Abstract
Traditional knowledge is an important source of obtaining new phytotherapeutic agents. Ethnobotanical survey of medicinal plants was conducted in Nossa Senhora Aparecida do Chumbo District (NSACD), located in Poconé, Mato Grosso, Brazil using semi-structured questionnaires and interviews. 376 species of medicinal plants belonging to 285 genera and 102 families were cited. Fabaceae (10.2%), Asteraceae (7.82%) and Lamaceae (4.89%) families are of greater importance. Species with the greater relative importance were Himatanthus obovatus (1.87), Hibiscus sabdariffa (1.87), Solidago microglossa (1.80), Strychnos pseudoquina (1.73) and Dorstenia brasiliensis, Scoparia dulcis L., and Luehea divaricata (1.50). The informant consensus factor (ICF) ranged from 0.13 to 0.78 encompassing 18 disease categories,of which 15 had ICF greater than 0.50, with a predominance of disease categories related to injuries, poisoning and certain other consequences of external causes (ICF = 0.78) having 65 species cited while 20 species were cited for mental and behavioral disorders (ICF = 0.77). The results show that knowledge about medicinal plants is evenly distributed among the population of NSACD. This population possesses medicinal plants for most disease categories, with the highest concordance for prenatal, mental/behavioral and respiratory problems.
1. Introduction
Despite the fact that modern medicine, on the basis of the complex pharmaceutical industry, is well developed in most part of the world, the World Health Organization (WHO) through it Traditional Medicine Program recommends its Member States to formulate and develop policies for the use of complementary and alternative medicine (CAM) in their national health care programmes [1]. Among the components of CAM, phytotherapy practiced by the greater percentage of the world population through the use of plants or their derivatives, occupies a significant and unique position [2].
In this sense, documentation of the indigenous knowledge through ethnobotanical studies is important in the conservation and utilization of biological resources [3].
Brazil is a country with floral megadiversity, possessing six ecological domains, namely, Amazonian forest, Caatinga, Pampas, Cerrado, Atlantic Forest, and the Pantanal [4]. Mato Grosso region is noteworthy in this regard, as it occupies a prominent position both in the national and international settings, for it presents three major Brazilian ecosystems (the Pantanal, Cerrado, and Amazonian rainforest). Besides this, it also hosts diverse traditional communities in its territories, namely, the Indians descents (Amerindians), African descents, and the white Europeans. However, due to the mass migration from the rural areas and technological development, coupled with globalization of knowledge by the dominant nations, cultural tradition concerning the use of medicinal plants is in the major phase of declining [5].
The Pantanal is distinguishably the largest wetland ecosystem of the world, according to the classification by UNESCO World Heritage Center (Biosphere Reserve) [4]. The Pantanal vegetation is a mosaic consisting of species of the Amazonian rainforest, Cerrado, Atlantic forest, and Bolivian Chaco, adapted to special conditions, where there is alternations of both high humidity and pronounced dryness during the time of the year [4]. The presence in the Pantanal of the traditional populations that use medicinal plants for basic health care makes this region an important field for the ethnobotanical and ethnopharmacological studies [6, 7].
Because of the fact that the Pantanal communities are relatively isolated, they have developed private lives that involved much reliance on profound knowledge of the biological cycles, utilization of natural resources, and traditional technology heritage [8].
As a result of the aforementioned, this study aimed to systematically and quantitatively evaluate the information gathered from these Pantanal communities, highlight the relevance of the ethnobotanical findings, and cite and discuss relevant literatures related to medicinal plants with greater relative importance (RI) and high informant consensus factor (ICF) values obtained in the study.
2. Materials and Methods
2.1. Study Area
For the choice of study area, literature search was conducted to identify the Pantanal region in Mato Grosso, consisting of traditional communities where such studies have not yet been conducted and/or there were no ethnobotanical survey publications. The study design was cross-sectional and was conducted between the period of November, 2009 and February, 2010. The study setting chosen was NSACD located in the Poconé municipality, Mato Grosso State, Central West of Brazil (Figure 1) with coordinates of 16° 02′ 90′′ S and 056° 43′ 49′′ W. Poconé is located within the region of Cuiabá River valley, with an altitude of 142 m, occupies a territorial area of 17,260.86 km2, and of tropical climate. The mean annual temperature is 24°C (4–42°C) and the mean annual rainfall is 1,500 mm with rainy season occurring between December and February. The municipality is composed of 2 Districts (NSAC and Cangas), 5 villages, 11 settlements, 14 streets, and 72 communities (countryside) [9]. The population of NSACD is estimated to be 3,652 inhabitants, representing 11.5% of Poconé municipality [10]. The principal economic activities are mainly livestock farming, mining, and agriculture with great tourism potentials, because Poconé municipality is the gateway to the Pantanal region [9].
Figure 1.
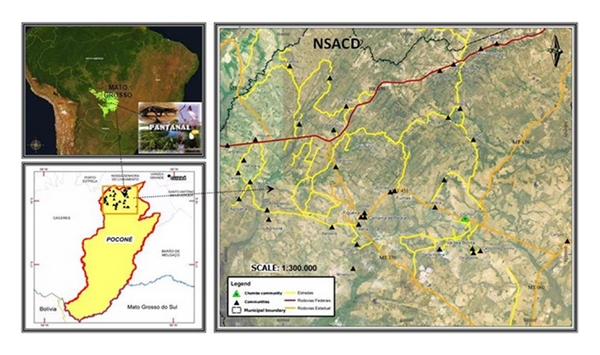
Location of the study area. Poconé, Mato Grosso, in Midwest of Brazil.
2.2. Consent and Ethical Approval
Authorization and ethical clearance were sought from the relevant government (Health authority of Poconé and the National Council of Genetic Heritage of the Ministry of Environment (CGEN/MMA), Resolution 247 published in the Federal Official Gazette, in October, 2009, on access to the traditional knowledge for scientific research and Federal University of Mato Grosso and Júlio Muller Hospital Research Ethical Committees, Protocol 561/CEP-HUJM/08 authorities. Previsits were made to each community of NSACD to present the research project as well as to seek the consent of each potential informant.
2.3. Data Collection and Analysis
In this present study, sampling was done using probabilistic simple randomization and stratified sampling techniques [10, 11].
The population studied consists of inhabitants of 13 communities of NSACD, Mato Grosso State, considering an informant per family. The criteria for each informant chosen were age of 40 and above, residing in NSACD for more than 5 years (because there is large migration into the area because of the presence of ethanol producing factory).
These criteria are in line with the study objective coupled with the information gathered from the local authority [12].
In order to determine the estimated sample size (n), in this case, the number of families to be sampled per communities being considered, the following formula was utilized [11, 13]:
| (1) |
This study considered the population size of 1,179 families (N = 1, 179), confidence coefficient of 95% (z/2 = 1.96), sampling error of 0.05 (d = 0.05), a proportion of 0.5 (P = 0.5). It should be noted that the P = 0.5 was assigned due to nonexistence of previous information about this value as is usual in practice, to obtain conservative sample size which is representative at the same time.
In determining the sample size for the microarea, 5% error and 10% loss in sample were considered. To determine the sample size in each microarea, the sample size (290) was multiplied by the sampling fraction of each microarea and dividing the total number of families of the same microarea with the total number of families of all the microareas (1,179), thereby arriving at the sample sizes for each area as shown in Table 1.
Table 1.
Distribution of the 13 communities of Nossa Senhora Aparecida do Chumbo District.
| ID | COMMUNITY | Total number of individuals | Total number of families | Sample fraction | Sample size |
|---|---|---|---|---|---|
| 1 | Chumbo | 946 | 216 | 0.1832 | 52 |
| 2 | Canto do Agostinho, Santa Helena, Os Cagados, Várzea bonita | 179 | 52 | 0.0441 | 15 |
| 3 | Furnas II, Salobra, Zé Alves | 165 | 59 | 0.0500 | 15 |
| 4 | Campina II, Furnas I, Mundo Novo, Rodeio | 279 | 81 | 0.0687 | 20 |
| 5 | Campina de Pedra, Imbé | 188 | 67 | 0.0568 | 16 |
| 6 | Barreirinho, Coetinho, Figueira | 253 | 95 | 0.0806 | 23 |
| 7 | Bahia de Campo | 257 | 74 | 0.0628 | 18 |
| 8 | Agrovila, São Benedito | 184 | 66 | 0.0560 | 16 |
| 9 | Agroana | 372 | 178 | 0. 1510 | 44 |
| 10 | Bandeira, Minadouro | 248 | 82 | 0.0696 | 20 |
| 11 | Carretão, Deus Ajuda, Sangradouro, Pesqueiro, Varzearia | 216 | 77 | 0.0653 | 19 |
| 12 | Chafariz, Ramos, Sete Porcos, Urubamba | 208 | 67 | 0.0568 | 16 |
| 13 | Céu Azul, Capão Verde, Morro Cortado, Passagem de Carro, Varal | 157 | 65 | 0.0551 | 16 |
|
| |||||
| Total | 3,652 | 1,179 | 1.0000 | 290 | |
ID = identification of the microarea.
The interviews were conducted with the help of 12 trained applicators, under the supervision of the respective investigator. Data collected included sociodemographic details, vernacular names of the plant species with their medicinal uses, methods of drug preparation, and other relevant information. The ethnobotanical data were organized using the Microsoft Office Access 2003 program and statistically analyzed using SPSS, version 15 for Windows (SPSS Inc., Chicago, Illinois, USA).
2.4. Plant Collection, Identification, and Herborization
The collection of plant materials were done in collaboration with the local specialists, soon after the interviews. Both indigenous and scientific plant names were compiled. The plant materials collected during the study period were herborized, mounted as herbarium voucher specimens, and deposited for taxonomic identification and inclusion in the collection of Federal University of Mato Grosso and CGMS Herbarium of Federal University of Mato Grosso do Sul, Brazil.
Plant species were identified according to standard taxonomic methods, based on floral morphological characters, analytical keys, and using, where possible, samples for comparison, as well as consultations with experts and literature [6, 7, 14–19]. The plant species obtained were grouped into families according to the classification system of Cronquist [20], with the exception of the Pteridophyta and Gymnospermae. For corrections of scientific names and families, the official website of the Missouri Botanical Garden was consulted [21].
2.5. Quantitative Ethnobotany
The relative importance (RI) of each plant species cited by the informants was calculated according to a previously proposed method [22]. In order to calculate RI, the maximum obtainable by a species is two was calculated using (2) according to Oliveira et al. [23]
| (2) |
where RI: relative importance; NCS: number of body systems. It is given by the number of body systems, treated by a species (NSCS) over the total number of body system treated by the most versatile species (NSCSV): NCS = NSCS/NSCSV; NP: number of properties attributed to a specific species (NPS) over the total number of properties attributed to the most versatile species (NPSV): NP = NPS/NPSV.
We sought to identify the therapeutic indications which were more important in the interviews to determine the informant consensus factor (ICF), which indicates the homogenity of the information [23].
The ICF will be low (close to 0), if the plants are chosen randomly, or if the informants do not exchange information about their uses. The value will be high (close to 1), if there is a well defined criterion of selection in the community and/or if the information is exchanged among the informants [23].
ICF was calculated using the number of use citations in each category of plant disease (n ur), minus the number of species used (n t) divided by the number of use citations in each category minus one on the basis of (3):
| (3) |
The citations for therapeutic purposes were classified using the 20 categories of the International Classification of Diseases and Related Health Problems, 10th edition-CID [24]: injuries, certain infectious, and parasitic diseases (I); neoplasms-tumors (II), diseases of blood and blood-forming organs and certain disorders involving the immune mechanism (III), endocrine, nutritional and metabolic diseases (IV) mental and behavioral disorders (V), nervous system (VI), diseases of eye and adnexa (VII), diseases of the ear and mastoid process (VIII), diseases of the circulatory system (IX), respiratory diseases (X), digestive diseases (XI), diseases of the skin and subcutaneous tissue (XII), diseases of the musculoskeletal system and connective tissue (XIII), genitourinary diseases (XIV), pregnancy, childbirth and (XV), certain conditions originating during the perinatal period (XVI), symptoms, signs and abnormal clinical and laboratory findings, not elsewhere classified (XVIII) and injury, poisoning and certain other consequences of external causes (XIX).
We selected for further discussion species that presented RI ≥ 1.5, and are in a category with high ICF. We conducted literature review using among others, the databases of Web of Science, MEDLINE, SciELO and including nonindexed works. We also searched national data bases for dissertations and theses.
3. Results
A total of 262 informants were interviewed, representing 7.17% of the population of NSACD, 22.22% of the population aged ≥40 years and residing in the District for over five years. Of the respondents, 69% were female and 31% male, aged 40–94 years (median 55). 68% were born in the city of Poconé, and 62% have been residents for over 20 years in the District (Table 2).
Table 2.
Distribution of the 13 communities of Nossa Senhora Aparecida do Chumbo District, Poconé, Mato Grosso, Brazil.
| ID | Comunity | Population | Number of individualsa | Sample fraction | Sample size | N | Plant citations |
|---|---|---|---|---|---|---|---|
| 1 | Chumbo | 946 | 216 | 0.1832 | 52 | 50 | 827 |
| 2 | Canto do Agostinho, Santa Helena, Os Cagados, Várzea bonita | 179 | 52 | 0.0441 | 15 | 10 | 131 |
| 3 | Furnas II, Salobra, Zé Alves | 165 | 59 | 0.050 | 15 | 10 | 99 |
| 4 | Campina II, Furnas I, Mundo Novo, Rodeio | 279 | 81 | 0.0687 | 20 | 11 | 179 |
| 5 | Campina de Pedra, Imbé | 188 | 67 | 0.0568 | 16 | 12 | 173 |
| 6 | Barreirinho, Coetinho, Figueira | 253 | 95 | 0.0806 | 23 | 23 | 213 |
| 7 | Bahia de Campo | 257 | 74 | 0.0628 | 18 | 13 | 461 |
| 8 | Agrovila, São Benedito | 184 | 66 | 0.056 | 16 | 16 | 141 |
| 9 | Agroana | 372 | 178 | 0.151 | 44 | 38 | 349 |
| 10 | Bandeira, Minadouro | 248 | 82 | 0.0696 | 20 | 22 | 171 |
| 11 | Carretão, Deus Ajuda, Sangradouro, Pesqueiro, Varzearia | 216 | 77 | 0.0653 | 19 | 23 | 180 |
| 12 | Chafariz, Ramos, Sete Porcos, Urubamba | 208 | 67 | 0.0568 | 16 | 16 | 200 |
| 13 | Céu Azul, Capão Verde, Morro Cortado, Passagem de Carro, Varal | 157 | 65 | 0.0551 | 16 | 18 | 165 |
| N | 3,652 | 1,179 | 1.000 | 290 | 262 | 3,289 |
ID: Identification of the microarea; N: Sample size; aInformants with age ≥ 40 years and period of residing ≥ 5 years.
Of the 262 respondents, 259 (99.0%) reported the use of medicinal plants in self health care, with a minimum of 1 plant and a maximum of 250 plants among the female respondents and a minimum of 2 plants and a maximum of 54 among the male respondents. A total of 3,289 citations were recorded corresponding to 376 different plant species which belong to 285 genera and 102 families. Fabaceae (10.2%), Asteraceae (7.82%), and Lamaceae (4.89%) families were the most representative in this study (Table 3).
Table 3.
Relation of the relative importance of the plant species mentioned by informants of Nossa Senhora Aparecida do Chumbo District, Poconé, Mato Grosso, Brazil.
