Abstract
Objective
To assess the clinical efficacy of alternative techniques for biliary stricture cannulation in patients undergoing living donor liver transplantation (LDLT), after cannulation failure with a conventional (0.035-inch guidewire) technique.
Subjects and Methods
Of 293 patients with biliary strictures after LDLT, 19 (6%) patients, 11 men and 8 women of mean age 48.5 years, had the failed cannulation of the stricture by conventional techniques. Recannulation was attempted by using two alternative methods, namely a micro-catheter set via percutaneous access and a snare (rendezvous) technique using percutaneous and endoscopic approaches.
Results
Strictures were successfully cannulated in 16 (84%) of the 19 patients. A microcatheter set was used in 12 and a snare technique in four patients. Stricture cannulation failed in the remaining three patients, who finally underwent surgical revision.
Conclusion
Most technical failures using a conventional technique for biliary stricture cannulation after LDLT can be overcome by using a microcatheter set or a snare (rendezvous) technique.
Keywords: Living donor liver transplantation, Biliary complications, Endoscopy, Fluoroscopy
INTRODUCTION
Although surgical techniques for biliary reconstruction in liver transplantation (LT) have improved, postoperative biliary complications are not uncommon (1-3). Although the incidence of biliary complications following cadaveric donor LT has dropped to below 10% (4), this incidence has been found to range from 15% to 40% in patients undergoing living donor LT (LDLT) (5). Biliary stricture is the most common biliary complication after LDLT; etiologic factors for biliary stricture include ischemic changes in the biliary stump, biliary leakage, hepatic artery complications, cytomegalovirus infection, and blood type incompatibility (6, 7).
An endoscopic or radiologic percutaneous approach may be an initial minimally-invasive method for treating biliary strictures after LDLT (6-11). However, cannulation of these strictures is sometimes difficult due to the presence of a sharp or twisted angle within the stricture, or a tight or complete stricture (1, 7). This type of minimally-invasive intervention is therefore impossible when the stenosis cannot be approached or passed, making surgical revision or liver graft failure inevitable in these patients (7, 12). Other cannulation methods may avoid the need for surgery or retransplantation. We therefore assessed the clinical efficacy of alternative techniques for cannulation of biliary strictures after LDLT following cannulation failure with a conventional technique.
SUBJECTS AND METHODS
Patient Population
Of the 1081 patients who underwent LDLT at our institution between 1997 and 2005, 293 (27%) underwent percutaneous transhepatic biliary drainage (PTBD) and subsequent balloon dilation to treat biliary strictures. Failure to cross the stricture using a conventional technique was observed in 19 of these 293 (6%) patients, 11 men and 8 women, of mean age 48.5 years (range, 25-60 years). The characteristics of the patient population are summarized in Table 1. Biliary strictures were diagnosed based on combinations of clinical symptoms, biochemical data, and imaging findings, using ultrasonography, computed tomography, or diisopropyl iminodiacetic acid scans, and confirmed by T-tube cholangiography, percutaneous transhepatic cholangiography, or endoscopic retrograde cholangiography. The study protocol was approved by our institutional review board, and all patients provided written informed consent.
Table 1.
Patient Characteristics
Note.- BD = bile duct, CT = conventional technique, D-D = duct-to-duct, EA = endoscopic assistance, F = female, H-J = hepaticojejunostomy, L = left, M = male, MT = microcatheter technique, No. = number, N/A = nonapplicable, POD = postoperative day, PTBD = percutaneous transhepatic biliary drainage, R = right
Interventional Procedures
Intravenous Demerol (Keukdong Pharmaceuticals, Seoul, Korea) and intramuscular lidocaine (Jeil Pharmaceuticals, Daegu, Korea) were administered for sedation and local analgesia. Percutaneous transhepatic biliary cholangiography was initially performed using a 21-gauge needle (Chiba; Cook, Bloomington, IN, USA) under fluoroscopic guidance. Use of a right or left approach for percutaneous transhepatic biliary drainage was dependent on biliary anatomy and the ability to puncture an intrahepatic bile duct close to the site of blockage. After puncturing the intrahepatic bile duct, a needle and 0.018-inch guide wire (Cook) were inserted. The needle was subsequently exchanged for a 5-F coaxial dilator (consisting of a metal cannula, a 4-F plastic trocar, and a 5-F outer cannula) over the 0.018-inch guide wire. Subsequently, the 4-F plastic trocar and the metal cannula were removed, the 0.018-inch guidewire was exchanged for a 0.035-inch guidewire (Terumo, Tokyo, Japan), and the 5-F outer cannula was exchanged for a 6-7-F introducer sheath (Terumo) over the 0.035-inch guidewire. In a conventional technique, the 0.035-inch guide wire (Terumo) and a 5-F angled cobra or Kumpe catheter (Cook) were used to cross the stricture. Following balloon dilation using a balloon catheter (6-8 mm in diameter) (Synergy™; Boston Scientific, Watertown, MA, USA), an internal-external 8.5-F drainage catheter (Dawson-Mueller drainage catheter; Cook) was placed across the stricture.
