Abstract
Objective. To examine the effects of yoga versus an educational film program on sleep, mood, perceived stress, and sympathetic activation in older women with RLS. Methods. Participants were drawn from a larger trial regarding the effects of yoga on cardiovascular disease risk profiles in overweight, sedentary postmenopausal women. Seventy-five women were randomized to receive either an 8-week yoga (n = 38) or educational film (n = 37) program. All 75 participants completed an RLS screening questionnaire. The 20 women who met all four diagnostic criteria for RLS (n = 10 yoga, 10 film group) comprised the population for this nested study. Main outcomes assessed pre- and post-treatment included: sleep (Pittsburgh Sleep Quality Index), stress (Perceived Stress Scale), mood (Profile of Mood States, State-Trait Anxiety Inventory), blood pressure, and heart rate. Results. The yoga group demonstrated significantly greater improvements than controls in multiple domains of sleep quality and mood, and significantly greater reductions in insomnia prevalence, anxiety, perceived stress, and blood pressure (all P's≤0.05). Adjusted intergroup effect sizes for psychosocial variables were large, ranging from 1.9 for state anxiety to 2.6 for sleep quality. Conclusions. These preliminary findings suggest yoga may offer an effective intervention for improving sleep, mood, perceived stress, and blood pressure in older women with RLS.
1. Introduction
Restless legs syndrome (RLS) is a distressing and potentially debilitating sleep disorder, affecting up to 29% of U.S. and European general adult populations, and an estimated average of 19.5% of primary care patients [1]. RLS is characterized by a compelling urge to move the legs, usually accompanied by uncomfortable sensations in the legs, that: begins or worsens during periods of inactivity, is worse during the evening and nighttime hours, and is partially or totally relieved by movement [2]. Prevalence increases with age, and RLS is approximately twice as common in women as in men [1]. RLS has been repeatedly associated with significant reductions in quality of life comparable to or worse than those reported in Parkinson's disease, diabetes, stroke, and other serious chronic disorders [3–7]. RLS has also been linked to substantial impairment in sleep, mood, and health and is associated with significant societal and economic burden [4, 5, 7].
While RLS is considered a neurological disorder, the etiology of RLS remains poorly understood [8–10]. Defects in dopamine function and iron metabolism have been considered key factors in the pathogenesis of RLS for decades [11–14], based largely on clinical observations [14–18], although evidence remains inconclusive [8, 15, 19, 20]. An emerging body of evidence supports a potential role for autonomic and metabolic dysfunction. Recent studies have linked RLS to cardiovascular disease (CVD), as well as to key components of the metabolic syndrome, including diabetes, obesity, hypertension, and dyslipidemia, conditions associated with both autonomic and metabolic dysregulation [21]. RLS is characterized by elevated nocturnal blood pressure and heart rate [22–24], increased nocturnal hypothalamic-pituitary-adrenal (HPA) axis activation [25], elevated sympathetic activation, and reduced parasympathetic tone [26, 27], suggesting that autonomic and HPA axis dysfunction may in part underlie the development and/or progression of RLS and could help explain the observed association of RLS to CVD and related disorders [21].
There is no cure for RLS. Existing treatments are aimed at symptom reduction and include dopaminergic agents, opioids, sedative hypnotics, anticonvulsants, and benzodiazepines. Unfortunately, these medications can have serious side effects. For example, common side effects of dopaminergic agents, considered the first-line pharmacologic treatment for RLS sufferers [4, 16, 28], include rebound and augmentation of symptoms, dyskinesia, nausea and vomiting, hypotension, impulse control disorders, dizziness, and insomnia or drowsiness [7, 29–31]; common side effects of other RLS medications include potential for dependence, confusion, blurred vision, coordination problems, and other adverse sequellae [7, 29, 30]. These effects can be particularly problematic in older populations [32, 33], who also suffer disproportionately from RLS [29, 34]. In addition, the benefits of these medications may diminish over time [35, 36], leaving patients with few treatment options.
Given the substantial drawbacks of these pharmacologic treatments, investigation of safe, nonpharmacologic therapies that address apparent underlying risk factors is needed. Yet research remains very sparse. For example, there have to date been only three small trials examining the potential benefits of lifestyle or behavioral interventions for individuals suffering from RLS. These include two studies evaluating the effects of a 12–16 week exercise program versus usual care on RLS symptoms [37, 38], and a recent pre-post trial assessing the effects of cognitive behavioral therapy (CBT) in adults with primary RLS and mild-moderate psychosocial impairment [39]. Investigators reported significant improvements in RLS-related outcomes relative to the control group [37, 38] or baseline [39], suggesting that nonpharmacologic interventions may benefit those suffering from RLS.
Yoga, an ancient mind-body discipline that is increasingly popular in the U.S. [40], may represent a particularly promising nonpharmacologic therapy for RLS. Accumulating evidence from controlled trials suggests yoga can reduce blood pressure [41], improve glucose tolerance [41–43], lipid profiles [41, 44, 45], body composition [41, 45], and autonomic function [42, 44, 45], enhance mood [46–49], and improve sleep [48, 50, 51], factors linked to both RLS and CVD risk [8, 9, 16, 21]. In addition, studies suggest yoga can decrease muscular excitability and induce more rapid muscle relaxation [52], factors that have also been implicated in RLS [53, 54]. However, while yoga and other relaxation therapies are often recommended for RLS patients [55, 56], clinical trials are lacking. In this small, nested RCT, we investigated the effects of yoga on sleep, mood, stress, and associated outcomes in older women with RLS.
2. Methods
Participants for this study were drawn from a feasibility study regarding the effects of yoga on CVD risk profiles in sedentary, overweight postmenopausal women [57]. In this larger RCT, 75 women aged 45–79 years were recruited from the community using a combination of flyers, brochures, and newspaper advertisements. Eligible participants were nonsmoking women at least 45 years of age who were postmenopausal (≥12 months amenorrheic), physically inactive (exercising less than 20 minutes, 3 times per week), and overweight (body mass index (BMI, calculated as kg/m2) ≥25, and/or waist circumference ≥88 cm) or had a first-degree relative with diabetes or essential hypertension. Excluded were women who had practiced yoga within the last year, had uncontrolled hypertension, had been diagnosed with sleep apnea or with diabetes, cancer, heart failure, or other serious chronic disorders, or had any orthopedic, neurological, or other condition that might prevent them from safely completing an 8-week yoga program. Following enrollment, screening, and baseline assessment, eligible participants were randomized, using a computer-generated randomization list provided by a statistician not associated with the study, to receive either a gentle 8-week yoga program (n = 38) or an 8-week educational film program (n = 37). Each participant was administered her treatment assignment sequentially in order of enrollment, via coded opaque envelopes containing general study instructional materials, a welcome letter, and information pertinent to the yoga or educational film program. The study was approved by the University of Virginia Health Sciences Research Institutional Review Board, and all participants provided informed consent prior to study enrollment.
2.1. RLS and Outcome Assessment
Participants completed an RLS screening questionnaire at baseline. The questionnaire was adapted by the authors from the Athens Sleep Center Screening Questionnaire for RLS (http://www.athenssleepcenter.com/PDF/AScreeningQuestionaireRLS.pdf) to incorporate the established four criteria for RLS established by the International Restless Legs Syndrome Study Group (IRLSSG) [2]. Participants were asked if they ever experienced an urge to move with uncomfortable/funny (e.g., tingling, creeping, crawling) sensations in the legs, and if these feelings began or worsened when lying or sitting, were worse in the evening/night, and were relieved at least in part by movement (e.g., wiggling feet, toes, or walking). The questionnaire also included an item regarding frequency of symptoms (never, occasionally (<1x/month), sometimes (1–3x/month), frequently (1-2x/week to daily), or only in the past). Those participants endorsing all 4 diagnostic criteria and reporting symptoms at least once per month (N = 20) were considered to meet diagnostic criteria for RLS and were included in the present study.
Participants underwent a comprehensive assessment at baseline and following the 8-week intervention period. All assessments were conducted by experienced General Clinical Research Center and university clinical laboratory staff blinded to participant treatment assignment. Detailed baseline information was gathered on medical history, demographic characteristics, and lifestyle factors. Primary outcomes for this substudy included well-validated self-report measures of sleep (Pittsburgh Sleep Quality Index (PSQI)) [58], stress (Perceived Stress Scale (PSS)) [59], mood (Profile of Mood States (POMS)) [60], and anxiety (State-Trait Anxiety Inventory (STAI)) [61], as well as indices of sympathetic activation (blood pressure, heart rate). Clinical insomnia was defined as a score of greater than 5 on the PSQI [58, 62]. Blood pressure and heart rate were measured in a supine position following a 5-minute rest period; measurements were taken 3 times and averaged for a final score.
Additional outcomes included indices of abdominal adiposity (waist circumference (cm) and BMI (kg/m2)). At baseline, all women were screened for prediabetes (fasting glucose 100–125 mg/dL)/diabetes (fasting glucose ≥126 mg/dL), and serum levels of ferritin were measured. Blood samples were collected in the morning following an overnight fast and drawn by a trained phlebotomist using Vacutainer tubes. Blood samples (ferritin) were stored at −70°C until assay. Glucose was assessed using a Beckman glucose analyzer. Ferritin levels were measured using the ARCHITECT ferritin assay, a Chemiluminescent Microparticle Immunoassay (CMIA) for the quantitative determination of ferritin in human serum and plasma.
