Abstract
Cleft lip and palate (CLP) are birth defects that affect the upper lip and the roof of the mouth. CLP has a multifactorial etiology, comprising both genetic and environmental factors. In this review we discuss the recent data on the etiology of cleft lip and palate. We conducted a search of the MEDLINE database (Entrez PubMed) from January 1986 to December 2010 using the key words: ‘cleft lip,’ ‘cleft palate,’ ‘etiology,’ and ‘genetics.’ The etiology of CLP seems complex, with genetics playing a major role. Several genes causing syndromic CLP have been discovered. Three of them—T-box transcription factor-22 (TBX22), poliovirus receptor-like-1 (PVRL1), and interferon regulatory factor-6 (IRF6)—are responsible for causing X-linked cleft palate, cleft lip/palate–ectodermal dysplasia syndrome, and Van der Woude and popliteal pterygium syndromes, respectively; they are also implicated in nonsyndromic CLP. The nature and functions of these genes vary widely, illustrating the high vulnerability within the craniofacial developmental pathways. The etiological complexity of nonsyndromic cleft lip and palate is also exemplified by the large number of candidate genes and loci. To conclude, although the etiology of nonsyndromic CLP is still largely unknown, mutations in candidate genes have been identified in a small proportion of cases. Determining the relative risk of CLP on the basis of genetic background and environmental influence (including smoking, alcohol use, and dietary factors) will be useful for genetic counseling and the development of future preventive measures.
Keywords: Cleft lip, cleft palate, etiology, genetics
INTRODUCTION
Cleft lip (cheiloschisis) and cleft palate (palatoschisis), which can also occur together as cleft lip and palate, are variations of a type of clefting congenital deformity caused by abnormal facial development during gestation. Cleft lip and cleft palate are among the most common congenital malformations. Immediately after birth, individuals with cleft lip and palate (CLP) have facial deformation, feeding problems, and recurrent middle ear infection. Treatment requires interventions from multiple disciplines. At the age of speech acquisition, speech therapy is often needed to correct problems resulting from muscular defects of the cleft. As the individual continues to grow, defects in tooth development and malocclusion require dental and sometimes surgical treatment. The lengthy series of treatments from birth to adulthood is a heavy burden for the patient, family, and society. Various efforts have been made to understand the etiology of CLP so as to predict its occurrence and to prevent it. In recent years, advances in genetics and molecular biology have begun to reveal the basis of craniofacial development, and a number of genes associated with CLP have been identified. An increasing number of studies are being done on the combined genetic and environmental causes of CLP. This article reviews the recently discovered genes involved in CLP, and provides an update on the etiological factors underlying this common malformation.
Clinically, when CLP appears with other (usually two or more) malformations in recognizable patterns, it is classified as syndromic CLP (SCLP). If it appears as an isolated defect or if syndromes cannot be identified, the term nonsyndromic CLP (NSCLP) is used. The number of CLP syndromes is large and still growing.
DATA COLLECTION
A search of Online Mendelian Inheritance in Man (OMIM) database from January 1986 to December 2010 using the key words ‘cleft lip,’ ‘cleft palate,’ ‘etiology,’ and ‘genetics’ yielded close to 600 entries.[1] The distinction between NSCLP and SCLP, however, is sometimes not clear-cut. In families with SCLP, some affected members may present with only CLP because of variable expression of the syndrome. On the other hand, more than 20% of patients with NSCLP were found to have associated congenital malformations in one study.[2] Thus, some cases of SCLP and NSCLP might share a common etiology.
RECENTLY DISCOVERED GENES CAUSING OROFACIAL CLEFT SYNDROMES
T-box transcription factor-22
X-linked cleft palate (CPX) is characterized by isolated cleft palate and ankyloglossia (tongue-tie). The clinical expression of CPX is highly variable. High-arched palate, bifid uvula, or ankyloglossia could be the only presenting sign in affected males. Female carriers could be asymptomatic or they could express the full features of CPX. The syndrome has been found in a number of large families, with inheritance being in a mendelian X-linked semi-dominant pattern. By using genetic linkage analysis, Stanier et al.[3] located the disease gene locus to chromosome Xq21.
Braybrook et al.[4] performed extensive mutation analysis of candidate genes in the region and found mutations of the T-box transcription factor-22 gene (TBX22) in a large Icelandic family with CPX and in several smaller families from other countries. Animal experiments showed that expression of TBX22 was highly restricted to the palatal shelves just before their elevation to adopt a horizontal position, and at the base of the tongue corresponding to the frenulum. Both of these expression patterns closely matched the clinical presentation of CPX. Involvement of TBX22 in NSCLP has recently been indicated from a genome-wide sibling-pair analyses in which the chromosome Xcen-q region, where TBX22 is located, showed promising multipoint logarithm of odds (LOD) scores.[5] Mutation analysis of TBX22 in these patients could reveal whether the gene is involved in NSCLP as well.
Poliovirus receptor-like-1
Cleft lip/palate ectodermal dysplasia syndrome (CLPED) is characterized by cleft lip with or without cleft palate, hidrotic ectodermal dysplasia, syndactyly and, occasionally, mental retardation. Two other syndromes—the Zlotogora-Ogur syndrome and Margarita Island ectodermal dysplasia—are also classified as CLPED. The inheritance of CLPED appears to be autosomal recessive. Using positional cloning, Suzuki et al.[6] identified mutations of the poliovirus receptor-like-1 gene (PVRL1) in CLPED families from Margarita Island, Israel, and Brazil.
The protein product of PVRL1 was initially identified as poliovirus receptor-related protein (PRR). Takahashi et al.[7] confirmed the function of PRR as a cell adhesion molecule, and they renamed it nectin-1. All three PVRL1 mutations found in families with CLPED resulted in truncations in nectin-1, thereby destroying the nectin-afadin-ponsin (NAP)–dependent cell-adhesion system. In animal experiments, PVRL1 was expressed at the medial edge epithelium of the palatal shelves and the skin surface epithelium—locations that corresponded to the clinical phenotypes of CLPED.[6] Interestingly, heterozygous mutation of PVRL1 (W185X) was associated with NSCLP in northern Venezuela.[8] Thus, a certain proportion of NSCLP cases can be explained by PVRL1 mutations.
Interferon regulatory factor-6
Van der Woude syndrome (VDWS) is the most common form of SCLP and accounts for 2% of all CLP cases.[9] This syndrome is characterized by cleft lip with or without cleft palate, isolated cleft palate, pits or mucous cysts on the lower lip, and hypodontia. Popliteal pterygium syndrome (PPS) includes all the features of VDWS plus popliteal pterygium, syngnathia, distinct toe/nail abnormality, syndactyly, and genitourinary malformations. Owing to their clinical similarities, VDWS and PPS were thought to be allelic, i.e., caused by different mutations of the same gene.[10] Clinical expressions of VDWS and PPS are also highly variable; for example, some family members of patients with VDWS present only with Hypodontia, and in PPS, popliteal pterygium is not always present.
