Abstract
PURPOSE
The influence of the modified process in the fiber-reinforced post and resin core foundation treatment on the fracture resistance and failure pattern of premolar was tested in this study.
MATERIALS AND METHODS
Thirty-six human mandibular premolars were divided into 4 groups (n = 9). In group DCT, the quartz fibre post (D.T. Light-post) was cemented with resin cement (DUO-LINK) and a core foundation was formed with composite resin (LIGHT-CORE). In group DMO and DMT, resin cement (DUO-LINK) was used for post (D.T. Light-post) cementation and core foundation; in group DMO, these procedures were performed simultaneously in one step, while DMT group was accomplished in separated two steps. In group LCT, the glass fiber post (LuxaPost) cementation and core foundation was accomplished with composite resin (LuxaCore-Dual) in separated procedures. Tooth were prepared with 2 mm ferrule and restored with nickel-chromium crowns. A static loading test was carried out and loads were applied to the buccal surface of the buccal cusp at a 45 degree inclination to the long axis of the tooth until failure occurred. The data were analyzed with MANOVA (α = .05). The failure pattern was observed and classified as either favorable (allowing repair) or unfavorable (not allowing repair).
RESULTS
The mean fracture strength was highest in group DCT followed in descending order by groups DMO, DMT, and LCT. However, there were no significant differences in fracture strength between the groups. A higher prevalence of favorable fractures was detected in group DMT but there were no significant differences between the groups.
CONCLUSION
The change of post or core foundation method does not appear to influence the fracture strength and failure patterns.
Keywords: Fiber-reinforced post, Quartz fiber post, Glass fiber post, Composite resin core, Fracture test
INTRODUCTION
The restoration of a severely damaged tooth with inadequate residual tooth structure to retain and support an extensive coronal restoration usually needs a post and core as a part of treatment procedure. Number of materials have been developed and used to fabricate post and/or core, and development in composite resin materials and cementation techniques has allowed more conservative and aesthetic post and core restorations.1
Fiber-reinforced posts are fabricated using mixture of resin matrix and various filler components including carbon fiber, glass fiber, quartz fiber and ribbon fiber.2 The advantages of these systems include corrosion resistance, biocompatibility, conservative reduction of tooth structure, and aesthetic properties.3 Furthermore, these posts have similar modulus of elasticity to dentin which allows favorable (re-treatable) tooth fracture near the cementoenamel junction (CEJ) instead of untreatable root fracture.4,5
Subsequent to post cementation, core foundation can be made with several materials. Amalgam cores have good physical properties and economic benefits but they have prolonged setting time, limited bonding ability, and are tend to tarnish and corrode.6-8 Glass ionomer and compomer cements have short setting time, good bonding strength, and fluoride-releasing effect but have poor physical properties.6-8 Composite resins are most often recommended for their good physical and adhesive properties, tooth like colors, and short setting time.6-11 Freedman3 recommended that the use of an esthetic fiber-reinforced post, composite core, and resin cement as the most ideal treatment modality when a tooth restoration will include a post and core.
Although setting of a fiber-reinforced post and fabrication of its core with composite resin are done in a single appointment, this process can be more simplified by modifying bonding and build-up steps. Post cementation and composite core forming procedures require perfect moisture control and conditioning treatment to achieve proper bond between the tooth and bonding resin and/or layered composite material. Saliva contamination between the surfaces of the resin increments can decrease bond strength,12 and presence of many separated steps makes this bonding process susceptible. Recently, several products aiming to eliminate this gap by merging bonding and core build-up procedures are introduced; these products used single material for post cementation and core fabrication at the same time. However the clinical relevance of this one-step procedure is not fully defined, therefore the aim of this study was by comparing the fracture strength and failure patterns of teeth which were restored with conventional two-step technique or modified two-step technique to evaluate the influence of modification in this process. The hypotheses to be tested were: (1) there would be no difference in fracture strength and failure patterns between conventional and modified core fabrication procedures, and (2) materials used to form post and core foundations would not influence the fracture strength and failure patterns.