To assess the possible influence of physical activity and social support on change in outcomes over time, factors implicated in RLS [63] and strongly linked to both sleep and mood [64], participants completed the Physical Activity Scale for the Elderly (PASE) [65] and the Duke Social Support Index (abbreviated form [66]) pre- and posttreatment. To measure expectations of benefit, a brief treatment expectancy questionnaire was also administered to all participants. In addition, all subjects were asked to complete a short, anonymous exit questionnaire regarding their experience with the study.
2.2. Intervention
Each group (yoga and film intervention) attended a 90-minute class twice weekly for 8 weeks. Classes for the two programs were scheduled at the same times and in similar settings. Class size in both groups was limited to no more than 14 participants. Upon completing the study, all participants were given $150 for their time and travel expenses. Film group participants also received the yoga home practice materials, as well as coupons to attend local Iyengar yoga classes. Similarly, yoga group participants were also offered the opportunity to view the educational films following completion of the final assessment.
2.2.1. Yoga Intervention
Participants randomized to the yoga program completed a gentle Iyengar yoga program specifically designed for older, sedentary adults. In addition to attending classes, participants were asked to complete at least 30 minutes of home practice on nonclass days, with the aid of a DVD and a booklet illustrating the yoga home practice routines. Designed and taught by a senior Iyengar yoga instructor with over 30 years of experience, the yoga program included the following 23 active and restorative poses (asanas): Mountain (Tadasana and Urdhva hastasana in Tadasana); Standing wide apart legs (Prasarita padottanasana); Warrior I and II (Virabhadrasana I and II); Fierce or chair pose (Utkatasana); Extended hands and feet pose (Utthita hasta padasana); 1/2 forward bend (Ardha uttanasana); Triangle (Utthita trikonasana); Reverse triangle (Parivrtta trikonasana); Downward facing dog (Adho mukha svanasana); Marichi's pose (Marichyasana I and III, Utthita marichyasana); Seated twist in chair (Bharadvajasana); One leg straight forward spinal stretch (Janu sirsasana); Seated wide angle (Upavista konasana and Parsva upavista konasana); Seated bound angle (Baddha konasana); Extended legs up the wall (Urdhva prasarita padasana); Lying down holding big toe (Supta padangusthasana); Turned around belly (Jathara parivartanasana); Supported boat (Navasana); Supported bridge (Setu bandha sarvangasana); Crossed legs back arch (Supta swastikasana); Lying down bound angle (Supta baddha konasana); Reclined mountain (Supta tadasana); and Corpse pose (Savasana). Poses were modified and props (blankets, chairs, and straps) used as needed to allow participants to perform the sequences easily and safely. Each session began with a simple yogic centering and breathing exercise and ended with a 10–15 minute guided supine relaxation practice (Savasana).
2.2.2. Educational Film (Control) Intervention
This standardized educational film program, described in detail elsewhere [57], was designed to be easily replicable and to ensure comparability of staff attention, class time, and social interaction. Each class began with a brief meet and greet period, followed by viewing of an educational film chosen for its relevance and interest to our study population, then concluded with a 10–15 minute group discussion facilitated by a health professional with expertise in complementary and alternative therapies and women's health. To increase credibility and reduce participant bias, the educational film program was presented to potential participants as an informative, engaging, and relaxing alternative to the yoga classes.
2.3. Adherence and Adverse Events
Attendance at both the yoga and the film classes was recorded by the respective instructors. Participants in the yoga class also completed a check sheet and log after each home practice session, indicating the number of minutes practiced and any comments they might have regarding the session. Homework logs were turned in to the instructor at the first group class each week.
Adverse events were tracked via weekly review of participant yoga logs. At the beginning of each class, the yoga instructor also queried participants regarding potential problems; these were likewise recorded. In addition, participants were encouraged to contact study investigators and/or staff regarding any potential concerns.
2.4. Statistical Analysis
Data were analyzed using PASW v. 18. Differences between those who did versus did not meet criteria for RLS at baseline, and between yoga and control group participants at baseline were evaluated using chi-square (for categorical variables), student independent samples t tests (for continuous variables with a normal distribution), or Mann-Whitney U tests (for ordinal variables or continuous variables with evidence of skewing). Within group changes over time (pre- to postintervention) were evaluated using chi-square or McNemar test (categorical variables), paired t tests (continuous variables), or Wilcoxon signed rank test (ordinal or continuous variables with evidence of skewing). Between-group differences over time were assessed using Repeated Measures ANOVA (multivariate tests). Distributions of all dependent variables were examined to ensure the assumptions of normality and sphericity were met and variables transformed as necessary. Between-group differences over time in categorical variables were assessed using logistic regression. Effect sizes were calculated using Cohen's d [67], with between-group effect size adjusted for differences in baseline values.
3. Results
Twenty (27%) of the 75 women enrolled in the parent trial met the IRLSSG four essential diagnostic criteria for RLS, with symptoms at least once per month (n = 10 yoga group, 10 film group participants). Only 2 (10%) of the 20 reported having received an RLS diagnosis; neither were taking RLS medications. Of those with RLS, 17 (8 yoga, 9 control) experienced symptoms at least once/week. Baseline characteristics of the participants with versus without RLS are given in Table 1. Relative to those without RLS, women with RLS demonstrated significantly poorer sleep quality, greater prevalence of insomnia (85% versus 38% for those with versus without RLS, P = 0.0002), shorter sleep duration (6.2 ± 0.3 versus 7.1 ± 0.2 hours, P = 0.002), and higher diastolic and systolic blood pressure (P < 0.005) and were more likely to report a history of depression (P < 0.01). Participants with RLS were less likely to specify a history of hormone replacement therapy (P = 0.03) and indicated a significantly higher number of pregnancies than those without RLS (X = 2.9 ± 0.5 versus 1.8 ± 0.2, resp., P = 0.02). Those with RLS also tended to report higher trait anxiety, greater mood impairment, and lower vigor (P < 0.1). Women with RLS did not differ from those without RLS in baseline ferritin levels (81 ± 10.5 versus 84.7 ± 8.4 ng/mL, resp., P = 0.8) or in the prevalence of low ferritin levels (< 50 ng/mL, 30% versus 36%, resp., P = 0.6).
Table 1.
Baseline characteristics of participants with (N = 20) versus without (N = 55) symptoms of restless legs syndrome (RLS).
| Restless Legs Syndrome | |||||
|---|---|---|---|---|---|
| No | Yes | ||||
| Frequency/Mean | Percent/SE | Frequency/Mean | Percent/SE | P | |
| Demographic and lifestyle characteristics | |||||
| Age in years (Mean, SE) | 58.78 | 0.90 | 58.65 | 1.70 | NS |
| Race/ethnicity | NS | ||||
| Non-Hispanic White | 45 | 81.82% | 15 | 75.00% | |
| Minority | 10 | 18.18% | 5 | 25.00% | |
| Education | NS | ||||
| <4 years college | 13 | 23.64% | 7 | 35.00% | |
| ≥4 years college | 42 | 76.36% | 13 | 65.00% | |
| Employed | 39 | 70.91% | 13 | 65.00% | NS |
| Married/Cohabiting | 27 | 49.09% | 7 | 35.00% | NS |
| Mean daily intake of the following: | |||||
| Caffeine, mg (Mean, SE) | 148.89 | 24.86 | 156.47 | 31.49 | NS |
| Alcohol, g (Mean, SE) | 8.45 | 2.93 | 20.13 | 11.14 | NS |
| Health and reproductive history | |||||
| Reported history of: | |||||
| High blood pressure | 14 | 25.45% | 9 | 45.00% | 0.10 |
| Depression | 10 | 18.18% | 10 | 50.00% | 0.008 |
| Anxiety | 8 | 14.55% | 5 | 25.00% | NS |
| Hormone replacement therapy | 11 | 20.00% | 0 | 0.00% | 0.03 |
| Never pregnant | 14 | 25.45% | 2 | 10.00% | NS |
| Number of pregnancies | 1.82 | 0.20 | 2.90 | 0.55 | 0.02 |
| Sleep and psychosocial profiles | |||||
| Sleep Quality (PSQI) | |||||
| Sleep quality-Global | 5.39 | 0.51 | 8.33 | 0.75 | 0.003 |
| Sleep quality | 0.61 | 0.15 | 1.30 | 0.29 | 0.03 |
| Sleep latency | 0.92 | 0.14 | 1.05 | 0.26 | NS |
| Sleep duration | 0.65 | 0.09 | 1.35 | 0.20 | 0.0005 |
| Sleep efficiency | 0.40 | 0.11 | 1.00 | 0.26 | 0.02 |
| Sleep disturbance | 1.24 | 0.07 | 1.67 | 0.11 | 0.003 |
| Sleep medication use | 0.22 | 0.06 | 0.55 | 0.21 | 0.04 |
| Daytime dysfunction | 1.29 | 0.10 | 1.65 | 0.15 | 0.06 |
| Insomnia (PSQI > 5) (N, %) | 21 | 38.18% | 17 | 85.00% | 0.0002 |
| Average sleep duration in hours (Mean, SE) | 7.10 | 0.15 | 6.18 | 0.25 | 0.002 |
| Anxiety (STAI) | |||||
| Trait | 34.65 | 1.29 | 38.95 | 1.94 | 0.08 |
| State | 30.35 | 1.18 | 32.74 | 2.45 | NS |
| Mood (POMS) | |||||
| Total | 8.96 | 4.26 | 23.89 | 9.47 | 0.09 |
| Tension Anxiety | 3.19 | 0.74 | 4.80 | 1.44 | NS |
| Depression | 7.09 | 1.10 | 11.50 | 2.82 | 0.08 |
| Anger/hostility | 5.27 | 0.70 | 8.26 | 2.47 | NS |
| Vigor | 16.87 | 0.93 | 13.55 | 1.30 | 0.06 |
| Fatigue | 8.28 | 0.90 | 10.35 | 1.45 | NS |
| Confusion | 1.76 | 0.60 | 2.80 | 1.17 | NS |
| Perceived stress (PSS) | 19.60 | 1.01 | 20.95 | 2.16 | NS |
| Social support (DSSI) | |||||
| Social interaction | 8.75 | 0.53 | 10.05 | 0.72 | NS |
| Social support | 18.34 | 0.38 | 17.79 | 0.75 | NS |
| Blood Pressure | |||||
| Systolic (mmHg) | 122.76 | 2.26 | 141.85 | 4.71 | 0.0001 |
| Diastolic (mmHg) | 71.35 | 1.22 | 78.75 | 2.57 | 0.005 |
| Heart rate | 64.82 | 1.28 | 66.65 | 2.62 | NS |
| Anthropometrics | |||||
| Waist girth (cm) | 103.83 | 2.20 | 108.46 | 2.97 | NS |
| Hip girth (cm) | 110.26 | 1.51 | 113.58 | 1.43 | NS |
| Body mass index (kg/m2) | 31.56 | 0.96 | 33.31 | 1.29 | NS |
| Prediabetic (fasting glucose 100–125 mg/dL) | 21 | 38.18% | 10 | 50.00% | NS |
| Serum ferritin levels (ng/mL)(Mean, SE) | 84.72 | 8.43 | 81.00 | 10.50 | NS |
| Low ferritin level (<50 ng/mL) | 20 | 36.36% | 6 | 30.00% | NS |
Abbreviations. DSSI: Duke Social Support Index.