In 1990, the genetic locus for VDWS was localized to chromosome 1.[11] Through linkage and chromosomal analysis, the critical area for VDWS was gradually narrowed to 1q32-q41. In 1999, PPS was also linked to the same region.[12] In 2002, Kondo et al.[13] described a pair of monozygotic twins discordant for VDWS whose parents did not have the disorder. The VDWS in the affected twin was thought to arise from somatic mutation. Sequence analysis revealed a point mutation in the interferon regulatory factor-6 gene (IRF6), which is located within the VDWS critical region. Additional mutations of IRF6 were found in 45 unrelated families with VDWS as well as in 13 families with PPS, thereby confirming a common genetic etiology for both syndromes. In animal experiments, IRF6 was expressed in tissues affected by both VDWS and PPS.[13] The phenotypic heterogeneity of VDWS and PPS was shown to be due to different types of IRF6 mutation. In most cases of VDWS, IRF6 mutations produced a nonfunctional protein and haploinsufficiency. The IRF6 mutations, however, were missense mutations that affected the DNA-binding domain and caused a dominant-negative effect, which resulted in severe phenotypes. A partial or modifying role of IRF6 in NSCLP has been demonstrated in a study applying the transmission disequilibrium test, in which specific parental alleles at the VDWS locus were preferentially transmitted to the individuals with NSCLP.[14]
CANDIDATE GENES OR LOCI FOR NONSYNDROMIC CLEFT LIP AND PALATE
Transforming growth factor-alpha
In 1989, Ardinger et al.[15] showed in a case–control study that transforming growth factor-alpha (TGFA) was associated with NSCLP. A number of follow-up studies in different populations provided mixed results. Machida et al.[16] sequenced the TGFA gene in a group of NSCLP patients and found five mutations that could be etiological to orofacial clefts. The combined effect of TGFA mutation and environmental influence in NSCLP has been analyzed by several groups of researchers. The rare TGFA variant (TaqI C2 allele) and maternal smoking together could increase the risk of cleft palate by 6–8 times[17] and that of cleft lip with or without cleft palate by 2 times.[18] If multivitamins are not consumed during the first trimester of pregnancy and the baby is carrying the TGFA TaqI C2 allele, the relative risk for cleft lip with or without cleft palate increased by 3–8 times.[19]
Drosophila msx homeobox homolog-1
Mice lacking a functional Drosophila msx homeobox homolog-1 (MSX1) gene develop a cleft of the secondary palate and tooth agenesis.[20] In humans, MSX1 mutation was first shown to cause an autosomal dominant form of tooth agenesis.[21] Subsequently, van den Boogaard et al.[22] described a family with a common pattern of tooth agenesis and concomitant presence of cleft lip with or without cleft palate; direct sequencing of MSX1 revealed a disease-causing mutation. Recently, a large-scale sequence analysis of MSX1 performed on 917 CLP patients identified mutations in 16 patients with cleft lip with or without cleft palate, or cleft palate alone, providing evidence that this gene could be involved in both forms of cleft.[23] The authors estimated that MSX1 mutations contributed to 2% of all NSCLP cases. A recent study showed that the combined genetic background of rare variants of TGFA and MSX1 could increase the risk of cleft palate by up to 9.7 times, demonstrating the significance of gene–gene interaction in the etiology of NSCLP.[24]
5,10-Methylenetetrahydrofolate reductase
The association between folic acid deficiency and neural tube defects has been well established. 5,10 Methylenetetrahydrofolate reductase (MTHFR) is the enzyme responsible for catalyzing the conversion of 5,10-methylenetetrahydrofolate into 5-methyltetrahydrofolate in the folate metabolism pathway. The MTHFR C677T single-nucleotide polymorphism (SNP) is thermally labile and considered a risk factor for neural tube defects.[25] In NSCLP, the MTHFR C677T genotype in the mother conferred a risk of CLP in offspring that was increased by 4.6 times.[26] In periconceptional folic acid deficiency, the MTHFR thermally labile variant could lead to a risk of CLP that was increased by 10 times.[27]
Transforming growth factor-beta-3
Mice lacking a functional gene encoding transforming growth factor-beta-3 (TGFB3) displayed cleft palate because of defective adhesion of opposing palatal shelves.[28] In humans, TGFB3 was associated with NSCLP in different populations.[24,29] A newly discovered SNP of TGFB3 (IVS5+104 A>G) increased the risk of CLP by up to 16 times in a Korean population.[30]
Other genes and loci
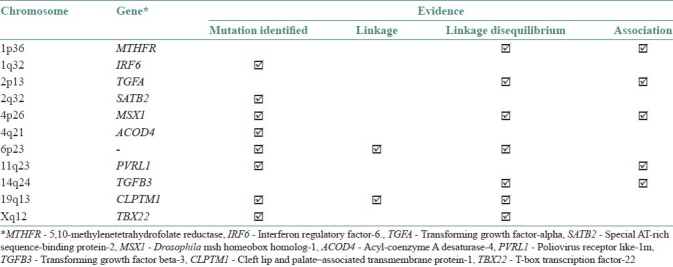
The special AT-rich sequence-binding protein-2 gene (SATB2) located at chromosome 2q32-33 was disturbed in two unrelated patients with cleft palate.[31] Involvement of this gene in palatogenesis was confirmed by expression analysis. Although an initial search for SATB2 mutations in 70 patients with cleft palate was negative, the gene could still be responsible for other CLP cases. Markers from chromosome 4q21 have been linked to familial NSCLP.[32] The acyl-coenzyme A desaturase-4 gene (ACOD4) from chromosome 4q21 was recently found disrupted in a family with cleft lip.[33] Mutation analysis of ACOD4 in families with 4q-linked CLP or other patients with CLP might reveal more mutations. Yoshiura et al.[34] reported a family with CLP in three generations; all affected members had a balanced translocation at chromosome 19q13. Breakpoint cloning revealed a novel gene that was termed ‘cleft lip and palate–associated transmembrane protein-1’ (CLPTM1). Eight rare variants of CLPTM1 were found in 74 patients with NSCLP, but none was significantly associated with cleft lip or palate. The authors concluded that CLPTM1 was not a major contributor to CLP. On the other hand, the same region of chromosome 19q13 has been implicated in NSCLP through linkage[35] and transmission disequilibrium studies.[36] Thus, CLPTM1 or other genes in this locus could still be associated with NSCLP. Chromosome 6p23 has been indicated to be involved in NSCLP by linkage studies.[5,37] Chromosomal aberrations involving 6p23 in patients with CLP have also been reported.[38] It is therefore likely that an as yet unidentified CLP gene exists at chromosome 6p23. A summary of the genes and loci implicated in NSCLP, along with chromosomal locations and other available evidence, is presented in Table 1.
Table 1.
Candidate genes or loci implicated in the etiology of nonsyndromic cleft lip and palate, and the available evidence
In addition to the genes and loci mentioned above, a number of other candidate genes have also demonstrated linkage to cleft lip and palate, but the reports have been contradictory. These other genes include the proto-oncogenes BCL3 (B-cell lymphoma 3) on chromosome 19q13.1-q13.2 and SKI (sarcoma viral oncogene homolog) on chromosome 1q22-q24, as well as the retinoic acid receptor–alpha (RARA) gene on chromosome 17q21.[39–41] More recent genome-wide linkage studies in families with multiple cases of NSCLP indicate that no single major cleft lip and palate locus exists and a multifactorial model is the most likely explanation of the genetic component of this disorder.[42–47] A role for these candidate genes therefore remains to be firmly established, but it is not unreasonable to suggest that these genes together and/or individually might have a modifying or additive role in the etiology of NSCLP.