| Family/species | Vernacular name | Application | Preparation (administration) | Uses listed | NCS | NP | RI |
|---|---|---|---|---|---|---|---|
| 1. ACANTHACEAE | |||||||
| 1.1. Justicia pectoralis Jacq. | Anador | pain, fever, laxative, and muscle relaxant | Infusion (I) | 36 | 2 | 3 | 0.40 |
| 2. ADOXACEAE | |||||||
| 2.1. Sambucus australis Cham. & Schltdl. | Sabugueiro | Fever and measles | Infusion (I, E) | 24 | 2 | 2 | 0.33 |
| 3. ALISMATACEAE | |||||||
| 3.1. Echinodorus macrophyllus (Kuntze.) Micheli | Chapéu-de- couro | blood cleanser, stomach, rheumatism, and kidneys | 43 | 4 | 4 | 0.67 | |
| 4. AMARYLLIDACEAE | |||||||
| 4.1. Allium cepa L. | Cebola | wound healing | Infusion (I) | 1 | 1 | 1 | 0.17 |
| 4.2. Allium fistulosum L. | Cebolinha | Flu | Infusion (I) | 1 | 1 | 1 | 0.17 |
| 4.3. Allium sativum L. | Alho | hypertension | Infusion (I) | 7 | 1 | 1 | 0.17 |
| 5. AMARANTHACEAE | |||||||
| 5.1. Alternanthera brasiliana (L.) Kuntze | Terramicina | wound healing, itching, diabetes, pain, bone fractures, throat, flu, inflammation uterine, and relaxative muscular | Infusion (I, E) | 41 | 6 | 9 | 1.20 |
| 5.2. Alternanthera dentata(Moench) Stuchlik ex R.E. Fr. | Ampicilina | wound healing and kidneys | Infusion (I, E) | 7 | 2 | 2 | 0.33 |
| 5.3. Alternanthera ficoide (L.) P. Beauv. | Doril | muscular relaxative | Infusion (I, E) | 3 | 1 | 1 | 0.17 |
| 5.4. Amaranthus aff. viridis L. | Caruru-de-porco | wound healing, pain, and kidneys | Infusion (I) | 4 | 3 | 3 | 0.50 |
| 5.5. Beta vulgaris L. | Beterraba | anemia | Infusion (I) | 1 | 1 | 1 | 0.17 |
| 5.6. Celosia argentea L. | Crista-de-galo | kidneys | 5 | 3 | 3 | 0.50 | |
| 5.7. Chenopodium ambrosioides L. | Erva-de-santa-maria | wound healing, heart, diabetes, bone fractures, flu, kidneys, cough, and worms | Infusion (I, E) | 102 | 7 | 8 | 1.23 |
| 5.8. Pfaffia glomerata (Spreng.) Pedersen | Ginseng-brasileiro | Obesity | Infusion (I) | 2 | 1 | 1 | 0.17 |
| 6. ANACARDIACEAE | |||||||
| 6.1. Anacardium humile A. St.– Hil. | Cajuzinho-do-campo | diabetes, dysentery, and hepatitis | Infusion (I, E) | 5 | 3 | 3 | 0.50 |
| 6.2. Anacardium occidentale L. | Cajueiro | abortive, wound healing, cholesterol, teeth, blood cleanser, diabetes, diarrhea, dysentery, and pain | Infusion (I, E) | 30 | 6 | 9 | 1.20 |
| 6.3. Astronium fraxinifolium Schott ex Spreng | Gonçaleiro | flu, hemorrhoids, and cough | Infusion and maceration (I, E) | 8 | 3 | 3 | 0.50 |
| 6.4. Mangifera indica L. | Mangueira | Bronchitis, flu, and cough | Infusion and maceration (I, E) | 11 | 2 | 3 | 0.40 |
| 6.5. Myracrodruon urundeuva (Allemão) Engl. | Aroeira | anemia, bladder bronchitis cancer, wound healing, blood cleanser, bone fractures, hernia, uterine inflammation, muscular relaxative, and cough | Infusion, maceration, and decoction (I, E) | 84 | 7 | 11 | 1.43 |
| 6.6. Spondias dulcis Parkinson | Caja-manga | scabies | Infusion (I, E) | 2 | 1 | 1 | 0.17 |
| 6.7. Spondias purpurea L. | Seriguela | wound healing and hepatitis | Infusion (I, E) | 2 | 2 | 2 | 0.33 |
| 7. ANNONACEAE | |||||||
| 7.1. Annona cordifolia Poepp. ex Maas & Westra | Araticum-abelha | Diabetes and bone fractures | Infusion and decoction (I, E) | 3 | 2 | 2 | 0.33 |
| 7.2. Annona crassiflora Mart. | Graviola | diabetes | Infusion (I, E) | 11 | 1 | 1 | 0.17 |
| 7.3. Duguetia furfuracea (A. St.- Hil.) Saff. | Beladona-do-cerrado | pain | Infusion (I, E) | 1 | 1 | 1 | 0.17 |
| 8. APIACEAE | |||||||
| 8.1. Coriandrum sativum L. | Coentro | flu | Infusion (I) | 1 | 1 | 1 | 0.17 |
| 8.2. Eryngium aff. pristis Cham. & Schltdl. | Lingua-de-tucano | Tooth and muscular relaxative | Infusion (I) | 3 | 2 | 2 | 0.33 |
| 8.3. Petroselinum crispum ((Mill) Fuss | Salsinha | flu | Infusion (I) | 1 | 1 | 1 | 0.17 |
| 8.4. Pimpinella anisum L. | Erva-doce | pain soothing, constipation, and kidneys | Infusion (I, E) | 12 | 3 | 3 | 0.50 |
| 9. APOCYNACEAE | |||||||
| 9.1. Aspidosperma polyneuron (Müll.) Arg. | Péroba | Stomach and laxative | Infusion and decoction (I, E) | 5 | 1 | 2 | 0.23 |
| 9.2. Aspidosperma tomentosum Mart. | Guatambu | gastritis | Infusion (I) | 4 | 1 | 1 | 0.17 |
| 9.3. Catharanthus roseus (L.) G. Don | Boa-noite | mumps fever and kidneys | Infusion (I) | 8 | 3 | 3 | 0.50 |
| 9.4. Geissospermum laeve (Vell.) Miers | Pau-tenente | Diabetes and pain | Infusion (I) | 6 | 2 | 2 | 0.33 |
| 9.5. Hancornia speciosa var. gardneri (A. DC.) Müll. Arg. | Mangava-mansa | itching, diarrhea, and stomach | Decoction and maceration (I, E) | 8 | 3 | 3 | 0.50 |
| 9.6. Himatanthus obovatus (Müll. Arg.) Woodson | Angélica | anemia, wound healing, cholesterol, blood cleanser, pain, nose bleeding, hypertension, uterine inflammation, labyrinthitis, pneumonia, relaxative muscular, worms, and vitiligo | Maceration (I) | 45 | 10 | 13 | 1.87 |
| 9.7. Macrosiphonia longiflora (Desf.) Müll. Arg. | Velame-do-campo | hearth, blood cleanser, stroke, diuretic, pain, throat, muscular relaxative, and vitiligo | Decoction (I) | 5 | 6 | 8 | 1.13 |
| 9.8. Macrosiphonia velame (A. St.-Hil.) Müll. Arg. | Velame-branco | flu | Decoction (I) | 73 | 1 | 1 | 0.17 |
| 10. ARACEAE | |||||||
| 10.1 Dieffenbachia picta Schott | Comigo-ninguém-pode | pain | Maceration (E) | 2 | 1 | 1 | 0.17 |
| 10.2. Dracontium sp. | Jararaquinha | snakebite | Infusion (I) | 10 | 1 | 1 | 0.17 |
| 11. ARECACEAE | |||||||
| 11.1. Acrocomia aculeata Lodd. ex. Mart. | Bocaiuveira | heart, hepatitis, hypertension, and kidneys | Decoction and syrup (I) | 20 | 4 | 4 | 0.67 |
| 11.2. Cocos nucifera L. | Cocô-da-bahia | kidneys | Maceration (I) | 2 | 1 | 1 | 0.17 |
| 11.3. Orbignya phalerata Mart. | Babaçu | inflammation | Decoction (I) | 8 | 1 | 1 | 0.17 |
| 11.4. Syagrus oleracea (Mart.) Becc. | Guariroba | kidneys | Maceration (I) | 2 | 1 | 1 | 0.17 |
| 12. ARISTOLOCHIACEAE | |||||||
| 12.1. Aristolochia cymbifera Mart & Zucc. | Cipó-de-mil-homem | dengue, blood cleanser, stomach, kidneys, and digestive | Infusion (I) | 11 | 4 | 5 | 0.73 |
| 12.2. Aristolochia esperanzae Kuntze | Papo-de-peru | wound healing | Infusion (I) | 3 | 1 | 1 | 0.17 |
| 13. ASTERACEAE | |||||||
| 13.1. Acanthospermum australe (Loefl.). Kuntze | Carrapicho, beijo-de-boi | colic, kidneys, and runny cough | Infusion (I) | 31 | 2 | 3 | 0.40 |
| 13.2. Acanthospermum hispidum DC. | Chifre-de-garrotinho | Gonorrhea and kidneys | Infusion (I) | 5 | 2 | 3 | 0.40 |
| 13.3. Achillea millefolium L. | Dipirona, Novalgina, | pain, flu, and muscular relaxative | Infusion (I) | 13 | 3 | 4 | 0.57 |
| 13.4. Achyrocline satureioides (Lam.) DC. | Macela-do-campo | diarrhea, pain, stomach, gastritis, flu, and hypertension | Infusion (I) | 13 | 5 | 6 | 0.90 |
| 13.5. Ageratum conyzoides L. | Mentrasto | pain, labor pain, stomach, swelling in pregnant woman, rheumatism, and cough | Infusion (I) | 18 | 5 | 6 | 0.90 |
| 13.6. Artemisia vulgaris L. | Artemisia | insomnia | Infusion (I) | 3 | 1 | 1 | 0.17 |
| 13.7. Artemisia absinthium L. | Losna, nor-vômica | pain, stomach, liver, hernia, and muscular relaxative | Infusion (I) | 39 | 4 | 5 | 0.73 |
| 13.8. Baccharis trimera (Less.) DC. | Carqueja | cancer, cholesterol, diabetes, diuretic, stomach, flu, and obesity | Infusion (I) | 31 | 5 | 7 | 0.97 |
| 13.9. Bidens pilosa L. | Picão-preto | hepatitis, enteric, and kidneys | Infusion (I, E) | 20 | 3 | 3 | 0.50 |
| 13.10. Brickellia brasiliensis (Spreng.) B.L. Rob. | Arnica-do-campo | wound healing, uterine inflammation, and kidneys | Infusion (I) | 13 | 2 | 3 | 0.40 |
| 13.11. Calendula officinalis L. | Calêndula | anxiety | Infusion (I) | 6 | 1 | 1 | 0.17 |
| 13.12. Centratherum aff. punctatum Cass. | Perpétua-roxa | muscular relaxative, and hearth | Infusion (I) | 3 | 2 | 2 | 0.33 |
| 13.13. Chamomilla recutita (L.) Rauschert. | Camomila | soothing colic, pain, stomach, fever, and flu | Infusion (I) | 78 | 5 | 6 | 0.90 |
| 13.14. Chaptalia integerrima (Vell.) Burkart | Lingua-de-vaca | worms | Infusion (I) | 6 | 1 | 1 | 0.17 |
| 13.15. Chromolaena odorata (L.) R.M. King & H. Rob | Cruzeirinho | colic, pain, bone fractures, pain, bone fractures, and kidneys | Infusion (I) | 7 | 3 | 4 | 0.57 |
| 13.16. Conyza bonariensis (L.) Cronquist | Voadeira | cancer itching, blood cleanser, leukemia, and worms | Infusion (I) | 15 | 4 | 5 | 0.73 |
| 13.17. Elephantopus mollis Kunth | Sussuaiá | blood cleanser, pain, and uterine inflammation | Infusion (I) | 11 | 2 | 3 | 0.40 |
| 13.18. Emilia fosbergii Nicolson | Serralha | conjunctivitis | Infusion (I) | 6 | 1 | 1 | 0.17 |
| 13.19. Eremanthus exsuccus (DC.) Baker | Bácimo-do-campo | wound healing, stomach, bone fractures, and skin | Infusion and maceration (I, E) | 11 | 3 | 4 | 0.57 |
| 13.20. Eupatorium odoratum L. | Arnicão | wound healing, muscular relaxative, and kidneys | Infusion (I, E) | 10 | 3 | 3 | 0.50 |
| 13.21. Mikania glomerata Spreng. | Guaco | bronchitis cough | Infusion (I) | 14 | 2 | 2 | 0.33 |
| 13.22. Mikania hirsutissima DC. | Cipó-cabeludo | diabetes | Infusion (I) | 10 | 1 | 1 | 0.17 |
| 13.23. Pectis jangadensis S. Moore | Erva-do-carregador | blood cleanser and diabetes | Infusion (I) | 4 | 2 | 2 | 0.33 |
| 13.24. Porophyllum ruderale (Jacq.) Cass. | Picão-branco | Hepatitis and kidneys | Infusion (I) | 11 | 2 | 2 | 0.33 |
| 13.25. Solidago microglossa DC. | Arnica-brasileira | wound healing, blood cleanser, pain, bone fractures, hypertension, uterine inflammation, muscular relaxative, kidneys, worms, pain, stomach, hypertension, pneumonia, constipation, and relaxative muscular | Infusion (I, E) | 82 | 8 | 15 | 1.80 |
| 13.26. Spilanthes acmella (L.) Murray | Jambú | liver | Infusion (I) | 5 | 1 | 1 | 0.17 |
| 13.27. Tagetes minuta L. | Cravo-de-defunto | Dengue and flu | Infusion (I) | 3 | 2 | 2 | 0.33 |
| 13.28. Taraxacum officinale L. | Dente-de-leão | blood cleanser | Infusion (I) | 18 | 1 | 1 | 0.17 |
| 13.29. Tithonia diversifolia (Hemsl.) A. Gray | Flor-da-amazônia | alcoholism, stomach, kidney, and constipation | Infusion (I) | 16 | 3 | 3 | 0.50 |
| 13.30.Vernonia condensata Baker | Figatil-caferana | cancer stomach and liver | Infusion (I) | 48 | 2 | 3 | 0.40 |
| 13.31. Vernonia scabra Pers. | Assa-peixe | bronchitis blood cleanser, fever, flu, pneumonia, cold, and cough | Infusion and syrup (I) | 38 | 2 | 7 | 0.67 |
| 13.32. Zinnia elegans Jacq. | Jacinta | pain | Infusion (I) | 1 | 1 | 1 | 0.17 |
| 14. BERBERIDACEAE | |||||||
| 14.1. Berberis laurina Billb. | Raiz-de-são-joão | blood cleanser and diarrhea | Decoction and bottle (I, E) | 6 | 2 | 2 | 0.33 |
| 15. BIGNONIACEAE | |||||||
| 15.1. Anemopaegma arvense (Vell.) Stellfeld & J.F. Souza | Verga-teso, Alecrim-do-campo, Catuaba | anxiety soothing kidneys | Decoction and bottle (I, E) | 13 | 2 | 3 | 0.40 |
| 15.2. Arrabidaea chica (Humb. & Bonpl.) B. Verl. | Crajirú | wound healing and blood cleanser | Infusion (I) | 6 | 2 | 2 | 0.33 |
| 15.3. Cybistax antisyphilitica (Mart.) Mart. | Pé-de-anta | fever, flu, relaxative muscular, and worms | Infusion (I) | 13 | 4 | 4 | 0.67 |
| 15.4. Jacaranda caroba (Vell.) A. DC. | Caroba | wound healing | Decoction and bottle (I, E) | 3 | 1 | 1 | 0.17 |
| 15.5. Jacaranda decurrens Cham. | Carobinha | allergy cancer wound healing, blood cleanser, diabetes, leprosy, hemorragia no nariz, inflammation uterina, and kidneys | Decoction and bottle (I, E) | 94 | 8 | 9 | 1.40 |
| 15.6. Tabebuia aurea (Silva Manso) B. & H. f. ex S. Moore | Ipê-amarelo | worms | Decoction and bottle (I) | 2 | 1 | 1 | 0.17 |
| 15.7. Tabebuia caraiba (Mart.) Bureau | Para-tudo | prostate cancer anemia, bronchitis cancer blood cleanser, diarrhea, pain, stomach, cough, and worms | Decoction and bottle (I, E) | 67 | 6 | 10 | 1.27 |
| 15.8. Tabebuia impetiginosa (Mart. ex DC.) Standl. | Ipê-roxo | prostate cancer cough | Decoction and bottle (I) | 8 | 2 | 2 | 0.33 |
| 15.9. Tabebuia serratifolia Nicholson | Piúva | prostate cancer | Decoction and bottle (I, E) | 3 | 1 | 1 | 0.17 |
| 15.10. Zeyhera digitalis (Vell.) Hochn. | Bolsa-de-pastor | Stomach | Decoction and bottle (I) | 9 | 1 | 1 | 0.17 |
| 16. BIXACEAE | |||||||
| 16.1. Bixa orellana L. | Urucum | cholesterol, stroke, bone fractures, and measles | Infusion (I) | 11 | 4 | 4 | 0.67 |
| 16.2. Cochlospermum regium (Schrank) Pilg. | Algodãozinho-do-campo | blood cleanser, stomach, bone fractures, inflammation uterina, syphilis, vitiligo, gonorrhea, and ringworm | Infusion (I) | 37 | 6 | 9 | 1.20 |
| 17. BOMBACACEAE | |||||||
| 17.1. Pseudobombax longiflorum (Mart. Et Zucc.) Rob. | Embiriçu-do-cerrado | pneumonia, cough, and tuberculosis | Infusion (I) | 17 | 3 | 3 | 0.50 |
| 17.2. Eriotheca candolleana (K. Schum.) | Catuaba | prostate cancer | 1 | 1 | 1 | 0.17 | |
| 18. BORAGINACEAE | |||||||
| 18.1. Cordia insignis Cham. | Calção-de-velho | cough | Infusion (I) | 5 | 1 | 1 | 0.17 |
| 18.2. Heliotropium filiforme Lehm. | Sete-sangria | thooth, blood cleanser, hypertension, and tuberculosis | Infusion (I) | 43 | 4 | 4 | 0.67 |
| 18.3. Symphytum asperrimum Donn ex Sims | Confrei | wound healing, heart, throat, and obesity | Infusion (I, E) | 10 | 4 | 4 | 0.67 |
| 19. BRASSICACEAE | |||||||
| 19.1. Nasturtium officinale R. Br. | Agrião | bronchitis | Infusion (I) | 2 | 1 | 1 | 0.17 |
| 20. BROMELIACEAE | |||||||
| 20.1. Ananas comosus (L.) Merr. | Abacaxi | diuretic and cough | Infusion (I) | 9 | 2 | 2 | 0.33 |
| 20.2. Bromelia balansae Mez | Gravatá | cough and bronhitis | Infusion (I) | 2 | 2 | 2 | 0.33 |
| 21. BURSERACEAE | |||||||
| 21.1. Commiphora myrrha (T. Nees) Engl. | Mirra | Menstruation and rheumatism | Infusion (I) | 3 | 2 | 2 | 0.33 |
| 21.2. Protium heptaphyllum (Aubl.) Marchand | Almésica | blood cleanser, stroke, pain, muscular relaxative, rheumatism, and cough | 23 | 3 | 6 | 0.70 | |
| 22. CACTACEAE | |||||||
| 22.1. Cactus alatus Sw. | Cacto | Colic and guard delivery | Infusion (I, E) | 10 | 2 | 2 | 0.33 |
| 22.2. Opuntia sp. | Palma | column | 2 | 1 | 1 | 0.17 | |
| 22.3. Pereskia aculeata Mill. | Oro-pro-nobis | anemia | Infusion (I) | 2 | 1 | 1 | 0.17 |
| 23. CAPPARACEAE | |||||||
| 23.1. Crataeva tapia L. | Cabaça | cough | Infusion (I) | 2 | 1 | 1 | 0.17 |
| 23.2. Cleome affinis DC. | Mussambé | diarrhea | 1 | 1 | 1 | 0.17 | |
| 24. CARICACEAE | |||||||
| 24.1. Carica papaya L. | Mamoeiro | worms, thooth, stomach, hepatitis, muscular relaxative, and cough | Infusion (I) | 17 | 4 | 6 | 0.80 |
| 25. CARYOCARACEAE | |||||||
| 25.1. Caryocar brasiliense A. St.-Hil. | Pequizeiro | diabetes, hypertension, labyrinthitis, and obesity | 11 | 4 | 4 | 0.67 | |
| 26. CELASTRACEAE | |||||||
| 26.1. Maytenus ilicifolia Mart.ex Reissek | Espinheira-santa | uric acid, bronchitis diarrhea, stomach, gastritis, flu, and cough | Infusion (I) | 8 | 5 | 7 | 0.97 |
| 27. CECROPIACEAE | |||||||
| 27.1. Cecropia pachystachya Trécul | Embaúba | cholesterol, blood cleanser, diabetes, pain, hypertension, leukemia, pneumonia, kidneys, and cough | Infusion (I) | 38 | 6 | 9 | 1.20 |
| 28. CLUSIACEAE | |||||||
| 28.1. Kielmeyera aff. grandiflora (Wawra) Saddi | Pau-santo | anemia | 1 | 1 | 1 | 0.17 | |
| 29. COMBRETACEAE | |||||||
| 29.1. Terminalia argentea Mart. | Pau-de-bicho | itching, diabetes, and cough | 8 | 3 | 3 | 0.50 | |
| 29.2. Terminalia catappa L. | Sete-copa | conjunctivitis | Infusion (I, E) | 2 | 1 | 1 | 0.17 |
| 30. COMMELINACEAE | |||||||
| 30.1. Commelina benghalensis L. | Capoeraba | hemorrhoids | Infusion (I) | 1 | 1 | 1 | 0.17 |
| 30.2. Commelina nudiflora L. | Erva-de-santa-luzia | wound healing and conjunctivitis | Infusion (I) | 3 | 2 | 2 | 0.33 |
| 30.3. Dichorisandra hexandra (Aubl.) Standl. | Cana-de-macaco | flu, hypertension, and kidneys | Infusion (I) | 1 | 3 | 3 | 0.50 |
| 31. CONVOLVULACEAE | |||||||
| 31.1. Cuscuta racemosa Mart. | Cipó-de-chumbo | pain | Infusion (I) | 1 | 1 | 1 | 0.17 |
| 31.2. Ipomoea batatas (L.) Lam. | Batata-doce | hearth | Infusion (I) | 1 | 1 | 1 | 0.17 |