MATERIALS AND METHODS
Thirty-six recently extracted human single-rooted mandibular premolars with similar size without dental caries and fracture were used. The tooth size was measured with digital caliper (ABS Digimatic caliper CD-15CPX, Mitutoyo Corp. Kawasaki, Japan) at the prospective finish line, and resultant size was 7.50±0.51 mm in bucco-lingual diameter, and 5.09±0.32 mm in mesio-distal. The teeth were soaked for 2 hours in 3% NaOCl solution to remove any foreign substance and soft tissue residue then placed in a saline solution until experiment began. To prepare endodontic treatment, crown portion was removed 2 mm coronal to the CEJ using a water-cooled high speed hand piece and a diamond rotary cutting instrument (Shofu Diamond Point FG C102R; Shofu Inc, Kyoto, Japan). The coronal portion of the root canal was prepared using a carbide rotary cutting instrument (Gates-Glidden Drill; Dentsply Maillefer, Ballaigues, Switzerland). The canal was enlarged to the size of a #40 file using a rotary file (ProTaper Ni-Ti; Dentsply Maillefer) and irrigated with saline solution. After preparation, the canal was obturated with gutta-percha (Dia-Pro; DiaDent, Cheongju, Korea) and sealer (AH-26; Dentsply DeTrey GmbH, Konstanz, Germany) using a thermal condensation device (Obtura II; Obtura Corp, Fenton, MO, USA) and technique.
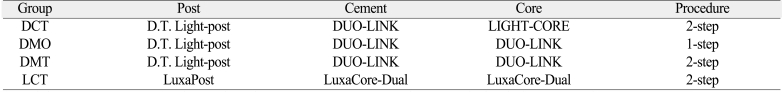
After the endodontic treatment, the post space was prepared to a depth of 10.0 mm (8.0 mm apical from the CEJ). All the post spaces were prepared to the same depth in order to eliminate variables caused by difference of post length. After removing the gutta-percha from the canal using a carbide rotary cutting instrument (Gates Glidden), the preparation was completed with drills prescribed for each system used. Before performing a definitive drilling of the post spaces, the teeth were classified randomly into 4 groups, each to be restored with post and core foundations of different materials and methods (Table 1). One-way ANOVA test affirmed absence of any significant difference in diameter between the groups (data not shown).
Table 1.
Experimental groups used in this study (n = 9)
D.T Light-post (X-80751P #1); Bisco, Schaumburg, IL. Lot 0700004126. Diameter at the level of crown margin was 1.3 mm.
Luxa-post (Luxa-post 1.5); DMG, Hamburg, Germany. Lot 566897. Diameter at the level of crown margin was 1.45 mm.
In group DCT (double tapered quartz fiber post and core foundation with conventional two-step method), all procedures were performed according to the manufacturer's manual. First, the post space was etched using 35% phosphoric acid compound (UNI-ETCH; Bisco, Schaumburg, IL, USA) for 15 seconds, rinsed with water, and then air dried. Subsequently, dentin primer (ONE-STEP; Bisco, Schaumburg, IL, USA) was applied, and the excess primer was removed using paper points. The canal was dried with gentle air for 10 seconds and light-polymerized for further 10 seconds with a visible light-curing unit (1000 mW/cm2, Optilux 501, Demetron/Kerr, Danbury, CT) from 1 mm distance. Subsequently, the post (D.T. Light-post; Bisco, Schaumburg, IL, USA) was cemented with adhesive resin cement (DUO-LINK; Bisco, Schaumburg, IL, USA); excess cement was removed and light-polymerized for 40 seconds from the coronal direction. After the post cementation, the core foundation was formed with composite resin core material (LIGHT-CORE; Bisco, Schaumburg, IL, USA) and light-polymerized for 40 seconds.