NS: nonsignificant (P > 0.1).
POMS: Profile of Mood States.
PSQI: Pittsburgh Sleep Quality Index.
PSS: Perceived Stress Scale.
SE: standard error of the mean.
STAI: State-Trait Anxiety Inventory.
Of those 20 participants screening positive for RLS, 5 (25%) were African American, 65% had completed at least 4 years of college, 65% were employed at least part time, 35% were married, and 50% were pre-diabetic (fasting glucose 100–125 mg/dL). Participant age averaged 58.8 ± 0.9 years. As indicated in Table 2, treatment and control groups did not differ in demographic characteristics, or in baseline lifestyle factors, anthropometric characteristics, medical history, health profiles, prevalence of insomnia, or reported frequency of RLS symptoms. Mood and sleep profiles were also similar between the groups (P > 0.3, data not shown). Eighteen of the 20 participants with RLS completed the final assessment (8 yoga, 10 controls). Those leaving the study (one non-Hispanic white, one African American) dropped out during the first 2-3 weeks due to health reasons unrelated to the yoga program. Adherence in both the yoga and the educational film group was very good overall. Class attendance in the two groups was similar (mean attendance = 13.1 ± 1.4 versus 13.6 ± 0.8 classes (of 16 total classes) for the yoga versus film group participants, respectively, P = 0.75). Yoga group participants completed homework practice a mean of 4.1 ± 0.2 days/week, with an average 28.0 ± 3.3 minutes/practice session. Participant feedback on open-ended exit questionnaires was also positive, with participants of both groups expressing enthusiasm for their respective programs [57]. Of the 8 yoga group participants completing the study, all cited high satisfaction with the yoga program and all reported multiple benefits on their yoga logs and/or exit questionnaires, including increased strength, flexibility and mobility (N = 6), reduced pain (N = 3), enhanced energy and well-being (N = 6), increased feelings of peace, tranquility, and relaxation (N = 8), and greater body awareness (N = 4). While three yoga group participants indicated some mild, temporary muscle soreness in the first few weeks, no participants reported significant pain, discomfort or other adverse events in association with the yoga program.
Table 2.
Baseline characteristics of participants with restless legs syndrome (RLS) assigned to the yoga (N = 10) versus the educational film (control) group (N = 10).
| Treatment Group | |||||
|---|---|---|---|---|---|
| Yoga | Educational Film (control) | ||||
| Frequency/Mean | Percent/SE | Frequency/Mean | Percent/SE | P | |
| Demographic and lifestyle characteristics | |||||
| Age in years (Mean, SE) | 58.40 | 2.00 | 58.90 | 2.88 | NS |
| Race/ethnicity | NS | ||||
| Non-Hispanic White | 8 | 80.00% | 7 | 70.00% | |
| African American | 2 | 20.00% | 3 | 30.00% | |
| Education | NS | ||||
| <4 years college | 3 | 30.00% | 4 | 40.00% | |
| ≥4 years college | 7 | 70.00% | 6 | 60.00% | |
| Employed | 7 | 70.00% | 6 | 60.00% | NS |
| Married/Cohabiting | 4 | 40.00% | 3 | 30.00% | NS |
| Mean daily intake of the following: | |||||
| Caffeine (mg) | 162.68 | 49.93 | 147.77 | 35.74 | NS |
| Alcohol (g) | 19.57 | 15.91 | 20.42 | 16.38 | NS |
| Health history | |||||
| Reported history of: | |||||
| High blood pressure | 4 | 40.00% | 5 | 50.00% | NS |
| Depression | 5 | 50.00% | 5 | 50.00% | NS |
| Anxiety | 2 | 20.00% | 3 | 30.00% | NS |
| Prediabetic (fasting glucose 100–125 mg/dL) | 5 | 50.00% | 5 | 50.00% | NS |
| Serum ferritin levels (ng/mL) | 81.40 | 15.35 | 80.56 | 15.32 | NS |
| RLS symptoms | NS | ||||
| 1–3x/month | 2 | 20.00% | 1 | 10.00% | |
| At least 1x/week | 8 | 80.00% | 9 | 90.00% | |
| Obese (body mass index ≥30) | 6 | 60.00% | 5 | 50.00% | NS |
Abbreviations. NS: nonsignificant (P > 0.5).
As illustrated in Table 3, yoga group participants showed significant reduction over time in prevalence of insomnia (P = 0.01) and significant improvement in sleep quality, both overall (P = 0.001) and in the domains of sleep duration (P = 0.02), efficiency (P = 0.01), disturbance (P = 0.03), and daytime dysfunction (P = 0.002). Reported average sleep duration increased from 5.7 ± 0.5 to 7.3 ± 0.5 hours (P = 0.001). Yoga participants also demonstrated significant, or marginally significant improvements in all but one domain of mood (P ≤ 0.08), as well as significant reductions in state anxiety, perceived stress, and both systolic and diastolic blood pressure (P < 0.05).
Table 3.
Change over time in psychosocial and physiological profiles in sedentary, overweight postmenopausal women with RLS (N = 8 yoga, 10 controls).
| Yoga | Educational film (Control) | Between-group difference over time | ||||||
|---|---|---|---|---|---|---|---|---|
| Pre | Post | P | Pre | Post | P | P | Effect size¥ | |
| (Mean ± SE) | (Mean ± SE) | (Mean ± SE) | (Mean ± SE) | |||||
| Sleep quality, stress, and mood | ||||||||
| Pittsburgh Sleep Quality Index (PSQI) | ||||||||
| Global | 8.71 ± 1.15 | 3.57 ± 0.53 | 0.001 | 9.25 ± 1.05 | 8.00 ± 0.93 | NS | 0.01 | 2.59 |
| Sleep latency | 0.88 ± 0.40 | 0.88 ± 0.35 | NS | 1.25 ± 0.41 | 1.50 ± 0.38 | NS | NS | 0.25 |
| Sleep quality | 1.38 ± 0.50 | 0.75 ± 0.41 | NS | 1.88 ± 0.40 | 1.38 ± 0.50 | 0.04 | NS | 0.11 |
| Sleep duration | 1.50 ± 0.38 | 0.50 ± 0.27 | 0.02 | 1.40 ± 0.40 | 1.30 ± 0.0.34 | NS | 0.04 | 1.18 |
| Sleep efficiency | 1.75 ± 0.41 | 0.63 ± 0.38 | 0.01 | 0.75 ± 0.37 | 0.38 ± 0.26 | 0.08 | 0.03 | 0.70 |
| Sleep disturbance | 1.71 ± 0.18 | 1.14 ± 0.14 | 0.03 | 1.75 ± 0.16 | 1.75 ± 0.25 | NS | 0.07 | 1.44 |
| Sleep medication | 0.13 ± 0.13 | 0.00 ± 0.00 | NS | 0.88 ± 0.35 | 0.63 ± 0.38 | NS | NS | −0.33 |
| Daytime dysfunction | 2.00 ± 0.27 | 0.88 ± 0.13 | 0.002 | 1.50 ± 0.17 | 1.35 ± 0.21 | NS | 0.01 | 2.64 |
| Average sleep duration in hours | 5.72 ± 0.45 | 7.33 ± 0.53 | 0.001 | 6.40 ± 0.32 | 6.28 ± 0.30 | NS | 0.0001 | −1.35 |
| Prevalence of insomnia (PSQI > 5) (%) | 87.50% | 12.50% | 0.01 | 100.00% | 70.00% | NS | 0.03 | — |
| Perceived Stress Scale | 24.00 ± 1.88 | 14.71 ± 2.75 | 0.006 | 18.44 ± 1.47 | 19.67 ± 1.39 | NS | 0.03 | 1.98 |
| Profile of Mood States | ||||||||
| Total | 24.00 ± 4.11 | −12.50 ± 7.06 | 0.02 | 18.60 ± 2.71 | 24.11 ± 8.96 | NS | 0.02 | 2.35 |
| Tension/Anxiety | 5.75 ± 1.28 | 0.88 ± 1.69 | 0.07 | 4.22 ± 0.53 | 5.78 ± 1.55 | NS | 0.05 | 1.78 |
| Confusion | 3.43 ± 2.28 | 0.00 ± 0.49 | NS | 1.50 ± 1.45 | 2.00 ± 1.67 | NS | 0.09 | 2.84 |
| Depression | 13.25 ± 0.73 | 2.88 ± 1.23 | 0.001 | 11.22 ± 1.03 | 11.11 ± 1.87 | NS | 0.06 | 4.97 |
| Anger/Hostility | 5.14 ± 0.64 | 2.29 ± 0.67 | 0.02 | 7.33 ± 0.78 | 9.78 ± 1.30 | 0.06 | 0.06 | 2.93 |
| Vigor | 12.50 ± 1.08 | 19.88 ± 2.41 | 0.015 | 16.33 ± 0.91 | 15.67 ± 0.98 | NS | 0.02 | −2.63 |
| Fatigue | 13.29 ± 1.95 | 7.43 ± 2.95 | 0.08 | 8.22 ± 1.20 | 9.33 ± 1.51 | NS | 0.05 | 1.26 |
| State-Trait Anxiety Inventory | ||||||||
| State | 33.29 ± 2.59 | 26.14 ± 2.22 | 0.05 | 28.13 ± 2.44 | 32.75 ± 3.37 | 0.05 | 0.002 | 1.87 |
| Trait | 39.71 ± 3.90 | 33.43 ± 4.02 | NS | 36.38 ± 2.77 | 34.88 ± 3.53 | NS | NS | 0.43 |
| Duke Social Support Index | ||||||||
| Social Interaction | 10.00 ± 1.33 | 10.00 ± 1.02 | NS | 10.75 ± 1.13 | 11.00 ± 0.89 | NS | NS | NA |
| Social Support | 17.17 ± 1.19 | 19.50 ± 0.43 | NS | 18.38 ± 0.71 | 18.13 ± 0.69 | NS | NS | NA |
| Heart rate and blood pressure | ||||||||
| Average heart rate (supine) | 68.13 ± 3.48 | 65.00 ± 3.64 | NS | 66.80 ± 4.56 | 64.60 ± 3.42 | NS | NS | 0.09 |