| 31.3. Ipomoea (Desr.) Roem. & asarifolia Schult | Batatinha-do-brejo | Stomach and worms | Infusion (I) | 4 | 2 | 2 | 0.33 |
| 32. COSTACEAE | |||||||
| 32.1. Costus spicatus (Jacq.) Sw. | Caninha-do-brejo | bladder diuretic, inflammation uterina, muscular relaxative, and kidneys | Infusion (I) | 40 | 3 | 5 | 0.63 |
| 33. CRASSULACEAE | |||||||
| 33.1. Kalanchoe pinnata (Lam.) Pers. | Folha-da-fortuna | allergy, bronchitis blood cleanser, and flu | Infusion and juice (I) | 11 | 2 | 4 | 0.47 |
| 34. CUCURBITACEAE | |||||||
| 34.1. Cayaponia tayuya (Cell.) Cogn. | Raiz-de-bugre | blood cleanser, pain, and hepatitis | Infusion (I) | 17 | 2 | 3 | 0.40 |
| 34.2. Citrullus vulgaris Schrad. | Melância | bladder colic | Infusion (I) | 2 | 1 | 2 | 0.23 |
| 34.3. Cucumis anguria L. | Máxixe | anemia | Infusion (I) | 1 | 1 | 1 | 0.17 |
| 34.4. Cucumis sativus L. | Pepino | hypertension | Maceration (I) | 1 | |||
| 34.5. Cucurbita maxima Duchesne ex Lam. | Abóbora | Pain and worms | Infusion (I) | 4 | 2 | 2 | 0.33 |
| 34.6. Luffa sp | Bucha | Anemia and kidneys | Infusion (I) | 7 | 2 | 2 | 0.33 |
| 34.7. Momordica charantia L. | Melão-de-são-caetano | bronchitis dengue, stomach, fever, flu, hepatitis, swelling in pregnant woman, malaria, muscular relaxative, and worms | Infusion (I) | 50 | 6 | 10 | 1.27 |
| 34.8. Siolmatra brasiliensis (Cogn.) Baill. | Taiuá | Ulcer | Infusion (I) | 6 | 1 | 1 | 0.17 |
| 35. CYPERACEAE | |||||||
| 35.1. Bulbostylis capillaris (L.) C.B. Clarke | Barba-de-bode | diuretic, stomach, kidneys, and worms | Infusion (I) | 12 | 3 | 4 | 0.57 |
| 35.2. Cyperus rotundus L. | Tiririca | Pain | Infusion (I) | 1 | 1 | 1 | 0.17 |
| 36. DILLENIACEAE | |||||||
| 36.1. Curatella americana L. | Lixeira | wound healing, colic, diarrhea, flu, kidneys, and cough | Infusion (I, E) | 24 | 5 | 6 | 0.90 |
| 36.2. Davilla elliptica A. St.-Hil. | Lixeira-de-cipó | kidneys | 3 | 1 | 1 | 0.17 | |
| 36.3. Davilla nitida (Vahl.) Kubitzki | Lixeirinha | delivery help, liver, hernia, and kidneys | Infusion (I) | 10 | 3 | 4 | 0.57 |
| 37. DIOSCOREACEAE | |||||||
| 37.1. Dioscorea sp. | Cará-do-cerrado | boil | Infusion (I) | 25 | 1 | 1 | 0.17 |
| 37.2. Dioscorea trifida L | Cará | blood cleanser | Infusion (I) | 6 | 1 | 1 | 0.17 |
| 38. EBENACEAE | |||||||
| 38.1. Diospyros hispida A. DC. | Olho-de-boi | Pain and leprosy | Infusion (I) | 5 | 2 | 2 | 0.33 |
| 39. EQUISETACAE | |||||||
| 39.1. Equisetum arvense L. | Cavalinha | gastritis and kidneys | Infusion (I) | 8 | 2 | 2 | 0.33 |
| 40. ERYTHROXYLACEAE | |||||||
| 40.1 Erythroxylum aff. Daphnites Mart. | Vasoura-de-bruxa | syphilis | Infusion (I) | 1 | 1 | 1 | 0.17 |
| 41. EUPHORBIACEAE | |||||||
| 41.1. Croton antisyphiliticus Mart. | Curraleira | Hypertension and uterine inflammation | Infusion (I) | 6 | 2 | 2 | 0.33 |
| 41.2. Croton sp. | Curraleira-branca | uterine inflammation | Infusion (I) | 3 | 1 | 1 | 0.17 |
| 41.3. Croton urucurana Baill. | Sangra-d'água | cancer prostate cancer healing, diabetes, stomach, gastritis, uterine inflammation, kidneys, and ulcer | Maceration (I) | 37 | 5 | 9 | 1.10 |
| 41.4. Euphorbia aff. Thymifolia L. | Trinca-pedra | kidneys | Infusion (I) | 3 | 1 | 1 | 0.17 |
| 41.5. Euphorbia prostrata Aiton | Fura-pedra | kidneys | Infusion (I) | 4 | 1 | 1 | 0.17 |
| 41.6. Euphorbia tirucalli L | Aveloz | cancer uterine inflammation | Maceration (I) | 3 | 2 | 2 | 0.33 |
| 41.7. Jatropha sp. | Capa-rosa | diabetes | Infusion (I) | 10 | 1 | 1 | 0.17 |
| 41.8. Jatropha elliptica (Poh) Oken | Purga-de-lagarto | allergy | Infusion (I) | 38 | 1 | 1 | 0.17 |
| 41.9. Jatropha aff. Gossypiifolia L. | Pinhão-roxo | wound healing, prostrate cancer, itching, blood cleanser, stroke, snakebite, syphilis, worms, and vitiligo | Maceration(I, E) | 7 | 6 | 10 | 1.27 |
| 41.10. Jatropha urens L. | Cansansão | diabetes | Maceration (I, E) | 6 | 1 | 1 | 0.17 |
| 41.11. Manihot esculenta Crantz | Mandioca-braba | itching | Maceration (I, E) | 2 | 1 | 1 | 0.17 |
| 41.12. Manihot utilissima Pohl. | Mandioca | itching | Maceration (I, E) | 7 | 1 | 1 | 0.17 |
| 41.13. Ricinus communis L. | Mamona | wound healing and blood cleanser | Maceration (I, E) | 8 | 2 | 2 | 0.33 |
| 41.14. Synadenium grantii Hook. f. | Cancerosa | gastritis, prostate cancer stomach, and pneumonia | Maceration (I, E) | 12 | 3 | 4 | 0.57 |
| 42. FABACEAE | |||||||
| 42.1. Acosmium dasycarpum (Volgel) Yakovlev | Cinco-folha | column, blood cleanser, pain, and kidneys | Infusion (I) | 19 | 2 | 4 | 0.47 |
| 42.2. Acosmium subelegans (Mohlenbr.) Yakovlev | Quina-gensiana | wound healing, blood cleanser, pain, liver, uterine inflammation, delivery relapse, and kidneys | Decoction (I) | 16 | 5 | 7 | 0.97 |
| 42.3. Albizia niopoides (Spr. ex Benth.) Burkart. | Angico-branco | bronhitis | Decoction (I) | 1 | 1 | 1 | 0.17 |
| 42.4. Amburana cearensis (Allemão) A. C. Sm. | Imburana | cough | Decoction (I) | 13 | 1 | 1 | 0.17 |
| 42.5. Anadenanthera colubrina (Vell.) Brenan | Angico | asthma, wound healing, expectorant, uterine inflammation, pneumonia, and cough | Decoction (I) | 12 | 5 | 6 | 0.90 |
| 42.6. Andira anthelminthica Benth. | Angelim | diabetes | Decoction (I) | 3 | 1 | 1 | 0.17 |
| 42.7. Bauhinia variegata L. | Unha-de-boi | kidneys | Decoction (I) | 4 | 1 | 1 | 0.17 |
| 42.8. Bauhinia ungulata L. | Pata-de-vaca | diabetes | Infusion (I) | 11 | 1 | 1 | 0.17 |
| 42.9. Bauhinia glabra Jacq. | Cipó-tripa-de-galinha | diarrhea, dysentery, and pain | Infusion (I) | 7 | 3 | 3 | 0.50 |
| 42.10. Bauhinia rubiginosa Bong. | Tripa-de-galinha | kidneys | Infusion (I) | 2 | 1 | 1 | 0.17 |
| 42.11. Bauhinia rufa (Bong.) Steud. | Pata-de-boi | diabetes | Infusion (I) | 1 | 1 | 1 | 0.17 |
| 42.12. Bowdichia virgilioides Kunth | Sucupira | blood cleanser, paom, stomach, nose bleeding, cough, and worms | Bottle (I) | 20 | 4 | 6 | 0.80 |
| 42.13. Caesalpinia ferrea Mart. | Jucá | wound healing, stomach, bone fractures, and inflammation of uterine | Maceration (I, E) | 15 | 3 | 4 | 0.57 |
| 42.14. Cajanus bicolor DC. | Feijão-andu | diarrhea, stomach and worms | Infusion (I) | 8 | 2 | 3 | 0.40 |
| 42.15. Cassia desvauxii Collad. | Sene | constipation, pain, fever, uterine inflammation, and labyrinthitis | Infusion (I) | 18 | 4 | 5 | 0.73 |
| 42.16. Chamaecrista desvauxii (Collad.) Killip | Sene-do-campo | constipation, blood cleanser, pain, and fever | Infusion (I) | 10 | 2 | 4 | 0.47 |
| 42.17. Copaifera sp. | Pau-d'óleo | wound healing, kidneys, ulcer | Infusion (I) | 8 | 3 | 3 | 0.50 |
| 42.18. Copaifera langsdorffii var. glabra (Vogel) Benth. | Copaiba | bronchitis prostate cancer stroke, pain, throat, and tuberculosis | Maceration and syrup (I) | 13 | 5 | 6 | 0.90 |
| 42.19. Copaifera marginata Benth. | Guaranazinho | ulcer | Infusion (I) | 4 | 1 | 1 | 0.17 |
| 42.20. Desmodium incanum DC. | Carrapicho | bladder itching, diarrhea, pain, hepatitis, and kidneys | Infusion (I) | 18 | 5 | 6 | 0.90 |
| 42.21. Dimorphandra mollis Benth. | Fava-de-santo-inácio | bronchitis wound healing, pain, flu, hypertension, pneumonia, rheumatism, cough, and worms | Infusion (I) | 21 | 6 | 9 | 1.20 |
| 42.22. Dioclea latifolia Benth. | Fruta-olho-de-boi | stroke | Infusion (I) | 3 | 1 | 1 | 0.17 |
| 42.23. Dioclea violacea Mart. Zucc. | Coronha-de-boi | osteoporosis | Infusion (I) | 6 | 2 | 2 | 0.33 |
| stroke | |||||||
| 42.24. Dipteryx alata Vogel | Cumbarú | bronchitis cicartrizante, diarrhea, dysentery, pain, throat, flu, snakebite, and cough | Infusion (I) | 43 | 4 | 9 | 1.00 |
| 42.25. Galactia glaucescens Kunth | Três-folhas | column, pain, bone fractures, and kidneys | Infusion (I) | 8 | 4 | 4 | 0.67 |
| 42.26. Hymenaea courbaril L. | Jatobá-mirim | bladder bronchitis flu, pneumonia, and cough | Syrup and decoction (I) | 36 | 3 | 5 | 0.63 |
| 42.27. Hymenaea stigonocarpa Mart. ex Hayne | Jatoba-do-cerrado | bronchitis prostate cancer pain, fertilizer, flu, and cough | Syrup and decoction (I) | 31 | 5 | 6 | 0.90 |
| 42.28. Indigofera suffruticosa Mill. | Anil | ulcer | Infusion (I) | 2 | 1 | 1 | 0.17 |
| 42.29. Inga vera Willd. | Ingá | Laxative and kidneys | Infusion (I) | 5 | 2 | 2 | 0.33 |
| 42.30. Machaerium hirtum (Vell.) Stellfeld | Espinheira-santa-nativa | ulcer | Infusion (I) | 2 | 1 | 1 | 0.17 |
| 42.31. Melilotus officinalis (L) Pall. | Trevo-cheiroso | bone fractures and thyroid | Infusion (I) | 5 | 2 | 2 | 0.33 |
| 42.32. Mimosa debilis var. vestita (Benth.) Barneby | Dorme-dorme | soothing | Infusion (I) | 2 | 1 | 1 | 0.17 |
| 42.33. Mucuna pruriens (L.) DC. | Macuna | stroke | Infusion (I) | 2 | 1 | 1 | 0.17 |
| 42.34. Peltophorum dubium (Spreng.) Taub. | Cana-fistula | gastritis | Infusion (I) | 5 | 1 | 1 | 0.17 |
| 42.35. Platycyamus regnellii Benth. | Pau-porrete | anemia | Infusion (I) | 1 | 1 | 1 | 0.17 |
| 42.36. Pterodon pubescens (Benth.) Benth. | Sucupira-branca | worms, pain, and stomach | SYRope, decoction and maceration (I) | 2 | 3 | 3 | 0.50 |
| 42.37. Senna alata (L.) Roxb. | Mata-pasto | throat, worms, and vitiligo | Infusion (I) | 6 | 3 | 3 | 0.50 |
| 42.38. Senna occidentalis (L.) Link | Fedegoso | blood cleanser, pain, flu, cough, and worms | Infusion (I) | 42 | 3 | 5 | 0.63 |
| 42.39. Stryphnodendron obovatum Benth. | Barbatimão 1 | wound healing | Syrup and decoction (I, E) | 57 | 1 | 1 | 0.17 |
| 42.40. Stryphnodendron adstringens (Mart.) Coville | Barbatimão 2 | bladder bronchitis, colic, stomach, bone fractures, uterine inflammation, relaxative muscular, and ulcer | Syrup and decoction (I, E) | 15 | 4 | 9 | 1.00 |
| 42.41. Tamarindus indica L. | Tamarindo | anxiety pain, thooth, laxative, osteoporosis, syphilis, and worms | Maceration and juice (I) | 30 | 6 | 7 | 1.07 |
| 43. FLACOURTIACEAE | |||||||
| 43.1. Casearia silvestris Sw. | Guaçatonga | Epilepsy and kidneys | Infusion (I) | 3 | 2 | 2 | 0.33 |
| 44. GINKGOACEAE | |||||||
| 44.1. Ginkgo biloba L. | Ginco-biloba | vertebral | Infusion (I) | 1 | 1 | 1 | 0.17 |
| 45. HERRERIACEAE | |||||||
| 45.1. Herreria salsaparilha Mart. | Salsaparilha | column, blood cleanser, muscular relaxative, and kidneys | Infusion (I) | 12 | 3 | 4 | 0.57 |
| 46. HIPPOCRATEACEAE | |||||||
| 46.1. Salacia aff. elliptica (Mart. ex Schult.) G. Don | Saputa-do-brejo | pain | Infusion (I) | 6 | 1 | 1 | 0.17 |
| 47. IRIDACEAE | |||||||
| 47.1. Eleutherine bulbosa (Mill.) Urb. | Palmeirinha | pain, hemorrhoids, cough, and blood cleanser | Infusion (I) | 11 | 2 | 4 | 0.47 |
| 48. LAMIACEAE | |||||||
| 48.1. Hyptis cf. hirsuta Kunth | Hortelã-do-campo | diabetes, stomach, flu, cough, and worms | Infusion (I) | 23 | 5 | 5 | 0.83 |
| 48.2. Hyptis paludosa St.-Hil.ex Benht. | Alevante | cold | Infusion (I) | 4 | 1 | 1 | 0.17 |
| 48.3. Hyptis sp. | Hortelã-bravo | Diabetes and cough | Infusion (I) | 6 | 2 | 2 | 0.33 |
| 48.4. Hyptis suaveolens (L.) Poit. | Tapera-velha | pain, stomach, flu, constipation, kidneys, and worms | Infusion (I) | 42 | 5 | 6 | 0.90 |
| 48.5. Leonotis nepetifolia (L.) R. Br. | Cordão-de-são-francisco | column, hearth, blood cleanser, stomach, fever, gastritis, flu, hypertension, labyrinthitis, muscular relaxative, and kidneys | Infusion (I) | 38 | 7 | 11 | 1.43 |
| 48.6. Marsypianthes chamaedrys (Vahl) Kuntze | Alfavaca/Hortelã-do-mato | flu, hypertension, and cough | Infusion (I) | 8 | 3 | 3 | 0.50 |
| 48.7. Melissa officinalis L | Melissa | soothing | Infusion (I) | 2 | 1 | 1 | 0.17 |
| 48.8. Mentha crispa L. | Hortelã-folha-miuda | anemia, liver, cough, and worms | Infusion (I) | 16 | 4 | 4 | 0.67 |
| 48.9. Mentha pulegium L. | Poejo | bronchitis soothing fever, flu, cold, and cough | Infusion (I) | 59 | 3 | 6 | 0.70 |
| 48.10. Mentha spicata L. | Hortelã-vicki | bronchitis flu, wound healing, stomach, and worms | Infusion (I) | 24 | 4 | 5 | 0.73 |
| 48.11. Mentha x piperita L. | Hortelã-pimenta | bronchitis flu, cough and worms | Infusion (I) | 42 | 3 | 4 | 0.57 |
| 48.12. Mentha x villosa Huds. | Hortelã-rasteira | stomach, flu, cold, and worms | Infusion (I) | 86 | 3 | 4 | 0.57 |
| 48.13. Ocimum kilimandscharicum Baker ex Gürke | Alfavacaquinha | flu | Infusion (I) | 2 | 1 | 1 | 0.17 |
| 48.14. Ocimum minimum L. | Manjericão | kidneys, sinusitis, and worms | Infusion (I) | 7 | 3 | 3 | 0.50 |
| 48.15. Origanum majorana L. | Manjerona | heart | Infusion (I) | 4 | 1 | 1 | 0.17 |
| 48.16. Origanum vulgare L. | Orégano | cough | Infusion (I) | 1 | 1 | 1 | 0.17 |
| 48.17. Plectranthus amboinicus (Lour.) Spreng. | Hortelã-da-folha-gorda | bronchitis flu, uterine inflammation, and cough | Infusion and syrup (I) | 7 | 3 | 4 | 0.57 |
| 48.18. Plectranthus barbatus Andrews | Boldo-brasileiro | pain, stomach, liver, and malaise | Maceration (I) | 99 | 2 | 4 | 0.47 |
| 48.19. Plectranthus neochilus Schltr. | Boldinho | stomach | Maceration (I) | 1 | 1 | 1 | 0.17 |
| 48.20. Rosmarinus officinalis L. | Alecrim | anxiety soothing hearth, pain, hypertension, insomnia, labyrinthitis, sluggishness memory, tachycardia, and vitiligo | Infusion and maceration (I) | 31 | 6 | 10 | 1.27 |
| 49. LAURACEAE | |||||||
| 49.1. Cinnamomum camphora (L.) Nees & Eberm. | Cânfora | pain | Infusion and maceration (I) | 1 | 1 | 1 | 0.17 |
| 49.2. Cinnamomum zeylanicum Breyne | Canela-da-india | aphrodisiac, tonic, obesity, and cough | Infusion (I) | 11 | 3 | 4 | 0.57 |
| 49.3. Persea americana Mill. | Abacateiro | diuretic, hypertension, and kidneys | Infusion and maceration (I) | 31 | 3 | 3 | 0.50 |
| 50. LECYTHIDACEAE | |||||||
| 50.1. Cariniana rubra Gardner ex Miers | Jequitibá | bladder wound healing, colic, pain, uterine inflammation, rheumatism, cough, and ulcer | Infusion and maceration (I) | 49 | 5 | 8 | 1.03 |
| 51. LOGANIACEAE | |||||||
| 51.1. Strychnos pseudoquina A. St.-Hil. | Quina | anemia, wound healing, cholesterol, blood cleanser, pain, stomach, bone fractures, flu, uterine inflammation, pneumonia, muscle relaxant, cough, ulcer, and worms | Decoction and maceration (I, E) | 107 | 8 | 14 | 1.73 |
| 52. LORANTHACEAE | |||||||
| 52.1. Psittacanthus calyculatus (D.C.) G. Don | Erva-de-passarinho | stroke, pain, flu, and pneumonia | Infusion and maceration (I) | 14 | 3 | 4 | 0.57 |
| 53. LYTHRACEAE | |||||||
| 53.1. Adenaria floribunda Kunth | Veludo-vermelho | kidneys | 3 | 1 | 1 | 0.17 | |
| 53.2. Lafoensia pacari A. St.-Hil. | Mangava-braba | wound healing, diarrhea, pain, stomach, gastritis, kidneys, and ulcer | Decoction and maceration (I, E) | 73 | 5 | 7 | 0.97 |
| 54. MALPIGHIACEAE | |||||||
| 54.1. Byrsonima orbignyana A. Juss. | Angiquinho | wound healing | Decoction and maceration (I) | 2 | 1 | 1 | 0.17 |
| 54.2. Byrsonima sp. | Semaneira | pain | Infusion (I) | 1 | 1 | 1 | 0.17 |
| 54.3. Byrsonima verbascifolia (L.) DC. | Murici-do-cerrado | column | Infusion (I) | 3 | 2 | 2 | 0.33 |
| uterine inflammation | |||||||
| 54.4. Camarea ericoides A. St.-Hil. | Arniquinha | wound healing | Infusion (I) | 11 | 1 | 1 | 0.17 |
| 54.5. Galphimia brasiliensis (L.) A. Juss. | Mercúrio-do-campo | wound healing, itching, thooth, and bone fractures | Infusion (I) | 7 | 3 | 4 | 0.57 |
| 54.6. Heteropterys aphrodisiaca O. Mach. | Nó-de-cachorro | brain, wound healing, blood cleanser, impotence, muscular relaxative, and rheumatism | Decoction (I) | 23 | 5 | 6 | 0.90 |
| 54.7. Malpighia emarginata DC. | Cereja | wound healing | Infusion (I) | 5 | 1 | 1 | 0.17 |
| 54.8. Malpighia glabra L. | Aceroleira | bronchitis dengue, stomach, fever, and flu | Infusion (I) | 24 | 4 | 5 | 0.73 |
| 55. MALVACEAE | |||||||
| 55.1. Brosimum gaudichaudii Trécul | Mama-cadela | stomach | Infusion (I) | 13 | 1 | 1 | 0.17 |
| 55.2. Gossypium barbadense L. | Algodão-de-quintal | blood cleanser, stomach, vitiligo, inflammation, and gonorrhea | Infusion (I) | 47 | 5 | 5 | 0.83 |
| 55.3. Guazuma ulmifolia var. tomentosa (Kunth) K. Schum. | Chico-magro | diarrhea, kidneys, bronchitis wound healing | Infusion and decoction (I) | 10 | 4 | 4 | 0.67 |
