Abstract
There is limited information about the nature of anxiety among youth with symptoms of autism spectrum disorder (ASD). The present study examined (a) differences in the clinical characteristics of anxious youth with and without symptoms of ASD and (b) the symptoms of anxiety that best distinguish between these groups. Results indicated that anxious youth with elevated ASD symptoms had significantly more diagnoses (e.g., specific phobias), and were more likely to meet diagnostic criteria for social phobia (and list social concerns among their top fears) than youth without elevated ASD symptoms. At the symptom level, severity of interpersonal worry based on parent report and severity of fear of medical (doctor/dentist) visits based on youth report best differentiated ASD status. The findings inform diagnostic evaluations, case conceptualization, and treatment planning for youth with anxiety disorders and ASD symptoms.
Keywords: child anxiety disorders, autism spectrum disorders, comorbidity, anxiety symptoms, distinguishing characteristics
1. Introduction
Anxiety is among the most common psychopathologies in childhood, with prevalence rates ranging from approximately 3% to 24% in community samples (see Cartwright-Hatton, McNicol, & Doubleday, 2006 for a review) and varying from 5.7% to as high as 57.7% among youth in clinical settings (e.g., Esbjørn, Hoeyer, Dyrborg, Leth, & Kendall, 2010; Hammerness et al., 2008; Weiss & Last, 2001). A recent study on lifetime prevalence of mental disorders among adolescents in the United States indicated that nearly 1 in 3 adolescents met criteria for an anxiety disorder (Merikangas et al., 2010). Autism spectrum disorders (ASDs), which are characterized by deficits in social interaction and communication, and the presence of restricted interests or stereotyped behavior (American Psychiatric Association, 2000), are one of the more common, serious developmental disabilities, affecting as many as 1 in 91 children (1 in 58 boys) in the United States (Centers for Disease Control and Prevention, 2007; Fombonne, 2005; Kogan et al., 2009). Research suggests anxiety and ASD often co-occur: anxiety is substantially more common among children with ASD relative to their typically developing peers (e.g., Bellini, 2004; Guttmann-Steinmetz, Gadow, DeVincent, & Crowell, 2010; Russell & Sofronoff, 2005). Approximately 42-55% of youth with ASD meet criteria for an anxiety disorder (White, Oswald, Ollendick, & Scahill, 2009) and as many as 62% of youth with mood or anxiety disorders show elevated autism spectrum traits (Constantino et al., 2006; Pine, Guyer, Goldwin, Towbin, & Leibenluft, 2008; Towbin, Pradella, Gorrindo, Pine, & Leibenluft, 2005).
Although anxiety symptoms have been observed across the full spectrum of autism impairment, they may be particularly pronounced in youth with milder ASDs. Several studies suggest that children with Asperger’s syndrome and pervasive developmental disorder-not otherwise specified (PDD-NOS), ASDs characterized by higher adaptive functioning and less cognitive impairment, may experience greater anxiety than more severely affected children (Muris, Steerneman, Merckelbach, Holdrinet, & Meesters, 1998; Thede & Coolidge, 2007; Weisbrot, Gadow, DeVincent, & Pomeroy, 2005). Given evidence that higher functioning youth with ASD often experience distressing symptoms of anxiety, along with research suggesting that ASD symptoms are continuously distributed in the general population (Constantino & Todd, 2003), it is likely that a substantial number of children who present for treatment of anxiety disorders will also exhibit ASD traits that may influence their responsiveness to treatment (e.g., Puleo & Kendall, 2011).
Studies have explored anxiety in children with ASD (see Puleo & Kendall, 2012 and White et al., 2009 for reviews), with anxiety-related concerns identified as one of the most common presenting problems for youth with ASD in clinical settings (Ghaziuddin, 2002), but few have considered the prevalence and ramifications of subthreshold autism spectrum symptoms in children with anxiety disorders. When they have been examined, autism spectrum symptoms have typically been measured in mixed samples, including children with anxiety, bipolar disorder and depression (e.g., Towbin et al., 2005), or an even broader range of non-ASD psychiatric conditions (Constantino et al., 2006). Though these studies suggest that children with non-ASD psychopathology may still demonstrate elevated autism spectrum symptoms, the specific relationship between anxiety disorders and autism spectrum symptoms remains unclear. Few studies have assessed the prevalence of these features in youth with principal anxiety disorders (as opposed to general psychopathology), and none have considered the presentation of anxiety in these youth (Constantino et al., 2006). Rather, such questions have previously been limited to studies of anxiety in children who meet full diagnostic criteria for ASD.
Questions remain regarding the nature, expression, and diagnostic classification of anxiety in children with ASD (Puleo & Kendall, 2012, White et al., 2009; Wood & Gadow, 2010), as both ASD and deficits associated with ASD may influence the presentation of anxiety. Wood and Gadow (2010) proposed that core ASD symptoms can lead to stressful experiences that generate anxiety. Expression of ASD symptoms, such as preferences to engage in preferred routines, or sensory sensitivities, may conflict with social expectations and lead to negative reactions from others (Bellini, 2004; 2006; Gillott & Standen, 2007; Goodwin, Groden, Velicer, & Diller, 2007). Social interactions may be particularly confusing and unpredictable to individuals with ASD who struggle to understand and anticipate the emotional states and intentions of others (e.g., Baron-Cohen, Leslie, & Frith, 1985; Baron-Cohen & Wheelwright, 2004; Demurie, De Corel, & Roeyers, 2011). Given the special stressors experienced by youth with ASD, the presentation of anxiety among these youth may differ from that of their typically developing peers, and such differences may also be apparent in anxious youth with subthreshold ASD features. Although the current study explores subthreshold ASD symptoms among youth with a principal anxiety disorder, the literature available for review largely focused on youth who meet full diagnostic criteria for ASD.
1.1. Anxiety Presentation Among Youth with ASD
Research on anxiety in children with ASD may guide hypotheses regarding the clinical presentations of anxious youth with ASD features. Previous studies suggest that ASD children may show a different pattern of anxiety than anxious youth without ASD. Children with ASD meet diagnostic criteria for specific phobias (e.g., Mattila et al., 2010; Sukhodolsky et al., 2008) at a substantially higher rate than the 3.5-7.9% prevalence reported in community samples (e.g., Essau, Conradt, & Petermann, 2000; Kim et al., 2010). Research also suggests variation in the frequency of particular types of specific phobias. Children with ASD have been found to have more parent-reported physical injury fears compared to typically developing anxious youth, a pattern that may be explained by a heightened sensitivity to noise and touch among youth with ASD (Russell & Sofronoff, 2005). When compared to youth with Down Syndrome, mentally age-matched children, and chronologically age-matched children, ASD youth were more fearful of specific situations and had more medical fears based on parent-reports (Evans, Canavera, Kleinpeter, Maccubbin, & Taga, 2005). Leyfer and colleagues (2006) found that the most common DSM-IV lifetime diagnosis in their sample of ASD children was specific phobia, with 44% meeting diagnostic criteria. They also reported fear of needles and/or shots and crowds as the most common specific phobias, whereas phobias typically observed among children in the general population (e.g., fears of flying, bridges, tunnels) occurred at very low rates, again suggesting a different presentation of specific phobias among ASD youth. In addition, more than 10% of youth with ASD in the Leyfer et al. (2006) study met criteria for a specific phobia of loud noises. Given that heightened sensitivity to environmental stimulation and difficulties in sensory modulation are related to anxiety in individuals with ASD (Green & Ben-Sasson, 2010; Pfeiffer Kinnealey, Reed, & Herzberg, 2005), it is not surprising that specific phobias involving adverse sensory stimulation more commonly arise among these youth. Differences in the somatic expression and severity of anxiety in ASD youth have also been noted, with some studies suggesting that ASD youth display more difficulty controlling their worries and more severe overall anxiety, despite fewer physiological symptoms of anxiety (Helverschou & Martinsen, 2011; Russell & Sofronoff, 2005; Weisbrot et al., 2005).
