Abstract
A 47-year-old Korean woman with right middle lobe lung adenocarcinoma, malignant pleural effusion, and multiple lymph node and bone metastases, after three months of lung cancer diagnosis, presented with a palpable right breast mass. Images of the right breast demonstrated architectural distortion that strongly suggested primary breast cancer. Breast biopsy revealed metastatic lung cancer with a negative result for estrogen receptor (ER), progesterone receptor (PR) and mammaglobin, and a positive result for thyroid transcription factor-1 (TTF-1). We present a case of breast metastasis from a case of lung cancer with an extensive micropapillary component, which was initially misinterpreted as a primary breast cancer due to unusual image findings with architectural distortion.
Keywords: Metastasis, Breast images, Lung cancer, Micropapillary carcinoma
INTRODUCTION
Common image findings of breast metastases from extra-mammary malignancy are single or multiple, round, usually circumscribed mass(es) variable in size (1). This is known to be due to a nonductal pattern of metastatic spread and lack of desmoplastic reaction in breast metastasis. If architectural distortion is seen on mammography, the possibility of metastasis from extra-mammary malignancy is very low and primary breast lesion including primary cancer is rather favored.
Here, we present a case of breast metastasis from lung cancer with extensive micropapillary component which was initially favored to be the primary breast cancer rather than metastasis because the breast lesion was associated with an architectural distortion on mammography.
CASE REPORT
A 47-year-old woman initially presented with chest pain and dyspnea for the last three months and with 3 kg in weight loss over the last six months. Her past medical history includes a right thyroid lobectomy for a large benign thyroid nodule and cyst about two years ago. A chest computed tomography (CT) from the outside hospital showed a 2.3 × 1.8 cm sized mass in the right middle lobe with pleural effusion (Fig. 1A). On a positron emission tomography (PET) image, hot uptakes were noted at multiple sites including the main lung mass, multiple mediastinal and right cardiophrenic lymph nodes, and bones (ribs and right femoral head).
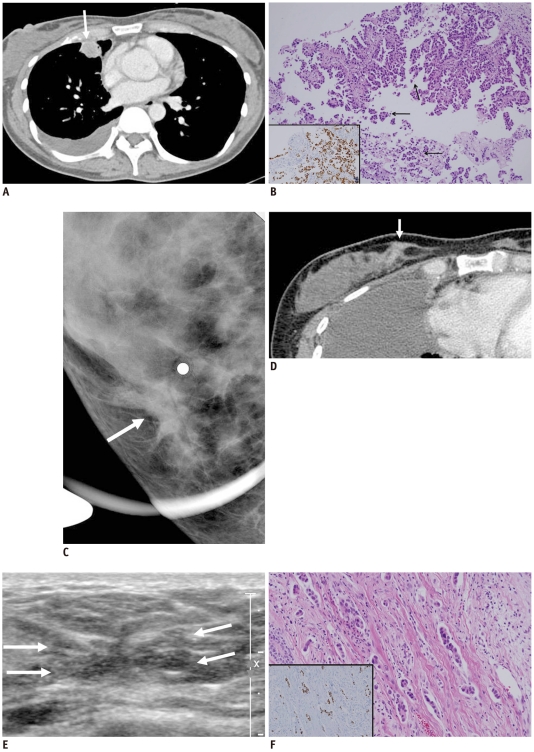
Fig. 1.
Images and pathologic findings in 47-year-old woman with primary lung cancer.
A. Outside chest CT shows round mass with internal necrosis in right middle lobe (arrow), with right pleural effusion. B. Primary lung cancer shows adenocarcinoma with papillary and micropapillary carcinoma (arrow; Hematoxylin and Eosin staining, × 100). TTF-1 stain reveals nuclear positivity (inset, TTF-1 immunostaining, × 200). C. Spot compression view of right breast shows focal architectural distortion (arrow) in right lower inner quadrant without evidence of microcalcifications or discrete mass. Metallic marker is attached to area of palpable site. D. Follow-up chest CT shows irregular enhancing lesion of right breast in lower inner quadrant (arrow). E. Breast US demonstrates 1 cm sized ill-defined irregular shaped isoechoic lesion (arrows) with focal infiltration at 4 o'clock position in right breast. F. Breast biopsy shows micropapillary carcinoma with small tumor cell nests in empty lacunar spaces and desmoplastic reaction in stroma (Hematoxylin and Eosin staining, × 100). TTF-1 stain reveals nuclear positivity, supporting metastasis from lung (TTF-1 immunostaining, × 100).
Clinically, lung cancer with distant metastasis (clinical stage IV) was suspected and the patient was transferred to our hospital. A lung biopsy was performed and a primary lung adenocarcinoma with predominantly micropapillary carcinoma component was diagnosed (Fig. 1B). The patient was treated with chemotherapy consisting of Cisplatin followed by Irinotecan.
Three months after the initiation of chemotherapy, she complained of a palpable mass in her right breast. For evaluation of the right breast lesion, she underwent mammography and spot magnification with metallic marker attachment (Fig. 1C).