Alternative Techniques
If cannulation of the stricture was not possible using a conventional technique, cannulation was re-attempted using one of two alternative techniques: a micro-catheter set (Renegade and Transcend wire; Boston Scientific) (Fig. 1A) or a snare (rendezvous) method (Fig. 1B). In the latter, a 0.035-inch guide wire was used to access the stricture through an endoscopic nasobiliary drainage (ENBD) catheter, while a 5-mm diameter loop snare (ev3, Plymouth, MA, USA) was introduced via percutaneous access (through the 6-7-F introducer sheath) to capture the guidewire. After the guidewire was captured, a 5-F guiding catheter was advanced to close the snare loop, and the snare, guiding catheter and guide wire were pulled to open the stricture.
Fig. 1.
Schematic drawings of two alternative techniques.
A. Technique using microcatheter set (arrow head). B. Technique using snare (rendezvous technique). Guide wire was inserted into stricture through endoscopic nasobiliary drainage catheter (arrowhead), while snare (arrow) was introduced through percutaneous transhepatic biliary drainage catheter. Snare was used to capture guide wire and pull it through stricture to complete cannulation of stricture.
The microcatheter technique was used in all patients who underwent hepatico-jejunostomy biliary reconstruction due to the inaccessibility of endoscopy, and was used initially in patients with duct-to-duct biliary reconstruction. If this technique failed in patients with duct-to-duct biliary reconstruction, the snare (rendezvous) technique was used.
Follow-up
Within a week after initial PTBD and balloon dilation, the drainage tube was exchanged for an internal-external 10-F drainage tube. If follow-up cholangiography showed missing bile ducts or other biliary strictures, these ducts were cannulated, followed by balloon dilation, through the initial PTBD tract. A second PTBD was performed in patients with complex type strictures that could not be cannulated through the initial PTBD tract. Following improvements in symptoms and biochemical data, patients were discharged with clamping of the drainage tube.
Patients underwent follow-up cholangiography and serial exchanges of drainage tubes for larger diameter tubes, up to 14-F, with or without repeat balloon dilations every 4-6 weeks on an out-patient basis. The 14-F drainage catheter was maintained for at least 3 months to minimize elastic restenosis. The distal tip of the catheter was then positioned peripheral to the stricture and the catheter was clamped for 4-6 weeks to evaluate the presence of elastic restenosis. If follow-up cholangiography showed fluent passage of contrast media through the resolved stricture without patient symptoms or a deterioration in biochemical data, the drainage catheter was removed. However, if follow-up examinations showed evidence of elastic restenosis, such as stasis of contrast media, progression of bile duct dilation, recurrent symptoms, or deterioration in biochemical data, balloon dilation was repeated and the drainage tube was repositioned across the stricture for an additional 3-6 months.
RESULTS
Cholangiography before attempting alternative techniques revealed that the obstructions were complete (i.e., no passage of contrast medium through the stricture) in 15 patients and incomplete in the remaining 4. Strictures were successfully cannulated using the microcatheter set (Fig. 2) in 12 patients and the snare technique (Fig. 3) in 4. Cannulation failed in the remaining three patients, who thereafter underwent surgical revision. The technical failure rate was higher in patients who underwent Roux-en-Y hepaticojejunostomy (33%, 2/6) than duct-to-duct biliary reconstruction (8%, 1/13), but the difference was not statistically significant (p = 0.222, Fisher's exact test). There were no procedure-related complications. The median number of attempted conventional techniques prior to the use of an alternative technique was 4 (range, 1-23).
Fig. 2.
Technique using microcatheter set in 56-year-old man with stricture in duct to duct anastomosis following right-lobe living donor liver transplantation.
A. Cholangiogram showing severe, twisted stricture (arrow) in duct-to-duct anastomosis. Due to severity of stricture, cannulation failed using conventional technique. B. Cholangiogram showing successful cannulation of stricture using microcatheter set (arrowhead).