| Systolic blood pressure | 145.75 ± 9.80 | 125.50 ± 3.24 | 0.04 | 139.93 ± 6.44 | 131.13 ± 4.51 | NS | 0.05 | 1.25 |
| Diastolic blood pressure | 83.13 ± 4.36 | 73.75 ± 3.68 | 0.02 | 74.40 ± 3.42 | 73.80 ± 2.59 | NS | 0.03 | 0.89 |
| Anthropometrics | ||||||||
| Waist (cm) | 108.95 ± 5.79 | 106.91 ± 4.78 | NS | 108.60 ± 4.63 | 110.68 ± 4.74 | NS | NS | 0.25 |
| Weight (kg) | 88.83 ± 4.33 | 87.67 ± 4.30 | NS | 83.56 ± 3.66 | 84.26 ± 4.12 | NS | NS | 0.15 |
| Body mass index (kg/m2) | 33.59 ± 2.13 | 32.96 ± 1.74 | NS | 32.27 ± 1.95 | 32.30 ± 2.15 | NS | NS | 0.11 |
¥Between-group effect size (Cohen's d), adjusted for differences in baseline values, NS: Non-significant (P > 0.10).
Despite limited study power, the yoga group demonstrated significantly greater improvement than controls in several domains of sleep quality, greater reductions in prevalence of insomnia, and greater increases in average sleep duration. Relative to controls, yoga group participants also showed significantly greater reductions in perceived stress, mood disturbance, state anxiety, and both systolic and diastolic blood pressure (all P's ≤0.05). Adjusted intergroup effect sizes for psychosocial variables were large, with those for summary scores ranging from 1.9 for state anxiety to 2.6 for sleep quality (Table 3); intergroup effect sizes for blood pressure were also substantial, calculated as 0.9 for diastolic blood pressure and 1.25 for systolic blood pressure. Intent to treat analysis, using the conservative last value carried forward method to address missing data, did not appreciably alter these findings. Neither treatment expectancy scores nor change in physical activity or social support differed significantly between the two groups; moreover, adjustment for these variables did not materially alter the results, suggesting that these factors did not explain the observed between-group differences.
4. Discussion
RLS is a common sleep and sensorimotor disorder associated with significant reductions in quality of life that are largely attributable to the substantial impairment in sleep and mood commonly accompanying RLS [4]. In light of the potentially serious side effects of existing pharmacological treatments for RLS, investigation of promising lifestyle and behavioral interventions is clearly warranted. To our knowledge, this is the first study to examine the effects of yoga in persons with RLS, and among the few trials to examine the potential benefits of any nonpharmacologic intervention for those suffering from this disorder. Findings of this preliminary RCT suggest that yoga can significantly improve sleep, enhance mood, reduce stress and anxiety, and decrease blood pressure in postmenopausal women with RLS, and thus may offer a promising new treatment modality for this population. Moreover, the overall excellent compliance, high participant satisfaction, and lack of adverse events observed in this study suggest that a gentle yoga program is both feasible and acceptable to older women with RLS.
Consistent with our findings, a nonrandomized controlled trial in 14 dialysis patients with RLS reported significant improvements in sleep and mood in those completing a 16-week aerobic exercise program, with adjusted intergroup effect sizes ranging from 0.75 to 1.00 [37]. Likewise, a pre-post study of 25 outpatients with psychosocial impairment due to RLS reported significant, although more modest improvements in sleep and mood following 8 weeks of CBT (effect sizes 0.1–0.8) [39], improvements that appeared attributable at least in part to mindfulness, breathing, and other stress-reduction exercises. Although no published studies have assessed the effects of yoga on blood pressure in RLS patients, a number of controlled studies have reported yoga interventions to reduce blood pressure in other both healthy and chronically ill populations [41, 49, 68–70].
While we did not assess the effects of yoga specifically on symptoms of RLS, change in sleep and mood are endpoints recommended for use in clinical trials by the IRLSSG [7] and have been used in trials regarding the efficacy of dopamine agonists and other pharmaceutical treatments for RLS [71–76]. Of particular note, the improvements in sleep quality and mood observed following our 8-week yoga program appear comparable to those reported in recent pharmaceutical trials that used similar measures in RLS patients [71, 72, 74, 76, 77], suggesting that yoga could possibly provide a viable alternative to pharmaceutical therapy for some patients. Given these promising preliminary findings, larger controlled trials are warranted to investigate the potential utility of yoga as an adjunct or primary treatment for RLS.
Only 10% of study participants screening positive for RLS had received a physician diagnosis, comparable to the low diagnostic rates generally reported in other, larger studies [78–80]. Consistent with previous research [81–83], participants with RLS reported higher parity and demonstrated significantly greater sleep deficits and mood disturbance than those without RLS, with 85% indicating insomnia at baseline and 50% reporting a history of depression. In agreement with several, but not all recent studies [21], RLS was associated with significantly higher blood pressure in this study. Participants with RLS were also less likely to report use of hormone replacement therapy (HRT) than those without RLS. Evidence from recent experimental studies in postmenopausal women suggest HRT may decrease complaints of restless legs [84], improve subjective sleep quality [85, 86], suppress muscle sympathetic nerve activity [87], and reduce nocturnal arousals [84], findings consistent with a possible protective effect of HRT for RLS. However, the relation between HRT and RLS remains unclear, with 2 epidemiological studies indicating positive, although nonsignificant, associations between RLS and HRT [88, 89], and a French study of 440 postmenopausal women with RLS reporting no relation of HRT use to symptom severity [90].
Although mechanisms underlying the improvements with yoga observed in this study remain speculative, yoga may benefit those with RLS via several possible interrelated pathways, illustrated in Figure 1. For example, by reducing the activation and reactivity of the sympathetic nervous system and the HPA axis, factors recently implicated in RLS etiology [9, 21, 25] and known to have strong, bidirectional relationships with sleep and mood [91, 92], yoga may attenuate RLS-associated pain and discomfort, reduce perceived stress and promote feelings of well-being, enhance sleep, lower muscle excitability, and foster positive downstream changes in metabolic status, neuroendocrine function, and inflammatory responses. Second, as illustrated in pathway 2, yoga may also alleviate the distressing symptoms of RLS by directly enhancing parasympathetic output, possibly via stimulation of the vagus nerve [93–95], and in this way, shift the autonomic nervous system balance from primarily sympathetic to parasympathetic [93, 95]. This, in turn, may enhance sleep and mood, reduce perceived pain, promote muscle relaxation, and lead to positive changes in cardiovagal function and related neuroendocrine, metabolic, and inflammatory responses.
Figure 1.
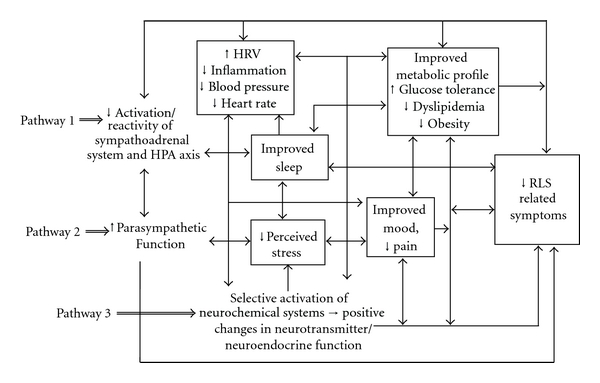
Possible pathways by which yoga may attenuate the distressing symptoms associated with RLS.