ENVIRONMENTAL FACTORS
Smoking
The relationship between maternal smoking and CLP is not strong, but it is significant. Several studies have consistently yielded a relative risk of about 1.3–1.5.[48] When maternal smoking was considered together with a positive genetic background, the combined effect was more significant. Furthermore, van Rooij et al.[49] found that a maternal glutathione s-transferase (GSTT1) genotype, when combined with smoking, could significantly increase the risk of CLP (odds ratio=4.9). Beaty et al.[50] reported that maternal smoking and infant MSX1 genotypes acted together to increase the risk for CLP by 7.16 times.
Alcohol use
Heavy maternal drinking, apart from causing fetal alcohol syndrome, also increases the risk of CLP. Munger et al.[51] showed that maternal drinking increased the risk for CLP by 1.5–4.7 times in a dose-dependent manner. The results were supported by Shaw and Lammer[52] who showed that mothers who consumed more than five drinks per occasion had 3.4 times increased risk of delivering an infant with CLP. Low-level alcohol consumption, however, did not seem to increase the risk of orofacial clefts.[53] The link between alcohol consumption and genotypes on the risk of CLP has yet to be demonstrated.
Use of folic acid and multivitamins
Shaw et al.[54] reported that if vitamin supplements namely folic acid and cobalamins were not taken during early pregnancy the risk for CLP could be tripled. Folic acid deficiency with a pre-existing TGFA TaqI C2 genotype was also found to increase the risk of CLP.[55] In addition, defective maternal vitamin-dependent homocysteine metabolism is a risk factor for CLP in the offspring. In a case–control study, mothers of patients with CLP had significantly higher homocysteine level, lower level of whole-blood vitamin B6, and higher rate of hyperhomocysteinemia.[56] The role of folic acid supplementation in the prevention of CLP has been investigated in several studies. It seems that low-dose folic acid supplementation by fortification of cereal grain products cannot protect against CLP.[57] Only a very high dose of supplementary folic acid (10 mg/day) could reduce the risk of CLP significantly (65% reduction was observed).[58]
Steroids
Corticosteroids form the first-line drugs for the management of a variety of conditions in women of childbearing age. The clefting role of corticosteroid in animal models is well known.[59] CLP is induced in the progeny of pregnant mice that are given glucocorticoids. The incidence, however, varies among inbred strains and also with the dose given and the stage of gestation when the drug is given. Diewert and Pratt[60] found that cortisone not only affected the content of extracellular matrix (ECM) and the number of palatal shelf cells in A/J mice but that shelf elevation was delayed and only half of the cortisone-treated palates achieved complete horizontal positioning of the shelves in all regions of the palate. Melnick et al.[61] studied the teratological effects on lip morphogenesis after the administration of triamcinolone hexacetonide on the eighth day of gestation. The frequency of CLP in treated A/J mice was found to be more than three times greater than the spontaneous frequency in untreated controls. Affected A/J embryos showed a severe reduction in the size of the lateral nasal processes. Gasser et al.[62] examined strains of mice for susceptibility to cortisone-induced CLP and confirmed the role of genes linked to H-2 on chromosome 17. Later, the same group[63] refined the chromosome region carrying the cleft palate susceptibility-1 (Cps-1) gene. Juriloff and Mah[64] mapped a major CL(P)-causing gene to mouse chromosome 11 in a region having linkage homology with human 17q21 through 24.
Studies have investigated the association between maternal corticosteroid use during the periconceptional period (1 month before conception to 3 months after conception) and the delivery of infants with selected congenital anomalies. Carmichael and Shaw[65] found an increased risk of NSCLP. A Spanish case–control study by Rodriguez-Pinilla and Martinez-Frias found an association between maternal systemic use of glucocorticoids and the birth of an infant with CLP, based on five exposed patients, one of which had multiple malformations and may have been a trisomy 13.[66] Park-Wyllie et al.[67] have also demonstrated that although prednisone does not represent a major teratogenic risk in human beings at therapeutic doses, it does increase the risk of oral cleft by 3.4-fold, which is consistent with the findings of existing animal studies. A retrospective study by Pradat et al. found a positive association between systemic corticoids use and the occurrence of cleft lip with or without cleft palate.[68] Similarly, as has been reported in a previous study, Carmichael et al. in a recent population-based case–control investigation observed a moderately increased risk of CLP in the offspring of women who used corticosteroids during early pregnancy.[69]
Anticonvulsants
Anticonvulsants (phenytoin/hydantoin, oxazolidinones, and valproic acid) are associated with a clearly demonstrated increased risk for congenital defects.[70] All three therapeutic classes are liable to produce CLP, although inconsistently, as part of severe and significantly overlapping embryopathies. It is also worth noting that a significant increase in benzodiazepine use was detected in mothers of infants with cleft palate alone, and a nonsignificant increase was found in mothers of CLP infants.[71] Safra and Oakley[72] reported the association of CLP with first trimester exposure to diazepam. In a further study, Czeizel et al.[73] addressed the question of benzodiazepine teratogenicity as a whole. Although diazepam at high doses is a weak teratogen in susceptible mice, its interference with fetal face development is probably modest or nonexistent. It is well known that women with epilepsy have an increased risk of having offspring with orofacial clefts. This risk has been attributed mostly to the teratogenic effects of antiepileptic drugs, but other risk factors have also been suggested, including epilepsy per se or some underlying genetic defects associated with epilepsy.[74]
COMMON OROFACIAL CLEFT LIP AND PALATE SYNDROMES AND THEIR UNDERLYING GENETIC BASIS
Apert syndrome
Wilkie et al. identified one of two mutations in exon 7 of the FGFR2 gene–S252W or P253R–in all 40 unrelated patients with Apert syndrome in their series. The findings confirmed that Apert syndrome is allelic with Crouzon syndrome. In a patient with Apert syndrome, Oldridge et al. identified a non-canonical mutation in exon 7 of the FGFR2 gene. In a series of 260 cases of Apert syndrome, Oldridge et al. found that 172 carried the S252W mutations and 85 had the P253R mutation, indicating that the molecular mechanism of Apert syndrome is exquisitely specific. Lajeunie et al. also identified the S252W and P253R mutations in 23 (64%) and 12 (33%) of 36 Apert syndrome patients, respectively. One affected fetus had the S252F mutation. Moloney et al. found that 74 of 118 patients with Apert syndrome had the FGFR2 S252W mutation and 44 had the P253R mutation.[75–79]
Crouzon syndrome
Rollnick[80] described 21 affected brothers born to normal, unrelated parents and proposed germinal mosaicism as the explanation for the manifestation of Crouzon syndrome. Kreiborg and Cohen[81] suggested germinal mosaicism as the basis for Crouzon syndrome in two affected siblings with the same mother but different fathers. The mother and both fathers were completely normal. Meyers et al.[82] reported that the two patients with Crouzon syndrome in this kindred had different mutations: One had Crouzon syndrome caused by an FGFR2 ser347-to-cys mutation, whereas the other patient had Crouzon syndrome with acanthosis nigricans due to an FGFR3 ala391-to-glu mutation. In a large kindred with Crouzon craniofacial dysostosis, Preston et al.[85] found linkage between CFD1 and three loci (DlOSI90, DlOS209, and DI0S216 markers) that span a 13-cM region on chromosome 109. Preston et al. noted that a newly available and highly informative marker, DlOS587, located 7 cM distal to DlOS209, increased the linkage between CFD 1 and D10S209. Two of the genetic marker loci to which the CFD 1 locus is tightly linked are within l0q25-q26. The developmental gene PAX2 maps to l0q25 and is therefore an attractive candidate gene. Reardon et al.[79] demonstrated mutations in the FGFR2 gene in 9 of 20 patients with Crouzon syndrome. Because linkage studies showed no evidence of genetic heterogeneity, the authors concluded that mutations in parts of the FGFR2 gene other than in the B exon were responsible for the remaining cases.