Research on social phobia among ASD youth has yielded mixed results, and studying characteristics of ASD within anxiety disorders may add clarification. Some studies suggest social concerns are among the more common sources of anxiety for children with ASD (Farrugia & Hudson, 2006; Sukhodolsky et al., 2008; Weisbrot et al., 2005), and it has been speculated that social phobia may be particularly prevalent in ASD youth with higher cognitive abilities given the substantial social impairments inherent to ASDs (Attwood, 2000). However, other research suggests that diagnosis of social phobia among ASD youth may be primarily based on avoidance of social situations rather than interpersonal concerns per se (Leyfer et al., 2006). It is unclear whether the lower rate of friendships among individuals with ASD is due to a lack of desire for social relationships or deficits in skills needed to form and maintain these relationships (Mesibov, Schopler, Schaffer, & Michal, 1989; Orsmond, Krauss, & Seltzer, 2004; Rutter, 1970), a confusion that may also complicate social phobia diagnosis in youth with ASD symptoms. Though it is sometimes assumed that youth with ASD prefer not to engage in social interactions, many individuals with ASD are acutely aware of and distressed by their social difficulties (Attwood, 2000). High functioning ASD youth have been found to report more social worries and social anxiety (Burnette et al., 2005; Gillott, Furniss, & Walter, 2001; Kuusikko et al., 2008), and have significantly higher social phobia severity ratings compared to non-ASD youth (Gadow, DeVincent, Pomeroy, & Azizian, 2005). Recent research suggests that adults with PDD desire social interactions; however, they experience increases in negative affect and anxiety in the presence of less familiar people, akin to the experience of individuals with social anxiety (Hintzen, Delespaul, van Os, & Myin-Germeys, 2010). It is possible that anxiety compounds the overall social impairment associated with ASD, and the social difficulties associated with ASD produce anxiety (White et al., 2009). This may be particularly true among higher functioning children or children with autism spectrum deficits who lack a formal diagnosis, as these youth are more likely to have awareness of their social deficits.
Concerns have been raised regarding the ability of current diagnostic systems to accurately characterize anxiety in ASD youth. Confusion regarding substantial symptom overlap between ASD and anxiety disorders as well as a lack of clearly defined criteria for differential diagnosis has contributed to inconsistencies in the reported prevalence of many anxiety disorders in this population (Puleo & Kendall, 2012; White et al., 2009). Core symptoms of ASD may be misidentified as co-occurring anxiety, particularly for social phobia (Wood & Gadow, 2010). Conclusions regarding differential rates of anxiety diagnoses among ASD youth remain unclear. For example, some studies suggest that children with ASD experience generalized anxiety disorder (GAD) at rates higher than that found in the general population, with 9.4% to 22.7% of the samples examined meeting diagnostic criteria (Gadow et al., 2005; Kim, Szatmari, Bryson, Streiner, & Wilson, 2000; Muris et al., 1998; Simonoff et al., 2008; Sukhodolsky et al., 2008). However, Leyfer and colleagues (2006) found only a 2.4% rate of GAD in their sample of ASD children. The classification of anxiety among children with ASD may also be complicated by the difficulty these youth have reporting their anxiety symptoms, as they may lack insight into their internal feelings and anxious thoughts even though they can describe overt signs of anxiety when asked (White et al., 2009).
Although there is evidence to suggest that anxiety manifests differently in children with ASD, some research suggests the contrary; that is, youth with ASD seem to experience similar anxiety symptoms as typically developing youth, with presentation of symptoms affected primarily by age and cognitive functioning (Mayes, Calhoun, Murray, Ahuja, & Smith, 2011; Weisbrot et al., 2005). White and colleagues (2009) noted that although the developmental progression of anxiety symptoms in ASD youth may closely resemble that of non-ASD youth, the presentation of these symptoms nonetheless differs in other respects, such as association with sensory sensitivities and lack of emotional insight. The lack of agreement across studies underscores the need for further research. An empirically based understanding of the overlapping anxiety and ASD spectrums is needed to inform assessment, case conceptualization and effective treatment planning (White et al., 2009), particularly among children identified with principal anxiety disorders, for whom research remains comparatively scarce.
1.2. The Present Study
The present study explored the characteristics and symptomatology of anxious youth with ASD traits. In particular, the clinical diagnoses, severity of symptoms of depression, and coping ability of youth with and without elevated levels of ASD symptoms were compared. Depressive symptomatology and coping ability were examined given that previous research has explored elevated ASD symptoms in youth with broad mood disorders (Pine et al., 2008; Towbin et al., 2005), and these constructs are often explored in studies of youth with anxiety disorders (e.g., Beidel et al., 2007; Hirshfeld-Becker et al., 2010; Kendall et al., 1997; Kendall, Hudson, Gosch, Flannery-Schroeder, & Suveg, 2008; Walkup et al., 2008) as common, co-occurring characteristics of anxious youth with implications for anxiety presentation and treatment (Crawley, Beidas, Benjamin, Martin, & Kendall, 2008; Kendall, 1992; Southam-Gerow, Kendall, & Weersing, 2001). It was hypothesized that patterns of anxiety reported in previous research with ASD youth would be reflected in youth with moderate, but subthreshold symptoms of the disorder in the current study. Specifically, anxious youth with elevated ASD symptoms were expected to present with more social and specific phobias, and a greater number of diagnoses overall. In addition, at the symptom level and as an exploratory aim, we examined symptoms that best distinguish between children with and without ASD traits.
2. Method
2.1. Participants
Participants were 100 youth (aged 7–16) who presented for treatment at an anxiety disorders outpatient clinic (n = 33) or who participated in a randomized clinical trial (RCT) evaluating cognitive-behavioral therapy (n = 67; Kendall et al., 2008). Parents of youth who participated in the RCT were recontacted to complete an additional measure for the purposes of the current study and all reachable families agreed to participate. Participant children had met criteria for a principal diagnosis of GAD (n = 46), social phobia (n = 30), separation anxiety disorder (SAD; n = 23), or specific phobia (n =1). Comorbidity was common: 27% of children were comorbid with GAD, 32% with SAD, 39% with social phobia, 36% with specific phobia, 23% with attention-deficit/hyperactivity disorder (ADHD), 8% with oppositional defiant disorder, 8% with dysthymia, and 5% with major depressive disorder. This high degree of comorbidity is consistent with rates found in other samples of youth with anxiety disorders (e.g., Kendall et al., 2010). Youth with a pre-existing ASD diagnosis based on parent report and youth whose principal diagnosis was not an anxiety disorder were not included. Fifty-five percent of the children were male. Regarding race, 91% were Caucasian, 6% were African American, and 3% identified as “other” or mixed race. Children aged 7-11 years comprised 67% of the sample, and the remaining 33% were 12-16 years old (mean age = 10.57, SD = 2.38). Family income was reported as below $20,000 (1.1%), up to $40,000 (8.4%), up to $60,000 (16.9%), up to $80,000 (26.3%), and above $80,000 (47.4%). Fathers’ and mothers’ education level was reported as did not complete high school (2% and 1%, respectively), high school graduates without college (22% and 20%), some college education (20% and 15%), completed a 4-year college (34% and 37%), attended graduate school (21% and 25%), or “other” (1% and 2%).
2.2. Measures
Anxiety Disorders Interview Schedule for Children (ADIS-C/P; Silverman & Albano, 1996)
The ADIS-C/P is a semi-structured interview that assesses DSM-IV anxiety disorders in youth. Interviews are independently administered to parent and child, and combined for a composite report using the either/or rule, such that diagnoses are assigned if either the parent or child reports a disorder of clinical severity. Interviewers provide clinician severity ratings (CSRs) for each diagnosis on a 0-8 scale (≥ 4 required for a diagnosis). Studies indicate favorable psychometrics (March & Albano, 1998), including high inter-rater reliability (Chavira, Stein, Bailey, & Stein, 2004; Lyneham, Abbott, & Rapee, 2007), retest reliability (Silverman, Saavedra, & Pina, 2001), convergent validity (Wood, Piacentini, Bergman, McCracken, & Barrios, 2002), and sensitivity to treatment (e.g., Kendall et al., 2008). Interviewers for the RCT and outpatient clinic were required to meet inter-rater reliability of 0.85 (Cohen’s κ). Diagnoses and symptoms of GAD, SAD, social phobia, and specific phobias recorded during the ADIS-C/P administration were examined.
Social Responsiveness Scale – Parent Version (SRS-P; Constantino & Gruber, 2005)
The 65-item SRS-P is a commonly used parent-report measure of ASD symptoms (e.g., Pine et al., 2008; Puleo & Kendall, 2011; Reiersen et al., 2008; Towbin et al., 2005). The SRS-P measures the social deficits characteristic of ASD that are relatively independent of other psychopathology and IQ (Constantino et al., 2003) and has been studied among youth with principal anxiety disorders (Pine et al., 2008). Parents rate their child from “0” (never true) to “3” (almost always true), on observed aspects of routine reciprocal social behavior and autistic preoccupations. Scores on this measure range from 0 to 195 with higher scores indicating greater social impairment. Of importance for this study, scores in the moderate range (standardized scores from 60 to 75) are stated as reflective of clinically significant deficits in reciprocal social behavior and characterize youth with mild or high functioning autism spectrum conditions or symptoms that might complicate other, more salient psychiatric difficulties. More severe scores are associated with more pronounced ASDs and substantial social interference (Constantino & Gruber, 2005). The SRS has high retest reliability (r = .83; Constantino et al., 2003), inter-rater reliability (between parents, r = .91; Constantino et al., 2003), and internal consistency (Cronbach’s alpha = .97; Constantino & Gruber, 2005). Internal consistency in this sample was excellent (Cronbach’s alpha = .92). The SRS has shown convergent validity with the Autism Diagnostic Interview-Revised (ADI-R; r = .7; Lord, Rutter, & Couteur, 1994; Constantino et al., 2003).