In group DMO (double tapered quartz fiber post and core foundation with modified one-step method), adhesive resin cement (DUO-LINK) was used to form core foundation instead of composite resin core material. The post space was conditioned in an identical manner as that performed in group DCT; however, the core foundation was fabricated immediately after the post (D.T. Light-post) placement with adhesive resin cement without separate light curing. Light-polymerization was done once only after all these procedures were finished.
The group DMT (double tapered quartz fiber post and core foundation with modified two-step method) differs from DMO in separate light curing for each steps; first light polymerization was done after post adaptation with resin cement, and second one was done after core build-up. The same adhesive resin cement (DUO-LINK) was used to bond post and to build core up.
In group LCT (LuxaPost and core foundation with conventional two-step method), all procedures were performed according to the manufacturer's recommendation. In this group the glass fiber post (LuxaPost; DMG) was cemented with composite resin core material (LuxaCore-Dual; DMG) which was also used for the core. First, the canal was treated with the primer (Contax primer; DMG) for 20 second and dried then bonding agent (Contax bond; DMG) were applied and light-polymerized for 20 seconds (Optilux 501). After that, the post space was filled with composite resin core material (Luxa Core-Dual) and the post (LuxaPost) was placed; the excess was removed and light-polymerized for 20 seconds (Optilux 501). After the post cementation, the core was formed with composite resin core material (LuxaCore-Dual) and light-polymerized for 20 seconds (Optilux 501). Core fabrication procedures in all groups were performed with free hand without preformed matrix.
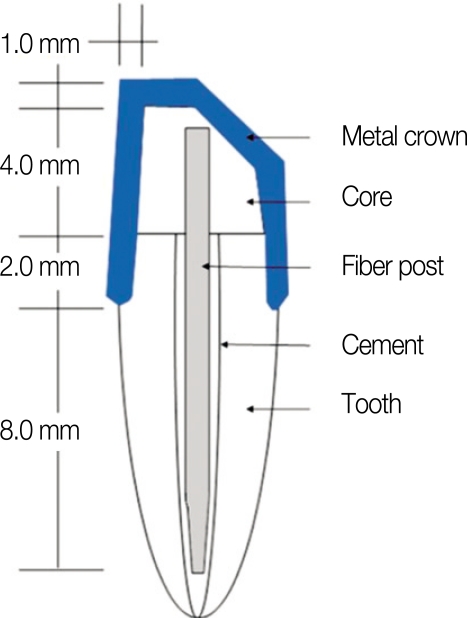
All specimens were prepared for full coverage metal cast crowns with milling machine; axial reduction was performed to obtain an approximate 6 degree total convergence angle, and a 45 degree bevel was made at the buccal inclination of buccal cusp (Fig. 1). The finish line was designed for a chamfer margin with 0.5 mm depth and placed 2 mm apically from core/dentin junction to provide proper ferrule effect.13-15 The total length of the core and residual coronal structure from the margin was 6.0 mm.
Fig. 1.
Schematic design of specimen.
Wax patterns were fabricated directly on the teeth in a uniform thickness of 1.0 mm with a flat occlusal table and a 45 degree bevelled surfaces on buccal inclination of buccal cusp corresponding with the standardized tooth preparation. The wax patterns were invested and casted with nickel-chromium alloy (Rexillium III; Rx Jeneric Inc., Wallingford, CT, USA). After casting and devesting, the crowns were inspected and finished. All procedures were performed by the same operator.
The crowns were cemented with adhesive resin cement (DUO-LINK); the teeth surfaces were cleaned with pumice and etched with phosphoric acid (UNI-ETCH) for 15 seconds, rinsed with water and then dried before cementation. A constant force was applied while the cement was polymerizing and the excess cement was removed after 4 minutes. After cementation, each specimen was initially embedded in auto-polymerizing acrylic resin (Ortho-Jet; Lang Dental Mf Co, Inc, Wheeling, IL, USA) to a level 2 mm below the cast crown margin. The second embedding was performed to locate the specimens at a 45 degree inclination to the longitudinal axis making the flat buccal cusp inclination face toward loading point.