Hemifacial microsomia
Keegan et al.[83] performed a retrospective analysis of eight patients with Hemifacial microsomia (HFM)-expanded spectrum and anal anomalies to determine whether this subset had Townes-Brocks syndrome (TBS). Two patients had major phenotypic findings of TBS. Sequencing of the SALL1 (SAL-like 1) gene in four of the eight patients revealed one with a C-to-T transition resulting in a nonsense mutation arg276 to a mutation hotspot. Keegan et al.[83] suggested that patients with overlapping features of both Townes-Brocks syndrome and hemifacial microsomia–expanded spectrum should be screened for SALL1 mutations. Kelberrnan et al.[84,85] performed a genome-wide search for linkage in two families with features of hemifacial microsomia. In one family, the data were highly suggestive of linkage to a region of approximately 10.7 cM on chromosome 14q32, between microsatellite markers D14S987 and D14S65. Linkage to this region was included in the second family, suggesting genetic heterogeneity. Based on mapping, mouse expression, and phenotype data, Kelberman et al. considered the goosecoid (GSC) gene to be an excellent candidate gene for hemifacial microsomia.[88,89]
Pierre Robin syndrome
Houdayer et al. described the association of Pierre Robin sequence with deletion 2q32.3-q33.2. They refined the deletion interval by molecular analysis and found that it mapped to a chromosome region previously shown to have a nonrandom association with cleft palate.[90]
Treacher Collins syndrome
Treacher Collins syndrome (TCS) is an autosomal dominant disorder with variable expression. Intrafamilial variation is wide. There seems to be a significant increase in affected offspring from affected females and a decrease in affected offspring from affected males. Splendore et al. found that 2 of 28 families with TCS did not show apparent pathogenic mutation in the TCOFI gene (Treacher Collins–Franceschetti syndrome 1). They suggested the possibility of a different mechanism leading to TCS or genetic heterogeneity for this condition. Wise et al. postulated that the disorder resulted from defects in a nucleolar trafficking protein that is critically required during human craniofacial development. Marsh et al. suggested that the disorder results from aberrant expression of a nucleolar protein. They observed that mutations in the TCOFI gene (606847) cause truncated proteins to be mislocalized within the cell. Balestrazzi et al., described TCS in a girl with a de novo balanced translocation involving chromosome 5. The level of hexosaminidase B was decreased; the HEXB locus is thought to be at 5q 13. The possibility that the TCS locus is on 5q was raised by these findings. Am et al. described a mild but entirely typical case of TCS in association with a small interstitial deletion of 3p: 46, XY, del (3) (p23p24.l2). By the time Am et al. reported this case, the TCS locus in familial cases had been assigned to 5q31.3. Jabs et al. observed a patient with severe manifestations of TCS and a de novo chromosomal deletion in region 4pI5.32-pI4.[91–97]
The complexity and heterogeneity of CLP as shown by its extensive involvement in craniofacial syndromes and the number of anticipated candidate genes could be anticipated from the long developmental duration of the primary and secondary palates. Disruption of the coordinated migration and fusion of various facial processes by genetic, environmental, or combined factors at any time point could lead to CLP. Genes such as those encoding transcription factors (e.g., TBX22, MSX1), growth factors (e.g., TGFA, TGFB3), and adhesion molecules (e.g., PVRL1) have all been implicated in the etiology of CLP. In the search for the genes causing SCLP, current methods of positional cloning or positional candidate approaches could be applied to families or patients. With the completion of the sequencing of the human genome, gene discovery has been accelerated by the availability of target sequences. Close collaboration between clinicians and scientists is still essential, as illustrated by the example of VDWS.
The future search for genes in NSCLP will not be straightforward. Mutations in SCLP genes or other candidate genes so far could only be found in a handful of NSCLP cases or families. Promising NSCLP gene candidates, such as MSX1, were expected to cause up to 2% of NSCLP cases.[23] The proportion was remarkably similar to that of VDWS in all CLP cases. Therefore, MSX1 mutations may represent a new syndrome, which has variable penetrance for the CLP and tooth agenesis phenotypes.
Instead of directly searching for disease-causing mutations in NSCLP, studies exploring the relative risk imparted by candidate genes and gene–environment interactions are becoming popular approaches for several reasons. Firstly, the amount of sequence data, such as SNPs, on candidate genes is constantly increasing. These sequence data not only allow more CLP-associated mutations to be identified but also allow functional correlation to be attributed to some of these subtle variations. Secondly, high-throughput genotyping such as DNA microarray analyses is now more readily available, and a large number of candidate genes and SNPs can now be tested simultaneously. In the near future, the relative contribution from these candidate CLP genes could be integrated into a genetic test for estimating the weighted risk of CLP. Such data could provide additional information on prospective parents in genetic counseling, which will allow preventive measures, including dietary supplementation and lifestyle modifications, to be prescribed accordingly.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
REFERENCES
- 1.Online Mendelian Inheritance in Man. [Last accessed 2011 Jan 3]. National Library of Medicine website: Available from: http://www.ncbi.nlm.nih.gov/omim/
- 2.Stoll C, Alembik Y, Dott B, Roth MP. Associated malformations in cases with oral clefts. Cleft Palate Craniofac J. 2000;37:41–7. doi: 10.1597/1545-1569_2000_037_0041_amicwo_2.3.co_2. [DOI] [PubMed] [Google Scholar]