Multidimensional Anxiety Scale for Children (MASC; March, Parker, Sullivan, Stallings, & Conners, 1997)
The MASC is a 39-item parent- and child-report that assesses children’s anxiety symptoms. The scale assesses four factors: physical symptoms, social anxiety, harm avoidance, and separation anxiety, and yields an overall anxiety score. The scale asks children to report how they have been thinking, feeling, or acting over the last 2 weeks on a scale of 1 (never) to 4 (often). The MASC demonstrates solid psychometric properties, including internal consistency (α = .86), convergent validity (March & Albano, 1998; March et al., 1997; Wood et al., 2002), diagnostic discrimination (Villabø, Gere, Torgersen, March, & Kendall, 2012), test-retest reliability (March, Sullivan, & Parker, 1999), and treatment sensitivity (Walkup et al., 2008). Internal consistency of the MASC was found to be excellent in this sample (Cronbach’s alpha = .91).
Coping Questionnaire – Child and Parent (CQ-C/P; Kendall & Marrs-Garcia, 1999)
The CQ-C/P assesses child- and parent-perceptions of a child’s ability to cope with anxious distress in three challenging situations. The child and parent independently rate the child’s ability to cope with situationally-based and individualized areas of difficulty (coping scenarios), which the child identifies as feared situations at the conclusion of the diagnostic interview (rated on a scale from 1, “not at all able to help” to 7, “totally able to help myself”). The three items are summed for a total score. Analyses indicate adequate internal consistency, strong retest reliability, moderate interrater agreement, and sensitivity to treatment (Kendall et al., 2008).
Children’s Depression Inventory (CDI; Kovacs, 1985; 1992)
The 27-item CDI measures self-reported cognitive, affective, and behavioral symptoms of depression. Internal consistency, moderate retest reliability, and convergent validity have been demonstrated (Ivarsson, Svalander, & Litlere, 2006; Kovacs, 1992; Masip, Amador-Campos, Gómez-Benito, & del Barrio Gándara, 2010). In this sample, the internal consistency of the CDI was .88 (Cronbach’s alpha).
Children’s Global Assessment Scale (CGAS; Shaffer et al., 1983)
The CGAS is a clinician rating of children’s global functioning across settings. Ratings take into account the child’s functioning at home and school, and the nature and quality of the child’s peer relationships. Scores range from 0 to 100, with lower scores reflecting greater impairment. The CGAS has adequate inter-rater reliability (Dyrborg et al., 2000; Shaffer et al., 1983), retest reliability (Bird, Canino, Rubio-Stipec, & Ribera, 1987), sensitivity to change over time (e.g., Findling et al., 2003), and discriminant validity (Steinhausen & Metzke, 2001). Inter-rater reliability for the CGAS among diagnosticians in the clinic was found to be acceptable (intraclass correlation = .73).
2.3. Statistical Analyses
Consistent with the characterizations associated with the SRS-P, children with a T-score ≥ 60 on the SRS-P were considered to have elevated levels of ASD symptoms. The clinical characteristics of youth with and without elevated ASD symptoms were examined using ANOVA, t-test, and chi-square analyses. To explore how symptoms of anxiety differ among youth with and without ASD traits, data were analyzed using recursive partitioning (RP), a type of exploratory decision tree analysis (Zhang & Singer, 1999) developed for disease diagnosis and treatment (Breiman, Freidman, Olshen, & Stone, 1984; Zhang & Singer, 1999). RP is an appropriate statistical analysis to determine which anxiety symptoms assessed by the ADIS distinguish between youth with and without elevated levels of ASD symptoms. RP is a nonparametric data mining procedure that builds a “tree” that identifies exhaustive orthogonal subgroups of a population, called “nodes”, whose members share common characteristics that influence the dependent variable (Lemon, Roy, Clark, Friedmann, & Rakowski, 2003). The data are then split into smaller and smaller nodes using a recursive procedure until each group is perfectly homogenous. This recursive splitting takes place separately for each “branch” of the tree. RP allows for analysis of highly dimensional and highly correlated data in small samples (Breiman et al., 1984; Strobl, Malley, & Tutz, 2009) and addresses the problem of analyzing highly dimensional data by reducing it to a series of one-dimensional problems to identify a parsimonious set of predictor variables that is sufficient to predict the outcome (i.e., differentiating between those with and without elevated ASD symptoms).
The resulting RP tree is both a reflection of the properties of the underlying population and the random features of the specific sample from which it was derived. Because of this, the final model is often overfit to the specific sample and not necessarily representative of the underlying population. The goal, however, is to specify a model that will be applicable to any random sample from the population. The second stage of the RP procedure consists of using cross validation to prune the full tree to an “appropriate size” to reach this goal. When a new dataset is not available to conduct confirmatory testing on the tree, resampling the original sample, or bootstrapping, is used to create samples to conduct confirmatory tests of the tree. The bootstrap cross-validation procedure estimates the cross-validated prediction error, and related standard error, for different numbers of splits. Breiman et al. (1984) suggested using a ±1 standard error rule to choose appropriate tree size. In other words, a good-fitting tree is one with the least number of splits and the smallest cross-validation error, given that the tree’s cross-validation error plus its standard error is less than 1 (per definition, the relative error of a model with no splits).
The cross-validation error rate and associated variability (standard error of the cross-validation rate) are comparable to the estimate of explained variance (1 - R2) and a confidence interval around it in an ANOVA framework (Hellemann, Conner, Anglin, & Longshore, 2009). In other words, saying that a tree that has a cross-validation error rate = 0.70 with a standard error = .05 is similar to saying that in 95% of samples, 25% to 35% of the variance is explained by the tree. The relative error of the sample used to estimate the initial tree, or the relative error, is interpreted as 1 - relative error = variance explained in the original sample. In other words, a relative error = .65 indicates that the tree explains 35% of the variance in the original sample.
In this study, the size of the terminal nodes was set at 5 to avoid comparisons among groups that are too small to be clinically meaningful. The cross validation was based on 100 bootstrapped samples. The rpart package version 3.1-46 (Therneau & Atkinson, 2010), as implemented in version 2.11.1 of the R software package, was used to estimate the RP trees.
3. Results
3.1. Characteristics of Youth with Elevated ASD Symptoms
Youth with meaningful ASD symptoms (T-scores ≥ 60 on the SRS-P) comprised 42% of the sample. No significant differences were found between youth with or without elevated ASD symptoms with respect to their age, sex, race, parental education or SES. In terms of diagnostics, youth with elevated ASD symptoms had significantly more diagnoses relative to youth without elevated ASD symptoms, t(98) = -2.08, p = .04, though no differences were evident in their principal diagnoses (Table 1). Youth with elevated ASD symptoms were significantly more likely to meet diagnostic criteria for social phobia than youth without ASD symptoms, χ2 (1, N = 100) = 4.84, p = .03, and had significantly more specific phobias than youth without elevated ASD symptoms, t(98) = -2.09, p = .04, though both groups were equally likely to meet criteria for at least one specific phobia diagnosis. That is, though youth with elevated ASD symptoms had a significantly greater number of specific phobias than youth without elevated ASD symptoms, the likelihood that an individual from either group would meet criteria for one specific phobia was not significantly different. Youth with ASD symptoms were not more likely to have multiple anxiety disorders or to be diagnosed with GAD, SAD, panic disorder, obsessive-compulsive disorder (OCD), ADHD, a specific phobia, an externalizing disorder (either oppositional defiant disorder or conduct disorder), or a unipolar mood disorder (either dysthymia or major depressive disorder) relative to youth without elevated ASD symptoms.
Table 1.