On the right lower inner quadrant, focal architectural distortion was detected without evidence of microcalcifications or mass on images. A follow-up chest CT shows an irregular enhancing lesion of the right breast in the lower inner quadrant (Fig. 1D). A breast ultrasound (US) was performed to localize the lesion and for a biopsy. The breast US showed an about 1 cm sized ill-defined irregular-shaped isoechoic lesion in the right lower inner quadrant, about 4 cm from the right nipple (Fig. 1E). Color Doppler US demonstrated no vascularity. In order to confirm the image finding of primary breast cancer and to exclude the possibility of metastatic lung cancer, an US-guided core needle biopsy (14 gauge automated gun, Acecut®, TSK Laboratory, Tochigi, Japan) was performed and 4 core tissue samples were obtained.
The breast biopsy showed an adenocarcinoma with a micropapillary component as well as a desmoplastic reaction and lymphovascular invasion, which was morphologically similar to that seen in the primary lung cancer (Fig. 1F). The surrounding breast ducts and lobules were unremarkable with no atypical changes. To further support the metastatic carcinoma from the lung and to exclude the primary breast cancer, immunohistochemistry was recommended. Immunohistochemical markers for breast including ER, PR, and mammaglobin, were negative and lung cancer marker of TTF-1 was strongly positive, which further supported the lung adenocarcinoma with metastasis to the breast.
After 4 cycles of cisplatin followed by Irinotecan, the chemotherapeutic agent was changed to Erlotinib. Five months after performing an US-guided core biopsy of the right breast, the volume of the main lung mass and pleural effusion was minimally decreased and the patient's dyspneic symptoms were relieved. She did not undergo any follow-up examination for the breast lesion. She is currently alive with disease eight months after initial diagnosis of lung cancer.
DISCUSSION
In contrast to primary breast cancer being the most common malignancy of adult females worldwide, metastatic involvement of the breast is rare with a reported frequency of 0.4-1.3% in clinical series (2, 3). Despite its rarity, metastatic disease to the breast is an important diagnostic clinical problem, because its treatment differs greatly from that of primary breast cancer.
Carcinomas with micropapillary components have been reported at several anatomical sites, including the breast, urinary bladder, ovary, major salivary glands, and recently the lungs (4). The micropapillary component is being increasingly recognized as a prognostic predictor for aggressive behavior with a tendency to metastasize to the lymph nodes and other organs (5, 6). Maounis et al. (7) reported a case of metastasis to the breast from lung adenocarcinoma with an extensive micropapillary component, focused on the pathologic and immunohistochemical differentiation of the primary lung versus breast. To the best of our knowledge, our case is the second case of lung adenocarcinoma with a micropapillary component metastatic to the breast. Our case and Maounis et al.'s case shared some similarities in that they were more compatible with primary breast cancer than the metastasis on initial image findings. Based on the rare reported cases, it is difficult to document whether lung cancer with a micropapillary component has a unique pattern of breast metastasis or not on image findings. However, it is worthwhile to accumulate more cases to support our findings.
The distinction between metastasis from lung adenocarcinoma, particularly with extensive micropapillary patterns, and primary mammary micropapillary adenocarcinoma may cause a significant diagnostic dilemma. The immunohistochemistry could contribute to a differential diagnosis. TTF-1 is expressed in 68-80% of lung adenocarcinoma cases, and has never been reported to stain positive in breast adenocarcinoma cases (8). ER expression in lung adenocarcinoma cases using monoclonal antibodies, is very low (9). Finally, mammaglobin is expressed in 48-72% of mammary adenocarcinoma cases, but stains negative in pulmonary adenocarcinoma (8, 10). Consequently, a panel of markers must be used, as no single antibody is 100% sensitive and false negative results do occur. The panel for distinguishing lung adenocarcinoma from breast carcinoma includes ER, PR and mammaglobin for the breast and TTF-1 for the lung. Our case demonstrated a typical immunohistochemical finding of lung cancer with ER, PR and mammaglobin negative, and TTF-1 positive.
Imaging findings of primary invasive micropapillary carcinoma of the breast are highly suggestive of malignancy. The lesion is known to be a high-density irregular mass with indistinct margins associated and microcalcifications on mammograms; a solid irregular hypoechoic mass with indistinct margins and frequent axillary nodal involvement on sonograms (11). In our case, microcalcifications were not seen on mammogram.
The most common radiologic appearance of blood-borne metastasis to the breast is one or more round, discrete nodules in the breast (12). From a purely radiologic view, these nodules cannot be differentiated from small benign nodules such as cysts or fibroadenomas. To differentiate radiologically metastatic carcinoma to the breast from the primary breast cancer, several points should be kept in mind. A discrete nodule in the mammography of patients known to have extra-mammary cancer should alert one to the possibility of blood-borne metastasis, particularly if other soft tissue metastases are also present. Likewise, an unusual or eccentric location of a discrete nodule in subcutaneous fat rather than glandular tissue should suggest the possibility of blood-borne metastasis. In addition, the rapid growth of breast nodules between two mammogram intervals may also be an important clue favoring metastasis (12). Another type of metastasis to the breast from extra-mammary malignancy is cross lymphatic, with the earliest radiologic finding of this type is skin thickening (12).