| 55.4. Hibiscus pernambucensis Bertol. | Algodão-do-brejo | wound healing, colic, flu, and uterine inflammation | Infusion (I) | 2 | 3 | 4 | 0.57 |
| 55.5. Hibiscus rosa-sinensis L. | Primavera | pain | Infusion (I) | 2 | 1 | 1 | 0.17 |
| 55.6. Hibiscus sabdariffa L. | Quiabo-de-angola, Hibisco | anxiety hearth, flu, tachycardia, kidneys, colic, runny, diarrhea, pain, uterine inflammation, labyrinthitis, snakebite, and pneumonia | Infusion (I) | 18 | 10 | 13 | 1.87 |
| 55.7. Helicteres sacarolha A. St.-Hil. | Semente-de-macaco | Hypertension and ulcer | Infusion (I) | 2 | 2 | 2 | 0.33 |
| 55.8. Malva sylvestris L. | Malva-branca | wound healing, conjunctivitis, runny, blood cleanser, diuretic, boil, uterine inflammation, and rheumatism | Infusion (I) | 31 | 7 | 8 | 1.23 |
| 55.9. Malvastrum corchorifolium (Desr.) Britton ex Small | Malva | tonsillitis wound healing, pain, and uterine inflammation | Infusion (I) | 13 | 4 | 4 | 0.67 |
| 55.10. Sida rhombifolia L. | Guaxuma | obesity | Infusion (I) | 5 | 1 | 1 | 0.17 |
| 56. MELASTOMATACEAE | |||||||
| 56.1. Leandra purpurascens (DC.) Cogn. | Pixirica | rheumatism | Infusion (I) | 1 | 1 | 1 | 0.17 |
| 56.2. Tibouchina clavata (Pers.) Wurdack | Cibalena | pain | Infusion (I) | 3 | 1 | 1 | 0.17 |
| 56.3. Tibouchina urvilleana (DC.) Cogn. | Buscopam-de-casa | stomach | Infusion (I) | 1 | 1 | 1 | 0.17 |
| 57. MELIACEAE | |||||||
| 57.1. Azadirachta indica A. Juss. | Neem | diabetes | Infusion and decoction (I, E) | 1 | 1 | 1 | 0.17 |
| 57.2. Cedrela odorata L. | Cedro | wound healing | Infusion (I) | 3 | 1 | 1 | 0.17 |
| 58. MENISPERMACEAE | |||||||
| 58.1. Cissampelos sp. | Orelha-de-onça | Column and kidneys | Infusion (I) | 3 | 2 | 2 | 0.33 |
| 59. MORACEAE | |||||||
| 59.1. Artocarpus integrifolia L.f. | Jaca | diuretic | Infusion (I) | 1 | 1 | 1 | 0.17 |
| 59.2. Chlorophora tinctoria (L.) Gaudich. ex Benth. | Taiúva | osteoporosis and muscular relaxative | Infusion (I) | 2 | 2 | 2 | 0.33 |
| 59.3. Dorstenia brasiliensis Lam. | Carapiá | wound healing, colic, thooth, blood cleanser, dysentery, pain, flu, laxative, menstruation, pneumonia, relapse delivery, and kidneys | Infusion (I) | 41 | 7 | 12 | 0.50 |
| 59.4. Ficus brasiliensis Link. | Figo | gastritis | Infusion (I) | 4 | 1 | 1 | 0.17 |
| 59.5. Ficus pertusa L. f. | Figueirinha | stomach | Infusion (I) | 5 | 1 | 1 | 0.17 |
| 60. MUSACEAE | |||||||
| 60.1. Musa x paradisiaca L. | Bananeira-de-umbigo | bronchitis anemia and pain | Infusion and syrup (I) | 9 | 3 | 3 | 0.50 |
| 61. MYRTACEAE | |||||||
| 61.1. Eucalyptus citriodora Hook. | Eucálipto | bronchitis diabetes, fever, flu, sinusitis, and cough | Infusion and syrup (I) | 22 | 3 | 6 | 0.70 |
| 61.2. Eugenia pitanga (O. Berg) Kiaersk. | Pitanga | pain, throat, flu, and kidneys | Infusion (I) | 10 | 3 | 4 | 0.57 |
| 61.3. Psidium guajava L. | Goiabeira | diarrhea | Infusion (I) | 19 | 1 | 1 | 0.17 |
| 61.4. Psidium guineense Sw. | Goiaba-áraça | pain, diarrhea, and hypertension | Infusion (I) | 11 | 3 | 3 | 0.50 |
| 61.5. Syzygium aromaticum (L.) Merr. & L. M. Perry | Cravo-da-india | Throat and cough | Infusion (I) | 5 | 1 | 2 | 0.23 |
| 61.6. Syzygium jambolanum (Lam.) DC. | Azeitona-preta | cholesterol | Decoction (I, E) | 4 | 1 | 1 | 0.17 |
| 62. NYCTAGINACEAE | |||||||
| 62.1. Boerhavia coccinea L. | Amarra-pinto | bladder icterus, inflammation uterina, and kidneys | Infusion (I) | 22 | 2 | 4 | 0.47 |
| 62.2. Mirabilis jalapa L. | Maravilha | heart, pain, and hypertension | Infusion (I) | 8 | 2 | 3 | 0.40 |
| 63. OLACACEAE | |||||||
| 63.1. Ximenia americana L. | Limão-bravo | Trush and diuretic | Infusion (I) | 4 | 2 | 2 | 0.33 |
| 64. OPILIACEAE | |||||||
| 64.1. Agonandra brasiliensis Miers ex Benth. & Hook f. | Pau-marfim | uterine inflammation | Decoction (I, E) | 1 | 1 | 1 | 0.17 |
| 65. ORCHIDACEAE | |||||||
| 65.1. Vanilla palmarum (Salzm. ex Lindl.) Lindl. | Baunilha | hypertension | Infusion (I) | 2 | 1 | 1 | 0.17 |
| 65.2. Oncidium cebolleta (Jacq.) Sw. | Orquidea | pain | Infusion (I) | 2 | 1 | 1 | 0.17 |
| 66. OXALIDACEAE | |||||||
| 66.1. Averrhoa carambola L. | Carambola | hypertension | Infusion (I) | 8 | 1 | 1 | 0.17 |
| 66.2. Oxalis aff. hirsutissima Mart. ex Zucc. | Azedinha | obesity | Infusion (I) | 9 | 1 | 1 | 0.17 |
| 67. PAPAVERACEAE | |||||||
| 67.1. Argemone mexicana L. | Cardo-santo | hypertension | Infusion (I) | 8 | 1 | 1 | 0.17 |
| 68. PASSIFLORACEAE | |||||||
| 68.1. Passiflora alata Curtis | Maracujá | Infusion (I) | 9 | 1 | 1 | 0.17 | |
| 68.2. Passiflora cincinnata Mast. | Maracujá-do-mato | soothing hypertension | Infusion (I) | 5 | 2 | 2 | 0.33 |
| 69. PEDALIACEAE | |||||||
| 69.1 Sesamum indicum L. | Gergelim | stomach, liver, gastritis, ulcer, and worms | Infusion and maceration (I) | 12 | 2 | 5 | 0.53 |
| 70. PHYLLANTHACEAE | |||||||
| 70.1. Phyllanthus niruri L. | Quebra-pedra | kidneys | Infusion (I) | 32 | 1 | 1 | 0.17 |
| 71. PHYTOLACCACEAE | |||||||
| 71.1. Petiveria alliacea L. | Guiné | rheumatism | Infusion (I, E) | 4 | 1 | 1 | 0.17 |
| 72. PIPERACEAE | |||||||
| 72.1. Piper callosum Ruiz & Pav | Ventre-livre/elixir paregórico | kidneys | Infusion (I) | 1 | 1 | 1 | 0.17 |
| 72.2. Piper cuyabanum C. DC. | Jaborandi | pain, stomach, and loss of hair | Infusion (I, E) | 10 | 3 | 3 | 0.50 |
| 72.3. Pothomorphe umbellata (L.) Miq. | Pariparoba | blood cleanser, stomach, liver, and pneumonia | Infusion (I) | 11 | 3 | 3 | 0.50 |
| 73. PLANTAGINACEAE | |||||||
| 73.1. Plantago major L. | Tanchagem | heart, pain, and laxative | Infusion (I) | 16 | 3 | 3 | 0.50 |
| 74. POACEAE | |||||||
| 74.1. Andropogon bicornis L. | Capim-rabo-de-lobo | uterine inflammation | Infusion (I) | 3 | 1 | 1 | 0.17 |
| 74.2. Coix lacryma-jobi L. | Lácrimas-de-nossa-senhora | kidneys | Infusion (I, E) | 4 | 1 | 1 | 0.17 |
| 74.3. Cymbopogon citratus (DC.) Stapfc | Capim-cidreira | soothing blood cleanser, pain, stomach, expectorant, fever, flu, hypertension, muscular relaxative, kidneys, tachycardia, and cough | Infusion and juice (I) | 49 | 5 | 12 | 1.30 |
| 74.4. Cymbopogon nardus (L.) Rendle. | Capim-citronela | flu, cough, and tuberculosis | Infusion (E) | 11 | 2 | 2 | 0.33 |
| 74.5. Digitaria insularis (L.) Mez ex Ekman | Capim-amargoso | wound healing, stomach, bone fractures, and rheumatism | Infusion (I) | 14 | 3 | 4 | 0.57 |
| 74.6. Eleusine indica (L.) Gaertn. | Capim-pé-de-galinha | Hypertension and swelling in pregnant woman | Infusion (I) | 6 | 2 | 2 | 0.33 |
| 74.7. Imperata brasiliensis Trin. | Capim-sapé | diabetes, pain, hepatitis, kidneys, and vitiligo | Infusion (I) | 12 | 5 | 5 | 0.83 |
| 74.8. Melinis minutiflora P. Beauv. | Capim-gordura | dengue, blood cleanser, stroke, flu, kidneys, sinusitis, cough, and tumors | Infusion (I) | 31 | 7 | 8 | 1.23 |
| 74.9. Oryza sativa L. | Arroz | bladder | Infusion (I) | 1 | 1 | 1 | 0.17 |
| 74.10. Saccharum officinarum L. | Cana-de-açúcar | kidneys, anemia, and hypertension | Infusion (I) | 2 | 3 | 3 | 0.50 |
| 74.11. Zea mays L. | Milho | bladder kidneys | Infusion (I) | 3 | 2 | 2 | 0.33 |
| 75. POLYGALACEAE | |||||||
| 75.1. Polygala paniculata L. | Bengué | rheumatism | Infusion (I) | 6 | 1 | 1 | 0.17 |
| 76. POLYGONACEAE | |||||||
| 76.1. Coccoloba cujabensis Wedd. | Uveira | diuretic | Infusion (I) | 1 | 1 | 1 | 0.17 |
| 76.2. Polygonum cf. punctatum Elliott | Erva-de-bicho | wound healing, dengue, stomach, fever, flu, and hemorrhoids | Infusion (I) | 41 | 5 | 6 | 0.90 |
| 76.3. Rheum palmatum L. | Ruibarbo | blood cleanser, dysentery, pain, and snakebite | Infusion (I) | 6 | 4 | 4 | 0.67 |
| 76.4. Triplaris brasiliana Cham. | Novatero | diabetes | Infusion (I) | 1 | 1 | 1 | 0.17 |
| 77. POLYPODIACEAE | |||||||
| 77.1. Phlebodium decumanum (Willd.) J. Sm. | Rabo-de-macaco | diuretic, hepatitis, and kidneys | Infusion (I) | 9 | 2 | 3 | 0.40 |
| 77.2. Pteridium aquilinum (L.) Kuhn | Samambaia | colic, blood cleanser, and rheumatism | Infusion (I) | 8 | 3 | 3 | 0.50 |
| 77.3. Pteridium sp. | Samambaia-de-cipo | rheumatism | Infusion (I) | 1 | 1 | 1 | 0.17 |
| 78. PONTEDERIACEAE | |||||||
| 78.1. Eichhornia azurea (Sw.) Kunth | Aguapé | ulcer | Infusion (I) | 3 | 1 | 1 | 0.17 |
| 79. PORTULACACEAE | |||||||
| 79.1. Portulaca oleracea L. | Onze-horas | hypertension | Infusion (I) | 3 | 1 | 1 | 0.17 |
| 80. PROTEACEAE | |||||||
| 80.1. Roupala montana Aubl. | Carne-de-vaca | muscular relaxative | Infusion (I) | 2 | 1 | 1 | 0.17 |
| 81. PUNICACEAE | |||||||
| 81.1. Punica granatum L. | Romã | colic, diarrhea, pain, throat, inflammation uterina, and kidneys | Infusion and maceration (I, E) | 41 | 3 | 6 | 0.70 |
| 82. RHAMNACEAE | |||||||
| 82.1. Rhamnidium elaeocarpum Reissek | Cabriteiro | anemia, diarrhea, diuretic, pain, stomach, and worms | Infusion (I) | 37 | 5 | 6 | 0.90 |
| 83. ROSACEAE | |||||||
| 83.1. Rosa alba L. | Rosa-branca | wound healing, pain, and uterine inflammation | Infusion and maceration (I, E) | 6 | 3 | 3 | 0.50 |
| 83.2. Rosa graciliflora Rehder & E. H. Wilson | Rosa-amarela | pain | Infusion and maceration (I, E) | 1 | 1 | 1 | 0.17 |
| 83.3. Rubus brasiliensis Mart. | Amoreira | cholesterol, hypertension, labyrinthitis, menopause, obesity, osteoporosis, and kidneys | Infusion and tintura (I) | 38 | 6 | 7 | 1.07 |
| 84. RUBIACEAE | |||||||
| 84.1. Chiococca alba (L.) Hitchc. | Cainca | pain, flu, and rheumatism | Infusion (I) | 8 | 3 | 3 | 0.50 |
| 84.2. Cordiera edulis (Rich.) Kuntze | Marmelada | worms | Maceration and syrup (I) | 3 | 1 | 1 | 0.17 |
| 84.3. Cordiera macrophylla (K. Schum.) Kuntze | Marmelada-espinho | worms | Maceration and syrup (I) | 1 | 1 | 1 | 0.17 |
| 84.4. Cordiera sessilis (Vell.) Kuntze | Marmelada-bola | Flu and worms | Maceration and syrup (I) | 4 | 2 | 2 | 0.33 |
| 84.5. Coutarea hexandra (Jacq.) K. Schum. | Murtinha | diarrhea | Infusion (I) | 1 | 1 | 1 | 0.17 |
| 84.6. Genipa americana L. | Jenipapo | appendicitis bronchitis diabetes and kidneys | Infusion and syrup (I) | 8 | 4 | 4 | 0.67 |
| 84.7. Guettarda viburnoides Cham. & Schltdl. | Veludo-branco | blood cleanser and ulcer | Infusion (I) | 5 | 2 | 2 | 0.33 |
| 84.8. Palicourea coriacea (Cham.) K. Schum. | Douradinha-do-campo | prostate cancer hearth, blood cleanser, diuretic, flu, hypertension, insomnia, relaxative muscular, and kidneys | Infusion (I) | 62 | 7 | 9 | 1.30 |
| 84.9. Palicourea rigida Kunth | Doradão | Kidneys and cough | Infusion and decoction (I) | 5 | 2 | 2 | 0.33 |
| 84.10. Rudgea viburnoides (Cham.) Benth. | Erva-molar | column, thooth, blood cleanser, dysentery, rheumatism, and kidneys | Infusion (I) | 44 | 5 | 6 | 0.90 |
| 84.11. Tocoyena formosa (Cham. & Schltdl.) K. Schum. | Jenipapo-bravo | kidneys | Infusion (I) | 1 | 1 | 1 | 0.17 |
| 84.12. Uncaria tomentosa (Willd. ex Roem. & Schult.) DC. | Unha-de-gato | intoxication, rheumatism, and kidneys | Infusion (I) | 10 | 3 | 3 | 0.50 |
| 85. RUTACEAE | |||||||
| 85.1. Citrus aurantiifolia (Christm.) Swingle | Lima | soothing hearth, and hypertension | Infusion (I) | 8 | 2 | 3 | 0.40 |
| 85.2. Citrus limon (L.) Osbeck | Limão | colic, diabetes, pain, liver, flu, hypertension, and cough | Infusion (I) | 17 | 5 | 7 | 0.97 |
| 85.3. Citrus sinensis (L.) Osbeck | Laranja | soothing wound healing, fever, flu, pneumonia, and thyroid | Infusion (I) | 30 | 4 | 6 | 0.80 |
| 85.4. Ruta graveolens L. | Arruda | colic, conjunctivitis, pain, stomach, fever, gastritis, nausea, and laxative muscular | Infusion (I) | 57 | 4 | 8 | 0.93 |
| 85.5. Spiranthera odoratissima A.St.-Hil. | Manacá | rheumatism | Infusion (I) | 6 | 1 | 1 | 0.17 |
| 85.6. Zanthoxylum cf. rhoifolium Lam. | Mamica-de-porca | diabetes, diarrhea, hemorrhoids, and muscular relaxative | Decoction (I, E) | 12 | 4 | 4 | 0.67 |
| 86. SALICACEAE | |||||||
| 86.1. Casearia silvestris Sw. | Chá-de-frade | blood cleanser, pain, and fever | Infusion (I) | 10 | 1 | 3 | 0.30 |
| 87. SAPINDACEAE | |||||||
| 87.1. Dilodendron bipinnatum Radlk. | Mulher-pobre | bone fractures | Infusion (I) | 5 | 2 | 2 | 0.33 |
| uterine inflammation | |||||||
| 87.2. Magonia pubescens A. St.-Hil. | Timbó | wound healing, pain, and cough | Maceration (I, E) | 7 | 2 | 3 | 0.40 |
| 87.3. Serjania erecta Radk. | Cinco-pontas | column, muscular relaxative, and kidneys | Infusion (I) | 9 | 2 | 3 | 0.40 |
| 87.4. Talisia esculenta (A. St.-Hil.) Radlk. | Pitomba | column, pain, and rheumatism | Infusion (I) | 6 | 2 | 3 | 0.40 |
| 88. SAPOTACEAE | |||||||
| 88.1. Pouteria glomerata (Miq.) Radlk. | Laranjinha-do-mato | fever | Infusion (I) | 1 | 1 | 1 | 0.17 |
| 88.2. Pouteria ramiflora (Mart.) Radlk. | Fruta-de-viado | Ulcer and kidneys | Infusion (I) | 1 | 2 | 2 | 0.33 |
| 89. SCROPHULARIACEAE | |||||||
| 89.1. Bacopa sp. | Vicki-de-batata | kidneys | Infusion (I) | 2 | 1 | 1 | 0.17 |
| 89.2. Scoparia dulcis L. | Vassorinha | bladder wound healing, hearth, blood cleanser, diabetes, pain, bone fractures, swelling in pregnant woman, pneumonia, kidneys, syphilis, and cough | Infusion (I) | 81 | 7 | 12 | 1.50 |
| 90. SIMAROUBACEAE | |||||||
| 90.1. Simaba ferruginea A. St.-Hil. | Calunga | anemia, wound healing, diabetes, digestive, pain, stomach, obesity, ulcer, and worms | Maceration (I) | 31 | 7 | 9 | 1.30 |
| 90.2. Simarouba versicolor A. St.-Hil. | Pé-de-perdiz | wound healing and uterine inflammation | Decoction (I, E) | 4 | 2 | 2 | 0.33 |
| 91. SIPARUNACEAE | |||||||
| 91.1. Siparuna guianensis Aubl. | Negramina | pain, fever, and flu | Infusion (I) | 20 | 2 | 3 | 0.40 |
| 92. SMILACACEAE | |||||||
| 92.1. Smilax aff. brasiliensis Spreng. | Japecanga | Column and rheumatism | Infusion (I) | 5 | 1 | 2 | 0.23 |
| 93. SOLANACEAE | |||||||
| 93.1. Capsicum sp. | Pimenta | Pain and hemorrhoids | Infusion (I, E) | 14 | 2 | 2 | 0.33 |
| 93.2. Nicotiana tabacum L. | Fumo | thyroid | Infusion (I, E) | 2 | 1 | 1 | 0.17 |
| 93.3. Physalis sp. | Tomate-de-capote | hepatitis | Infusion (I) | 1 | 1 | 1 | 0.17 |
| 93.4. Solanum americanum Mill. | Maria-pretinha | worms | Infusion (I) | 3 | 1 | 1 | 0.17 |
| 93.5. Solanum lycocarpum A. St.-Hil. | Fruta-de-lobo | Gastritis and ulcer | Infusion and maceration (I) | 6 | 1 | 2 | 0.23 |
| 93.6. Solanum sp. | Jurubeba | column, stomach, and liver | Infusion (I) | 8 | 2 | 3 | 0.40 |
| 93.7. Solanum sp. | Urtiga | boi | Infusion (I) | 1 | 1 | 1 | 0.17 |
| 93.8. Solanum melongena L. | Berinjela | cholesterol | Infusion and maceration (I) | 2 | 1 | 1 | 0.17 |
| 93.9. Solanum tuberosum L. | Batata-inglesa | Pain and gastritis | Infusion and maceration (I, E) | 13 | 2 | 2 | 0.33 |
| 93.10. Solanum viarum Dunal. | Joá-manso | Hemorrhoids | Infusion (I) | 7 | 1 | 1 | 0.17 |
| 94. TILIACEAE | |||||||
| 94.1. Apeiba tibourbou Aubl. | Jangadeira | liver | Decoction (I, E) | 1 | 1 | 1 | 0.17 |
| 94.2. Luehea divaricata Mart. | Açoita-cavalo | uric acid, column, blood cleanser, throat, flu, hemorrhoids, intestine, pneumonia, muscular relaxative, kidneys, cough, and tumors | Decoction and syrup (I) | 58 | 7 | 12 | 1.50 |
| 95. ULMACEAE | |||||||
| 95.1. Trema micrantha (L.) Blume | Piriquiteira | wound healing | Decoction (I, E) | 1 | 1 | 1 | 0.17 |
| 96. VERBENACEAE | |||||||
| 96.1. Casselia mansoi Schau | Saúde-da-mulher | thooth, blood cleanser, uterine inflammation, and menstruation | Infusion (I) | 9 | 3 | 4 | 0.57 |
| 96.2. Duranta repens L. | Pingo-de-ouro | diabetes | Infusion (I, E) | 3 | 1 | 1 | 0.17 |
| 96.3. Lantana camara L. | Cambará | cold and cough | Decoction (I) | 22 | 2 | 2 | 0.33 |
| 96.4. Lippia alba (Mill.) N. E. Br. ex Britton & P. Wilson | Erva-cidreira | soothing hearth, thooth, blood cleanser, pain, flu, hypertension, tachycardia, and cough | Infusion (I) | 75 | 5 | 9 | 1.10 |
| 96.5. Phyla sp. | Chá-mineiro | conjunctivitis, blood cleanser, pain, fever, muscular relaxative, rheumatism, and kidneys | Infusion (I) | 19 | 4 | 7 | 0.87 |
| 96.6. Priva lappulacea (L.) Pers. | Pega-pega | Stomach and sinusitis | Infusion (I) | 2 | 2 | 2 | 0.33 |