Differences in Diagnoses by ASD Symptom Level (N = 100)
| Diagnostic Variable | SRS-P Category
|
Significance Test | |
|---|---|---|---|
| Typical (SD or %) N = 58 | Elevated ASD Symptoms (SD or %) N = 42 | ||
| Total Number of Youth Diagnoses | 2.95 (1.43) | 3.59 (1.67) | t(98) = -2.08* |
| Presence of GAD Diagnosis | 43 (74%) | 29 (69%) | χ2 (1, N = 100) = .31 |
| Presence of SAD Diagnosis | 32 (55%) | 21 (50%) | χ2 (1, N = 100) = .26 |
| Presence of Social Phobia Diagnosis | 35 (60%) | 34 (81%) | χ2 (1, N = 100) = 4.84* |
| Total Number of Specific Phobias | .38 (.59) | .69 (.90) | t(98) = -2.10* |
| Principal Diagnoses | |||
| GAD | 36 (62%) | 23 (55%) | χ2 (1, N = 100) = .54 |
| SAD | 15 (29%) | 13 (34%) | χ2 (1, N = 100) = .66 |
| Social Phobia | 20 (35%) | 18 (43%) | χ2 (1, N = 100) = .73 |
| Comorbid Diagnoses | |||
| ADHD | 12 (21%) | 13 (31%) | χ2 (1, N = 100) = 1.37 |
| Mood Disorder | 7 (12%) | 10 (24%) | χ2 (1, N = 100) = 2.38 |
| Specific Phobia | 19 (33%) | 19 (45%) | χ2 (1, N = 100) = 1.61 |
| OCD | 3 (5%) | 3 (7%) | χ2 (1, N = 100) = 1.68 |
| Externalizing Disorders | 3 (5%) | 6 (14%) | χ2 (1, N = 100) = 2.47 |
| Panic Disorder | 5 (9%) | 2 (5%) | χ2 (1, N = 100) = .56 |
Note. ASD = Autism Spectrum Disorder; SRS-P = Social Responsiveness Scale – Parent Version; GAD = generalized anxiety disorder; SAD = separation anxiety disorder.
p < .05.
Regarding the severity of internalizing pathology, youth with elevated ASD symptoms were not rated as having more severe principal anxiety diagnoses than youth without elevated ASD symptoms.1 Similarly, CGAS scores based on information gathered from the parent and child diagnostic interviews were also not significantly different between groups. No significant differences were evident in mean total scores or on mean subscale scores of the MASC, including: physical symptoms, harm avoidance, social fear and separation anxiety. Depressive symptomatology (total scores on the CDI) as reported by youth was also undifferentiated by ASD symptom status.
Analyses of differences in coping skills and scenarios revealed that youth with elevated ASD symptoms were significantly more likely to list social/evaluation concerns (as opposed to academic/performance concerns, separations concerns, specific fears, or fears of physical danger) among their top three fears on the CQ-C/P than youth without such deficits, controlling for a diagnosis of social phobia, χ2 (2, N = 100) = 7.18, p = .01; Nagelkerke R2 = .31. No significant differences were evident in the likelihood of listing a specific phobia-related scenario (e.g., fear of doctor, dogs, heights) among the top three fears or in the total number of specific phobia-related situations listed by youth with and without elevated ASD symptoms on the CQ-C/P. There were also no significant differences in mean coping scores as rated by parents or children in the high and low ASD symptom groups.
3.2. Symptoms of Anxiety Associated with Elevated ASD Symptoms
RP results are depicted in Figure 1. All symptoms (i.e., presence of a symptom, severity ratings, and avoidance) from the SAD, social phobia, GAD, and specific phobia modules of the ADIS-C/P, as well as the presence of any diagnosis were entered into the model, for a total of 398 potential predictors. It is important to note that in RP analyses, variables are solely identified as salient rather than as significant predictors of outcome. As such, the variables that are identified are those whose values an individual would need to know to potentially best predict outcome. Thus, it is more important to evaluate model fit rather than the number of variables identified given that the results do not suggest that the predictors identified are the only “significant” predictors of outcome as is generally conceptualized within a regression framework.
Figure 1.
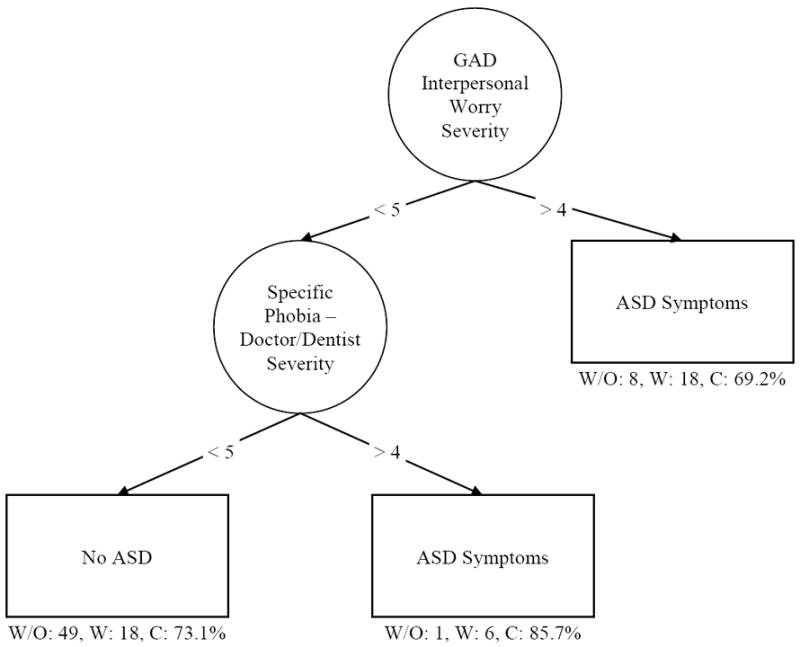
Final decision tree depicting the prediction of elevated or non-elevated levels of ASD symptoms. The model had a relative error = 0.64 and a cross validation error = 0.71 (SE = 0.11). Circles represent nodes and squares represent the outcome variable. Numbers on the lines represent the cut-points on the variables of interest that define the split (i.e., individuals whose score is > 4 on severity of interpersonal worry from the GAD section of the parent ADIS are split to the right, or the elevated ASD symptoms, side of the tree). Noted below each terminal node are the number of participants without elevated ASD symptoms (W/O), the number with elevated ASD symptoms (W), and the percentage of participants the tree classified correctly (C). Estimation was based on 100 participants and 398 variables.
The results revealed that the final tree explained 36% of the variance in the original sample (relative error = 0.64) and between 18% and 40% of the variance in random samples drawn from the population (cross validation error = 0.71, standard error = 0.11), indicating that the overall fit of the model was good. The proportion of variance explained by the model increases with every parameter that is added to the model (Strobl, Malley & Tutz, 2009); thus the final tree, which was based on two predictors, explained a meaningful portion of the variance. The best predictor of elevated ASD symptoms was severity of interpersonal worry from the GAD section (score > 4) of the parent ADIS. Individuals with an interpersonal worry severity score less than 5 were less likely to have elevated ASD symptoms, unless they had a score greater than 4 on the severity of specific phobia of the doctor/dentist (medical visits) based on the child ADIS. Severity of fear of medical visits was the best predictor of elevated ASD symptoms only in individuals with an interpersonal worry severity score less than 5. Having a score of less than 5 on severity of interpersonal worry from the GAD section of the parent ADIS and a score of less than 5 on severity of specific phobia of the doctor/dentist from the child ADIS was the best predictor of not having elevated ASD symptoms.
4. Discussion
Forty-two percent of youth presenting for treatment of principal anxiety disorders demonstrated clinically relevant levels of ASD symptoms according to parent report. The diagnoses and presentations of youth with ASD symptoms largely resembled those of youth without elevated ASD symptoms, with the following exceptions. Youth with elevated ASD symptoms had more diagnoses and were more likely to meet diagnostic criteria for social phobia, though social phobia was not more likely to be their principal diagnosis. Furthermore, even after controlling for a social phobia diagnosis, youth with elevated ASD symptoms were more likely to list social concerns among their top fears than youth without such symptoms. These findings are consistent with the elevated rates of social worry reported by ASD youth and their parents, particularly when cognitive impairments are minimal (e.g., Bellini, 2004; Kuusikko et al., 2008).
Consistent with previous research indicating that ASD youth have a higher rate of specific phobias than youth in the general community (e.g., Gadow et al., 2005; Mattila et al., 2010; Sukhodolsky et al., 2008), youth with elevated ASD symptoms were found to have significantly more specific phobias than those without elevated ASD symptoms. These distinctions are informative, but the dearth of diagnostic differences between groups suggests that children with elevated ASD symptoms are not easily distinguished from children without these deficits, an ambiguity that warrants attention given that children with ASD traits have differential responses to particular modalities of cognitive behavioral therapies (Puleo & Kendall, 2011).