In our case, the images did not indicate any mass or skin thickening. An architectural distortion was the main image finding. Therefore, the first impression was a primary breast malignancy even though the patient has a known history of lung adenocarcinoma.
The histology of metastases to the breast usually reflects the primary tumor well enough that the pathologic diagnosis is obvious. The metastatic tumor in the breast in the current case revealed an adenocarcinoma with micropapillary component with severe desmoplastic reaction and lymphovascular invasion, which could be a possible explanation of the architectural distortion on images. This was a unique finding, different from that of another case report described as diffuse asymmetric density on mammography (13).
We present a rare case of metastasis to the breast from lung adenocarcinoma with an extensive micropapillary component, which on mammography due to architectural distortion, a primary breast carcinoma was favored even though the patient had a history of known primary lung cancer and this pattern has never been described before as a metastasis. Therefore, in cases with architectural distortion on mammogram with known lung cancer history, before making the diagnosis of primary breast cancer, the possibility of metastasis from the known lung cancer should be carefully excluded, in addition to considering the presence of a micropapillary component.
References
- 1.Lee SH, Park JM, Kook SH, Han BK, Moon WK. Metastatic tumors to the breast: mammographic and ultrasonographic findings. J Ultrasound Med. 2000;19:257–262. doi: 10.7863/jum.2000.19.4.257. [DOI] [PubMed] [Google Scholar]
- 2.Hajdu SI, Urban JA. Cancers metastatic to the breast. Cancer. 1972;29:1691–1696. doi: 10.1002/1097-0142(197206)29:6<1691::aid-cncr2820290637>3.0.co;2-4. [DOI] [PubMed] [Google Scholar]
- 3.Vizcaíno I, Torregrosa A, Higueras V, Morote V, Cremades A, Torres V, et al. Metastasis to the breast from extramammary malignancies: a report of four cases and a review of literature. Eur Radiol. 2001;11:1659–1665. doi: 10.1007/s003300000807. [DOI] [PubMed] [Google Scholar]
- 4.Nassar H. Carcinomas with micropapillary morphology: clinical significance and current concepts. Adv Anat Pathol. 2004;11:297–303. doi: 10.1097/01.pap.0000138142.26882.fe. [DOI] [PubMed] [Google Scholar]
- 5.Amin MB, Tamboli P, Merchant SH, Ordóõez NG, Ro J, Ayala AG, et al. Micropapillary component in lung adenocarcinoma: a distinctive histologic feature with possible prognostic significance. Am J Surg Pathol. 2002;26:358–364. doi: 10.1097/00000478-200203000-00010. [DOI] [PubMed] [Google Scholar]
- 6.Maeda R, Isowa N, Onuma H, Miura H, Harada T, Touge H, et al. Lung adenocarcinomas with micropapillary components. Gen Thorac Cardiovasc Surg. 2009;57:534–539. doi: 10.1007/s11748-009-0436-y. [DOI] [PubMed] [Google Scholar]
- 7.Maounis N, Chorti M, Legaki S, Ellina E, Emmanouilidou A, Demonakou M, et al. Metastasis to the breast from an adenocarcinoma of the lung with extensive micropapillary component: a case report and review of the literature. Diagn Pathol. 2010;5:82. doi: 10.1186/1746-1596-5-82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Yang M, Nonaka D. A study of immunohistochemical differential expression in pulmonary and mammary carcinomas. Mod Pathol. 2010;23:654–661. doi: 10.1038/modpathol.2010.38. [DOI] [PubMed] [Google Scholar]
- 9.Gomez-Fernandez C, Mejias A, Walker G, Nadji M. Immunohistochemical expression of estrogen receptor in adenocarcinomas of the lung: the antibody factor. Appl Immunohistochem Mol Morphol. 2010;18:137–141. doi: 10.1097/PAI.0b013e3181bec23b. [DOI] [PubMed] [Google Scholar]
- 10.Bhargava R, Beriwal S, Dabbs DJ. Mammaglobin vs GCDFP-15: an immunohistologic validation survey for sensitivity and specificity. Am J Clin Pathol. 2007;127:103–113. doi: 10.1309/TDP92PQLDE2HLEET. [DOI] [PubMed] [Google Scholar]
- 11.Adrada B, Arribas E, Gilcrease M, Yang WT. Invasive micropapillary carcinoma of the breast: mammographic, sonographic, and MRI features. AJR Am J Roentgenol. 2009;193:W58–W63. doi: 10.2214/AJR.08.1537. [DOI] [PubMed] [Google Scholar]
- 12.Paulus DD, Libshitz HI. Metastasis to the breast. Radiol Clin North Am. 1982;20:561–568. [PubMed] [Google Scholar]
- 13.Masmoudi A, Mathieu MC, Soria JC. Breast metastasis from lung adenocarcinoma: a case report. Anticancer Res. 2003;23:1825–1826. [PubMed] [Google Scholar]