| 96.7. Stachytarpheta aff. cayennensis (Rich.) Vahl | Gervão | bronchitis blood cleanser, stomach, liver, bone fractures, gastritis, flu, constipation, relaxative muscular, cough, and worms | Infusion (I) | 80 | 6 | 11 | 1.33 |
| 96.8. Stachytarpheta sp. | Rabo-de-pavão | relaxative muscular | Infusion (I) | 3 | 1 | 1 | 0.17 |
| 96.9. Vitex cymosa Bert.ex Spregn. | Tarumeiro | blood cleanser, diarrhea, pain, and stomach | Infusion (I) | 8 | 3 | 4 | 0.57 |
| 97. VIOLACEAE | |||||||
| 97.1. Anchietea salutaris A. St.-Hil. | Cipó-suma | column, blood cleanser, fever, intoxication, and vitiligo | Infusion (I) | 18 | 4 | 5 | 0.73 |
| 97.2. Hybanthus calceolaria (L.) Schulze-Menz. | Poaia-branca | cough | Infusion (I) | 1 | 1 | 1 | 0.17 |
| 98. VITACEAE | |||||||
| 98.1. Cissus cissyoides L. | Insulina-de-ramo | diabetes | Infusion (I) | 10 | 1 | 1 | 0.17 |
| 98.2. Cissus gongylodes Burch. ex Baker | Cipó-de-arráia | relaxative muscular | Infusion (I) | 1 | 1 | 1 | 0.17 |
| 98.3. Cissus sp. | Rabo-de-arráia | hypertension | Infusion (I) | 3 | 2 | 2 | 0.33 |
| 98.4. Cissus sp. | Sofre-do-rim-quem-quer | inflammation uterina, relaxative muscular, and kidneys | Infusion (I) | 5 | 3 | 3 | 0.50 |
| 99. VOCHYSIACEAE | |||||||
| 99.1. Callisthene fasciculata Mart. | Carvão-branco | Hepatitis and icterus | Decoction (I, E) | 10 | 2 | 2 | 0.33 |
| 99.2. Qualea grandiflora Mart. | Pau-terra | Diarrhea and pain | Decoction (I, E) | 5 | 2 | 2 | 0.33 |
| 99.3. Qualea parviflora Mart. | Pau-terrinha | diarrhea | 1 | 1 | 1 | 0.17 | |
| 99.4. Salvertia convallariodora A. St.-Hil. | Capotão | diarrhea, diuretic, hemorrhoids, and relaxative muscular | Decoction (I, E) | 4 | 4 | 4 | 0.67 |
| 99.5. Vochysia cinnamomea Pohl | Quina-doce | flu | 3 | 1 | 1 | 0.17 | |
| 99.6. Vochysia rufa Mart. | Pau-doce | blood cleanser, diabetes, diarrhea, laxative, obesity, kidneys, cough, and worms | Decoction, Infusion (I, E) | 25 | 6 | 8 | 1.13 |
| 100. LILIACEAE | |||||||
| 100.1. Aloe barbadensis Mill. | Babosa | Cancer, prostate cancer, wound healing, diabetes, stomach, bone fractures, gastritis, hepatitis, laxative, and rheumatism | Syrup and maceration (I, E) | 87 | 5 | 9 | 1.10 |
| 101. ZAMIACEAE | |||||||
| 101.1. Zamia boliviana (Brongn.) A. DC. | Maquiné | stomach | Infusion (I) | 2 | 1 | 1 | 0.17 |
| 102. ZINGIBERACEAE | |||||||
| 102.1. Alpinia speciosa (J. C. Wendl.) K. Schum. | Colônia | soothing hearth, fever, flu, and hypertension | Infusion (I) | 36 | 4 | 5 | 0.73 |
| 102.2. Curcuma longa L. | Açafrão | column, diuretic, pain, stomach, and hepatitis | Infusion and maceration (I) | 18 | 4 | 5 | 0.73 |
| 102.3. Zingiber officinale Roscoe | Gengibre | pain, flu, sinusitis, and cough | Infusion and maceration (I) | 26 | 2 | 4 | 0.47 |
I: Internal, E: External; NSC: Number of body systems treated by species; NCS: number of body systems. NP: Number of properties of the species; RI: Relative importance of the species.
3.1. Relative Importance (RI)
The RI of the species cited by 262 respondents from NSACD ranged from 0.17 to 1.87. A total of 261 species had RI ≤ 0.5; 80 species, RI from 0.51 to 1.0; 30 species, RI from 1.1 to 1.5, and 4 species with RI from 1.51 to 2.0, among the latter, three species were native to Brazil. The species with RI ≥ 1.5, were Himatanthus obovatus (Müll. Arg.) Woodson (1.87), Hibiscus sabdariffa L. (1.87), Solidago microglossa DC. (1.80), Strychnos pseudoquina A. St.-Hil. (1.73), Dorstenia brasiliensis Lam., Scoparia dulcis L., and Luehea divaricata Mart. (1.50 each), as shown in Table 4.
Table 4.
Species with the highest values of relative importance.
| Family | Species | Application/citation | RF | RI |
|---|---|---|---|---|
| Apocynaceae | Himatanthus obovatus (Müll. Arg.) Woodson | anemia (1), wound healing (7), cholesterol (3), blood cleanser (9), pain (4), nose bleeding (1), hypertension (4), uterine inflammation (5), labyrinthitis (6), muscle relaxant (2), worms (1), vitiligo (1), and pneumonia (1) | 45 | 1.87 |
| Malvaceae | Hibiscus sabdariffa L | anxiety/heart (1), flu (1), tachycardia (1), kidneys (1), cramps (3), discharge (1), diarrhea (1), pain (1), inflammation uterine (2), labyrinthitis (3), snakebite (1), and pneumonia (2) | 18 | 1.87 |
| Asteraceae | Solidago microglossa DC. | wound healing (53), blood cleanser (11), pain (2), bone fractures (1), hypertension (1), uterine inflammation (3), muscle relaxant (6), kidneys (3), and worms (2) | 82 | 1.8 |
| Loganiaceae | Strychnos pseudoquina A. St.-Hil. | anemia (46), wound healing (3), cholesterol (1), blood cleanser (16), pain (13), stomach (3), bone fractures (1), flu (2), uterine inflammation (1), pneumonia (1), muscle relaxant (1), cough (10), ulcer (1), and worms (8) | 107 | 1.73 |
| Moraceae | Dorstenia brasiliensis Lam. | wound healing (1), colic (1), tooth ache (1), blood cleanser (4), dysentery (1), pain (7), flu (2), laxative (3), menstruation (1), pneumonia (6), relapse delivery (13), and kidneys (1) | 41 | 1.5 |
| Plantaginaceae | Scoparia dulcis L. | heart (6), blood cleanser (1), diabetes (1), pain (16), bone fractures (47), swelling in pregnant woman (4), pneumonia (1), kidneys, ( 1) syphilis (3), and cough (1) | 55 | 1.5 |
| Malvaceae | Luehea divaricata Mart. | uric acid (18), vertebral column (2), blood cleanser (1), throat (1), flu (1), hemorrhoids (7), intestine (1), pneumonia (8), muscle relaxant (2), kidneys (3), cough (10), and tumors (4) | 58 | 1.5 |
RF: Relative frequency; RI: Relative importance of the species.
3.2. Informant Consensus Factor (ICF)
In the disease categories according to CID, 10th ed., we observed that ICF values ranged from 0.43 to 0.77, with the exception of disease category included in CID VI (diseases of the nervous system), which was 0.13. The ICF for CID VI ranged between 0.13 and 0.78 (mean = 0.62, SD = 0.16, 95% CI: 0.53–0.70). The highest consensus value obtained was for the category related to injuries, poisoning, and some other consequences of external causes (ICF = 0.78), with 65 species and 286 citations. Three species were more common, namely, S. dulcis and S. microglossa (“Brazilian arnica”), with 49 citations each and L. pacari (manga-brava) with 42 citations. The main ailments addressed in this category were inflammation, pain, and gastric disorders.
Out of 20 disease categories, there were citations for 18 therapeutic indications, as shown in Table 5.
Table 5.
Categories of diseases, indications, form of use, preparation and the informant consensus factor of the main medicinal plants from Nossa Senhora Aparecida do Chumbo District, Poconé, Mato Grosso, Brazil.
| Disease category/CID, 10th ed. | Medicinal plants | Main indications | Main forms of use | Part utilized/ State of the plant | Species/citations | ICF |
|---|---|---|---|---|---|---|
| Injuries, poisoning, and certain other consequences of external causes— XIX | Scoparia dulcis L. Solidago microglossa D. C Lafoensia pacari A. St.-Hil. | inflammation and pain | Inf, Dec, Mac, and Tin | L, Wp, Rt (Fr, Dr) | 65/286 | 0.78 |
| Mental and behavioural disorders —V | Chamomilla recutita (L.) Rauschert. | soothing | Dec and Inf | L (In, Sc) | 20/85 | 0.77 |
| Symptoms, signs, and abnormal clinical and laboratory findings not elsewhere classified—XVIII | Macrosiphonia longiflora (Desf.) Müll. Arg. | blood depurative | Inf, Dec, and Mac | Rz (Fr, Dr) | 176/713 | 0.75 |
| Diseases of the genitourinary system —XIV | Palicourea coriacea (Cham.) K. Schum. | Kidneys and diuretic | Inf, Dec, and Syr | L (Fr, Dr) | 132/533 | 0.75 |
| Diseases of the digestive system—XI | Plectranthus barbatus Andrews | stomach, pain, liver, and malaise | Dec, Inf, Mac, and Juc | L (Fr, Dr) | 113/428 | 0.74 |
| Other infectious and parasitic diseases—I | Chenopodium ambrosioides L. | verminose | Inf, Mac, and Juc | L (Fr,Dr) | 82/300 | 0.73 |
| Diseases of the respiratory system—X | Mentha pulegium L. | flu, bronchitis, colds, and cough | Dec, Inf, Mac, and Syr | L (Fr, Dr) | 88/303 | 0.71 |
| Pregnancy, childbirth, and the puerperium—XV | Dorstenia brasiliensis Lam. | childbirth | Dec, Inf, and Syr | Rz (Fr, Dr) | 9/28 | 0.70 |
| Diseases of the circulatory system—IX | Alpinia speciosa (J. C. Wendl.) K. Schum. | Hypertension and heart | Inf and Mac | L (Fr, Dr) | 56/180 | 0.69 |
| Some disorders originating in the perinatal period—XVI | Bidens pilosa L. | Hepatitis and enteric | Dec and Inf | L (In, Sc) | 3/7 | 0.67 |
| Diseases of blood and blood forming organs and certain disorders involving the immune system—III | Strychnos pseudoquina A. St.-Hil. | anemia | Inf, Mac, and Syr | B (Fr, Dr) | 15/38 | 0.62 |
| Diseases of the eye and the surrounding structures—VII | Malva sylvestris L. | Discharge and conjuctivitis | Inf and Tin | L (Fr, Dr) | 6/14 | 0.61 |
| Diseases of endocrine of nutritional and metabolic origins—IV | Cissus cissyoides L. | diabetes | Inf | L (Fr, Dr) | 47/109 | 0.57 |
| Diseases of the ear and mastoid process—VIII | Himatanthus obovatus (Müll. Arg.) Woodson | labyrinthitis | Inf | L (Fr, Dr) | 7/15 | 0.57 |
| Diseases of musculoskeletal and connective tissue—XIII | Solidago microglossa DC. | bone fractures | Dec, Inf, Mac, and Tin | L (Fr, Dr) | 70/146 | 0.52 |
| Diseases of the skin and subcutaneous tissue—XII | Dioscorea brasiliensis Willd. | furuncules | Dec, Inf, Mac, Tin, and Out | Rz (Fr, Dr) | 29/51 | 0.44 |
| Neoplasia (tumors)—II | Aloe barbadensis Mill. | wound healing | Dec, Inf, Mac, Tin, and Out | L (Fr, Dr) | 22/38 | 0.43 |
| Diseases of the nervous system—VI | Macrosiphonia longiflora (Desf.) Müll. Arg. | leakage | Inf | 14/16 | 0.13 |
CID, 10th ed. categories of diseases in chapters according to International Classification of Diseases and Related Health Problems, 10th. edition [25]; ICF: informant consesus factor; Inf: infusion, Dec: decoction, Syr: syrup, Mac: maceration, Sal: salad, Tin: tinture, Juc: juice, Out: others (compression and bath). L: leave; Wp: whole plant; Rt: root; Rz: rhizome; B: bark. State of the plant: Fr: fresh; Dr: dried.
4. Discussion
In the present study, almost all the respondents (99%) claimed to know and use medicinal plants. Surveys conducted in other countries had reported values ranging from 42% to 98% depending on the region and country of the study [25–27]. Due to the low level of knowledge of traditional medicine in national capitals, ethnobotanical surveys in many developing countries including Brazil, primarily prefer to evaluate small communities or rural hometowns, whose population having knowledge and practical experience with traditional medicine are proportionately higher (between 80 and 100%) [28–30].
The high percentage of folk knowledge of medicinal plants identified in Brazil may be due to factors such as lower influence of the contemporary urban lifestyle and the strength of cultural traditions in the rural communities [31]. In fact, with the process of industrialization and migration to the cities, a significant part of traditional culture is maintained more in the communities farther from the metropolis via oral transmission of the knowledge of CAM and family traditions. Transmission and conservation of CAM knowledge is more pronounced in Brazil due to high degree of biodiversity.
One of the most important aspects of this research is the documentation of high number of taxa (285 genera and 102 families) and species (376) mentioned by the informants as medicinal. These findings confirmed the existence of the great diversity of plants used for therapeutic purpose and preserved traditional culture, as stated by Simbo [32]. It is worth mentioning here the presence of 8 (eight) local medicinal plant expert informants/healers among the 262 respondents in this study. These local expert informants/healers account for a significant number of citations (43 to 250) in this study. In Brazil, as in other countries, rural communities have developed knowledge about the medicinal and therapeutic properties of natural resources and have contributed to the maintenance and transmission of the ethnopharmacological knowledge within the communities.
The most representative plant families are Fabaceae (10.2%), Asteraceae (7.82%), and Lamiaceae (4.89%). These results are in accordance with other ethnobotanical surveys conducted in the tropical regions [33, 34] including Brazil [7, 35]. Furthermore, the results from our study are also in conformity with the findings of the most comprehensive ethnobotanical survey conducted by V. J. Pott and A. Pott in the Brazilian Pantanal region [19].
Featuring greater potential for bioprospecting are 231 (61.6%) species indicated for the treatment of at least two diseases, and RI between 0.17 and 1.87 (mean = 0.46, SD = 0.357, 95% CI: 0.4250–0.4973). The seven species with the highest RI were H. obovatus (Müll. Arg.) Woodson (13 therapeutic indications and RI = 1.87, H. sabdariffa L. (12 therapeutic indications and RI = 1.87); S. microglossa DC. (9 therapeutic indications and RI = 1.80) S. pseudoquina A. St. - Hil. (14 therapeutic indications and RI = 1.73) and D. brasiliensis Lam., S. dulcis L., and L. divaricata Mart. (12, 10, and 12 therapeutic indications respectively with RI = 1.50) (Table 4). For the sake of brevity, we will focus most of our discussion on these seven most cited medicinal plants highlighting the most important available literature on them and including L. pacari. It should be noted that although 146 (39%) species presented RI below 0.17, with just a single indication, they cannot be considered as of lower pharmacological potential or importance, because as Albuquerque et al. [36] have noted elsewhere, these may be species of recent introduction in the culture of the community under study but might have been validated by the customary use in other social groups.
A total of 105 different folkways, including 18 disease categories, according to Brasil [24], were codified as shown in Table 5. The highest frequencies in decreasing magnitude were indications for the treatment of pain and inflammation (10.8%), kidney disease (7.6%), and wound healing (6.8%). In part, these data can be explained by the characteristics of the informants (elderly, rural activity, low level of education, and poor sanitation at home) with higher frequency of chronic, inflammatory, and infectious diseases. In addition, the search for natural treatments for infected wounds is very common in populations of agrarian labor or menial worker as stated by Akerreta et al. [37]. As ICF values were generally close to 1.0, it may be presumed that there is certain homogeneity in knowledge of medicinal plants among the population of NSACD.
4.1. Literature Survey and Discussions on the Selected Species with Higher Relative Importance
Himatanthus obovatus, var. obovatus had the highest relative importance, being cited for 13 different ailments that fall into 11 categories of CID, 10th ed. with a total of 29 citations. The most commonly mentioned of these indications for this plant were its traditional use as a blood cleansing, wound healing, and other conditions associated with infections, which seems to point to its possible antibiotic activity. Indeed, some studies have demonstrated the in vitro activity of its different extracts against promastigotes of Leishmania donovani [38]. A few others also showed experimentally its antiviral, antitumor activities, cellular proliferation activities, and inflammatory and immune response [39, 40]. On the basis of these aforementioned, it is possible that its use in the folk medicine may be related to its ability to modulate the immune system, which may enhance physiological mechanisms involved in resolving inflammation, pain, and wound healing. We did not encounter any literature pertaining to its use in anemia, nosebleeding, muscle relaxant, deworming, or vitiligo treatment. Its indications as a blood cleansing and as antihypercholesterolemic are important targets for future biomedical research.