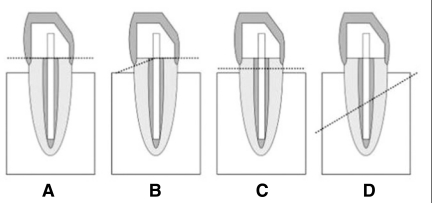
The specimens were fixed in the universal testing machine (Instron 8871; Instron Ltd, High Wycombe, Bucks, UK) and loaded with a compressive force applied at a crosshead speed of 1 mm/min until specimen failure occurred. The loading force was directed perpendicular to the buccal inclination of buccal cusp of the crown and 135 degrees to specimen's long axis. The measurements were recorded in Newtons (N) and failure patterns were observed with naked eyes after the fracture strength tests. The locations of the fracture lines were confirmed by separating the fractured fragments from the acrylic resin blocks. As illustrated in Fig. 2, core fracture (A), core-root fracture (B), and root fracture superior to the resin block (C) were classified as favorable fractures which allow repair. Root fractures inferior to the resin block (D) were regarded as unfavorable ones which does not allow repair. The correlation between tooth size (B-L, M-D diameter) and fracture aspects (fracture strength and pattern) were evaluated statistically to find any significant influencing factors.
Fig. 2.
Failure patterns of specimens. A: Core fracture, B: Core-root fracture, C: Favorable root fracture, D: Unfavorable root fracture.
Statistical software (SPSS version 12.0; SPSS, Chicago, IL, USA) was used for statistical analysis. Multivariate analysis of variance (MANOVA) was used to evaluate the significance of the differences in fracture strength and failure patterns among the groups; bucco-lingual and mesio-distal diameters were considered as covariate. The significance level (α) was .05 for all statistical tests.
RESULTS
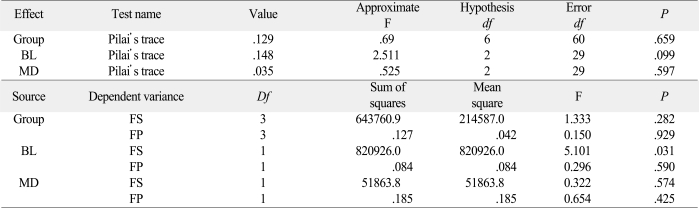
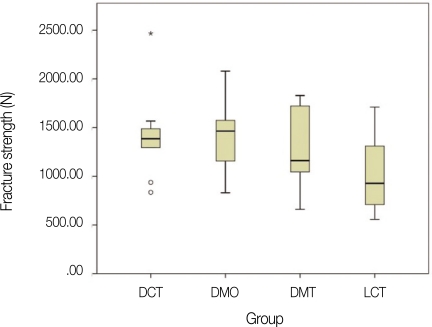
The mean fracture strength was highest in group DCT (1420.7±464.1 N) followed in descending order by groups DMO (1381.9±386.7 N), DMT (1307.6±451.1 N), and LCT (1050.1±438.8 N). However, there was no significant difference in fracture strength between the groups. Groups DCT, DMT and DMO, which used the quartz fiber posts (D.T. Light-post), showed higher fracture resistance than group LCT, in which the glass fiber posts (LuxaPost) were used. However, the differences were not significant (Table 2) (Fig. 3).
Table 2.
Multivariate analysis of variance test results for fracture strength and fracture pattern
BL: bucco-lingual diameter, MD: mesio-distal diameter, FS: fracture strength, FP: fracture pattern.
Fig. 3.
Box plot of the fracture strength of the test groups.