- 3.Stanier P, Forbes SA, Arnason A, Bjornsson A, Sveinbjornsdottir E, Williamson R, et al. The localization of a gene causing X-linked cleft palate and ankyloglossia (CPX) in an Icelandic kindred is between DXS326 and DXYS1X. Genomics. 1993;17:549–55. doi: 10.1006/geno.1993.1370. [DOI] [PubMed] [Google Scholar]
- 4.Braybrook C, Doudney K, Marçano AC, Arnason A, Bjornsson A, Patton MA, et al. The T-box transcription factor gene TBX22 is mutated in X-linked cleft palate and ankyloglossia. Nat Genet. 2001;29:179–83. doi: 10.1038/ng730. [DOI] [PubMed] [Google Scholar]
- 5.Prescott NJ, Lees MM, Winter RM, Malcolm S. Identification of susceptibility loci for nonsyndromic cleft lip with or without cleft palate in a two stage genome scan of affected sib-pairs. Hum Genet. 2000;106:345–50. doi: 10.1007/s004390051048. [DOI] [PubMed] [Google Scholar]
- 6.Suzuki K, Hu D, Bustos T, Zlotogora J, Richieri-Costa A, Helms JA, et al. Mutations of PVRL1, encoding a cell-cell adhesion molecule/herpesvirus receptor, in cleft lip/palate-ectodermal dysplasia. Nat Genet. 2000;25:427–30. doi: 10.1038/78119. [DOI] [PubMed] [Google Scholar]
- 7.Takahashi K, Nakanishi H, Miyahara M, Mandai K, Satoh K, Satoh A, et al. Nectin/PRR: An immunoglobulin-like cell adhesion molecule recruited to cadherin-based adherens junctions through interaction with Afadin, a PDZ domain-containing protein. J Cell Biol. 1999;145:539–49. doi: 10.1083/jcb.145.3.539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Sözen MA, Suzuki K, Tolarova MM, Bustos T, Fernández Iglesias JE, Spritz RA. Mutation of PVRL1 is associated with sporadic, non-syndromic cleft lip/palate in northern Venezuela. Nat Genet. 2001;29:141–2. doi: 10.1038/ng740. [DOI] [PubMed] [Google Scholar]
- 9.Burdick AB. Genetic epidemiology and control of genetic expression in van der Woude syndrome. J Craniofac Genet Dev Biol Suppl. 1986;2:99–105. [PubMed] [Google Scholar]
- 10.Bixler D, Poland C, Nance WE. Phenotypic variation in the popliteal pterygium syndrome. Clin Genet. 1973;4:220–8. doi: 10.1111/j.1399-0004.1973.tb01146.x. [DOI] [PubMed] [Google Scholar]
- 11.Murray JC, Nishimura DY, Buetow KH, Ardinger HH, Spence MA, Sparkes RS, et al. Linkage of an autosomal dominant clefting syndrome (Van der Woude) to loci on chromosome Iq. Am J Hum Genet. 1990;46:486–91. [PMC free article] [PubMed] [Google Scholar]
- 12.Lees MM, Winter RM, Malcolm S, Saal HM, Chitty L. Popliteal pterygium syndrome: A clinical study of three families and report of linkage to the Van der Woude syndrome locus on 1q32. J Med Genet. 1999;36:888–92. [PMC free article] [PubMed] [Google Scholar]
- 13.Kondo S, Schutte BC, Richardson RJ, Bjork BC, Knight AS, Watanabe Y, et al. Mutations in IRF6 cause Van der Woude and popliteal pterygium syndromes. Nat Genet. 2002;32:285–9. doi: 10.1038/ng985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Houdayer C, Bonaïti-Pellié C, Erguy C, Soupre V, Dondon MG, Bürglen L, et al. Possible relationship between the van der Woude syndrome (vWS) locus and nonsyndromic cleft lip with or without cleft palate (NSCL/P) Am J Med Genet. 2001;104:86–92. doi: 10.1002/1096-8628(20011115)104:1<86::aid-ajmg10053>3.0.co;2-e. [DOI] [PubMed] [Google Scholar]
- 15.Ardinger HH, Buetow KH, Bell GI, Bardach J, VanDemark DR, Murray JC. Association of genetic variation of the transforming growth factor-alpha gene with cleft lip and palate. Am J Hum Genet. 1989;45:348–53. [PMC free article] [PubMed] [Google Scholar]
- 16.Machida J, Yoshiura K, Funkhauser CD, Natsume N, Kawai T, Murray JC. Transforming growth factor-alpha (TGFA): Genomic structure, boundary sequences, and mutation analysis in nonsyndromic cleft lip/palate and cleft palate only. Genomics. 1999;61:237–42. doi: 10.1006/geno.1999.5962. [DOI] [PubMed] [Google Scholar]
- 17.Hwang SJ, Beaty TH, Panny SR, Street NA, Joseph JM, Gordon S, et al. Association study of transforming growth factor alpha (TGF alpha) TaqI polymorphism and oral clefts: Indication of gene-environment interaction in a population-based sample of infants with birth defects. Am J Epidemiol. 1995;141:629–36. doi: 10.1093/oxfordjournals.aje.a117478. [DOI] [PubMed] [Google Scholar]
- 18.Shaw GM, Wasserman CR, Lammer EJ, O’Malley CD, Murray JC, Basart AM, et al. Orofacial clefts, parental cigarette smoking, and transforming growth factor-alpha gene variants. Am J Hum Genet. 1996;58:551–61. [PMC free article] [PubMed] [Google Scholar]
- 19.Shaw GM, Wasserman CR, Murray JC, Lammer EJ. Infant TGF-alpha genotype, orofacial clefts, and maternal periconceptional multivitamin use. Cleft Palate Craniofac J. 1998;35:366–70. doi: 10.1597/1545-1569_1998_035_0366_itagoc_2.3.co_2. [DOI] [PubMed] [Google Scholar]
- 20.Satokata I, Maas R. Msx1 deficient mice exhibit cleft palate and abnormalities of craniofacial and tooth development. Nat Genet. 1994;6:348–56. doi: 10.1038/ng0494-348. [DOI] [PubMed] [Google Scholar]
- 21.Vastardis H, Karimbux N, Guthua SW, Seidman JG, Seidman CE. A human MSX1 homeodomain missense mutation causes selective tooth agenesis. Nat Genet. 1996;13:417–21. doi: 10.1038/ng0896-417. [DOI] [PubMed] [Google Scholar]
- 22.van den Boogaard MJ, Dorland M, Beemer FA, van Amstel HK. MSX1 mutation is associated with orofacial clefting and tooth agenesis in humans. Nat Genet. 2000;24:342–3. doi: 10.1038/74155. [DOI] [PubMed] [Google Scholar]
- 23.Jezewski PA, Vieira AR, Nishimura C, Ludwig B, Johnson M, O’Brien SE, et al. Complete sequencing shows a role for MSX1 in non-syndromic cleft lip and palate. J Med Genet. 2003;40:399–407. doi: 10.1136/jmg.40.6.399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Jugessur A, Lie RT, Wilcox AJ, Murray JC, Taylor JA, Saugstad OD, et al. Variants of developmental genes (TGFA, TGFB3, and MSX1) and their associations with orofacial clefts: A case-parent triad analysis. Genet Epidemiol. 2003;24:230–9. doi: 10.1002/gepi.10223. [DOI] [PubMed] [Google Scholar]