Third, findings of recent neuroimaging and neurophysiological studies [93, 96, 97] suggest that yogic practices may, by selectively activating specific neurochemical systems implicated in RLS, likewise promote beneficial changes in sympathetic/parasympathetic balance, in neuroendocrine function, in affect, sleep, and pain processing, and in related metabolic and inflammatory responses (pathway 3). For example, yogic practices have been shown to increase brain levels of dopamine [98], a neurotransmitter long implicated in the development of RLS and thought to play a key role in pain processing [99], sleep [100], motor control [101], and metabolic regulation [102, 103]. Yoga also increases GABA [97], an inhibitory neurotransmitter involved in the regulation of muscular excitability [104], mood [105], sleep [100], and pain processing [106]; the GABA agonist gabapentin, an anticonvulsant used in treating RLS [73, 77], as well as chronic pain, mood disorders, and insomnia [107–109], is thought to operate at least in part by increasing brain GABA [73, 77].
4.1. Strengths and Limitations
Strengths of this study include the community-based design, randomization of participants, between-group similarity in baseline characteristics, high participant retention and adherence, and a comparison condition designed to control for time, attention, and social interaction. Limitations of this pilot study are several. Sample sizes were small, reducing our power to detect between-group differences over time. However, despite limited power, we observed significant improvement in the yoga versus control group in several clinically important parameters, again arguing for a potentially powerful beneficial effect of the yoga program. Although the educational film program was designed to control for staff attention, setting, and class time, control group participants did not receive homework assignments. In addition, while assessors were blinded to participant treatment status, participants could not be masked. However, response to the educational film (control) program was enthusiastic, and both retention and compliance were excellent [57]. Treatment expectancies did not differ between-groups, and adjustment for treatment expectancies did not materially alter findings, suggesting that placebo effects did not explain the observed findings. Moreover, observed effect sizes were substantially larger than would be expected with placebo [110], and significantly greater than those observed in the controls.
The study population was restricted to sedentary, overweight, postmenopausal women, and findings may therefore not be generalizable to other populations. RLS diagnosis was based on self-report, and some degree of diagnostic error is thus likely. However, affirmative response to all 4 essential criteria renders inclusion of mimics less likely [111]. Finally, the parent study was not designed specifically to address effects of yoga practice on RLS, and we did not measure change in RLS symptoms per se. However, as indicated above, we did screen for RLS at baseline and assess change in sleep quality and mood, which are outcomes that have been recommended for inclusion in clinical trials of RLS [7] and often used as secondary endpoints in pharmaceutical trials of RLS patients [112–116]. Significant sleep and mood impairment have been repeatedly documented in studies of RLS [7, 117, 118]. Sleep loss is the most common presenting complaint of patients seeking medical care for RLS [118, 119] and is thought to explain, in large part, the negative effects of RLS on health and quality of life [80].
5. Conclusions
These preliminary findings suggest that yoga may offer a safe, beneficial intervention for reducing sleep and mood disturbance, perceived stress, anxiety, and blood pressure in older women with RLS. Larger controlled trials are needed to confirm these benefits in this and other adult populations with RLS, examine the effects of yoga practice specifically on RLS symptoms and symptom severity, and to evaluate potential underlying mechanisms.
Conflict of Interests
No competing interests or conflict of interest are declared by any of the author.
Acknowledgments
The authors would like to thank Dr. Ivora Hinton, Dr. Gina Alexander, and Research Assistants Sarah Cottingham, Sarah Hasan, and Sundas Idrees for their assistance with data collection. They are also grateful to Dr. Ann Taylor for essential logistical support, to Jewel Holmberg for technical assistance, and to Iyengar Yoga Master Sandra Pleasants, who was largely responsible for the design and implementation of the yoga program. This work was performed at the University of Virginia and West Virginia University and was supported by the National Center for Complementary and Alternative Medicine and the Office of Research on Women's Health (Grant nos. R21-AT002982 and 1-K01-AT004108 to K. E. Innes); and the National Center for Research Resources (Grant no. M01-RR00847). The contents are solely the responsibility of the authors and do not represent the official views of the University of Virginia, West Virginia University, or the National Institutes of Health.
References
- 1.Innes KE, Selfe TK, Agarwal P. Prevalence of restless legs syndrome in North American and Western European populations: a systematic review. Sleep Medicine. 2011;12(7):623–634. doi: 10.1016/j.sleep.2010.12.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Allen RP, Picchietti D, Hening WA, et al. Restless legs syndrome: diagnostic criteria, special considerations, and epidemiology. A report from the restless legs syndrome diagnosis and epidemiology workshop at the National Institutes of Health. Sleep Medicine. 2003;4(2):101–119. doi: 10.1016/s1389-9457(03)00010-8. [DOI] [PubMed] [Google Scholar]
- 3.Abetz L, Allen R, Follet A, et al. Evaluating the quality of life of patients with restless legs syndrome. Clinical Therapeutics. 2004;26(6):925–935. doi: 10.1016/s0149-2918(04)90136-1. [DOI] [PubMed] [Google Scholar]
- 4.Reese JP, Stiasny-Kolster K, Oertel WH, Dodel RC. Health-related quality of life and economic burden in patients with restless legs syndrome. Expert Review of Pharmacoeconomics and Outcomes Research. 2007;7(5):503–521. doi: 10.1586/14737167.7.5.503. [DOI] [PubMed] [Google Scholar]
- 5.Reinhold T, Mller-Riemenschneider F, Willich SN, Brggenjrgen B. Economic and human costs of restless legs syndrome. PharmacoEconomics. 2009;27(4):267–279. doi: 10.2165/00019053-200927040-00001. [DOI] [PubMed] [Google Scholar]
- 6.Happe S, Reese JP, Stiasny-Kolster K, et al. Assessing health-related quality of life in patients with restless legs syndrome. Sleep Medicine. 2009;10(3):295–305. doi: 10.1016/j.sleep.2008.01.002. [DOI] [PubMed] [Google Scholar]
- 7.Earley CJ, Silber MH. Restless legs syndrome: understanding its consequences and the need for better treatment. Sleep Medicine. 2010;11(9):807–815. doi: 10.1016/j.sleep.2010.07.007. [DOI] [PubMed] [Google Scholar]
- 8.Winkelman JW. Considering the causes of RLS. European Journal of Neurology. 2006;13(2):8–14. doi: 10.1111/j.1468-1331.2006.01586.x. [DOI] [PubMed] [Google Scholar]
- 9.Walters AS, Rye DB. Review of the relationship of restless legs syndrome and periodic limb movements in sleep to hypertension, heart disease, and stroke. Sleep. 2009;32(5):589–597. doi: 10.1093/sleep/32.5.589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Smith JE, Tolson JM. Recognition, diagnosis, and treatment of restless legs syndrome. Journal of the American Academy of Nurse Practitioners. 2008;20(8):396–401. doi: 10.1111/j.1745-7599.2008.00337.x. [DOI] [PubMed] [Google Scholar]
- 11.Matthews WB. Letter: iron deficiency and restless legs. British Medical Journal. 1976;1(6014):p. 898. doi: 10.1136/bmj.1.6014.898-a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Sandyk R. The restless legs syndrome (Ekbom’s syndrome) South African Medical Journal. 1983;63(18):701–702. [PubMed] [Google Scholar]
- 13.O’Keeffe ST. Restless legs syndrome: a review. Archives of Internal Medicine. 1996;156(3):243–248. [PubMed] [Google Scholar]
- 14.Allen R. Dopamine and iron in the pathophysiology of restless legs syndrome (RLS) Sleep Medicine. 2004;5(4):385–391. doi: 10.1016/j.sleep.2004.01.012. [DOI] [PubMed] [Google Scholar]
- 15.Trotti LM, Bhadriraju S, Rye DB. An update on the pathophysiology and genetics of restless legs syndrome. Current Neurology and Neuroscience Reports. 2008;8(4):281–287. doi: 10.1007/s11910-008-0044-8. [DOI] [PubMed] [Google Scholar]