RP revealed that ASD symptoms were best predicted by having a GAD interpersonal worry severity score greater than 4 on the parent ADIS, a finding that reflects that youth with elevated ASD symptoms were best distinguished from youth without such elevations by parent impressions of their child’s interpersonal worry. For youth with a parent-reported GAD interpersonal worry severity score less than 5, having a score greater than 4 on the severity of fear of the doctor/dentist based on the specific phobia module of the child ADIS was the best predictor of elevated ASD symptoms. In other words, if parents did not report severe interpersonal worry, youth with ASD symptoms could still be distinguished by higher child-reported fear of going to the doctor or dentist. Notably, these two symptoms distinguished between youth with and without symptoms of ASD better than the presence of any diagnosis obtained from the ADIS-C/P. RP identified GAD interpersonal worry and fear of medical visits as the best from a set of 398 possible predictors, suggesting that these are salient predictors of elevated ASD symptoms that can facilitate clinicians’ ability to identify children with elevated ASD symptoms among youth presenting for treatment of anxiety disorders in the absence of an ASD-specific assessment.
It is important to note that GAD interpersonal worry is somewhat distinct from the social fears characteristic of social phobia. Social phobia is primarily associated with fear of not meeting the standards set by others; by contrast, GAD is usually associated with self-imposed standards (i.e., having high standards for oneself). GAD worry about interpersonal matters focuses on worries children have about the impression they make on others, their appearance, being a good friend, and having enough friends rather than fears of rejection or negative evaluation from others in the presence or anticipated presence of others (Albano & Silverman, 1996). The GAD interpersonal worry item therefore assesses the extent to which children worry about not being good enough interpersonally rather than fear of and distress related to being in certain social situations.
The question of whether youth with ASD are aware of and distressed by worries of an interpersonal nature remains unclear. Youth with ASD symptoms presenting to a primary anxiety disorders clinic tend to be high functioning and lack severe cognitive impairments; thus, they may have better awareness of their social skills deficits relative to the broader ASD population. Alternatively, it may be that parents believe their children are worrying about interpersonal matters because this is likely to be an area of weakness when in fact these youth are not concerned about the implications of their social skills deficits. Such an explanation would be consistent with theories that autism spectrum deficits are related to a reduced desire for and competence in social interaction. As noted by Wood and Gadow (2010) and Puleo and Kendall (2012), instruments for the assessment of anxiety disorders may misattribute ASD-related impairment to anxiety. Impairments in areas such as peer relationships may be attributed to anxiety based on current anxiety instruments, yet the central problem may be ASD-related social deficits. This view is consistent with the finding that ASD children are less likely to meet criteria for social phobia if assessment items focus on interpersonal concerns rather than avoidance (Leyfer et al., 2006).
However, other research suggests that youth with ASD, particularly high-functioning children who have awareness of how they are different from their peers, are concerned about such interpersonal matters (e.g., Farrugia & Hudson, 2006; Sukhodolsky et al., 2008). There is evidence that individuals with ASD desire social relationships, yet lack friendships due to feelings of anxiety and depression that occur in the presence of less familiar people (Hintzen et al., 2010). Parent-reported severity of interpersonal worry may therefore reflect the presence of this type of worry among high functioning children with elevated ASD symptoms. The current findings are consistent with previous research suggesting parent report of their child’s social worries is higher than child self-report among ASD youth, perhaps signifying that parent reports are more accurate in this domain because these youth lack understanding about the connection between social deficits and anxiety (Russell & Sofronoff, 2005). Taken together with the finding that youth with elevated ASD symptoms in this sample were more likely to identify social concerns as one of their top fears, it seems likely that these children were experiencing high levels of worry regarding interpersonal matters. It is important to note that regardless of whether parent-report of severity of interpersonal worry reflects true anxiety in this domain as experienced by youth with ASD symptoms, severity on this assessment item can help clinicians identify youth with elevated ASD traits who present to an anxiety outpatient clinic.
Results are also consistent with previous research suggesting youth with ASD have a greater fear of physical injury and medical situations relative to youth without ASD (e.g., Russell & Sofronoff, 2005). In particular, previous studies suggest that the specific phobias apparent among youth with ASD are more likely to involve situations in which sensory stimulation is salient (e.g., receiving needles and/or shots, being in crowds, loud noises; Leyfer et al., 2006). Given that youth with ASD often show heightened sensitivity to environmental stimulation and difficulties in sensory modulation that are related to anxiety (Pfeiffer et al., 2005), these youth may be more likely to show fears of situations involving intense, unwanted sensory stimulation. It is possible that fear of doctor/dentist visits distinguished youth with ASD symptoms in this sample better than fear related to other specific phobias involving sensory stimulation due to the specific sound and touch sensitivities elicited by these visits. Whereas both youth with and without ASD symptoms are commonly distressed by getting a shot or having their blood drawn, youth with ASD symptoms may report relatively more intense fear of going to the dentist or doctor as a result of the unwanted sound and touch stimulation that occurs during these visits (e.g., sound of dental equipment or touch during physical examination) that does not distress youth without ASD symptoms to the same degree. Whether these symptoms warrant a separate diagnosis of specific phobia or are better conceptualized as an ASD-related sensory deficit remains open to question.
Potential study limitations should be noted. Participants did not meet diagnostic criteria for ASD; thus, generalization of these findings to children with more impairing ASD deficits is unclear. Assessment of ASD symptoms was based on parent-report, and multiple method assessment of ASD symptoms would strengthen the conclusions. Participants were mostly Caucasian and middle to upper class; thus, other samples are needed to determine the generalizability to children of other racial and economic backgrounds. The recursive partitioning analyses were exploratory and confirmatory analyses in other samples are needed. Finally, further research on the SRS is needed among youth with anxiety disorders to determine if SRS scores capture symptoms of anxiety that may overlap with ASD.
The current study has several notable clinical implications. The findings confirm that a large percentage of youth presenting for treatment at an anxiety clinic have clinically meaningful symptoms of ASD. The lack of diagnostic differences among these youth suggests that children with elevated ASD symptoms are not easily distinguished from children without such deficits on the basis of anxiety diagnoses alone. However, youth with ASD symptoms can be identified by differences in anxiety symptoms. Children with elevated ASD deficits are less likely to benefit from individual compared to family-based cognitive-behavioral treatments for anxiety disorders relative to children without moderately elevated ASD deficits (Puleo & Kendall, 2011). This differential treatment response underscores the need for early identification of such youth to allow for a more tailored treatment. The present findings suggest an efficient path to help identify and treat youth otherwise at risk for suboptimal treatment outcomes based on differences in anxiety presentation. Specifically, the results suggest that youth with ASD symptoms experience more severe interpersonal worry and fear of medical visits, which are both important treatment targets. Such differences in anxiety symptoms will likely influence the focus of their treatment. The clinical implications of these findings warrant replication and compel further research regarding the presentation of co-occurring anxiety and autism spectrum symptoms in children as well as the development of personalized anxiety interventions for these youth.
Highlights.
> We examined anxiety characteristics associated with autism spectrum (ASD) symptoms. > Youth with elevated ASD symptoms had more diagnoses, particularly specific phobias. > ASD youth were also more likely to meet diagnostic criteria for social phobia. > Interpersonal worry and fear of medical visits best differentiated ASD status. > Findings inform case conceptualization for youth with anxiety and ASD symptoms.