- 25.van der Put NM, Steegers-Theunissen RP, Frosst P, Trijbels FJ, Eskes TK, van den Heuvel LP, et al. Mutated methylenetetrahydrofolate reductase as a risk factor for spina bifida. Lancet. 1995;346:1070–1. doi: 10.1016/s0140-6736(95)91743-8. [DOI] [PubMed] [Google Scholar]
- 26.Prescott NJ, Winter RM, Malcolm S. Maternal MTHFR genotype contributes to the risk of non-syndromic cleft lip and palate. J Med Genet. 2002;39:368–9. doi: 10.1136/jmg.39.5.368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.van Rooij IA, Vermeij-Keers C, Kluijtmans LA, Ocké MC, Zielhuis GA, Goorhuis-Brouwer SM, et al. Does the interaction between maternal folate intake and the methylenetetrahydrofolate reductase polymorphisms affect the risk of cleft lip with or without cleft palate? Am J Epidemiol. 2003;157:583–91. doi: 10.1093/aje/kwg005. [DOI] [PubMed] [Google Scholar]
- 28.Proetzel G, Pawlowski SA, Wiles MV, Yin M, Boivin GP, Howles PN, et al. Transforming growth factor-beta 3 is required for secondary palate fusion. Nat Genet. 1995;11:409–14. doi: 10.1038/ng1295-409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Vieira AR, Orioli IM, Castilla EE, Cooper ME, Marazita ML, Murray JC. MSX1 and TGFB3 contribute to clefting in South America. J Dent Res. 2003;82:289–92. doi: 10.1177/154405910308200409. [DOI] [PubMed] [Google Scholar]
- 30.Kim MH, Kim HJ, Choi JY, Nahm DS. Transforming growth factor-beta3 gene SfaN1 polymorphism in Korean nonsyndromic cleft lip and palate patients. J Biochem Mol Biol. 2003;36:533–7. doi: 10.5483/bmbrep.2003.36.6.533. [DOI] [PubMed] [Google Scholar]
- 31.FitzPatrick DR, Carr IM, McLaren L, Leek JP, Wightman P, Williamson K, et al. Identification of SATB2 as the cleft palate gene on 2q32-q33. Hum Mol Genet. 2003;12:2491–501. doi: 10.1093/hmg/ddg248. [DOI] [PubMed] [Google Scholar]
- 32.Beiraghi S, Foroud T, Diouhy S, Bixler D, Conneally PM, Delozier-Blanchet D, et al. Possible localization of a major gene for cleft lip and palate to 4q. Clin Genet. 1994;46:255–6. doi: 10.1111/j.1399-0004.1994.tb04236.x. [DOI] [PubMed] [Google Scholar]
- 33.Beiraghi S, Zhou M, Talmadge CB, Went-Sumegi N, Davis JR, Huang D, et al. Identification and characterization of a novel gene disrupted by a pericentric inversion inv(4)(p13.1q21.1) in a family with cleft lip. Gene. 2003;309:11–21. doi: 10.1016/s0378-1119(03)00461-x. [DOI] [PubMed] [Google Scholar]
- 34.Yoshiura K, Machida J, Daack-Hirsch S, Patil SR, Ashworth LK, Hecht JT, et al. Characterization of a novel gene disrupted by a balanced chromosomal translocation t(2;19)(q11.2;q13.3) in a family with cleft lip and palate. Genomics. 1998;54:231–40. doi: 10.1006/geno.1998.5577. [DOI] [PubMed] [Google Scholar]
- 35.Stein J, Mulliken JB, Stal S, Gasser DL, Malcolm S, Winter R, et al. Nonsyndromic cleft lip with or without cleft palate: Evidence of linkage to BCL3 in 17 multigenerational families. Am J Hum Genet. 1995;57:257–72. [PMC free article] [PubMed] [Google Scholar]
- 36.Wyszynski DF, Maestri N, McIntosh I, Smith EA, Lewanda AF, Garcia-Delgado C, et al. Evidence for an association between markers on chromosome 19q and nonsyndromic cleft lip with or without cleft palate in two groups of multiplex families. Hum Genet. 1997;99:22–6. doi: 10.1007/s004390050303. [DOI] [PubMed] [Google Scholar]
- 37.Eiberg H, Bixler D, Nielsen LS, Conneally PM, Mohr J. Suggestion of linkage of a major locus for nonsyndromic orofacial cleft with F13A and tentative assignment to chromosome 6. Clin Genet. 1987;32:129–32. doi: 10.1111/j.1399-0004.1987.tb03340.x. [DOI] [PubMed] [Google Scholar]
- 38.Davies AF, Stephens RJ, Olavesen MG, Heather L, Dixon MJ, Magee A, et al. Evidence of a locus for orofacial clefting on human chromosome 6p24 and STS content map of the region. Hum Mol Genet. 1995;4:121–8. doi: 10.1093/hmg/4.1.121. [DOI] [PubMed] [Google Scholar]
- 39.Jagomägi T, Nikopensius T, Krjutskov K, Tammekivi V, Viltrop T, Saag M, et al. MTHFR and MSX1 contribute to the risk of nonsyndromic cleft lip/palate. Eur J Oral Sci. 2010;118:213–20. doi: 10.1111/j.1600-0722.2010.00729.x. [DOI] [PubMed] [Google Scholar]
- 40.Lidral AC, Moreno LM. Progress toward discerning the genetics of cleft lip. Curr Opin Pediatr. 2005;17:731–9. doi: 10.1097/01.mop.0000185138.65820.7f. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Vieira AR, Avila JR, Daack-Hirsch S, Dragan E, Félix TM, Rahimov F, et al. Medical sequencing of candidate genes for non-syndromic cleft lip and palate. PLoS Genet. 2005;1:e64. doi: 10.1371/journal.pgen.0010064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Maestri NE, Beaty TH, Hetmanski J, Smith EA, McIntosh I, Wyszynski DF, et al. Application of transmission disequilibrium tests to non-syndromic oral clefts: Including candidate genes and environmental exposures in the models. Am J Med Genet. 1997;73:337–44. doi: 10.1002/(sici)1096-8628(19971219)73:3<337::aid-ajmg21>3.0.co;2-j. [DOI] [PubMed] [Google Scholar]
- 43.Marazita ML, Murray JC, Lidral AC, Arcos-Burgos M, Cooper ME, Goldstein T, et al. Meta-analysis of 13 genome scans reveals multiple cleft lip/palate genes with novel loci on 9q21 and 2q32-35. Am J Hum Genet. 2004;75:161–73. doi: 10.1086/422475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Gaspar DA, Matioli SR, Pavanello RC, Araújo BC, André M, Steman S, et al. Evidence that BCL3 plays a role in the etiology of nonsyndromic oral clefts in Brazilian families. Genet Epidemiol. 2002;23:364–74. doi: 10.1002/gepi.10189. [DOI] [PubMed] [Google Scholar]
- 45.Blanco R, Suazo J, Santos JL, Paredes M, Sung H, Carreño H, et al. Association between 10 microsatellite markers and nonsyndromic cleft lip palate in the Chilean population. Cleft Palate Craniofac J. 2004;41:163–7. doi: 10.1597/02-147. [DOI] [PubMed] [Google Scholar]