- 16.Ekbom K, Ulfberg J. Restless legs syndrome. Journal of Internal Medicine. 2009;266(5):419–431. doi: 10.1111/j.1365-2796.2009.02159.x. [DOI] [PubMed] [Google Scholar]
- 17.Trenkwalder C, Högl B, Winkelmann J. Recent advances in the diagnosis, genetics and treatment of restless legs syndrome. Journal of Neurology. 2009;256(4):539–553. doi: 10.1007/s00415-009-0134-9. [DOI] [PubMed] [Google Scholar]
- 18.Trenkwalder C, Paulus W. Restless legs syndrome: pathophysiology, clinical presentation and management. Nature Reviews Neurology. 2010;6(6):337–346. doi: 10.1038/nrneurol.2010.55. [DOI] [PubMed] [Google Scholar]
- 19.Earley CJ, Allen RP, Connor JR, Ferrucci L, Troncoso J. The dopaminergic neurons of the A11 system in RLS autopsy brains appear normal. Sleep Medicine. 2009;10(10):1155–1157. doi: 10.1016/j.sleep.2009.01.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.McDonagh B, King T, Guptan RC. Restless legs syndrome in patients with chronic venous disorders: an untold story. Phlebology. 2007;22(4):156–163. doi: 10.1258/026835507781477145. [DOI] [PubMed] [Google Scholar]
- 21.Innes KE, Selfe TK, Agarwal P. Restless legs syndrome and conditions associated with metabolic dysregulation, sympathoadrenal dysfunction, and cardiovascular disease risk: a systematic review. Sleep Medicine Reviews. 2011;38(5):1–31. doi: 10.1016/j.smrv.2011.04.001. [DOI] [PubMed] [Google Scholar]
- 22.Ferri R, Zucconi M, Rundo F, Spruyt K, Manconi M, Ferini-Strambi L. Heart rate and spectral EEG changes accompanying periodic and non-periodic leg movements during sleep. Clinical Neurophysiology. 2007;118(2):438–448. doi: 10.1016/j.clinph.2006.10.007. [DOI] [PubMed] [Google Scholar]
- 23.Siddiqui F, Strus J, Ming X, Lee IA, Chokroverty S, Walters AS. Rise of blood pressure with periodic limb movements in sleep and wakefulness. Clinical Neurophysiology. 2007;118(9):1923–1930. doi: 10.1016/j.clinph.2007.05.006. [DOI] [PubMed] [Google Scholar]
- 24.Pennestri MH, Montplaisir J, Colombo R, Lavigne G, Lanfranchi PA. Nocturnal blood pressure changes in patients with restless legs syndrome. Neurology. 2007;68(15):1213–1218. doi: 10.1212/01.wnl.0000259036.89411.52. [DOI] [PubMed] [Google Scholar]
- 25.Schilling C, Schredl M, Strobl P, Deuschle M. Restless legs syndrome: evidence for nocturnal hypothalamic-pituitary- adrenal system activation. Movement Disorders. 2010;25(8):1047–1052. doi: 10.1002/mds.23026. [DOI] [PubMed] [Google Scholar]
- 26.Cikrikcioglu MA, Hursitoglu M, Erkal H, et al. Oxidative stress and autonomic nervous system functions in restless legs syndrome. European Journal of Clinical Investigation. 2011;41(7):734–742. doi: 10.1111/j.1365-2362.2010.02461.x. [DOI] [PubMed] [Google Scholar]
- 27.Ferrin-Strambi L, Poccia F, Oldani A, et al. Heart rate variability during wakefulness and sleep in restless legs. Syndrome Journal of Sleep Research. 2000;9, article 63 [Google Scholar]
- 28.Oertel WH, Trenkwalder C, Zucconi M, et al. State of the art in restless legs syndrome therapy: practice recommendations for treating restless legs syndrome. Movement Disorders. 2007;22(supplement 18):S466–S475. doi: 10.1002/mds.21545. [DOI] [PubMed] [Google Scholar]
- 29.Spiegelhalder K, Hornyak M. Restless legs syndrome in older adults. Clinics in Geriatric Medicine. 2008;24(1):167–180. doi: 10.1016/j.cger.2007.08.004. [DOI] [PubMed] [Google Scholar]
- 30.Trenkwalder C, Hening WA, Montagna P, et al. Treatment of restless legs syndrome: an evidence-based review and implications for clinical practice. Movement Disorders. 2008;23(16):2267–2302. doi: 10.1002/mds.22254. [DOI] [PubMed] [Google Scholar]
- 31.García-Borreguero D, Williams AM. Dopaminergic augmentation of restless legs syndrome. Sleep Medicine Reviews. 2010;14(5):339–346. doi: 10.1016/j.smrv.2009.11.006. [DOI] [PubMed] [Google Scholar]
- 32.Milligan SA, Chesson AL. Restless legs syndrome in the older adult: diagnosis and management. Drugs and Aging. 2002;19(10):741–751. doi: 10.2165/00002512-200219100-00003. [DOI] [PubMed] [Google Scholar]
- 33.Wolkove N, Elkholy O, Baltzan M, Palayew M. Sleep and aging: 2. Management of sleep disorders in older people. CMAJ. 2007;176(10):1449–1454. doi: 10.1503/cmaj.070335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Cochen V, Arbus C, Soto ME, et al. Sleep disorders and their impacts on healthy, dependent, and frail older adults. Journal of Nutrition, Health and Aging. 2009;13(4):322–329. doi: 10.1007/s12603-009-0030-0. [DOI] [PubMed] [Google Scholar]
- 35.Winkelman JW, Johnston L. Augmentation and tolerance with long-term pramipexole treatment of restless legs syndrome (RLS) Sleep Medicine. 2004;5(1):9–14. doi: 10.1016/j.sleep.2003.07.005. [DOI] [PubMed] [Google Scholar]
- 36.Garcia-Borreguero D, Allen R, Kohnen R, et al. Loss of response during long-term treatment of restless legs syndrome: guidelines approved by the International Restless Legs Syndrome Study Group for use in clinical trials. Sleep Medicine. 2010;11(9):956–957. doi: 10.1016/j.sleep.2010.08.001. [DOI] [PubMed] [Google Scholar]
- 37.Sakkas GK, Hadjigeorgiou GM, Karatzaferi C, et al. Intradialytic aerobic exercise training ameliorates symptoms of restless legs syndrome and improves functional capacity in patients on hemodialysis: a pilot study. ASAIO Journal. 2008;54(2):185–190. doi: 10.1097/MAT.0b013e3181641b07. [DOI] [PubMed] [Google Scholar]
- 38.Aukerman MM, Aukerman D, Bayard M, Tudiver F, Thorp L, Bailey B. Exercise and restless legs syndrome: a randomized controlled trial. Journal of the American Board of Family Medicine. 2006;19(5):487–493. doi: 10.3122/jabfm.19.5.487. [DOI] [PubMed] [Google Scholar]
- 39.Hornyak M, Grossmann C, Kohnen R, et al. Cognitive behavioural group therapy to improve patients' strategies for coping with restless legs syndrome: a proof-of-concept trial. Journal of Neurology, Neurosurgery and Psychiatry. 2008;79(7):823–825. doi: 10.1136/jnnp.2007.138867. [DOI] [PubMed] [Google Scholar]
- 40.Barnes PM, Bloom B, Nahin RL. Complementary and alternative medicine use among adults and children: United States, 2007. National Health Statistics Reports. 2009;(12):1–23. [PubMed] [Google Scholar]
- 41.Yang K. A review of yoga programs for four leading risk factors of chronic diseases. Evidence-Based Complementary and Alternative Medicine. 2007;4(4):487–491. doi: 10.1093/ecam/nem154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Innes KE, Vincent HK. The influence of yoga-based programs on risk profiles in adults with type 2 diabetes mellitus: a systematic review. Evidence-Based Complementary and Alternative Medicine. 2007;4(4):469–486. doi: 10.1093/ecam/nel103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Gordon LA, Morrison EY, McGrowder DA, et al. Effect of exercise therapy on lipid profile and oxidative stress indicators in patients with type 2 diabetes. BMC Complementary and Alternative Medicine. 2008;8, article 21 doi: 10.1186/1472-6882-8-21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Ross A, Thomas S. The health benefits of yoga and exercise: a review of comparison studies. Journal of Alternative and Complementary Medicine. 2010;16(1):3–12. doi: 10.1089/acm.2009.0044. [DOI] [PubMed] [Google Scholar]
- 45.Innes KE, Selfe TK, Taylor AG. Menopause, the metabolic syndrome, and mind-body therapies. Menopause. 2008;15(5):1005–1013. doi: 10.1097/01.gme.0b013e318166904e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Khalsa SBS, Shorter SM, Cope S, Wyshak G, Sklar E. Yoga ameliorates performance anxiety and mood disturbance in young professional musicians. Applied Psychophysiology Biofeedback. 2009;34(4):279–289. doi: 10.1007/s10484-009-9103-4. [DOI] [PubMed] [Google Scholar]
- 47.Butler LD, Waelde LC, Hastings TA, et al. Meditation with yoga, group therapy with hypnosis, and psychoeducation for long-term depressed mood: a randomized pilot trial. Journal of Clinical Psychology. 2008;64(7):806–820. doi: 10.1002/jclp.20496. [DOI] [PubMed] [Google Scholar]
- 48.Chen KM, Chen MH, Lin MH, Fan JT, Lin HS, Li CH. Effects of yoga on sleep quality and depression in elders in assisted living facilities. The Journal of Nursing Research. 2010;18(1):53–61. doi: 10.1097/JNR.0b013e3181ce5189. [DOI] [PubMed] [Google Scholar]
- 49.Innes KE, Selfe TK, Vishnu A. Mind-body therapies for menopausal symptoms: a systematic review. Maturitas. 2010;66(2):135–149. doi: 10.1016/j.maturitas.2010.01.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Chen KM, Chen MH, Chao HC, Hung HM, Lin HS, Li CH. Sleep quality, depression state, and health status of older adults after silver yoga exercises: cluster randomized trial. International Journal of Nursing Studies. 2009;46(2):154–163. doi: 10.1016/j.ijnurstu.2008.09.005. [DOI] [PubMed] [Google Scholar]