Hibiscus sabdariffa calyces are used in many parts of the world to make cold and hot drinks as well as in folk medicine [41]. Due to its many health-enhancing benefits, extensive works have been carried to validate its traditional therapeutic claims. In fact, its medicinal importance is widely acknowledged in many traditional herbal systems [42].
The benefits associated with the use of H. sabdariffa may in part be due to its high content of beneficial phytochemical constituents. These include alkaloids, L-ascorbic acid, anisaldehyde, anthocyanin, β-carotene, β-sitosterol, citric acid, cyanidin-3-rutinoside, delphinidin, galactose, gossypetin, hibiscetin, mucopolysaccharide, pectin, protocatechuic acid, polysaccharide, quercetin, stearic acid, and flavonoids [42, 43]. Studies have highlighted the role of polyphenol acids, flavonoids, and anthocyanins that may act as antioxidants or through other mechanisms that may contribute to its cardioprotective activity [44, 45].
In additions to folkloric use of H. sabdariffa noted in this study, other previous reports have indicated its use in the treatment of liver disease, hypocholesterolemic, antispasmodic, intestinal antiseptic, sedative, and as mild laxative [42, 46]. The most extensively studied is its antihypertensive activity. This effect was confirmed in several in vitro and animal studies [47–49]. The hypotensive effect of H. sabdariffa and its constituents may be mediated, at least partially, by a cholinergic and/or histaminergic mechanism and it has been confirmed to act via inhibitiory action on angiotensin I converting enzyme, vasorelaxation [50], and diuretic action [51]. For detailed review on this aspect, see [41]. In addition to literature reports on the medicinal uses of this plant, we also report here its indications in the treatment of anxiety and labyrinthitis and as anti-snake venom. To the best of our knowledge, these indications remained to be proven experimentally.
In concordance with the traditional use of H. sabdariffa in the treatment of uterine inflammation and pain, its aqueous ethanol extract was shown experimentally to presents anti-inflammatory, uterine antispasmodic activities, and attenuation of intestinal spasm [52–54]. In addition to its confirmed pharmacological activities, its antiobese/weight-reducing [50, 55], hepatoprotective [56–58], anticancer [46, 59, 60], free-radical scavenging [61], antioxidant [42], immunomodulatory [62], lipid-lowering [43, 63] effects and attenuation of oxidants-mediated complications in diabetes [64] have been well documented. Besides, the plant extract is characterized by a very low degree of toxicity [41]. Moreover, apart from its medicinal uses, the plant seed oil was also shown to be a good source of lipidsoluble antioxidants, particularly γ-tocopherol, thus it could have important industrial applications [65].
Solidago microglossa is popularly known in Brazil as “arnica,” “arnica-do-mato,” “arnica-silvestre,” “erva-federal,” “arnica-vulgar,” “erva-lanceta,” and “rabo-de-rojão” [66]. It is usually confused with Arnica montana L., a native of the mountainous regions of Europe, due to the similarity in their medicinal flowers and having the same color (yellow), S. microglossa is not cultivated in Brazil due to it low adaptation to the tropical conditions [66]. In our study, S. microglossa was indicated for treatment of 15 different diseases corresponding to 8 classes of CID, 10th ed. and had a total of 49 citations. The key citations for this plant were its use in wound healing and blood cleansing. Other popular indications found in this study were similar to those previously reported, especially its use in the treatment of wounds, acne, bruises, and stomach-related ailments [67].
Several classes of compounds and metabolites have been isolated from S. microglossa, especially phenols, acetophenones, carotenoids, lactones (helenalin and dihydro-helenalin) [68, 69], flavonoids [70, 71] saponins [72], and polyacetylenes [70]. The cicatrizant activity of the plant's extract has been confirmed experimentally [73]. Although not mentioned directly by respondents in this study, some lines of evidence suggest important antibiotic activity with the use of S. microglossa, which can justify its indication for uterine inflammation. Morel et al. [74] showed that the essential oil of S. microglossa and three of its components (quercetrin, α-espinasterol, and solidagenone) are capable of significantly inhibiting the growth of Staphylococcus aureus, Staphylococcus epidermidis, Klebsiella pneumoniae, Escherichia coli, Salmonella setubal, Bacillus subtilis, Pseudomonas aeruginosa, Saccharomyces cerevisiae, and Candida albicans [74]. In addition, cicatrizant activity was observed with the administration of the plant's extract [73]. Its use in ameliorating renal ailments, blood cleansing, and hypotensive and antiparasitic activities may be associated with the presence in high concentrations of tannins [75, 76] and flavonoids in this species [76–79]. Its indication for muscle relaxation may also derive from its antispasmodic effect [80]. Further studies are warranted in these regards.
Other pharmacological properties not mentioned here, but have been established in preclinical studies, include hypoglycemic effect [81] and antitumor activity. In fact, the latter effect has attracted intense interest in the discovery of new chemotherapeutic agents. The extract of S. microglossa demonstrated antiproliferative effect (but not mutagenic) against young shoot cells of onion (Allium cepa) strain [82]. Some of these activities may be related to the presence of secondary metabolites such as helenalin [83].
Although Strychnos pseudoquina is referred to locally as “quinas”, similar to the local name used for species such as Cinchona sp. (source of quinine), it has been shown to be inactive against Plasmodium berghei [84] contrary to its popular use in folk medicine elsewhere [84]. Theoretically, some of the indications may result from the classification bias in the community due to an erroneous popular cultural belief that plants referred to as “quinas” are useful for “anemic” patients infected with malaria parasite. This perhaps helps to explain why the highest indication for this plant in our study was to treat anemia.
Among the components isolated from S. pseudoquina metabolites are isoramnetin, strychnobiflavone, and 11-diaboline metoxidiaboline [85]. Silva et al. [86] demonstrated the gastroprotective effect of S. pseudoquina in models of gastric lesions induced by nonsteroidal anti-inflammatory agents and some necrotizing agents, thus confirming its indication for gastric ulcer and stomach disorders as noted in this present study. On the other hand, its indication in wound healing has not been experimentally confirmed at least in the diabetic wound model in rats [87] or in local hemorrhage induced by Bothrops jararaca venom [88]. Other medicinal uses indicated like “blood depurative” and analgesic effect may be subject of future investigation as a potential agent with antinociceptive and metabolic disorders ameliorating effects. Regarding its toxicity, Santos et al. [81] showed that only the methanol extract (but not dichloromethane) from the leaves of S. pseudoquina have mutagenic effect in Salmonella strains TA98 (−S9) and TA100 (+ S9, −S9) and that it induces formation of micronuclei after acute treatment [81].
Dorstenia brasiliensis, known as “Carapiá” is a perennial herb of the early geological point of view, typical of the fields in southern Brazil, Paraguay, Uruguay, and Argentina [89, 90]. Phytochemical analysis of roots of D. brasiliensis indicated the presence of dorstenic acid A and B (triterpenoids), isopimarane-type diterpenoid, and six different types of coumarins. The two triterpenoids showed moderate cytotoxicity against leukemia cells (L-1210 and HL-60) [91]. Furthermore, some authors have suggested that its use in cutaneow disease (such as psoriases and vitiligo) may be associated with the presence of furanocoumarins in the species of Dorstenia [92]. Bartericin A and B, stigmasterol, isobavachalcone, 4-hydroxylonchocarpin, dorsmanin F, 6,8-diprenyleridictyol, quercetin, quercitrin, amentoflavone [93], psoralen, bergapten (from rhizome), and umbelliferone [94] are some of the compounds isolated this medicinal plant.
Some few pharmacological studies have demonstrated analgesic and anti-inflammatory activities of D. brasiliensis in animal models [95]. These data corroborated the popular use of D. brasiliensis as an analgesic. There is dearth of information confirming its use in the popular medicine use as an anti-inflammatory agent. Moreover, D. brasiliensis may possesses some biologically active compounds similar to other Dorstenia species from the same genus and may thus share similar pharmacological profile. The following compounds and pharmacological activities have been reported in other Dorstenia species: chalcones (D. prorepens and D. zenkeri) [96], furocoumarins (D. bahiensis and D. bryoniifolia), triterpenes (D. bahiensis, D. bryoniifolia, D. carauntae, D. cayapiaa, and D. heringerii) [97]. This is a point to be noted for future research. Some authors have investigated its potential use as antivenom, antiinfective, anti-rheumatic [96, 97] while others established its antitrichomonal [93], antitussive [98], antioxidant [93, 99] and antileishmanial [100] activities.
Scoparia dulcis, popularly known as “vassourinha”, grows wild in backyards, gardens, and fields in Brazil. Phytochemical studies have identified the presence of more than 12 interesting pharmacologically active compounds in this species, namely, scoparic acid A [101], iso-dulcinol, 4-epi-scopadulcic acid B, dulcidiol, scopanolal, dulcinol/scopadulciol, scopadiol [102], scoparinol [103], scopadulcic acid B [104–106], glutinol [107] and scopadulin [105]. Scopadulcic acid B inhibited the effects of tumor promoter 12-O-tetradecanoylphorbol-13-acetate (TPA) in vitro and in vivo, and also suppressed the promoting effect of TPA on skin tumor formation, demonstrating stronger effect than antitumor-promoting terpenoids, such as glycyrrhetinic acid [104]. In fact, its cytotoxicity has been investigated against antitumor activity [102] and nerve growth factor-mediated neurite outgrowth and neurodegenerative disorders [103, 108].
The analgesic and anti-inflammatory activities of ethanol extracts of S. dulcis and glutinol have been demonstrated in writhing induced by acetic acid and carrageenan-induced paw edema, respectively [107]. However, S. dulcis extracts were ineffective in the central pain models (tail flick) and paw edema induced by dextran. Another secondary metabolite, scoparinol, also showed significant analgesic and anti-inflammatory activity [109]. In regard to its toxicological effects, it is worthwhile to mention that glutinol and scoparinol markedly potentiated pentobarbital-induced sedation and duration of sleeping time in these two studies mentioned above.
In contrast to its toxicity, S. dulcis seems to possess potential hepatoprotective activity in different models, which have been attributed to its free-radical scavenging potential activities [110–113]. Corroborating with antibiotic use for some infections (like gonorrhea), some authors have investigated inhibition of multidrug resistance (MDR) bacteria, fungi [114, 115], leishmanial parasite [116], and herpes simplex virus type 1 growths [96].
Paradoxically, despite the low citation in gastric ulcer and diabetes treatments in this study, the antiulcer and antihyperglycemic activities of this species are well documented. Inhibitory activities of S. dulcis extracts was demonstrated in pylorus ligature model, histamine- or bethanechol-stimulated gastric secretion, and acute gastric lesions induced by indomethacin [117, 118]. S. dulcis was also demonstrated to inhibit both proton pump (H+, K+-ATPase) and proton transport into gastric vesicles [105]. In regard to its antihyperglycemic effect, experimental evidences demonstrated that S. dulcis extracts reduced blood glucose, glycosylated haemoglobin, prevented decrease in the body weight, and improved glucose tolerance similarly with glibenclamide [119]. Even in the insulin resistance stage, S. dulcis-treated L6 myotubes were found to be more capable of stimulating glucose transport than insulin treatment [120]. In addition, scoparic acid D was able to stimulate insulin secretion and receptor binding in streptozotoci- (STZ-) induced diabetic rats [121].
Luehea divaricata is a native tree of the Brazilian Cerrado popularly known as “açoita-cavalo”. Just as popularly indicated, some studies have reported the following pharmacological activities of L. divaricata: the leaves as used as diuretic, the stems as anti-inflammatory, the bark and aerial parts are used for healing skin wounds, pimples, and for vaginal washes [122, 123].
Phytochemical screening of L. divaricata reported the presence of flavonoids, tannins and saponins and afforded the presence of 3b-p-hydroxybenzoyl-tormentic acid [124], maslinic acid [122], vitexin and glucopyranosylsitosterol, and (−)-epicatechin [123].
The presence of flavonoids and metabolites such as the vitexin [125, 126] and maslinic acid [127, 128] may be associated with the popular indication of its anti-inflammatory properties formation of urate (18) and antitumor (4). Extracts of L. divaricata has been shown to have antioxidant activity and analgesic property [129], lack toxicity in vivo [130], or mutagenicity [131]. Its extract also showed cytotoxicity against tumor cell lines [123]. Due to the high level of citation for the treatment of urate aleviation (18), we believe that its antigout or uricosuric activity may be an important target of pharmacological interest. Another indication prominently cited by the respondents is the use of L. divaricata in the treatment of lung diseases and upper airway. However, there is no scientific evidence on its regulatory activity on cough, while its antibiotic properties also vary. Some authors have demonstrated its inhibitory effect on the growth of dermatophytes [132] but not in other fungi species [123, 129]. In addition, the extract of L. divaricata was shown to strongly inhibit the growth of S. aureus, S. epidermitis, K. pneumonia, and E. coli in a study [129] but showed only moderately in another study elsewhere [123].
It is worth mentioning that although Lafoensia pacari A.St.-Hil. had low relative importance value, all the same, it is among the three plants with the highest informant consesus factor in addition to being a native plant in the region. The other two (S. dulcis and S. microglossa) have been discussed previously.
L. pacari popularly called “mangava-brava”, belongs to the family Lythraceae, is a tree native to the Brazilian Cerrado [133]. It is commonly used for gastrointestinal disorders, wound healing, diarrhea, and kidney problems. In our study, it was referenced for the treatment of seven disorders distributed into five classes of CID, 10th ed. Preliminary phytochemical studies of methanol extract of the stem bark of L. pacari revealed the presence of free steroids, saponins, tannins catechins, pyrogalic tannins (in particular, ellagic acid), triterpenoids, simple phenols, strong and weak fixed acids, alkali, and quaternary amino acids [134–136]. Acute toxicity studies or subchronic oral administration of extracts of L. pacari did not indicate any harmful effects [137]. However, it is also indicated for its adverse reactions and used as an abortifacient, diarrheic, weight loss, and tachycardia. Among the 42 citations for L. pacari, 29 were for the treatment of ulcer, and four and two for gastritis and stomach, respectively. These indications have been confirmed with the use of methanol crude extract of L. pacari and its major active components, ellagic acid, in different experimental ulcer models [138–143]. In addition, the antiulcer activity of the methanol extract (capsules) of L. pacari was confirmed in the clinical trial with 55 patients with dyspepsia [144].
We did not encounter any studies concerning its activities in wound healing, antidiarrheal or alleviation of kidney disorders. This phenomenon of plant selection by local people for certain indications may be, for instance, to consolidate best practice of the medicinal properties of the plants at the expense of using other plants substitute for these indications. In fact, the broad community access to Amazon or Pantanal biome, and the close relationship with the indigenous native populations, promotes a variety of possibilities of ethnobotanical indications. Examples of other popular uses of L. pacari that have been experimentally confirmed includes weight loss [145], anorectic effect [142], antipyretic activity [146], anti-inflammatory [147], antiallergic [148], and analgesic property [149].
It is also worth mentioning other studies focused on the medicinal uses of L. pacari, including its potent antifungal activity [150], have demonstrated that the main compound responsible is found in the methanol extract of this plant. A patent application of lotion with the infusion prepared from the leaves of L. pacari, as a component of the formulation was also solicited [151]. To the best of our knowledge, there is currently no available literature concerning its claims as wound healing, antidiarrheal, or in kidney disorders.
5. Conclusions
The present study identified the several plant species and their medicinal uses in NSACD highlighting significant cultural diversity in the Pantanal region. In fact, one of the important components of this community is the contribution of Amerindian culture, which highlights its importance in the identification of indigenous popular knowledge relevance in the identification of native popular knowledge.
Analytically, the data were categorized according to the highest values of relative importance and consensus among informants, ensuring the best evidence for ethnobotanical bioprospecting of medicinal plants. Thus, we identified seven native species with the highest relative importance, which are H. obovatus, H. sabdariffa, S. microglossa, S. pseudoquina and D.brasiliensis, S. dulcis, and L. divaricata including L. pacari. The three plants with the highest value of consensus among informants were S. dulcis, S. microglossa, and L. pacari.
The preservation of local culture, the practice of traditional medicinal plant species themselves represent important strategies for sustenance of popular knowledge of CAM in the local systems of health care and environmental education. Moreover, ethnobotanical and pharmacological studies provide information essential for guidance in bioprospecting for new drugs of plant origin in the consolidation of therapeutic practices of the community.
Acknowledgments
The authors thank all the informants and staffs of Family Health Programme of NSACD, for the assistance and contributions made throughout ethnobotanical fieldwork, FAPEMAT and CNPq for granting scholarships, researcher, Dr. Rosilene Rodrigues Silva, UFMT Herbarium and Vali Joana Pott (MSc.) of CGMS Herbarium of Federal University of Mato Grosso do Sul, Campo Grande, for technical assistance in identification of plant species, National Institute for Science and Technology in Wetlands (INAU), National Council for Scientific and Technological Development CNPq/MCT, and Pantanal Research Center (CPP) for funding the research work.
References
- 1.OMS. Organización Mundial DE La Salud. Estrategia de la OMS sobre medicina tradicional 2002–2005. Geneva, Switzerland: OMS; 2002. [Google Scholar]
- 2.Brasil. Ministério da Saúde. Portaria nº 971. Aprova a Política Nacional de Práticas Integrativas e Complementares no SUS. Diário Oficial [da] República Federativa do Brasil, Poder Executivo, Brasília, DF, 2006.
- 3.Cakilcioglu U, Turkoglu I. An ethnobotanical survey of medicinal plants in Sivrice. Journal of Ethnopharmacology. 2010;132(1):165–175. doi: 10.1016/j.jep.2010.08.017. [DOI] [PubMed] [Google Scholar]
- 4.Brasil. Flora, vegetação, etnobotânica-conservação de recursos vegetais no pantanal. Cuiabá, 2006.
- 5.Mato Grosso. Plano plurianual 2004–2007 do Governo do Estado. Projeto de lei. Seplan, MT. 2005.
- 6.Amorozo MCM. Uso e diversidade de plantas medicinais em Santo Antônio do Leverger, MT. Acta Botanica Brasílica. 2002;16(2):189–203. [Google Scholar]
- 7.Guarim Neto G. O saber tradicional pantaneiro: as plantas medicinais e a Educação Ambiental. REMEA. Julho a dezembro, FURG/PPGEA. 2006.
- 8.Diegues ACD. O Mito Moderno da Natureza Intocada. São Paulo, Brazil: Hucitec; 1998. [Google Scholar]
- 9.Poconé. Plano Municipal de Saúde de Poconé. Prefeitura Muncipal de Poconé. Secretaria municipal de Saúde. Poconé – MT, 2010.
- 10.Scheaffer RL, Mendnhall W, Ott L. Elementos de Muestreo. México: Editora Iberoamericana; 1987. [Google Scholar]
- 11.Bolfarine H, Bussab WO. Elementos de amostragem. São Paulo, Brazil: Edgar Blucher; 2005. [Google Scholar]
- 12.Brasil. Ministério do Desenvolvimento, Indústria e Comércio. Sistema Aliceweb: informações sobre o comércio exterior brasileiro. Brasília, 2007.
- 13.Levy PS, Lemeshow S. Sampling of populations. Methods and Applications. New York, NY, USA: John Wiley & Sons; 2008. [Google Scholar]
- 14.Pio Correa M. Dicionário das plantas úteis do Brasil e das exóticas cultivadas. Instituto Brasileiro de Desenvolvimento Florestal, IBDF, Rio de Janeiro, 6 v.il. 1926–1969.
