr, Nikitakis NG, Sauk JJ. Ameloblastoma in children. J Oral Maxillofac Surg. 2002;60:762–70. doi: 10.1053/joms.2002.33242. discussion, 770-1. [DOI] [PubMed] [Google Scholar]
- 3.Ajayi OF, Ladeinde AL, Adeyemo WL, Ogunlewe MO. Odontogenic tumors in Nigerian children and adolescents- A retrospective study of 92 cases. World J Surg Oncol. 2004;2:39. doi: 10.1186/1477-7819-2-39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Robinson L, Martinez MG. Unicystic ameloblastoma: A prognostically distinct entity. Cancer. 1977;40:2278–85. doi: 10.1002/1097-0142(197711)40:5<2278::aid-cncr2820400539>3.0.co;2-l. [DOI] [PubMed] [Google Scholar]
- 5.Dehner LP. Tumors of the mandible and maxilla in children. I. Clinicopathologic study ofhistologically benign lesions. Cancer. 1973;31:364–84. doi: 10.1002/1097-0142(197302)31:2<364::aid-cncr2820310216>3.0.co;2-z. [DOI] [PubMed] [Google Scholar]
- 6.Kumar Dutta H. Jaw and gum tumours in children. Pediatr Surg Int. 2009;25:781–4. doi: 10.1007/s00383-009-2427-6. [DOI] [PubMed] [Google Scholar]
- 7.Iatrou I, Theologie-Lygidakis N, Leventis M. Intraosseous cystic lesions of the jaws in children: A retrospective analysis of 47 consecutive cases. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2009;107:485–92. doi: 10.1016/j.tripleo.2008.10.004. [DOI] [PubMed] [Google Scholar]
- 8.Dehner LP. Tumors of the mandible and maxilla in children. II. A study ofprimary and secondary malignant tumors. Cancer. 1973;32:112–20. doi: 10.1002/1097-0142(197307)32:1<112::aid-cncr2820320115>3.0.co;2-d. [DOI] [PubMed] [Google Scholar]