- 51.Yurtkuran M, Alp A, Yurtkuran M, Dilek K. A modified yoga-based exercise program in hemodialysis patients: a randomized controlled study. Complementary Therapies in Medicine. 2007;15(3):164–171. doi: 10.1016/j.ctim.2006.06.008. [DOI] [PubMed] [Google Scholar]
- 52.Bhatnagar OP, Anantharaman V. The effect of Yoga training on neuromuscular excitability and muscular relaxation. Neurology India. 1977;25(4):230–232. [PubMed] [Google Scholar]
- 53.Tergau F, Wischer S, Paulus W. Motor system excitability in patients with restless legs syndrome. Neurology. 1999;52(5):1060–1063. doi: 10.1212/wnl.52.5.1060. [DOI] [PubMed] [Google Scholar]
- 54.Scalise A, Pittaro-Cadore I, Janes F, Marinig R, Gigli GL. Changes of cortical excitability after dopaminergic treatment in restless legs syndrome. Sleep Medicine. 2010;11(1):75–81. doi: 10.1016/j.sleep.2009.05.003. [DOI] [PubMed] [Google Scholar]
- 55.Chaudhuri KR. The restless legs syndrome: time to recognize a very common movement disorder. Practical Neurology. 2003;3(4):204–213. [Google Scholar]
- 56.MacMahon D, Muzerengi S, Chaudhuri KR. Treatment and identification of restless legs syndrome. Prescriber. 2008;5:56–59. [Google Scholar]
- 57.Innes KE, Selfe TK, Alexander GK, Taylor AG. A new educational film control for use in studies of active mind-body therapies: acceptability and feasibility. Journal of Alternative and Complementary Medicine. 2011;17(5):453–458. doi: 10.1089/acm.2010.0401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Buysse DJ, Reynolds CF, Monk TH, Berman SR, Kupfer DJ. The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research. Psychiatry Research. 1989;28(2):193–213. doi: 10.1016/0165-1781(89)90047-4. [DOI] [PubMed] [Google Scholar]
- 59.Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. Journal of Health and Social Behavior. 1983;24(4):385–396. [PubMed] [Google Scholar]
- 60.Berger BG, Motl RW. Exercise and mood: a selective review and synthesis of research employing the Profile of Mood States. Journal of Applied Sport Psychology. 2000;12(1):69–92. [Google Scholar]
- 61.Ramanaiah NV, Franzen M, Schill T. A psychometric study of the State-Trait Anxiety Inventory. Journal of Personality Assessment. 1983;47(5):531–535. doi: 10.1207/s15327752jpa4705_14. [DOI] [PubMed] [Google Scholar]
- 62.Backhaus J, Junghanns K, Broocks A, Riemann D, Hohagen F. Test-retest reliability and validity of the Pittsburgh Sleep Quality Index in primary insomnia. Journal of Psychosomatic Research. 2002;53(3):737–740. doi: 10.1016/s0022-3999(02)00330-6. [DOI] [PubMed] [Google Scholar]
- 63.Picchietti D, Winkelman JW. Restless legs syndrome, periodic limb movements in sleep, and depression. Sleep. 2005;28(7):891–898. [PubMed] [Google Scholar]
- 64.Ströhle A. Physical activity, exercise, depression and anxiety disorders. Journal of Neural Transmission. 2009;116(6):777–784. doi: 10.1007/s00702-008-0092-x. [DOI] [PubMed] [Google Scholar]
- 65.Washburn RA, McAuley E, Katula J, Mihalko SL, Boileau RA. The physical activity scale for the elderly (PASE): evidence for validity. Journal of Clinical Epidemiology. 1999;52(7):643–651. doi: 10.1016/s0895-4356(99)00049-9. [DOI] [PubMed] [Google Scholar]
- 66.Koenig HG, Westlund RE, George LK, Hughes DC, Blazer DG, Hybels C. Abbreviating the Duke Social Support Index for use in chronically ill elderly individuals. Psychosomatics. 1993;34(1):61–69. doi: 10.1016/S0033-3182(93)71928-3. [DOI] [PubMed] [Google Scholar]
- 67.Cohen J. Statistical Power Analysis for the Behavioral Sciences. 2nd edition. Hillsdale,, NJ, USA: Lawrence Erlbaum Associates; 1988. [Google Scholar]
- 68.Cohen DL, Bloedon LT, Rothman RL, et al. Iyengar yoga versus enhanced usual care on blood pressure in patients with prehypertension to stage i hypertension: a randomized controlled trial. Evidence-based Complementary and Alternative Medicine. 2011;2011:8 pages. doi: 10.1093/ecam/nep130. Article ID 546428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Innes KE, Bourguignon C, Taylor AG. Risk indices associated with the insulin resistance syndrome, cardiovascular disease, and possible protection with yoga: a systematic review. Journal of the American Board of Family Practice. 2005;18(6):491–519. doi: 10.3122/jabfm.18.6.491. [DOI] [PubMed] [Google Scholar]
- 70.Saptharishi LG, Soudarssanane MB, Thiruselvakumar D, et al. Community-based randomized controlled trial of non-pharmacological interventions in prevention and control of hypertension among young adults. Indian Journal of Community Medicine. 2009;34(4):329–334. doi: 10.4103/0970-0218.58393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Saletu M, Anderer P, Högl B, et al. Acute double-blind, placebo-controlled sleep laboratory and clinical follow-up studies with a combination treatment of rr-L-dopa and sr-L-dopa in restless legs syndrome. Journal of Neural Transmission. 2003;110(6):611–626. doi: 10.1007/s00702-003-0814-z. [DOI] [PubMed] [Google Scholar]
- 72.Inoue Y, Kuroda K, Hirata K, Uchimura N, Kagimura T, Shimizu T. Long-term open-label study of pramipexole in patients with primary restless legs syndrome. Journal of the Neurological Sciences. 2010;294(1-2):62–66. doi: 10.1016/j.jns.2010.04.003. [DOI] [PubMed] [Google Scholar]
- 73.Happe S, Klösch G, Saletu B, Zeitlhofer J. Treatment of idiopathic restless legs syndrome (RLS) with gabapentin. Neurology. 2001;57(9):1717–1719. doi: 10.1212/wnl.57.9.1717. [DOI] [PubMed] [Google Scholar]
- 74.Bogan RK, Fry JM, Schmidt MH, Carson SW, Ritchie SY. Ropinirole in the treatment of patients with restless legs syndrome: a US-based randomized, double-blind, placebo-controlled clinical trial. Mayo Clinic Proceedings. 2006;81(1):17–27. doi: 10.4065/81.1.17. [DOI] [PubMed] [Google Scholar]
- 75.Partinen M, Hirvonen K, Jama L, et al. Efficacy and safety of pramipexole in idiopathic restless legs syndrome: a polysomnographic dose-finding study-The PRELUDE study. Sleep Medicine. 2006;7(5):407–417. doi: 10.1016/j.sleep.2006.03.011. [DOI] [PubMed] [Google Scholar]
- 76.McCormack PL, Siddiqui MAA. Pramipexole: in restless legs syndrome. CNS Drugs. 2007;21(5):429–440. doi: 10.2165/00023210-200721050-00008. [DOI] [PubMed] [Google Scholar]
- 77.Garcia-Borreguero D, Larrosa O, De la Llave Y, Verger K, Masramon X, Hernandez G. Treatment of restless legs syndrome with gabapentin: a double-blind, cross-over study. Neurology. 2002;59(10):1573–1579. doi: 10.1212/wnl.59.10.1573. [DOI] [PubMed] [Google Scholar]
- 78.Tison F, Crochard A, Léger D, Bouée S, Lainey E, El Hasnaoui A. Epidemiology of restless legs syndrome in French adults—a nationwide survey: the INSTANT Study. Neurology. 2005;65(2):239–246. doi: 10.1212/01.wnl.0000168910.48309.4a. [DOI] [PubMed] [Google Scholar]
- 79.Allen RP, Walters AS, Montplaisir J, et al. Restless legs syndrome prevalence and impact: REST general population study. Archives of Internal Medicine. 2005;165(11):1286–1292. doi: 10.1001/archinte.165.11.1286. [DOI] [PubMed] [Google Scholar]
- 80.Allen RP, Stillman P, Myers AJ. Physician-diagnosed restless legs syndrome in a large sample of primary medical care patients in western Europe: prevalence and characteristics. Sleep Medicine. 2010;11(1):31–37. doi: 10.1016/j.sleep.2009.03.007. [DOI] [PubMed] [Google Scholar]
- 81.Berger K, Luedemann J, Trenkwalder C, John U, Kessler C. Sex and the risk of restless legs syndrome in the general population. Archives of Internal Medicine. 2004;164(2):196–202. doi: 10.1001/archinte.164.2.196. [DOI] [PubMed] [Google Scholar]
- 82.Lee HB, Hening WA, Allen RP, Earley CJ, Eaton WW, Lyketsos CG. Race and restless legs syndrome symptoms in an adult community sample in east Baltimore. Sleep Medicine. 2006;7(8):642–645. doi: 10.1016/j.sleep.2006.03.015. [DOI] [PubMed] [Google Scholar]
- 83.Winkelman JW, Finn L, Young T. Prevalence and correlates of restless legs syndrome symptoms in the Wisconsin Sleep Cohort. Sleep Medicine. 2006;7(7):545–552. doi: 10.1016/j.sleep.2006.01.004. [DOI] [PubMed] [Google Scholar]
- 84.Hachul H, Bittencourt LRA, Andersen ML, Haidar MA, Baracat EC, Tufik S. Effects of hormone therapy with estrogen and/or progesterone on sleep pattern in postmenopausal women. International Journal of Gynecology and Obstetrics. 2008;103(3):207–212. doi: 10.1016/j.ijgo.2008.07.009. [DOI] [PubMed] [Google Scholar]
- 85.Polo-Kantola P, Erkkola R. Sleep and the menopause. Journal of the British Menopause Society. 2004;10(4):145–150. doi: 10.1258/1362180042721076. [DOI] [PubMed] [Google Scholar]