Acknowledgments
This research was supported in part by National Institute of Mental Health Grants (MH59087; MH063747; MH086438) awarded to Philip C. Kendall. We would like to thank Craig C. Matz and Alyssa M. Forgione for their help with this project. Abstract
Footnotes
To further examine the relationship between SRS scores and anxiety severity, we conducted linear regression analyses using continuous SRS scores as the predictor. SRS scores were not significantly related to severity of the child’s principal anxiety disorder, F(1, 98) = .009, p >.05, nor MASC total scores, F(1, 96) = .075, p >.05, consistent with initial findings that ASD status (using a cut off score of ≥ 60 on the SRS) was unrelated to anxiety severity.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Albano AM, Silverman WK. Clinician’s guide for the Anxiety Disorders Interview Schedule for DSM-IV, Child Version. San Antonio, TX: The Psychological Corporation; 1996. [Google Scholar]
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 4. Washington, DC: Author; 2000. text revision. [Google Scholar]
- Attwood T. Strategies for improving the social integration of children with Asperger syndrome. Autism. 2000;4:85–100. doi: 10.1177/1362361300004001006. [DOI] [Google Scholar]
- Baron-Cohen S, Leslie AM, Frith U. Does the autistic child have a “theory of mind”? Cognition. 1985;21:37–46. doi: 10.1016/0010-0277(85)90022-8. [DOI] [PubMed] [Google Scholar]
- Baron-Cohen S, Wheelwright S. The empathy quotient: An investigation of adults with Asperger syndrome or high-functioning autism, and normal sex differences. Journal of Autism and Developmental Disorders. 2004;34:163–175. doi: 10.1023/B:JADD.0000022607.19833.00. [DOI] [PubMed] [Google Scholar]
- Beidel DC, Turner SM, Sallee FR, Ammerman RT, Crosby LA, Pathak S. SET-C versus fluoxetine in the treatment of childhood social phobia. Journal of the American Academy of Child and Adolescent Psychiatry. 2007;46:1622–1632. doi: 10.1097/chi.0b013e318154bb57. [DOI] [PubMed] [Google Scholar]
- Bellini S. Social skill deficits and anxiety in high-functioning adolescents with autism spectrum disorders. Focus on Autism and Other Developmental Disabilities. 2004;19:78–86. doi: 10.1177/10883576040190020201. [DOI] [Google Scholar]
- Bird HR, Canino G, Rubio-Stipec M, Ribera JC. Further measures of the psychometric properties of the Children’s Global Assessment Scale. Archives of General Psychiatry. 1987;44:821–824. doi: 10.1001/archpsyc.1987.01800210069011. [DOI] [PubMed] [Google Scholar]
- Breiman L, Freidman JH, Olshen RA, Stone CJ. Classification and regression trees. Belmont, CA: Wadsworth International; 1984. [Google Scholar]
- Burnette CP, Mundy PC, Meyer JA, Sutton SK, Vaughan AE, Charak D. Weak central coherence and its relations to theory of mind and anxiety in autism. Journal of Autism and Developmental Disorders. 2005;35:63–73. doi: 10.1007/s10803-004-1035-5. [DOI] [PubMed] [Google Scholar]
- Cartwright-Hatton S, McNicol K, Doubleday E. Anxiety in a neglected population: Prevalence of anxiety disorders in pre-adolescent children. Clinical Psychology Review. 2006;26:817–833. doi: 10.1016/j.cpr.2005.12.002. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. Prevalence of autism spectrum disorders—autism and developmental disabilities monitoring network, 14 sites, United States, 2002. Morbidity and Mortality Weekly Report Surveillance Summaries. 2007;56:12–28. [PubMed] [Google Scholar]
- Chavira DA, Stein MB, Bailey K, Stein MT. Comorbidity of generalized social anxiety disorder and depression in a pediatric primary care sample. Journal of Affective Disorders. 2004;80:163–171. doi: 10.1016/S0165-0327(03)00103-4. [DOI] [PubMed] [Google Scholar]
- Constantino JN, Davis SA, Todd RD, Schindler MK, Gross MM, Brophy SL, Reich W, et al. Validation of a brief quantitative measure of autistic traits: Comparison of the social responsiveness scale with the autism diagnostic interview–revised. Journal of Autism and Developmental Disorders. 2003;33:427–433. doi: 10.1023/A:1025014929212. [DOI] [PubMed] [Google Scholar]
- Constantino JN, Gruber CP. Social Responsiveness Scale (SRS) Manual. Los Angeles, CA: Western Psychological Services; 2005. [Google Scholar]
- Constantino JN, Lajonchere C, Lutz M, Gray T, Abbacchi A, McKenna K, Todd RD, et al. Autistic social impairment in the siblings of children with pervasive developmental disorders. The American Journal of Psychiatry. 2006;163:294–296. doi: 10.1176/appi.ajp.163.2.294. [DOI] [PubMed] [Google Scholar]
- Constantino JN, Todd R. Autistic traits in the general population: A twin study. Archives of General Psychiatry. 2003;60:524–530. doi: 10.1001/archpsyc.60.5.524. [DOI] [PubMed] [Google Scholar]
- Crawley SA, Beidas RS, Benjamin CL, Martin E, Kendall PC. Treating socially phobic youth with CBT: Differential outcomes and treatment considerations. Behavioral and Cognitive Psychotherapy. 2008;36:379–389. doi: 10.1017/S1352465808004542. [DOI] [Google Scholar]
- Demurie E, De Corel M, Roeyers H. Empathic accuracy in adolescents with autism spectrum disorders and adolescents with attention-deficit/hyperactivity disorder. Research in Autism Spectrum Disorders. 2011;5:126–134. doi: 10.1016/j.rasd.2010.03.002. [DOI] [Google Scholar]
- Dyrborg J, Larsen FW, Nielsen S, Byman J, Nielsen BB, Gautrè-Delay F. The Children’s Global Assessment Scale (CGAS) and Global Assessment of Psychosocial Disability (GAPD) in clinical practice – substance and reliability as judged by intraclass correlations. European Child and Adolescent Psychiatry. 2000;9:195–201. doi: 10.1007/s007870070043. [DOI] [PubMed] [Google Scholar]
- Esbjørn BH, Hoeyer M, Dyrborg J, Leth I, Kendall PC. Prevalence and co-morbidity among anxiety disorders in a national cohort of psychiatrically referred children and adolescents. Journal of Anxiety Disorders. 2010;24:866–872. doi: 10.1016/j.janxdis.2010.06.009. [DOI] [PubMed] [Google Scholar]
- Essau CA, Conradt J, Petermann F. Frequency, comorbidity, and psychosocial impairment of specific phobia in adolescents. Journal of Clinical Child Psychology. 2000;29:221–231. doi: 10.1207/S15374424jccp2902_8. [DOI] [PubMed] [Google Scholar]
- Evans DW, Canavera K, Kleinpeter FL, Maccubbin E, Taga K. The fears, phobias and anxieties of children with autism spectrum disorders and down syndrome: Comparisons with developmentally and chronologically age matched children. Child Psychiatry and Human Development. 2005;36:3–26. doi: 10.1007/s10578-004-3619-x. [DOI] [PubMed] [Google Scholar]
- Farrugia S, Hudson J. Anxiety in adolescents with Asperger syndrome: Negative thoughts, behavioral problems, and life interference. Focus on Autism and Other Developmental Disabilities. 2006;21:25–35. doi: 10.1177/10883576060210010401. [DOI] [Google Scholar]
- Findling RL, McNamara NK, Youngstrom EA, Branicky LA, Demeter CA, Schulz SC. A prospective, open-label trial of olanzapine in adolescents with schizophrenia. Journal of the American Academy of Child and Adolescent Psychiatry. 2003;42:170–175. doi: 10.1097/00004583-200302000-00010. [DOI] [PubMed] [Google Scholar]
- Fombonne E. Epidemiology of autistic disorder and other pervasive developmental disorders. Journal of Clinical Psychiatry. 2005;66:3–8. [PubMed] [Google Scholar]
- Gadow KD, DeVincent CJ, Pomeroy J, Azizian A. Comparison of DSM-IV symptoms in elementary school-age children with PDD versus clinic and community samples. Autism. 2005;9:392–415. doi: 10.1177/1362361305056079. [DOI] [PubMed] [Google Scholar]
- Ghaziuddin M. Asperger syndrome: Associated psychiatric and medical conditions. Focus on Autism and Other Developmental Disabilities. 2002;17:138–144. doi: 10.1177/10883576020170030301. [DOI] [Google Scholar]
- Gillott A, Furniss F, Walter A. Anxiety in high functioning children with autism. Autism. 2001;5:277–286. doi: 10.1177/1362361301005003005. [DOI] [PubMed] [Google Scholar]
- Gillott A, Standen PJ. Levels of anxiety and sources of stress in adults with autism. Journal of Intellectual Disabilities. 2007;11:359–370. doi: 10.1177/1744629507083585. [DOI] [PubMed] [Google Scholar]