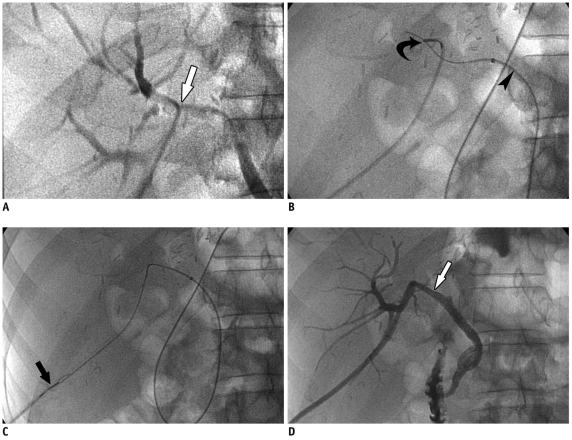
Fig. 3.
Technique using snare (rendezvous technique) in 46-year-old woman with stricture in duct to duct anastomosis following right-lobe living donor liver transplantation.
A. Cholangiogram showing severe stricture (arrow) at duct-to-duct anastomosis. B, C. View showing introduction of guide wire through endoscopic nasobiliary drainage tube (arrowhead) and capture of guide wire by snare (arrows). Guide wire was subsequently pulled through stricture to complete its cannulation. D. After successful cannulation and subsequent balloon dilation of stricture, percutaneous transhepatic biliary drainage tube (arrow) was advanced across stricture.
After cannulation of the strictures, the 16 patients underwent technically successful balloon dilation, with a median number of 8 sessions (range, 3-15 sessions). All 16 patients showed improved symptoms with normalized biochemical data during indwelling of the PTBD catheter for a median period of 15 months (range, 6-32 months). Follow-up cholangiography revealed fluent passage of contrast media through the resolved stricture in 13 of the 16 patients (81%) without patient symptoms or deterioration in biochemical data, allowing removal of the PTBD catheter from these 13 patients.
One patient showed a recurrent stricture 5 months after PTBD catheter removal and underwent ENBD with subsequent balloon dilation. The other 12 patients did not experience recurrent strictures during a median follow-up of 10.5 months (range, 3-86 months) after PTBD catheter removal.
DISCUSSION
Biliary stricture after LDLT leads to a deterioration of liver function, abscess, and even sepsis if adequate biliary diversion is not provided at an early stage (4). Early recognition and appropriate treatment of biliary strictures can greatly improve transplanted liver grafts and patient survival (13).
Biliary strictures in LT recipients are initially treated endoscopically, with percutaneous treatment reserved primarily for patients who fail endoscopic retrograde cholangio-pancreatography (ERCP) or in whom ERCP is impossible to perform (7, 11). The reasons for failure include duodenal stenosis, failure to pass the biliary stricture, failure to cannulate the papilla, or prior creation of a Roux-en-Y hepaticojejunostomy biliary reconstruction. Percutaneous treatment of biliary strictures after LDLT is the preferred option in our institution because it is successful in most patients. Furthermore, percutaneous access may be easier in the treatment of nonanastomotic intrahepatic strictures, allowing one or more appropriate segments to be chosen.
Passage of the guidewire through the stricture, by endoscopic or percutaneous access, is essential for successful treatment. For example, ERCP for strictures at duct-to-duct anastomoses after cadaveric LT was unsuccessful in 7 of 36 (19%) patients due to the inability to pass the guidewire through the stricture (12). A percutaneous approach, however, was successful in 3 of these 7 patients. In another series (9), a guidewire could not pass the stricture in 3 of 4 patients who underwent surgical revision after failure of percutaneous treatment for anastomotic biliary stricture after LDLT, suggesting that a more meticulous technique would be necessary to cannulate the stricture site to avoid reoperation.
We found that 16 of 19 patients who could not be successfully cannulated by conventional techniques benefited from alternative methods, including 12 who benefited from the microcatheter technique and 4 who benefited from endoscopic assistance. After successful cannulation, all 16 patients showed good results. Although one patient showed a recurrent stricture 5 months after PTBD catheter removal, the recurrent stricture was easily cannulated by ENBD and was successfully treated by subsequent balloon dilation.
The advantage of the microcatheter technique over the conventional technique may consist of the use of a smaller wire, which may pass through a stricture that does not allow a 0.035-inch wire to pass. Endoscopic assistance is a useful adjunctive method to identify the distal bile duct segment over the stricture and may provide a retrograde approach when the passage of a wire is not feasible with an anterograde approach. These methods can therefore be used to cannulate severe or even complete biliary strictures.
Only one alternative method (microcatheter technique) can be performed in patients with Roux-en-Y hepaticojejunostomy biliary reconstruction because of the inaccessibility of the problem to endoscopy. In contrast, endoscopy is possible in patients with duct-to-duct biliary reconstruction, suggesting that this method of reconstruction may be more advantageous than Roux-en-Y hepaticojejunostomy. We found that the technical failure rate was higher in patients with Roux-en-Y hepaticojejunostomy (33%, 2/6) than duct-to-duct (8%, 1/12) biliary reconstruction. Although the difference was not statistically significant, due to the small number of study patients, our results suggest that a larger study might also find a higher technical success rate in patients with duct-to-duct than Roux-en-Y hepaticojejunostomy biliary reconstruction.