- 46.Park BY, Sull JW, Park JY, Jee SH, Beaty TH. Differential parental transmission of markers in BCL3 among Korean cleft case-parent trios. J Prev Med Public Health. 2009;42:1–4. doi: 10.3961/jpmph.2009.42.1.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Moreno LM, Arcos-Burgos M, Marazita ML, Krahn K, Maher BS, Cooper ME, et al. Genetic analysis of candidate loci in non-syndromic cleft lip families from Antioquia-Colombia and Ohio. Am J Med Genet Part A. 2004;125A:135–44. doi: 10.1002/ajmg.a.20425. [DOI] [PubMed] [Google Scholar]
- 48.Wyszynski DF, Wu T. Use of US birth certificate data to estimate the risk of maternal cigarette smoking for oral clefting. Cleft Palate Craniofac J. 2002;39:188–92. doi: 10.1597/1545-1569_2002_039_0188_uousbc_2.0.co_2. [DOI] [PubMed] [Google Scholar]
- 49.van Rooij IA, Wegerif MJ, Roelofs HM, Peters WH, Kuijpers-Jagtman AM, Zielhuis GA, et al. Smoking, genetic polymorphisms in biotransformation enzymes, and nonsyndromic oral clefting: A gene-environment interaction. Epidemiology. 2001;12:502–7. doi: 10.1097/00001648-200109000-00007. [DOI] [PubMed] [Google Scholar]
- 50.Beaty TH, Hetmanski JB, Zeiger JS, Fan YT, Liang KY, VanderKolk CA, et al. testing candidate genes for non-syndromic oral clefts using a case-parent trio design. Genet Epidemiol. 2002;22:1–11. doi: 10.1002/gepi.1039. [DOI] [PubMed] [Google Scholar]
- 51.Munger RG, Romitti PA, Daack-Hirsch S, Burns TL, Murray JC, Hanson J. Maternal alcohol use and risk of orofacial cleft birth defects. Teratology. 1996;54:27–33. doi: 10.1002/(SICI)1096-9926(199607)54:1<27::AID-TERA4>3.0.CO;2-0. [DOI] [PubMed] [Google Scholar]
- 52.Shaw GM, Lammer EJ. Maternal periconceptional alcohol consumption and risk for orofacial clefts. J Pediatr. 1999;134:298–303. doi: 10.1016/s0022-3476(99)70453-1. [DOI] [PubMed] [Google Scholar]
- 53.Natsume N, Kawai T, Ogi N, Yoshida W. Maternal risk factors in cleft lip and palate: Case control study. Br J Oral Maxillofac Surg. 2000;38:23–5. doi: 10.1054/bjom.1999.0133. [DOI] [PubMed] [Google Scholar]
- 54.Shaw GM, Nelson V, Carmichael SL, Lammer EJ, Finnell RH, Rosenquist TH. Maternal periconceptional vitamins: Interactions with selected factors and congenital anomalies? Epidemiology. 2002;13:625–30. doi: 10.1097/00001648-200211000-00005. [DOI] [PubMed] [Google Scholar]
- 55.Jugessur A, Lie RT, Wilcox AJ, Murray JC, Taylor JA, Saugstad OD, et al. Cleft palate, transforming growth factor alpha gene variants, and maternal exposures: Assessing gene-environment interactions in case-parent triads. Genet Epidemiol. 2003;25:367–74. doi: 10.1002/gepi.10268. [DOI] [PubMed] [Google Scholar]
- 56.Wong WY, Eskes TK, Kuijpers-Jagtman AM, Spauwen PH, Steegers EA, Thomas CM, et al. Nonsyndromic orofacial clefts: Association with maternal hyperhomocysteinemia. Teratology. 1999;60:253–7. doi: 10.1002/(SICI)1096-9926(199911)60:5<253::AID-TERA4>3.0.CO;2-V. [DOI] [PubMed] [Google Scholar]
- 57.Ray JG, Meier C, Vermeulen MJ, Wyatt PR, Cole DE. Association between folic acid food fortification and congenital orofacial clefts. J Pediatr. 2003;143:805–7. doi: 10.1067/S0022-3476(03)00495-5. [DOI] [PubMed] [Google Scholar]
- 58.Tolarova M, Harris J. Reduced recurrence of orofacial clefts after periconceptional supplementation with high-dose folic acid and multivitamins. Teratology. 1995;51:71–8. doi: 10.1002/tera.1420510205. [DOI] [PubMed] [Google Scholar]
- 59.Baxter H, Fraser FC. Production of congenital defects in offspring of female mice treated with cortisone. McGill Med J. 1950;19:245–9. [PubMed] [Google Scholar]
- 60.Diewert VM, Pratt RM. Cortisone-induced cleft palate in A/J mice: Failure of palatal shelf contact. Teratology. 1981;24:149–62. doi: 10.1002/tera.1420240206. [DOI] [PubMed] [Google Scholar]
- 61.Melnick M, Jaskoll T, Slavkin HC. Corticosteroid-induced cleft lip in mice: A teratologic, topographic, and histologic investigation. Am J Med Genet. 1981;10:333–50. doi: 10.1002/ajmg.1320100406. [DOI] [PubMed] [Google Scholar]
- 62.Gasser DL, Mele L, Lees DD, Goldman AS. Genes in mice that affect susceptibility to cortisone-induced cleft palate are closely linked to Ir genes on chromosomes 2 and 17. Proc Natl Acad Sci U S A. 1981;78:3147–50. doi: 10.1073/pnas.78.5.3147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Gasser DL, Goldner-Sauvé A, Katsumata M, Goldman AS. Restriction fragment length polymorphisms, glucocorticoid receptors, and phenytoin-induced cleft palate in congenic strains of mice with steroid susceptibility differences. J Craniofac Genet Dev Biol. 1991;11:366–71. [PubMed] [Google Scholar]
- 64.Juriloff DM, Mah DG. The major locus for multifactorial non-syndromic cleft lip maps to mouse chromosome 11. Mamm Genome. 1995;6:63–9. doi: 10.1007/BF00303246. [DOI] [PubMed] [Google Scholar]
- 65.Carmichael SL, Shaw GM. Maternal corticosteroid use and risk of selected congenital anomalies. Am J Med Genet. 1999;86:242–4. doi: 10.1002/(sici)1096-8628(19990917)86:3<242::aid-ajmg9>3.0.co;2-u. [DOI] [PubMed] [Google Scholar]
- 66.Rodriquez-Pinilla E, Martınez-Frıas ML. Corticosteroids during pregnancy and oral clefts: A case-control study. Teratology. 1998;58:2–5. doi: 10.1002/(SICI)1096-9926(199807)58:1<2::AID-TERA2>3.0.CO;2-4. [DOI] [PubMed] [Google Scholar]
- 67.Park-Wyllie L, Mazzotta P, Pastuszak A, Moretti ME, Beique L, Hunnisett L, et al. Birth defects after maternal exposure to corticosteroids: Prospective cohort study and meta-analysis of epidemiological studies. Teratology. 2000;62:385–92. doi: 10.1002/1096-9926(200012)62:6<385::AID-TERA5>3.0.CO;2-Z. [DOI] [PubMed] [Google Scholar]
- 68.Pradat P, Robert-Gnansia E, Di Tanna GL, Rosano A, Lisi A, Mastroiacovo P. First trimester exposure to corticosteroids and oral clefts. Birth Defects Res A Clin Mol Teratol. 2003;67:968–70. doi: 10.1002/bdra.10134. [DOI] [PubMed] [Google Scholar]
- 69.Carmichael SL, Shaw GM, Ma C, Werler MM, Rasmussen SA, Lammer EJ. Maternal corticosteroid use and orofacial clefts. Am J Obstet Gynecol. 2007;197(585):e1–7. doi: 10.1016/j.ajog.2007.05.046. discussion 683-4. [DOI] [PubMed] [Google Scholar]
- 70.Gorlin R, Cohen M, Levin S. Syndromes of the Head and Neck. Oxford: Oxford University Press; 1990. [Google Scholar]