- Goodwin MS, Groden J, Velicer WF, Diller A. Brief report: Validating the stress survey schedule for persons with autism and other developmental disabilities. Focus on Autism and Other Developmental Disabilities. 2007;22:183–189. doi: 10.1177/10883576070220030501. [DOI] [PubMed] [Google Scholar]
- Green SA, Ben-Sasson A. Anxiety disorders and sensory over-responsivity in children with autism spectrum disorders: Is there a causal relationship? Journal of Autism and Developmental Disorders. 2010;40:1495–1504. doi: 10.1007/s10803-010-1007-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guttmann-Steinmetz S, Gadow KD, DeVincent CJ, Crowell J. Anxiety symptoms in boys with autism spectrum disorder, attention-deficit hyperactivity disorder, or chronic multiple tic disorder and community controls. Journal of Autism and Developmental Disorders. 2010;40:1006–1016. doi: 10.1007/s10803-010-0950-x. [DOI] [PubMed] [Google Scholar]
- Hammerness P, Harpold T, Petty C, Menard C, Zar-Kessler C, Biederman J. Characterizing non-OCD anxiety disorders in psychiatrically referred children and adolescents. Journal of Affective Disorders. 2008;105:213–219. doi: 10.1016/j.jad.2007.05.012. [DOI] [PubMed] [Google Scholar]
- Hellemann GS, Conner BT, Anglin MD, Longshore D. Seeing the trees despite the forest: Applying recursive partitioning to the evaluation of drug treatment retention. Journal of Substance Abuse Treatment. 2009;36:59–64. doi: 10.1016/j.jsat.2008.03.005. [DOI] [PubMed] [Google Scholar]
- Helverschou SB, Martinsen H. Anxiety in people diagnosed with autism and intellectual disability: Recognition and phenomenology. Research in Autism Spectrum Disorders. 2011;5:377–387. doi: 10.1016/j.rasd.2010.05.003. [DOI] [Google Scholar]
- Hintzen A, Delespaul P, van Os J, Myin-Germeys I. Social needs in daily life in adults with pervasive developmental disorders. Psychiatry Research. 2010;179:75–80. doi: 10.1016/j.psychres.2010.06.014. [DOI] [PubMed] [Google Scholar]
- Hirshfeld-Becker DR, Masek B, Henin A, Blakely LR, Pollock-Wurman RA, McQuade J, Biederman J, et al. Cognitive behavioral therapy for 4- to 7-year-old children with anxiety disorders: A randomized clinical trial. Journal of Consulting and Clinical Psychology. 2010;78:498–510. doi: 10.1037/a0019055. [DOI] [PubMed] [Google Scholar]
- Ivarsson T, Svalander P, Litlere O. The Children’s Depression Inventory (CDI) as measure of depression in Swedish adolescents. A normative study. Nordic Journal of Psychiatry. 2006;60:220–226. doi: 10.1080/08039480600636395. [DOI] [PubMed] [Google Scholar]
- Kendall PC. Childhood coping: Avoiding a lifetime of anxiety. Behaviour Change. 1992;9:229–237. [Google Scholar]
- Kendall PC, Compton SN, Walkup JT, Birmaher B, Albano AM, Sherrill J, Piacentini J, et al. Clinical characteristics of anxiety disordered youth. Journal of Anxiety Disorders. 2010;24:360–365. doi: 10.1016/j.janxdis.2010.01.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kendall PC, Flannery-Schroeder E, Panichelli-Mindel SM, Southam-Gerow M, Henin A, Warman M. Therapy for youths with anxiety disorders: A second randomized clinical trial. Journal of Consulting and Clinical Psychology. 1997;65:366–380. doi: 10.1037//0022-006X.65.3.366. [DOI] [PubMed] [Google Scholar]
- Kendall PC, Hudson JL, Gosch E, Flannery-Schroeder E, Suveg C. Cognitive behavioral therapy for anxiety disordered youth: A randomized clinical trial evaluating child and family modalities. Journal of Consulting and Clinical Psychology. 2008;76:282–297. doi: 10.1037/0022-006X.76.2.282. [DOI] [PubMed] [Google Scholar]
- Kendall PC, Marrs-Garcia A. Psychometric analyses of a therapy-sensitive measure: The Coping Questionnaire (CQ) Temple University; 1999. Unpublished manuscript. [Google Scholar]
- Kim S-J, Kim B-N, Cho S-C, Kim J-W, Shin M-S, Yoo H-J, Kim HW. The prevalence of specific phobia and associated co-morbid features in children and adolescents. Journal of Anxiety Disorders. 2010;24:629–634. doi: 10.1016/j.janxdis.2010.04.004. [DOI] [PubMed] [Google Scholar]
- Kim JA, Szatmari P, Bryson SE, Streiner DL, Wilson FJ. The prevalence of anxiety and mood problems among children with autism and Asperger syndrome. Autism. 2000;4:117–132. doi: 10.1177/1362361300004002002. [DOI] [Google Scholar]
- Kogan MD, Blumberg SJ, Schieve LA, Boyle CA, Perrin JM, Ghandour RM, van Dyck PC, et al. Prevalence of parent-reported diagnosis of autism spectrum disorder among children in the US, 2007. Pediatrics. 2009;124:1395–1403. doi: 10.1542/peds.2009-1522. [DOI] [PubMed] [Google Scholar]
- Kovacs M. The Children’s Depression Inventory (CDI) Psychopharmacology Bulletin. 1985;21:995–998. [PubMed] [Google Scholar]
- Kovacs M. The Children’s Depression Inventory (CDI) manual. North Tonawanda, NY: Multi-Health Systems; 1992. [Google Scholar]
- Kuusikko S, Pollock-Wurman R, Jussila K, Carter AS, Mattila M-L, Ebeling H, Moilanen I, et al. Social anxiety in high-functioning children and adolescents with autism and Asperger syndrome. Journal of Autism and Developmental Disorders. 2008;38:1697–1709. doi: 10.1007/s10803-008-0555-9. [DOI] [PubMed] [Google Scholar]
- Lemon SC, Roy J, Clark MA, Friedmann PD, Rakowski W. Classification and regression tree analysis in public health: Methodological review and comparison with logistic regression. Annals of Behavioral Medicine. 2003;26:172–181. doi: 10.1207/S15324796ABM2603_02. [DOI] [PubMed] [Google Scholar]
- Leyfer OT, Folstein SE, Bacalman S, Davis NO, Dinh E, Morgan J, Lainhart JE, et al. Comorbid psychiatric disorders in children with autism: Interview development and rates of disorders. Journal of Autism and Developmental Disorders. 2006;36:849–861. doi: 10.1007/s10803-006-0123-0. [DOI] [PubMed] [Google Scholar]
- Lord C, Rutter M, Couteur A. Autism Diagnostic Interview-Revised: A revised version of a diagnostic interview for caregivers of individuals with possible pervasive developmental disorders. Journal of Autism and Developmental Disorders. 1994;24:659–685. doi: 10.1007/BF02172145. [DOI] [PubMed] [Google Scholar]
- Lyneham HJ, Abbott MJ, Rapee RM. Inter-rater reliability of the anxiety disorders interview schedule for DSM-IV: Child and parent versions. Journal of the American Academy of Child and Adolescent Psychiatry. 2007;46:731–736. doi: 10.1097/chi.0b013e3180465a09. [DOI] [PubMed] [Google Scholar]
- March JS, Albano AM. New developments in assessing pediatric anxiety disorders. Advances in Clinical Child Psychology. 1998;20:213–241. [Google Scholar]
- March JS, Parker J, Sullivan K, Stallings P, Conners C. The Multidimensional Anxiety Scale for Children (MASC): Factor structure, reliability and validity. Journal of the American Academy of Child and Adolescent Psychiatry. 1997;36:554–565. doi: 10.1097/00004583-199704000-00019. [DOI] [PubMed] [Google Scholar]
- March JS, Sullivan K, Parker J. Test-retest reliability of the multidimensional anxiety scale for children. Journal of Anxiety Disorders. 1999;13:349–358. doi: 10.1016/S0887-6185(99)00009-2. [DOI] [PubMed] [Google Scholar]
- Masip AF, Amador-Campos JA, Gómez-Benito J, del Barrio Gándara V. Psychometric properties of the Children’s Depression Inventory in community and clinical sample. The Spanish Journal of Psychology. 2010;13:990–999. doi: 10.1017/s1138741600002638. [DOI] [PubMed] [Google Scholar]
- Mattila M-L, Hurtig T, Haapsamo H, Jussila K, Kuusikko-Gauffin S, Kielinen M, Moilanen I, et al. Comorbid psychiatric disorders associated with Asperger syndrome/high-functioning autism: A community and clinic-based study. Journal of Autism and Developmental Disorders. 2010;40:1080–1093. doi: 10.1007/s10803-010-0958-2. [DOI] [PubMed] [Google Scholar]
- Mayes SD, Calhoun SL, Murray MJ, Ahuja M, Smith LA. Anxiety, depression, and irritability in children with autism relative to other neuropsychiatric disorders and typical development. Research in Autism Spectrum Disorders. 2011;5:474–485. doi: 10.1016/j.rasd.2010.06.012. [DOI] [Google Scholar]