In conclusion, alternative techniques to cannulate severe biliary strictures after LDLT seem to be clinically effective. Most technical failures by conventional technique can be overcome using a microcatheter set or snare (rendezvous) technique.
References
- 1.Chang JH, Lee IS, Chun HJ, Choi JY, Yoon SK, Kim DG, et al. Usefulness of the rendezvous technique for biliary stricture after adult right-lobe living-donor liver transplantation with duct-to-duct anastomosis. Gut Liver. 2010;4:68–75. doi: 10.5009/gnl.2010.4.1.68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kim JH, Ko GY, Sung KB, Yoon HK, Gwon DI, Kim KR, et al. Bile leak following living donor liver transplantation: clinical efficacy of percutaneous transhepatic treatment. Liver Transpl. 2008;14:1142–1149. doi: 10.1002/lt.21501. [DOI] [PubMed] [Google Scholar]
- 3.Choo SW, Shin SW, Do YS, Liu WC, Park KB, Sung YM, et al. The balloon dilatation and large profile catheter maintenance method for the management of the bile duct stricture following liver transplantation. Korean J Radiol. 2006;7:41–49. doi: 10.3348/kjr.2006.7.1.41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Moser MA, Wall WJ. Management of biliary problems after liver transplantation. Liver Transpl. 2001;7:S46–S52. doi: 10.1053/jlts.2001.28518. [DOI] [PubMed] [Google Scholar]
- 5.Ramacciato G, Varotti G, Quintini C, Masetti M, Di Benedetto F, Grazi GL, et al. Impact of biliary complications in right lobe living donor liver transplantation. Transpl Int. 2006;19:122–127. doi: 10.1111/j.1432-2277.2005.00248.x. [DOI] [PubMed] [Google Scholar]
- 6.Yazumi S, Chiba T. Biliary complications after a right-lobe living donor liver transplantation. J Gastroenterol. 2005;40:861–865. doi: 10.1007/s00535-005-1698-5. [DOI] [PubMed] [Google Scholar]
- 7.Kasahara M, Egawa H, Takada Y, Oike F, Sakamoto S, Kiuchi T, et al. Biliary reconstruction in right lobe living-donor liver transplantation: comparison of different techniques in 321 recipients. Ann Surg. 2006;243:559–566. doi: 10.1097/01.sla.0000206419.65678.2e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hwang S, Lee SG, Sung KB, Park KM, Kim KH, Ahn CS, et al. Long-term incidence, risk factors, and management of biliary complications after adult living donor liver transplantation. Liver Transpl. 2006;12:831–838. doi: 10.1002/lt.20693. [DOI] [PubMed] [Google Scholar]
- 9.Chang JM, Lee JM, Suh KS, Yi NJ, Kim YT, Kim SH, et al. Biliary complications in living donor liver transplantation: imaging findings and the roles of interventional procedures. Cardiovasc Intervent Radiol. 2005;28:756–767. doi: 10.1007/s00270-004-0262-7. [DOI] [PubMed] [Google Scholar]
- 10.Yazumi S, Yoshimoto T, Hisatsune H, Hasegawa K, Kida M, Tada S, et al. Endoscopic treatment of biliary complications after right-lobe living-donor liver transplantation with duct-to-duct biliary anastomosis. J Hepatobiliary Pancreat Surg. 2006;13:502–510. doi: 10.1007/s00534-005-1084-y. [DOI] [PubMed] [Google Scholar]
- 11.Shah JN, Ahmad NA, Shetty K, Kochman ML, Long WB, Brensinger CM, et al. Endoscopic management of biliary complications after adult living donor liver transplantation. Am J Gastroenterol. 2004;99:1291–1295. doi: 10.1111/j.1572-0241.2004.30775.x. [DOI] [PubMed] [Google Scholar]
- 12.Verdonk RC, Buis CI, Porte RJ, van der Jagt EJ, Limburg AJ, van den Berg AP, et al. Anastomotic biliary strictures after liver transplantation: causes and consequences. Liver Transpl. 2006;12:726–735. doi: 10.1002/lt.20714. [DOI] [PubMed] [Google Scholar]
- 13.Park JS, Kim MH, Lee SK, Seo DW, Lee SS, Han J, et al. Efficacy of endoscopic and percutaneous treatments for biliary complications after cadaveric and living donor liver transplantation. Gastrointest Endosc. 2003;57:78–85. doi: 10.1067/mge.2003.11. [DOI] [PubMed] [Google Scholar]