- 15.Diegues AC. Etnoconservação na natureza: enfoques alternativos. In: Diegues AC, editor. Etnoconservação, novos rumos para a conservação da natureza nos trópicos. São Paulo, Brazil: Hucitec Nupaub-USP; 2000. pp. 1–46. [Google Scholar]
- 16.Borba AM, Macedo M. Medicinal plants used for oral health in the Santa Cruz neighborhood, Chapada dos Guimarães, Mato Grosso State, Brazil. Acta Botanica Brasilica. 2006;20(4):771–782. [Google Scholar]
- 17.Pasa MC, Soares JJ, Guarim Neto G. Estudo etnobotânico na comunidade de Conceição-Açu (alto da bacia do rio Aricá Açu, MT, Brasil) Acta Botanica Brasilica. 2004;19(2):195–207. [Google Scholar]
- 18.De La Cruz MG. Plantas Medicinais de Mato Grosso-A Farmacopéia Popular dos Raizeiros. Ed. Carlini e Caniato Editorial; 2008. [Google Scholar]
- 19.Pott VJ, Pott A. Plantas do Pantanal. Brasília, Brazil: EMBRAPA-CPAP; 1994. [Google Scholar]
- 20.Cronquist A. The evolution classification of flowering plants. 2nd edition. New York, NY, USA: The New York Botanical Garden; 1988. [Google Scholar]
- 21.Missouri Botanical Garden - MOBOT. April 2010, http://www.tropicos.org/
- 22.Bennett BC, Prance GT. Introduced plants in the indigenous pharmacopoeia of northern South America. Economic Botany. 2000;54(1):90–102. [Google Scholar]
- 23.de Oliveira GL, de Oliveira AFM, Andrade LHC. Medicinal plants used in the urban community of Muribeca, Northeast Brazil. Acta Botanica Brasilica. 2010;24(2):571–577. [Google Scholar]
- 24.Brasil. Classificação Internacional de Doenças e de Problemas Relacionados a Saúde. Décima Revisão – CID-10, DATASUS. 2008.
- 25.Eisenberg DM, Davis RB, Ettner SL, et al. Trends in alternative medicine use in the United States, 1990–1997: results of a follow-up national survey. Journal of the American Medical Association. 1998;280(18):1569–1575. doi: 10.1001/jama.280.18.1569. [DOI] [PubMed] [Google Scholar]
- 26.Taddei-Bringas GA, Santillana-Macedo MA, Romero-Cancio JA, Romero-Téllez MB. Acceptance and use of therapeutic medical plants in family medical care. Salud Publica de Mexico. 1999;41(3):216–220. [PubMed] [Google Scholar]
- 27.Bekalo TH, Woodmatas SD, Woldemariam ZA. An ethnobotanical study of medicinal plants used by local people in the lowlands of Konta Special Woreda, southern nations, nationalities and peoples regional state, Ethiopia. Journal of Ethnobiology and Ethnomedicine. 2009;5, article no. 26 doi: 10.1186/1746-4269-5-26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Bieski IGC. Plantas Medicinais e Aromáticas no Sistema Único de Saúde da Região Sul de Cuiabá-MT. Lavras Minas Gerais – Brazil: Secretaria Municipal de Saúde de Cuiabá-MT; 2005. [Google Scholar]
- 29.Vendruscolo GS, Mentz LA. Study of use citations agreement and importance of medicinal used species and families to the community of Ponta Grossa neighborhood, Porto Alegre, Rio Grande do Sul State, Brazil. Acta Botanica Brasilica. 2006;20(2):367–382. [Google Scholar]
- 30.Santos EB, Dantas GS, Santos HB, Melo Diniz MFF, Sampaio FC. Etnobotanical studies of medicinal plants for oral conditions in the municipality of João Pessoa, Brazil. Brazilian Journal of Pharmacognosy. 2009;19(1B):321–324. [Google Scholar]
- 31.Upadhyay B, Parveen, Dhaker AK, Kumar A. Ethnomedicinal and ethnopharmaco-statistical studies of Eastern Rajasthan, India. Journal of Ethnopharmacology. 2010;129(1):64–86. doi: 10.1016/j.jep.2010.02.026. [DOI] [PubMed] [Google Scholar]
- 32.Simbo DJ. An ethnobotanical survey of medicinal plants in Babungo, Northwest Region, Cameroon. Journal of Ethnobiology and Ethnomedicine. 2010;6, article no. 8 doi: 10.1186/1746-4269-6-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Polhill RM. Papilionoideae. In: Polhill RM, Raven PH, editors. Advances in Legume Systematics I. Royal Botanic Gardens, Kew; 1981. pp. 191–208. [Google Scholar]
- 34.Lewis G, Schrire B, MacKinder B, Lock M, editors. Legumes of the World. UK: Royal Botanical Gardens, Kew; 2005. [Google Scholar]
- 35.Pilla MAC, Amorozo MCDM, Furlan A. Acquisition and use of medicinal plants in Martim Francisco district, Mogi Mirim Municipality, São Paulo State, Brazil. Acta Botanica Brasilica. 2006;20(4):789–802. [Google Scholar]
- 36.Albuquerque UP, et al. Evaluating two quantitative ethnobotanical Techniques. Ethnobotany Research and Applications. 2006;4:051–060. [Google Scholar]
- 37.Akerreta S, Cavero RY, López V, Calvo MI. Analyzing factors that influence the folk use and phytonomy of 18 medicinal plants in Navarra. Journal of Ethnobiology and Ethnomedicine. 2007;3, article no. 16 doi: 10.1186/1746-4269-3-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.De Mesquita ML, Desrivot J, Bories C, et al. Antileishmanial and trypanocidal activity of Brazilian Cerrado plants. Memorias do Instituto Oswaldo Cruz. 2005;100(7):783–787. doi: 10.1590/s0074-02762005000700019. [DOI] [PubMed] [Google Scholar]
- 39.Tan GT, Lee S, Lee IS, et al. Natural-product inhibitors of human DNA ligase I. Biochemical Journal. 1996;314(3):993–1000. doi: 10.1042/bj3140993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Vlietinck AJ, De Bruyne T, Apers S, Pieters LA. Plant-derived leading compounds for chemotherapy of human immunodeficiency virus (HIV) infection. Planta Medica. 1998;64(2):97–109. doi: 10.1055/s-2006-957384. [DOI] [PubMed] [Google Scholar]
- 41.Ali BH, Al Wabel N, Blunden G. Phytochemical, pharmacological and toxicological aspects of Hibiscus sabdariffa L.: a review. Phytotherapy Research. 2005;19(5):369–375. doi: 10.1002/ptr.1628. [DOI] [PubMed] [Google Scholar]
- 42.Hirunpanich V, Utaipat A, Morales NP, et al. Antioxidant effects of aqueous extracts from dried calyx of hibiscus sabdariffa Linn. (roselle) in vitro using rat low-density lipoprotein (LDL) Biological and Pharmaceutical Bulletin. 2005;28(3):481–484. doi: 10.1248/bpb.28.481. [DOI] [PubMed] [Google Scholar]
- 43.Carvajal-Zarrabal O, Waliszewski SM, Barradas-Dermitz DM, et al. The consumption of Hibiscus sabdariffa dried calyx ethanolic extract reduced lipid profile in rats. Plant Foods for Human Nutrition. 2005;60(4):153–159. doi: 10.1007/s11130-005-9023-x. [DOI] [PubMed] [Google Scholar]
- 44.Crawford RS, Kirk EA, Rosenfeld ME, LeBoeuf RC, Chait A. Dietary antioxidants inhibit development of fatty streak lesions in the LDL receptor-deficient mouse. Arteriosclerosis, Thrombosis, and Vascular Biology. 1998;18(9):1506–1513. doi: 10.1161/01.atv.18.9.1506. [DOI] [PubMed] [Google Scholar]
- 45.Rimm EB, Stampfer MJ. Antioxidants for vascular disease. Medical Clinics of North America. 2000;84(1):239–249. doi: 10.1016/s0025-7125(05)70216-9. [DOI] [PubMed] [Google Scholar]
- 46.Hou DX, Tong X, Terahara N, Luo D, Fujii M. Delphinidin 3-sambubioside, a Hibiscus anthocyanin, induces apoptosis in human leukemia cells through reactive oxygen species-mediated mitochondrial pathway. Archives of Biochemistry and Biophysics. 2005;440(1):101–109. doi: 10.1016/j.abb.2005.06.002. [DOI] [PubMed] [Google Scholar]
- 47.Mojiminiyi FBO, Dikko M, Muhammad BY, et al. Antihypertensive effect of an aqueous extract of the calyx of Hibiscus sabdariffa. Fitoterapia. 2007;78(4):292–297. doi: 10.1016/j.fitote.2007.02.011. [DOI] [PubMed] [Google Scholar]
- 48.Haji Faraji M, Haji Tarkhani AH. The effect of sour tea (Hibiscus sabdariffa) on essential hypertension. Journal of Ethnopharmacology. 1999;65(3):231–236. doi: 10.1016/s0378-8741(98)00157-3. [DOI] [PubMed] [Google Scholar]
- 49.Herrera-Arellano A, Flores-Romero S, Chávez-Soto MA, Tortoriello J. Effectiveness and tolerability of a standardized extract from Hibiscus sabdariffa in patients with mild to moderate hypertension: a controlled and randomized clinical trial. Phytomedicine. 2004;11(5):375–382. doi: 10.1016/j.phymed.2004.04.001. [DOI] [PubMed] [Google Scholar]
- 50.Sarr M, Ngom S, Kane MO, et al. In vitro vasorelaxation mechanisms of bioactive compounds extracted from Hibiscus sabdariffa on rat thoracic aorta. Nutrition and Metabolism. 2009;6, article no. 45 doi: 10.1186/1743-7075-6-45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Prasongwatana V, Woottisin S, Sriboonlue P, Kukongviriyapan V. Uricosuric effect of Roselle (Hibiscus sabdariffa) in normal and renal-stone former subjects. Journal of Ethnopharmacology. 2008;117(3):491–495. doi: 10.1016/j.jep.2008.02.036. [DOI] [PubMed] [Google Scholar]
- 52.Dafallah AA, Al-Mustafa Z. Investigation of the anti-inflammatory activity of acacia nilotica and hibiscus sabdariffa. American Journal of Chinese Medicine. 1996;24(3-4):263–269. doi: 10.1142/S0192415X96000323. [DOI] [PubMed] [Google Scholar]
- 53.Beltran-Debon. The aqueous extract of Hibiscus sabdariffa calices modulates the production of monocytechemo attractant protein-1 in humans. Phytomedicine. 2010;17:186–191. doi: 10.1016/j.phymed.2009.08.006. [DOI] [PubMed] [Google Scholar]
- 54.Kao E-S, Hsu J-D, Wang C-J, Yang S-H, Cheng S-Y, Lee H-J. Polyphenols extracted from hibiscus sabdariffa L. inhibited lipopolysaccharide-induced inflammation by improving antioxidative conditions and regulating cyclooxygenase-2 expression. Bioscience, Biotechnology and Biochemistry. 2009;73(2):385–390. doi: 10.1271/bbb.80639. [DOI] [PubMed] [Google Scholar]
- 55.Carvajal-Zarrabal O, Hayward-Jones PM, Orta-Flores Z, et al. Effect of hibiscus sabdariffa L. dried calyx ethanol extract on fat absorption-excretion, and body weight implication in rats. Journal of Biomedicine and Biotechnology. 2009;2009:5 pages. doi: 10.1155/2009/394592. Article ID 394592. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Ali BH, Mousa HM, El-Mougy S. The effect of a water extract and anthocyanins of Hibiscus sabdariffa L. on paracetamol-induced hepatoxicity in rats. Phytotherapy Research. 2003;17(1):56–59. doi: 10.1002/ptr.1084. [DOI] [PubMed] [Google Scholar]
- 57.Tseng TH, Kao ES, Chu CY, Chou FP, Lin Wu HW, Wang CJ. Protective effects of dried flower extracts of Hibiscus sabdariffa L. against oxidative stress in rat primary hepatocytes. Food and Chemical Toxicology. 1997;35(12):1159–1164. doi: 10.1016/s0278-6915(97)85468-3. [DOI] [PubMed] [Google Scholar]
- 58.Liu JY, Chen CC, Wang WH, Hsu JD, Yang MY, Wang CJ. The protective effects of Hibiscus sabdariffa extract on CCl 4-induced liver fibrosis in rats. Food and Chemical Toxicology. 2006;44(3):336–343. doi: 10.1016/j.fct.2005.08.003. [DOI] [PubMed] [Google Scholar]
- 59.Chang YC, Huang HP, Hsu JD, Yang SF, Wang CJ. Hibiscus anthocyanins rich extract-induced apoptotic cell death in human promyelocytic leukemia cells. Toxicology and Applied Pharmacology. 2005;205(3):201–212. doi: 10.1016/j.taap.2004.10.014. [DOI] [PubMed] [Google Scholar]
- 60.Lin HH, Chen JH, Kuo WH, Wang CJ. Chemopreventive properties of Hibiscus sabdariffa L. on human gastric carcinoma cells through apoptosis induction and JNK/p38 MAPK signaling activation. Chemico-Biological Interactions. 2007;165(1):59–75. doi: 10.1016/j.cbi.2006.10.011. [DOI] [PubMed] [Google Scholar]
- 61.Farombi EO, Fakoya A. Free radical scavenging and antigenotoxic activities of natural phenolic compounds in dried flowers of Hibiscus sabdariffa L. Molecular Nutrition and Food Research. 2005;49(12):1120–1128. doi: 10.1002/mnfr.200500084. [DOI] [PubMed] [Google Scholar]
- 62.Fakeye TO, Pal A, Bawankule DU, Khanuja SPS. Immunomodulatory effect of extracts of Hibiscus sabdariffa L. (family malvaceae) in a mouse model. Phytotherapy Research. 2008;22(5):664–668. doi: 10.1002/ptr.2370. [DOI] [PubMed] [Google Scholar]
- 63.Yang MY, Peng CH, Chan KC, Yang YIS, Huang CN, Wang CJ. The hypolipidemic effect of Hibiscus sabdariffa polyphenols via inhibiting lipogenesis and promoting hepatic lipid clearance. Journal of Agricultural and Food Chemistry. 2010;58(2):850–859. doi: 10.1021/jf903209w. [DOI] [PubMed] [Google Scholar]
- 64.Huang CN, Chan KC, Lin WT, Su SL, Wang CJ, Peng CH. Hibiscus sabdariffa inhibits vascular smooth muscle cell proliferation and migration induced by high glucoses-A mechanism involves connective tissue growth factor signals. Journal of Agricultural and Food Chemistry. 2009;57(8):3073–3079. doi: 10.1021/jf803911n. [DOI] [PubMed] [Google Scholar]
- 65.Mohamed R, Fernández J, Pineda M, Aguilar M. Roselle (Hibiscus sabdariffa) seed oil is a rich source of γ-tocopherol. Journal of Food Science. 2007;72(3):S207–S211. doi: 10.1111/j.1750-3841.2007.00285.x. [DOI] [PubMed] [Google Scholar]
- 66.Lorenzi HF, Matos FJA. Plantas Medicinais do Brasil, nativas e exóticas. 1st edition. São Paulo, Brazil: Plantarum; 2008. [Google Scholar]
- 67.Lorenzi H. Plantas medicinais no Brasil: nativas e exóticas cultivadas. Nova Odessa, Brazil: Instituto Plantarum; 2000. [Google Scholar]
- 68.Corrêa AD, Siqueira-Batista R, Quintas LEM. Plantas Medicinais – do Cultivo à Terapêutica-Rio de Janeiro. Editora Vozes; 1998. [Google Scholar]
- 69.Matos FJA. Plantas da medicina popular do Nordeste. Fortaleza. Edições UFC; 1999. [Google Scholar]
- 70.Tiansheng L, Menelaou MA, Vargas D, Fronczek FR, Fischer NH. Polyacetylenes and diterpenes from Solidago canadensis Phytochemistry. The International Journal of Plant Biochemistry. 1993;32(6):1483–1488. [Google Scholar]
- 71.Reznicek G, Jurenitsch J, Plasun M, et al. Four major saponins from Solidago canadensis. Phytochemistry. 1991;30(5):1629–1633. doi: 10.1016/0031-9422(91)84222-e. [DOI] [PubMed] [Google Scholar]
- 72.Reznicek G, Jurenitsch J, Michl G, Haslinger E. The first structurally confirmed saponin from solidago gigantea: structure elucidation by modern NMR techniques. Tetrahedron Letters. 1989;30(31):4097–4100. [Google Scholar]
- 73.Neto MAF, Fagundes DJ, Beletti ME, Novo NF, Juliano Y, Penha-Silva N. Systemic use of Solidago microglossa DC in the cicatrization of open cutaneous wounds in rats. Brazilian Journal of Morphological Sciences. 2004;21:204–210. [Google Scholar]
- 74.Morel AF, Dias GO, Porto C, Simionatto E, Stuker CZ, Dalcol II. Antimicrobial activity of extractives of Solidago microglossa. Fitoterapia. 2006;77(6):453–455. doi: 10.1016/j.fitote.2006.05.006. [DOI] [PubMed] [Google Scholar]
- 75.Hoste H, Jackson F, Athanasiadou S, Thamsborg SM, Hoskin SO. The effects of tannin-rich plants on parasitic nematodes in ruminants. Trends in Parasitology. 2006;22(6):253–261. doi: 10.1016/j.pt.2006.04.004. [DOI] [PubMed] [Google Scholar]
- 76.Yokozawa T, Nakagawa T, Lee KI, Cho EJ, Terasawa K, Takeuchi S. Effects of green tea tannin on cisplatin-induced nephropathy in LLC-PK1 cells and rats. Journal of Pharmacy and Pharmacology. 1999;51(11):1325–1331. doi: 10.1211/0022357991776912. [DOI] [PubMed] [Google Scholar]
- 77.Grassi D, Desideri G, Croce G, Tiberti S, Aggio A, Ferri C. Flavonoids, vascular function and cardiovascular protection. Current Pharmaceutical Design. 2009;15(10):1072–1084. doi: 10.2174/138161209787846982. [DOI] [PubMed] [Google Scholar]
- 78.Huang Y, Yao XQ, Tsang SY, Lau CW, Chen ZY. Role of endothelium/nitric oxide in vascular response, to flavonoids and epicatechin. Acta Pharmacologica Sinica. 2000;21(12):1119–1124. [PubMed] [Google Scholar]
- 79.Van Den Broucke CO, Lemli JA. Spasmolytic activity of the flavonoids from Thymus vulgaris. Pharmaceutisch Weekblad - Scientific Edition. 1983;5(1):9–14. doi: 10.1007/BF01959645. [DOI] [PubMed] [Google Scholar]
- 80.Kissmam KG, Groth D. Plantas infestantes e nocivas. 2nd edition. Vol. 2. São Paulo, Brazil: BASF; 1999. [Google Scholar]
- 81.Santos FV, Colus IMS, Silva MA, Vilegas W, Varanda EA. Assessment of DNA damage by extracts and fractions of Strychnos pseudoquina, a Brazilian medicinal plant with antiulcerogenic activity. Food and Chemical Toxicology. 2006;44(9):1585–1589. doi: 10.1016/j.fct.2006.03.012. [DOI] [PubMed] [Google Scholar]
- 82.Bagatini MD, Fachinetto JM, Da Silva ACF, Tedesco SB. Cytotoxic effects of infusions (tea) of Solidago microglossa DC. (Asteraceae) on the cell cycle of Allium cepa. Brazilian Journal of Pharmacognosy. 2009;19(2B):632–636. [Google Scholar]
- 83.Boulanger D, Brouillette E, Jaspar F, et al. Helenalin reduces Staphylococcus aureus infection in vitro and in vivo. Veterinary Microbiology. 2007;119(2–4):330–338. doi: 10.1016/j.vetmic.2006.08.020. [DOI] [PubMed] [Google Scholar]
- 84.Andrade-Neto VF, Brandão MGL, Stehmann JR, Oliveira LA, Krettli AU. Antimalarial activity of Cinchona-like plants used to treat fever and malaria in Brazil. Journal of Ethnopharmacology. 2003;87(2-3):253–256. doi: 10.1016/s0378-8741(03)00141-7. [DOI] [PubMed] [Google Scholar]