- Merikangas KR, He JP, Burstein M, Swanson SA, Avenevoli S, Cui L, Benjet C, Swendsen J, et al. Lifetime prevalence of mental disorders in U.S. adolescents: Results from the National Comorbidity Survey Replication-Adolescent Supplement (NCS-A) Journal of the American Academy of Child and Adolescent Psychiatry. 2010;49:980–989. doi: 10.1016/j.jaac.2010.05.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mesibov GB, Schopler E, Schaffer B, Michal N. Use of the childhood autism rating scale with autistic adolescents and adults. Journal of the American Academy of Child and Adolescent Psychiatry. 1989;28:538–541. doi: 10.1097/00004583-198907000-00012. [DOI] [PubMed] [Google Scholar]
- Muris P, Steerneman P, Merckelbach H, Holdrinet I, Meesters C. Comorbid anxiety symptoms in children with pervasive developmental disorders. Journal of Anxiety Disorders. 1998;12:387–393. doi: 10.1016/S0887-6185(98)00022-X. [DOI] [PubMed] [Google Scholar]
- Orsmond GI, Krauss MW, Seltzer MM. Peer relationships and social and recreational activities among adolescents and adults with autism. Journal of Autism and Developmental Disorders. 2004;34:245–256. doi: 10.1023/B:JADD.0000029547.96610.df. [DOI] [PubMed] [Google Scholar]
- Pfeiffer B, Kinnealey M, Reed C, Herzberg G. Sensory modulation and affective disorders in children and adolescents with Asperger’s disorder. American Journal of Occupational Therapy. 2005;59:335–345. doi: 10.5014/ajot.59.3.335. [DOI] [PubMed] [Google Scholar]
- Pine DS, Guyer AE, Goldwin M, Towbin KA, Leibenluft E. Autism Spectrum Disorder Scale Scores in Pediatric Mood and Anxiety Disorders. Journal of the American Academy of Child and Adolescent Psychiatry. 2008;47:652–661. doi: 10.1097/CHI.0b013e31816bffa5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Puleo CM, Kendall PC. Anxiety disorders in typically developing youth: Autism spectrum symptoms as a predictor of cognitive-behavioral treatment. Journal of Autism and Developmental Disorders. 2011;41:275–286. doi: 10.1007/s10803-010-1047-2. [DOI] [PubMed] [Google Scholar]
- Puleo CM, Kendall PC. Anxiety in autism spectrum disorders: Core or comorbid psychopathology? Revised manuscript awaiting final decision 2012 [Google Scholar]
- Reiersen AM, Constantino JN, Todd RD. Co-occurrence of motor problems and autistic symptoms in attention-deficit/hyperactivity disorder. Journal of the American Academy of Child and Adolescent Psychiatry. 2008;47:662–672. doi: 10.1097/CHI.0b013e31816bff88. [DOI] [PubMed] [Google Scholar]
- Russell E, Sofronoff K. Anxiety and social worries in children with Asperger syndrome. Australian and New Zealand Journal of Psychiatry. 2005;39:633–638. doi: 10.1080/j.1440-1614.2005.01637.x. [DOI] [PubMed] [Google Scholar]
- Rutter M. Autistic children: Infancy to adulthood. Seminars in Psychiatry. 1970;2:435–450. [PubMed] [Google Scholar]
- Shaffer D, Gould MS, Brasic J, Ambrosini P, Fischer P, Bird H, Aluwahlia S, et al. A children’s global assessment scale (CGAS) Archives of General Psychiatry. 1983;40:1228–1231. doi: 10.1001/archpsyc.1983.01790100074010. [DOI] [PubMed] [Google Scholar]
- Silverman WK, Albano AM. The Anxiety Disorders Interview Schedule for DSM-IV: Child and Parent Versions. San Antonio, TX: Psychological Corporation; 1996. [Google Scholar]
- Silverman WK, Saavedra LM, Pina AA. Test-retest reliability of anxiety symptoms and diagnoses with Anxiety Disorders Interview Schedule for DSM-IV: Child and Parent versions. Journal of the American Academy of Child and Adolescent Psychiatry. 2001;40:937–944. doi: 10.1097/00004583-200108000-00016. [DOI] [PubMed] [Google Scholar]
- Simonoff E, Pickles A, Charman T, Chandler S, Loucas T, Baird G. Psychiatric disorders in children with autism spectrum disorders: Prevalence, comorbidity, and associated factors in a population-derived sample. Journal of the American Academy of Child and Adolescent Psychiatry. 2008;47:921–929. doi: 10.1097/CHI.0b013e318179964f. [DOI] [PubMed] [Google Scholar]
- Southam-Gerow M, Kendall PC, Weersing VR. Examining outcome variability: Correlates of treatment response in a child and adolescent anxiety clinic. Journal of Clinical Child Psychology. 2001;30:422–436. doi: 10.1207/S15374424JCCP3003_13. [DOI] [PubMed] [Google Scholar]
- Steinhausen HC, Metzke CW. Global measures of impairment in children and adolescents: Results from a Swiss community survey. Australian and New Zealand Journal of Psychiatry. 2001;35:282–286. doi: 10.1046/j.1440-1614.2001.00901.x. [DOI] [PubMed] [Google Scholar]
- Strobl C, Malley J, Tutz G. An introduction to recursive partitioning: Rationale, application, and characteristics of classification and regression trees, bagging, and random forests. Psychological Methods. 2009;14:323–348. doi: 10.1037/a0016973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sukhodolsky DG, Scahill L, Gadow KD, Arnold LE, Aman MG, McDougle CJ, Vitiello B, et al. Parent-rated anxiety symptoms in children with pervasive developmental disorders: Frequency and association with core autism symptoms and cognitive functioning. Journal of Abnormal Child Psychology. 2008;36:117–128. doi: 10.1007/s10802-007-9165-9. [DOI] [PubMed] [Google Scholar]
- Thede LL, Coolidge FL. Psychological and neurobehavioral comparisons of children with Asperger’s disorder versus high-functioning autism. Journal of Autism and Developmental Disorders. 2007;37:847–854. doi: 10.1007/s10803-006-0212-0. [DOI] [PubMed] [Google Scholar]
- Therneau TM, Atkinson B. The rpart package. University of California, Los Angeles Statistics Department Comprehensive R Archive Network; 2010. Retrieved September 10, 2010 http://cran.stat.ucla.edu. [Google Scholar]
- Towbin KE, Pradella A, Gorrindo T, Pine DS, Leibenluft E. Autism spectrum traits in children with mood and anxiety disorders. Journal of Child and Adolescent Psychopharmacology. 2005;15:452–464. doi: 10.1089/cap.2005.15.452. [DOI] [PubMed] [Google Scholar]
- Villabø MA, Gere MK, Torgersen S, March J, Kendall PC. Diagnostic efficiency of the child and parent versions of the Multidimensional Anxiety Scale for Children (MASC) Journal of Clinical Child and Adolescent Psychology. 2012;41:75–85. doi: 10.1080/15374416.2012.632350. [DOI] [PubMed] [Google Scholar]
- Walkup JT, Albano AM, Piacentini J, Birmaher B, Compton SN, Sherrill JT, Kendall PC, et al. Cognitive behavioral therapy, sertraline, or a combination in childhood anxiety. The New England Journal of Medicine. 2008;359:2753–2766. doi: 10.1056/NEJMoa0804633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weisbrot DM, Gadow KD, DeVincent CJ, Pomeroy J. The presentation of anxiety in children with pervasive developmental disorders. Journal of Child and Adolescent Psychopharmacology. 2005;15:477–496. doi: 10.1089/cap.2005.15.477. [DOI] [PubMed] [Google Scholar]
- Weiss DD, Last CG. Developmental variations in the prevalence and manifestation of anxiety disorders. In: Vasey MW, Dadds MR, editors. The developmental psychopathology of anxiety. 1. Oxford: Oxford University Press; 2001. pp. 27–42. [Google Scholar]
- White SW, Oswald D, Ollendick T, Scahill L. Anxiety in children and adolescents with autism spectrum disorders. Clinical Psychology Review. 2009;29:216–229. doi: 10.1016/j.cpr.2009.01.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wood JJ, Gadow KD. Exploring the nature and function of anxiety in youth with autism spectrum disorders. Clinical Psychology Science and Practice. 2010;17:281–292. doi: 10.1111/j.1468-2850.2010.01220.x. [DOI] [Google Scholar]
- Wood JJ, Piacentini JC, Bergman RL, McCracken J, Barrios V. Concurrent validity of the anxiety disorders section of the Anxiety Disorders Interview Schedule for DSM-IV: Child and parent versions. Journal of Clinical Child & Adolescent Psychology. 2002;31:335–342. doi: 10.1207/S15374424JCCP3103_05. [DOI] [PubMed] [Google Scholar]
- Zhang H, Singer B. Recursive partitioning in the health sciences. New York: Springer-Verlag; 1999. [Google Scholar]