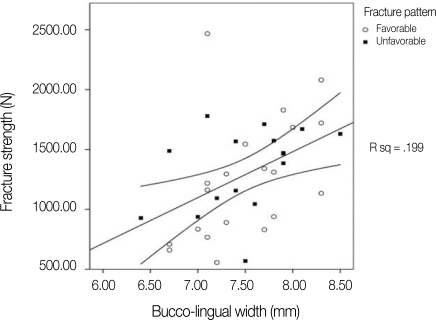
The multivariate analysis of variance result showed there was a significant interaction between fracture strength and buccolingual diameter (P<.05) (Fig. 4); although, there was no significant interaction to the fracture pattern.
Fig. 4.
Fracture strength and fracture patterns according to the buccolingual diameter of the teeth.
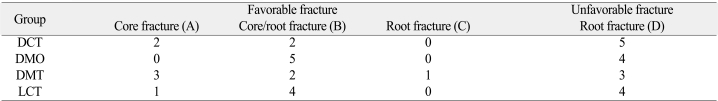
The prevalence of favorable fractures was the highest in group DMT and the least in group DCT (Table 3); even though, there was no significant difference in failure patterns between the groups. The overall prevalence of unfavorable fractures was 55.6%.
Table 3.
Failure pattern of specimen groups
DISCUSSION
Study about mechanical properties of fiber reinforced post and core foundation to restore endodontically treated premolar tooth was carried out to evaluate these next hypotheses. The hypothesis that there would have no difference in fracture strength and failure patterns between conventional and modified methods was supported by the results. The second hypothesis that the Materials used to form post and core foundations would not influence the fracture strength and failure patterns was also found to be accepted.
There have been studies about the influence of restoration materials. Akkayan and Gulmez5 reported that a quartz fiber post showed relevantly higher fracture strength than a glass fiber post in tooth preparations without the ferrule effect feature. Other authors also suggested that the material of the post and core has great importance on fracture strength and failure patterns.4,6,7,9,10 However, our study could not show significant differences between the groups. This might be due to the high standard deviation in each group.
It was assumed that when using natural teeth, variables, such as the differences in tooth strength and size, will have a stronger influence than the restorative material or method. Soresen and Engelman13 reported that the residual tooth structure above the crown margin is an important factor that determines the fracture strength. From the study on the fracture strength by Limbman and Nichollas14 who varied residual tooth structure height from 0.5 mm to 2.0 mm, they found that groups with a residual tooth structure over 1.5 mm showed better results. Ng et al.15 also showed the importance of residual tooth structure on the fracture resistance. These studies show the importance of preserving adequate amount of residual tooth structure. Therefore, it is essential to conserve as much of the tooth structure as possible and provide adequate ferrule effect for better fracture strength.
Current trend in fiber post and direct core restoration is universal use of post cement as a core material or use of core material as post cementation to simplify treatment procedure. In our present study, group LCT, DMO and DMT used homogeneous material for post cementation and core formation. From the result, use of adhesive resin cement as a core material did not show any adverse effect on fracture strength, and furthermore modified one-step cementation and build up technique maintained reasonable result.
During the assessment of the failure pattern, 55.6% of teeth showed unfavorable fractures in this study despite using fiber posts. This might be due to the fact that this study involved enough amount of ferrule portion allowing transmission of greater amount of compressive force through the crown margin to the tooth structure rather than through the post and core foundation.
The limitation of this study was hiring a static short-term loading test to evaluate fracture strength. Failure patterns and strength resulting from long term intermittent loading, combined with artificial aging, might show different results. Therefore further study about this type of modification is required.
CONCLUSION
Within the limitations of this study, the following conclusions were drawn:
The use of resin cement as a core material may not jeopardize fracture resistance of fiber post and core build up treatment.
One-step post bonding and core build up technique would not affect fracture strength and patterns.
The tooth size might have more influence than restoration material and technique on the fracture strength.