- 86.Saletu-Zyhlarz G, Anderer P, Gruber G, et al. Insomnia related to postmenopausal syndrome and hormone replacement therapy: sleep laboratory studies on baseline differences between patients and controls and double-blind, placebo-controlled investigations on the effects of a novel estrogen-progestogen combination (Climodien, Lafamme) versus estrogen alone. Journal of Sleep Research. 2003;12(3):239–254. doi: 10.1046/j.1365-2869.2003.00356.x. [DOI] [PubMed] [Google Scholar]
- 87.Weitz G, Elam M, Born J, Fehm HL, Dodt C. Postmenopausal estrogen administration suppresses muscle sympathetic nerve activity. Journal of Clinical Endocrinology and Metabolism. 2001;86(1):344–348. doi: 10.1210/jcem.86.1.7138. [DOI] [PubMed] [Google Scholar]
- 88.Rothdach AJ, Trenkwalder C, Haberstock J, Keil U, Berger K. Prevalence and risk factors of RLS in an elderly population: the MEMO study. Neurology. 2000;54(5):1064–1068. doi: 10.1212/wnl.54.5.1064. [DOI] [PubMed] [Google Scholar]
- 89.Wesström J, Nilsson S, Sundström-Poromaa I, Ulfberg J. Restless legs syndrome among women: prevalence, co-morbidity and possible relationship to menopause. Climacteric. 2008;11(5):422–428. doi: 10.1080/13697130802359683. [DOI] [PubMed] [Google Scholar]
- 90.Ghorayeb I, Bioulac B, Scribans C, Tison F. Perceived severity of restless legs syndrome across the female life cycle. Sleep Medicine. 2008;9(7):799–802. doi: 10.1016/j.sleep.2007.07.018. [DOI] [PubMed] [Google Scholar]
- 91.McEwen BS. Physiology and neurobiology of stress and adaptation: central role of the brain. Physiological Reviews. 2007;87(3):873–904. doi: 10.1152/physrev.00041.2006. [DOI] [PubMed] [Google Scholar]
- 92.McEwen BS. Sleep deprivation as a neurobiologic and physiologic stressor: allostasis and allostatic load. Metabolism. 2006;55(supplement 1):S20–S23. doi: 10.1016/j.metabol.2006.07.008. [DOI] [PubMed] [Google Scholar]
- 93.Brown RP, Gerbarg PL. Sudarshan Kriya yogic breathing in the treatment of stress, anxiety, and depression: part I—neurophysiologic model. Journal of Alternative and Complementary Medicine. 2005;11(1):189–201. doi: 10.1089/acm.2005.11.189. [DOI] [PubMed] [Google Scholar]
- 94.Innes KE, Vincent HK, Taylor AG. Chronic stress and insulin resistance-related indices of cardiovascular disease risk, part I: neurophysiological responses and pathological sequelae. Alternative Therapies in Health and Medicine. 2007;13(4):46–52. [PubMed] [Google Scholar]
- 95.Innes KE, Vincent HK, Taylor AG. Chronic stress and insulin resistance-related indices of cardiovascular disease risk, part 2: a potential role for mind-body therapies. Alternative Therapies in Health and Medicine. 2007;13(5):44–51. [PubMed] [Google Scholar]
- 96.Cohen DL, Wintering N, Tolles V, et al. Cerebral blood flow effects of yoga training: preliminary evaluation of 4 cases. Journal of Alternative and Complementary Medicine. 2009;15(1):9–14. doi: 10.1089/acm.2008.0008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Streeter CC, Jensen JE, Perlmutter RM, et al. Yoga Asana sessions increase brain GABA levels: a pilot study. Journal of Alternative and Complementary Medicine. 2007;13(4):419–426. doi: 10.1089/acm.2007.6338. [DOI] [PubMed] [Google Scholar]
- 98.Kjaer TW, Bertelsen C, Piccini P, Brooks D, Alving J, Lou HC. Increased dopamine tone during meditation-induced change of consciousness. Cognitive Brain Research. 2002;13(2):255–259. doi: 10.1016/s0926-6410(01)00106-9. [DOI] [PubMed] [Google Scholar]
- 99.Leknes S, Tracey I. A common neurobiology for pain and pleasure. Nature Reviews Neuroscience. 2008;9(4):314–320. doi: 10.1038/nrn2333. [DOI] [PubMed] [Google Scholar]
- 100.Mignot E, Taheri S, Nishino S. Sleeping with the hypothalamus: emerging therapeutic targets for sleep disorders. Nature Neuroscience. 2002;5:1071–1075. doi: 10.1038/nn944. [DOI] [PubMed] [Google Scholar]
- 101.Goerendt IK, Messa C, Lawrence AD, Grasby PM, Piccini P, Brooks DJ. Dopamine release during sequential finger movements in health and Parkinson’s disease: a PET study. Brain. 2003;126(2):312–325. doi: 10.1093/brain/awg035. [DOI] [PubMed] [Google Scholar]
- 102.Scranton R, Cincotta A. Bromocriptine unique formulation of a dopamine agonist for the treatment of type 2 diabetes. Expert Opinion on Pharmacotherapy. 2010;11(2):269–279. doi: 10.1517/14656560903501544. [DOI] [PubMed] [Google Scholar]
- 103.Belavic JM. A new treatment option for type 2 diabetes. The Nurse Practitioner. 2010;35(1):51–52. doi: 10.1097/01.NPR.0000366132.75858.20. [DOI] [PubMed] [Google Scholar]
- 104.Lloyd KG, Worms P. Neuropharmacological actions of GABA agonists: predictability for their clinical usefulness. Advances in Biochemical Psychopharmacology. 1981;29:59–67. [PubMed] [Google Scholar]
- 105.Shiah IS, Yatham LN. GABA function in mood disorders: an update and critical review. Life Sciences. 1998;63(15):1289–1303. doi: 10.1016/s0024-3205(98)00241-0. [DOI] [PubMed] [Google Scholar]
- 106.Enna SJ, McCarson KE. The role of GABA in the mediation and perception of pain. Advances in Pharmacology. 2006;54:1–27. doi: 10.1016/s1054-3589(06)54001-3. [DOI] [PubMed] [Google Scholar]
- 107.Chouinard G. The search for new off-label indications for antidepressant, antianxiety, antipsychotic and anticonvulsant drugs. Journal of Psychiatry and Neuroscience. 2006;31(3):168–176. [PMC free article] [PubMed] [Google Scholar]
- 108.Arnold LM, Goldenberg DL, Stanford SB, et al. Gabapentin in the treatment of fibromyalgia: a randomized, double-blind, placebo-controlled, multicenter trial. Arthritis and Rheumatism. 2007;56(4):1336–1344. doi: 10.1002/art.22457. [DOI] [PubMed] [Google Scholar]
- 109.Baillie JK, Power I. The mechanism of action of gabapentin in neuropathic pain. Current Opinion in Investigational Drugs. 2006;7(1):33–39. [PubMed] [Google Scholar]
- 110.Fulda S, Wetter TC. Where dopamine meets opioids: a meta-analysis of the placebo effect in restless legs syndrome treatment studies. Brain. 2008;131, part 4:902–917. doi: 10.1093/brain/awm244. [DOI] [PubMed] [Google Scholar]
- 111.Benes H, Walters AS, Allen RP, Hening WA, Kohnen R. Definition of restless legs syndrome, how to diagnose it, and how to differentiate it from RLS mimics. Movement Disorders. 2007;22(supplement 18):S401–S408. doi: 10.1002/mds.21604. [DOI] [PubMed] [Google Scholar]
- 112.Brindani F, Vitetta F, Gemignani F. Restless legs syndrome: differential diagnosis and management with pramipexole. Clinical Interventions in Aging. 2009;4:305–313. doi: 10.2147/cia.s4143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Hansen RA, Song L, Moore CG, et al. Effect of ropinirole on sleep outcomes in patients with restless legs syndrome: meta-Analysis of pooled individual patient data from randomized controlled trials. Pharmacotherapy. 2009;29(3):255–262. doi: 10.1592/phco.29.3.255. [DOI] [PubMed] [Google Scholar]
- 114.Conti CF, De Oliveira MM, Andriolo RB, et al. Levodopa for idiopathic restless legs syndrome: evidence-based review. Movement Disorders. 2007;22(13):1943–1951. doi: 10.1002/mds.21662. [DOI] [PubMed] [Google Scholar]
- 115.Conti CF, De Oliveira MM, Valbuza JS, Prado LBF, De Carvalho LBC, Prado GFD. Anticonvulsants to treat idiopathic restless legs syndrome: systematic review. Arquivos de Neuro-Psiquiatria. 2008;66(2):431–435. doi: 10.1590/s0004-282x2008000300034. [DOI] [PubMed] [Google Scholar]
- 116.Kushida CA. Ropinirole for the treatment of restless legs syndrome. Neuropsychiatric Disease and Treatment. 2006;2(4):407–419. doi: 10.2147/nedt.2006.2.4.407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Winkelman JW, Redline S, Baldwin CM, Resnick HE, Newman AB, Gottlieb DJ. Polysomnographic and health-related quality of life correlates of restless legs syndrome in the sleep heart health study. Sleep. 2009;32(6):772–778. doi: 10.1093/sleep/32.6.772. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Hornyak M, Kopasz M, Berger M, Riemann D, Voderholzer U. Impact of sleep-related complaints on depressive symptoms in patients with restless legs syndrome. Journal of Clinical Psychiatry. 2005;66(9):1139–1145. doi: 10.4088/jcp.v66n0909. [DOI] [PubMed] [Google Scholar]
- 119.Hening W, Walters AS, Allen RP, Montplaisir J, Myers A, Ferini-Strambi L. Impact, diagnosis and treatment of restless legs syndrome (RLS) in a primary care population: the REST (RLS epidemiology, symptoms, and treatment) primary care study. Sleep Medicine. 2004;5(3):237–246. doi: 10.1016/j.sleep.2004.03.006. [DOI] [PubMed] [Google Scholar]