- 71.Saxen I, Saxen L. Association between maternal intake of diazepam and oral clefts. Lancet. 1975;2:498. doi: 10.1016/s0140-6736(75)90567-x. [DOI] [PubMed] [Google Scholar]
- 72.Safra MJ, Oakley GP., Jr Association between cleft lip with or without cleft palate and prenatal exposure to diazepam. Lancet. 1975;2:478–80. doi: 10.1016/s0140-6736(75)90548-6. [DOI] [PubMed] [Google Scholar]
- 73.Czeizel A. Lack of evidence of teratogenicity of benzodiazepine drugs in Hungary. Reprod Toxicol. 1988;1:183–8. doi: 10.1016/s0890-6238(87)80031-x. [DOI] [PubMed] [Google Scholar]
- 74.Durner M, Greenberg DA, Delgado-Escueta AV. Is there a genetic relationship between epilepsy and birth defects? Neurology. 1992;42(4 Suppl 5):63–7. [PubMed] [Google Scholar]
- 75.Chang CC, Tsai F, Yang CC. Prenatal Diagnosis of Apert's Syndrome. Prenat Diag. 1998;18:621–5. [PubMed] [Google Scholar]
- 76.Wilkie AO, Slaney SF, Oldridge M, Poole MD, Ashworth GJ, Hockley AD, et al. Aperts syndrome results from localized mutations of FGFR2 and is allelic with Crouzon syndrome. Nat Genet. 1995;9:165–72. doi: 10.1038/ng0295-165. [DOI] [PubMed] [Google Scholar]
- 77.Slaney SF, Oldridge M, Hurst JA, Moriss-Kay GM, Hall CM, Poole MD, et al. Differential effects of FGFR2 mutations on syndactyly and cleft palate in Apert syndrome. Am J Hum Genet. 1996;58:923–32. [PMC free article] [PubMed] [Google Scholar]
- 78.Muenke M, Gripp KW, McDonald-McGinn DM, Gaudenz K, Whitaker LA, Bartlett SP, et al. A unique point mutation in the fibroblast growth factor receptor 3 gene (FGFR3) defines a new craniosynostosis syndrome. Am J Hum Genet. 1997;60:555–64. [PMC free article] [PubMed] [Google Scholar]
- 79.Reardon W, Wilkes D, Rutland P, Pulleyn LJ, Malcolm S, Dean JC, et al. Craniosynostosis associated with FGFR3 pro250arg mutation results in a range of clinical presentations including unisutural sporadic craniosynostosis. J Med Genet. 1997;34:632–6. doi: 10.1136/jmg.34.8.632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Rollnick BR. Germinal mosaicism in Crouzon syndrome. Clin Genet. 1988;33:145–50. doi: 10.1111/j.1399-0004.1988.tb03429.x. [DOI] [PubMed] [Google Scholar]
- 81.Kreiborg S, Cohen MM., Jr Germinal mosaicism in Crouzon syndrome. Hum Genet. 1990;84:487–8. doi: 10.1007/BF00195827. [DOI] [PubMed] [Google Scholar]
- 82.Keegan CE, Mulliken JB, Wu BL, Korf BR. Townes-Brocks syndrome versus expanded spectrum hemifacial microsomia: Review of eight patients and further evidence of a “hot spot” for mutation in the SALL1 gene. Genet Med. 2001;3:310–3. doi: 10.1097/00125817-200107000-00007. [DOI] [PubMed] [Google Scholar]
- 83.Kelberman D, Tyson J, Chandler DC, McInerney AM, Slee J, Albert D, et al. Hemifacial microsomia: Progress in understanding the genetic basis of a complex malformation syndrome. Hum Genet. 2001;109:638–45. doi: 10.1007/s00439-001-0626-x. [DOI] [PubMed] [Google Scholar]
- 84.Galvin BD, Hart KC, Meyer AN, Webster MK, Donoghue DJ. Constitutive receptor activation by Crouzon syndrome mutations in fibroblast growth factor receptor (FGFR) 2 and FGFR2/Neu chimeras. Proc Natl Acad Sci U S A. 1996;93:7894–9. doi: 10.1073/pnas.93.15.7894. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Preston RA, Post JC, Keats BJ, Aston CE, Ferrell RE, Priest J, et al. A gene for Crouzon craniofacial dysostosis maps to the long arm of chromosome 10. Nat Genet. 1994;7:149–53. doi: 10.1038/ng0694-149. [DOI] [PubMed] [Google Scholar]
- 86.Burck U. Genetic aspects of hemifacial microsomia. Hum Genet. 1983;64:291–6. doi: 10.1007/BF00279415. [DOI] [PubMed] [Google Scholar]
- 87.Kelberman D, Tyson J, Chandler DC, McInerney AM, Slee J, Albert D, et al. Hemifacial Microsomia progress in understanding the genetic basis of a complex malformation syndrome. Hum Genet. 2001;109:638–45. doi: 10.1007/s00439-001-0626-x. [DOI] [PubMed] [Google Scholar]
- 88.Thomas P. Goldenhar syndrome and Hemifacial microsomia: Observation on three patients. Europ J Pediat. 1980;133:287–92. doi: 10.1007/BF00496092. [DOI] [PubMed] [Google Scholar]
- 89.Wilson GN. Cranial defects in the Goldenhar syndrome. Am J Med Genet. 1983;14:435–43. doi: 10.1002/ajmg.1320140306. [DOI] [PubMed] [Google Scholar]
- 90.Houdayer C, Portnoï MF, Vialard F, Soupre V, Crumière C, Taillemite JL, et al. Pierre Robin sequence and interstitial deletion 2q32.3.q33.2. Am J Med Genet. 2001;102:219–26. doi: 10.1002/ajmg.1448. [DOI] [PubMed] [Google Scholar]
- 91.Dixon MJ. Treacher Collins syndrome. J Med Genet. 1995;32:806–8. doi: 10.1136/jmg.32.10.806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Dixon MJ. Treacher Collins syndrome. Hum Mol Genet. 1996;5:1391–6. doi: 10.1093/hmg/5.supplement_1.1391. [DOI] [PubMed] [Google Scholar]
- 93.Edwards SJ, Gladwin AJ, Dixon MJ. The mutational spectrum in Treacher Collins syndrome reveals a predominance of mutations that create a premature-termination codon. Am J Hum Genet. 1997;60:515–24. [PMC free article] [PubMed] [Google Scholar]
- 94.Dixon MJ, Read AP, Donnai D, Colley A, Dixon J, Williamson R. The gene for Treacher Collins syndrome maps to the long arm of chromosome 5. Am J Hum Genet. 1991;49:17–22. [PMC free article] [PubMed] [Google Scholar]
- 95.Arn PH, Mankinen C, Jabs EW. Mild mandibulofacial dysostosis in a child with a deletion of 3p. Am J Med Genet. 1993;46:534–6. doi: 10.1002/ajmg.1320460515. [DOI] [PubMed] [Google Scholar]
- 96.Jabs EW, Coss CA, Hayflick SJ, Whitmore TE, Pauli RM, Kirkpatrick SJ, et al. Chromosomal deletion 4p15.32—p14 in a Treacher Collins syndrome patient: Exclusion of the disease locus from and mapping of anonymous DNA sequences to this region. Genomics. 1991;11:188–92. doi: 10.1016/0888-7543(91)90117-w. [DOI] [PubMed] [Google Scholar]
- 97.Marsh KL, Dixon J, Dixon MJ. Mutations in the Treacher Collins syndrome gene lead to mislocalization of the neucleolar protein treacle. Hum Mol Genet. 1998;7:1795–800. doi: 10.1093/hmg/7.11.1795. [DOI] [PubMed] [Google Scholar]