References
- 1.Terry DA, Triolo PT, Jr, Swift EJ., Jr Fabrication of direct fiber-reinforced posts: a structure design concept. J Esthet Restor Dent. 2001;13:228–240. doi: 10.1111/j.1708-8240.2001.tb00269.x. [DOI] [PubMed] [Google Scholar]
- 2.Stewardson DA. Non-metal post systems. Dent Update. 2001;28:326–336. doi: 10.12968/denu.2001.28.7.326. [DOI] [PubMed] [Google Scholar]
- 3.Freedman GA. Esthetic post-and-core treatment. Dent Clin North Am. 2001;45:103–104. [PubMed] [Google Scholar]
- 4.Maccari PC, Cosme DC, Oshima HM, Burnett LH, Jr, Shinkai RS. Fracture strength of endodontically treated teeth with flared root canals and restored with different post systems. J Esthet Restor Dent. 2007;19:30–36. doi: 10.1111/j.1708-8240.2006.00060.x. [DOI] [PubMed] [Google Scholar]
- 5.Akkayan B, Gulmez T. Resistance to fracture of endodontically treated teeth restored with different post systems. J Prosthet Dent. 2002;87:431–437. doi: 10.1067/mpr.2002.123227. [DOI] [PubMed] [Google Scholar]
- 6.Medina Tirado JI, Nagy WW, Dhuru VB, Ziebert AJ. The effect of thermocycling on the fracture toughness and hardness of core buildup materials. J Prosthet Dent. 2001;86:474–480. doi: 10.1067/mpr.2001.120110. [DOI] [PubMed] [Google Scholar]
- 7.Cho GC, Kaneko LM, Donovan TE, White SN. Diametral and compressive strength of dental core materials. J Prosthet Dent. 1999;82:272–276. doi: 10.1016/s0022-3913(99)70079-x. [DOI] [PubMed] [Google Scholar]
- 8.Combe EC, Shaglouf AMS, Watts DC, Wilson NHF. Mechanical properties of direct resin core build-up materials. Dent Mater. 1999;15:158–165. doi: 10.1016/s0109-5641(99)00027-5. [DOI] [PubMed] [Google Scholar]
- 9.Levartovsky S, Goldstein GR, Georgescu M. Shear bond strength of several new core materials. J Prosthet Dent. 1996;75:154–158. doi: 10.1016/s0022-3913(96)90092-x. [DOI] [PubMed] [Google Scholar]
- 10.Yaman P, Thorsteinsson TS. Effect of core materials on the stress distribution of posts. J Prosthet Dent. 1992;68:416–420. doi: 10.1016/0022-3913(92)90403-w. [DOI] [PubMed] [Google Scholar]
- 11.Oliva RA, Lowe JA. Dimensional stability of composite used as a core material. J Prosthet Dent. 1986;56:554–561. doi: 10.1016/0022-3913(86)90421-x. [DOI] [PubMed] [Google Scholar]
- 12.Eiriksson SO, Pereira PN, Swift EJ, Jr, Heymann HO, Sigurdsson A. Effects of saliva contamination on resin-resin bond strength. Dent Mater. 2004;20:37–44. doi: 10.1016/s0109-5641(03)00066-6. [DOI] [PubMed] [Google Scholar]
- 13.Sorensen JA, Engelman MJ. Effect of post adaptation on fracture resistance of endodontically treated teeth. J Prosthet Dent. 1990;64:419–424. doi: 10.1016/0022-3913(90)90037-d. [DOI] [PubMed] [Google Scholar]
- 14.Libman WJ, Nichollas JI. Load fatigue of teeth restored with cast posts and cores and completes crowns. Int J Prosthodont. 1995;8:155–161. [PubMed] [Google Scholar]
- 15.Ng CC, Dumbrigue HB, Al-Bayat MI, Griggs JA, Wakefield CW. Influence of remaining coronal tooth structure location on the fracture resistance of restored endodontically treated anterior teeth. J Prosthet Dent. 2006;95:290–296. doi: 10.1016/j.prosdent.2006.02.026. [DOI] [PubMed] [Google Scholar]