- 85.Nicoletti M, Goulart MOF, De Lima RA, Goulart AE, Delle Monache F, Bettolo GBM. Flavonoids and alkaloids from Strychnos pseudoquina. Journal of Natural Products. 1984;47(6):953–957. doi: 10.1021/np50036a007. [DOI] [PubMed] [Google Scholar]
- 86.Aparecido Da Silva M, Murino Rafacho BP, Hiruma-Lima CA, et al. Evaluation of Strychnos pseudoquina St. Hil. leaves extract on gastrointestinal activity in mice. Chemical and Pharmaceutical Bulletin. 2005;53(8):881–885. doi: 10.1248/cpb.53.881. [DOI] [PubMed] [Google Scholar]
- 87.Honorio-Franca AC, Marins CM, Boldrini F, Franca EL. Evaluation of hypoglicemic activity and healing of extract from amongst bark of "Quina do Cerrado" (Strychnos pseudoquina ST. HILL) Acta Cirurgica Brasileira. 2008;23:504–510. doi: 10.1590/s0102-86502008000600007. [DOI] [PubMed] [Google Scholar]
- 88.Nishijima CM, Rodrigues CM, Silva MA, Lopes-Ferreira M, Vilegas W, Hiruma-Lima CA. Anti-hemorrhagic activity of four brazilian vegetable species against Bothrops jararaca venom. Molecules. 2009;14(3):1072–1080. doi: 10.3390/molecules14031072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Noll IB. Isolamento, identificação e doseamento de furanocumarinas. Porto Alegre: Universidade Federal do Rio Grande do Sul; 1984. M.S. thesis. [Google Scholar]
- 90.Simões CMO, et al. Plantas da medicina popular do Rio Grande do Sul. Porto Alegre: Editora da Universidade; 1996. [Google Scholar]
- 91.Uchiyama T, Hara S, Makino M, Fujimoto Y. seco-adianane-type triterpenoids from Dorstenia brasiliensis (moraceae) Phytochemistry. 2002;60(8):761–764. doi: 10.1016/s0031-9422(02)00180-2. [DOI] [PubMed] [Google Scholar]
- 92.Cardoso CAL, Vilegas W, Barison A, Honda NK. Simultaneous determination of furanocoumarins in infusions and decoctions from "Carapiá" (Dorstenia species) by high-performance liquid chromatography. Journal of Agricultural and Food Chemistry. 2002;50(6):1465–1469. doi: 10.1021/jf0107095. [DOI] [PubMed] [Google Scholar]
- 93.Omisore NOA, Adewunmi CO, Iwalewa EO, et al. Antitrichomonal and antioxidant activities of Dorstenia barteri and Dorstenia convexa. Brazilian Journal of Medical and Biological Research. 2005;38(7):1087–1094. doi: 10.1590/s0100-879x2005000700012. [DOI] [PubMed] [Google Scholar]
- 94.Garcia CM. Estudo fitoquímico e atividade biológica de Pavonia distinguenda A.ST.- HILL. et NAUDIN E Dorstenia brasiliensis LAM. Universidade Federal de Santa Maria - RS; 2007. Ph.D. thesis. [Google Scholar]
- 95.Ruppelt BM, Pereira EF, Gonçalves LC, Pereira NA. Pharmacological screening of plants recommended by folk medicine as anti-snake venom—I. Analgesic and anti-inflammatory activities. Memorias do Instituto Oswaldo Cruz. 1991;86:203–205. doi: 10.1590/s0074-02761991000600046. [DOI] [PubMed] [Google Scholar]
- 96.Abegaz BM, Ngadjui BT, Dongo E, Ngameni B, Nindi MN, Bezabih M. Chalcones and other constituents of Dorstenia prorepens and Dorstenia zenkeri. Phytochemistry. 2002;59(8):877–883. doi: 10.1016/s0031-9422(01)00483-6. [DOI] [PubMed] [Google Scholar]
- 97.Vilegas JHY, Lanças FM, Vilegas W, Pozetti GL. Further triterpenes, steroids and furocoumarins from Brazilian medicinal plants of Dorstenia genus (Moraceae) Journal of the Brazilian Chemical Society. 1997;8(5):529–535. [Google Scholar]
- 98.De Fátima Agra M, De Freitas PF, Barbosa-Filho JM. Synopsis of the plants known as medicinal and poisonous in Northeast of Brazil. Brazilian Journal of Pharmacognosy. 2007;17(1):114–140. [Google Scholar]
- 99.Balestrin L, Gaspari Dias JF, Miguel OG, Dall’Stella DSG, Miguel MD. Contribution to the phytochemical study of Dorstenia multiformis Miquel (Moraceae) with approach in antioxidant activity. Brazilian Journal of Pharmacognosy. 2008;18(2):230–235. [Google Scholar]
- 100.Iwu MM, Jackson JE, Tally JD, Klayman DL. Evaluation of plant extracts for antileishmanial activity using a mechanism-based radiorespirometric microtechnique (RAM) Planta Medica. 1992;58(5):436–441. doi: 10.1055/s-2006-961508. [DOI] [PubMed] [Google Scholar]
- 101.Kawasaki M, Hayashi T, Arisawa M, et al. Structure of scoparic acid A, a new labdane-type diterpenoid from A Paraguayan crude drug 'Typycha Kuratu' (Scoparia Dulcis L.) Chemical and Pharmaceutical Bulletin. 1987;35(9):3963–3966. doi: 10.1248/cpb.35.3963. [DOI] [PubMed] [Google Scholar]
- 102.Ahsan M, Islam SKN, Gray AI, Stimson WH. Cytotoxic diterpenes from Scoparia dulcis. Journal of Natural Products. 2003;66(7):958–961. doi: 10.1021/np020356j. [DOI] [PubMed] [Google Scholar]
- 103.Li Y, Chen X, Satake M, Oshima Y, Ohizumi Y. Acetylated flavonoid glycosides potentiating NGF action from Scoparia dulcis. Journal of Natural Products. 2004;67(4):725–727. doi: 10.1021/np0302908. [DOI] [PubMed] [Google Scholar]
- 104.Nishino H, Hayashi T, Arisawa M, Satomi Y, Iwashima A. Antitumor-promoting activity of scopadulcic acid B, isolated from the medicinal plant Scoparia dulcis L. Oncology. 1993;50(2):100–103. doi: 10.1159/000227156. [DOI] [PubMed] [Google Scholar]
- 105.Hayashi T, Okamura K, Kakemi M, et al. Scopadulcic acid B, a new tetracyclic diterpenoid from Scoparia dulcis L. Its structure, H+,K+-adenosine triphosphatase inhibitory activity and pharmacokinetic behaviour in rats. Chemical and Pharmaceutical Bulletin. 1990;38(10):2740–2745. doi: 10.1248/cpb.38.2740. [DOI] [PubMed] [Google Scholar]
- 106.Hayashi K, Niwayama S, Hayashi T, Nago R, Ochiai H, Morita N. In vitro and in vivo antiviral activity of scopadulcic acid B from Scoparia dulcis, Scrophulariaceae, against herpes simplex virus type 1. Antiviral Research. 1988;9(6):345–354. doi: 10.1016/0166-3542(88)90036-8. [DOI] [PubMed] [Google Scholar]
- 107.Freire SM, Torres LM, Roque NF, Souccar C, Lapa AJ. Analgesic activity of a triterpene isolated from Scoparia dulcis L. (Vassourinha) Memorias do Instituto Oswaldo Cruz. 1991;86:149–151. doi: 10.1590/s0074-02761991000600034. [DOI] [PubMed] [Google Scholar]
- 108.Li Y, Ohizumi Y. Search for constituents with neurotrophic factor-potentiating activity from the medicinal plants of Paraguay and Thailand. Yakugaku Zasshi. 2004;124(7):417–424. doi: 10.1248/yakushi.124.417. [DOI] [PubMed] [Google Scholar]
- 109.Ahmed M, Shikha HA, Sadhu SK, Rahman MT, Datta BK. Analgesic, diuretic, and anti-inflammatory principle from Scoparia dulcis. Pharmazie. 2001;56(8):657–660. [PubMed] [Google Scholar]
- 110.Babincová M, Sourivong P. Free radical scavenging activity of Scoparia dulcis extract. Journal of Medicinal Food. 2001;4(3):179–181. doi: 10.1089/109662001753165765. [DOI] [PubMed] [Google Scholar]
- 111.Praveen TK, Dharmaraj S, Bajaj J, et al. Hepatoprotective activity of petroleum ether, diethyl ether, and methanol extract of Scoparia dulcis L. against CCl4-induced acute liver injury in mice. Indian Journal of Pharmacology. 2009;41(3):110–114. doi: 10.4103/0253-7613.55206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Ratnasooriya WD, Jayakody JRAC, Premakumara GAS, Ediriweera ERHSS. Antioxidant activity of water extract of Scoparia dulcis. Fitoterapia. 2005;76(2):220–222. doi: 10.1016/j.fitote.2004.06.012. [DOI] [PubMed] [Google Scholar]
- 113.Tsai JC, Peng WH, Chiu TH, et al. Hepatoprotective effect of scoparia dulcis on carbon tetrachloride induced acute liver injury in mice. American Journal of Chinese Medicine. 2010;38(4):761–775. doi: 10.1142/S0192415X10008226. [DOI] [PubMed] [Google Scholar]
- 114.Latha M, Ramkumar KM, Pari L, Damodaran PN, Rajeshkannan V, Suresh T. Phytochemical and antimicrobial study of an antidiabetic plant: Scoparia dulcis L. Journal of Medicinal Food. 2006;9(3):391–394. doi: 10.1089/jmf.2006.9.391. [DOI] [PubMed] [Google Scholar]
- 115.Phan MG, Phan TS, Matsunami K, Otsuka H. Chemical and biological evaluation on scopadulane-type diterpenoids from Scoparia dulcis of Vietnamese origin. Chemical and Pharmaceutical Bulletin. 2006;54(4):546–549. doi: 10.1248/cpb.54.546. [DOI] [PubMed] [Google Scholar]
- 116.Gachet MS, Lecaro JS, Kaiser M, et al. Assessment of anti-protozoal activity of plants traditionally used in Ecuador in the treatment of leishmaniasis. Journal of Ethnopharmacology. 2010;128(1):184–197. doi: 10.1016/j.jep.2010.01.007. [DOI] [PubMed] [Google Scholar]
- 117.Babincová M, Schronerová K, Sourivong P. Antiulcer activity of water extract of Scoparia dulcis. Fitoterapia. 2008;79(7-8):587–588. doi: 10.1016/j.fitote.2008.05.001. [DOI] [PubMed] [Google Scholar]
- 118.Mesía-Vela S, Bielavsky M, Torres LMB, et al. In vivo inhibition of gastric acid secretion by the aqueous extract of Scoparia dulcis L. in rodents. Journal of Ethnopharmacology. 2007;111(2):403–408. doi: 10.1016/j.jep.2006.12.009. [DOI] [PubMed] [Google Scholar]
- 119.Pari L, Venkateswaran S. Hypoglycaemic activity of Scopariadulcis L. extract in alloxan induced hyperglycaemic rats. Phytotherapy Research. 2002;16:662–664. doi: 10.1002/ptr.1036. [DOI] [PubMed] [Google Scholar]
- 120.Beh JE, Latip J, Abdullah MP, Ismail A, Hamid M. Scoparia dulcis (SDF7) endowed with glucose uptake properties on L6 myotubes compared insulin. Journal of Ethnopharmacology. 2010;129(1):23–33. doi: 10.1016/j.jep.2010.02.009. [DOI] [PubMed] [Google Scholar]
- 121.Pari L, Latha M, Rao CA. Effect of Scoparia dulcis extract on insulin receptors in streptozotocin induced diabetic rats: Studies on insulin binding to erythrocytes. Journal of Basic and Clinical Physiology and Pharmacology. 2004;15(3-4):223–240. doi: 10.1515/jbcpp.2004.15.3-4.223. [DOI] [PubMed] [Google Scholar]
- 122.Lorenzi H. Árvores brasileiras: Manual de identificação e cultivo de plantas arbóreas nativas do Brasil. 2nd edition. Vol. 1. Nova Odessa, Brazil: Plantarum; 1998. [Google Scholar]
- 123.Tanaka JCA, Da Silva CC, Dias Filho BP, Nakamura CV, De Carvalho JE, Foglio MA. Chemical constituents of Luehea divaricata Mart. (Tiliaceae) Quimica Nova. 2005;28(5):834–837. [Google Scholar]
- 124.Barroso GM. Sistemática de angiospermas do Brasil. Vol. 1. São Paulo, Brazil: EDUSP; 1978. [Google Scholar]
- 125.Choi HJ, Eun JS, Kim BG, Kim SY, Jeon H, Soh Y. Vitexin, an HIF-1α inhibitor, has anti-metastatic potential in PC12 cells. Molecules and Cells. 2006;22(3):291–299. [PubMed] [Google Scholar]
- 126.Kim JH, Lee BC, Kim JH, et al. The isolation and antioxidative effects of vitexin from Acer palmatum. Archives of Pharmacal Research. 2005;28(2):195–202. doi: 10.1007/BF02977715. [DOI] [PubMed] [Google Scholar]
- 127.Hsum YW, Yew WT, Hong PLV, et al. Cancer chemopreventive activity of maslinic acid: suppression of COX-2 expression and inhibition of NF-KB and AP-1 activation in raji cells. Planta Medica. 2011;77(2):152–157. doi: 10.1055/s-0030-1250203. [DOI] [PubMed] [Google Scholar]
- 128.Li C, Yang Z, Zhai C, et al. Maslinic acid potentiates the anti-tumor activity of tumor necrosis factor α by inhibiting NF-κB signaling pathway. Molecular Cancer. 2010;9, article no. 73 doi: 10.1186/1476-4598-9-73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Müller JB, Ceron CS, Kuntz VT, Pozzatti P. Avaliação da Suscetibilidade Antifúngica e Antibacteriana do Extrato Bruto e Frações das Folhas de Luehea divaricata Martius. In: Anais da 58ª Reunião Anual da SBPC; 2006; Florianópolis, Brazil. [Google Scholar]
- 130.Bighetti AE, Antônio MA, Possent A, Foglio MA, Siqueira MG, Carvalho JE. Efeitos da administração aguda e subcrônica da Luehea divaricata Martus et Zuccarini. Lecta. 2004;22(1/2):53–58. [Google Scholar]
- 131.Felício LP, Silva EM, Ribeiro V, et al. Mutagenic potential and modulatory effects of the medicinal plant Luehea divaricata (Malvaceae) in somatic cells of Drosophila melanogaster: SMART/wing. Genetics and Molecular Research. 2011;10(1):16–24. doi: 10.4238/vol10-1gmr982. [DOI] [PubMed] [Google Scholar]
- 132.Zacchino S, Santecchia C, Lopez S, et al. In vitro antifungal evaluation and studies on mode of action of eight selected species from the Argentina flora. Phytomedicine. 1998;5:389–395. doi: 10.1016/S0944-7113(98)80022-6. [DOI] [PubMed] [Google Scholar]
- 133.Mendonça RC, Felfili JM, Walter BMT, et al. Flora vascular do cerrado. In: Sano SM, Almeida SP, editors. Cerrado: ambiente e flora. Planaltina; 1998. pp. 289–556. [Google Scholar]
- 134.Solon S, Lopes L, Sousa-Júnior PT, Schmeda-Hirschmann G. Free radical scavening activity of Lafoensia pacari. Journal of Ethnopharmacology. 2000;72:173–178. doi: 10.1016/s0378-8741(00)00233-6. [DOI] [PubMed] [Google Scholar]
- 135.Rogerio AP, Fontanari C, Melo MCC, et al. Anti-inflammatory, analgesic and anti-oedematous effects of Lafoensia pacari extract and ellagic acid. Journal of Pharmacy and Pharmacology. 2006;58(9):1265–1273. doi: 10.1211/jpp.58.9.0014. [DOI] [PubMed] [Google Scholar]
- 136.Rogerio AP, Fontanari C, Borducchi É, et al. Anti-inflammatory effects of Lafoensia pacari and ellagic acid in a murine model of asthma. European Journal of Pharmacology. 2008;580(1-2):262–270. doi: 10.1016/j.ejphar.2007.10.034. [DOI] [PubMed] [Google Scholar]
- 137.Porto MP, et al. Avaliação tóxico-genética do extrato de Lafoensia pacari em células somáticas de Drosophila melanogaste. In: Resumos do 54 Congresso Brasileiro de Genética,; 2008. [Google Scholar]
- 138.Murakami S, Isobe Y, Higima H, Nagai H, Muramatu M, Otomo S. Inibition of gastric H+K+ ATPase and acid secretion by ellagic acid. Planta Medica. 1991;57(4):305–308. doi: 10.1055/s-2006-960103. [DOI] [PubMed] [Google Scholar]
- 139.Akubue PI, Stohs SJ. Endrin-induced production of nitric oxide by rat peritoneal macrophages. Toxicology Letters. 1992;62(2-3):311–316. doi: 10.1016/0378-4274(92)90035-i. [DOI] [PubMed] [Google Scholar]
- 140.Ramanathan L, Das NP. Inhibitory effects of some natural products on metal-induced lipid oxidation in cooked fish. Biological Trace Element Research. 1992;34(1):35–44. doi: 10.1007/BF02783896. [DOI] [PubMed] [Google Scholar]
- 141.Sartori NT, Martins DTO. Screening’ farmacológico de plantas popularmente utilizadas como antiúlceras em Mato Gross. In: Simpósio de plantas medicinais do Brasil; 1996; Florianópolis, bRAZIL. p. 105. [Google Scholar]
- 142.Tamashiro Filho P. Avaliação da atividade antiúlcera do extrato bruto metanólico de Lafoensia pacari St. Hil. (mangava brava) Cuiabá, Brazil: Universidade Federal de Mato Grosso; 1999. M.S. thesis. [Google Scholar]
- 143.Beserra AMSS. Avaliação da atividade gastroprotetora do ácido elágico em modelos animais. Cuiabá, Brazil: Universidade Federal de Mato Grosso; 2008. M.S. thesis. [Google Scholar]
- 144.Da Mota Menezes V, Atallah AN, Lapa AJ, Catapani WR. Assessing the therapeutic use of Lafoensia pacari St. Hil. extract (Mangava-Brava) in the eradication of Helicobacter pylori: double-blind randomized clinical trial. Helicobacter. 2006;11(3):188–195. doi: 10.1111/j.1523-5378.2006.00399.x. [DOI] [PubMed] [Google Scholar]
- 145.Tonello VM. Estrutura de populações de Lafoensia pacari St. Hil. e dados etnobotânicos e fenológicos em Nossa Senhora do Livramento, Mato Grosso. Cuiabá, Brazil: Universidade Federal de Mato Grosso; 1997. M.S. thesis. [Google Scholar]
- 146.Albuquerque DA, Lopes L. Modulation of Delayed-Type Hypersensitivity by Lafoensia pacari St. Hil. Bollettino Chimico Farmaceutico. 1999;2(138):p. 120. [Google Scholar]
- 147.Rogério AP. Estudo da atividade antiinflamatória do extrato etanólico de Lafoensia pacari Jaume St. Hilaire (Lythraceae) Ribeirão Preto, Brazil: Universidade de São Paulo; 2002. M.S. thesis. [Google Scholar]
- 148.Rogerio AP, Sá-Nunes A, Faccioli LH. The activity of medicinal plants and secondary metabolites on eosinophilic inflammation. Pharmacological Research. 2010;62(4):298–307. doi: 10.1016/j.phrs.2010.04.005. [DOI] [PubMed] [Google Scholar]
- 149.Nascimento MVM, Galdino PM, Florentino IF, et al. Antinociceptive effect of Lafoensia pacari A. St.-Hil. independent of anti-inflammatory activity of ellagic acid. Journal of Natural Medicines. 2011;65(3-4):448–454. doi: 10.1007/s11418-011-0517-y. [DOI] [PubMed] [Google Scholar]
- 150.Silva Junior IF, et al. Avaliação da atividade antifúngica e modo de ação dos extratos da entrecasca, frações e ácido elágico de Lafoensia pacari A. St.-Hil., Lythraceae. Revista Brasileira de Farmacognosia. 2010;20(3):422–428. [Google Scholar]
- 151.Silva S-CFA. Loção para tratamento capilar e respectivo processo de preparação. Nº do Pedido: PI9903518-9 A2. Classiicação A61K 7/06. Instituto Nacional de Propriedade Industrial, 1996.


