Abstract
The purpose of this study was to improve the membrane permeability and oral absorption of the poorly permeable anti-influenza agent, zanamivir. The poor oral bioavailability is attributed to the high polarity (cLogP~-5) resulting from the polar and zwitterionic nature of zanamivir. In order to improve the permeability of zanamivir, prodrugs with amino acids were developed to target the intestinal membrane transporter, hPepT1. Several acyloxy ester prodrugs of zanamivir conjugated with amino acids were synthesized and characterized. The prodrugs were evaluated for their chemical stability in buffers at various pHs and for their transport and tissue activation by enzymes. The acyloxy ester prodrugs of zanamivir were shown to competitively inhibit [3H]Gly-Sar uptake in Caco-2 cells (IC50: 1.19±0.19mM for L-valyl prodrug of zanamivir). The L-valyl prodrug of zanamivir exhibited ~3 fold higher uptake in transfected HeLa/hPepT1 cells compared to wild type HeLa cells, suggesting, at least in part, carrier mediated transport by the hPepT1 transporter. Further, enhanced transcellular permeability of prodrugs across Caco-2 monolayer compared to the parent drug (Papp= 2.24E-06 ± 1.33E-07 cm/sec for L-valyl prodrug of zanamivir), with only parent zanamivir appearing in the receiver compartment, indicates that the prodrugs exhibited both enhanced transport and activation in intestinal mucosal cells. Most significantly several of these prodrugs exhibited high intestinal jejunal membrane permeability, similar to metoprolol, in the in situ rat intestinal perfusion system, a system highly correlated with human jejunal permeability.
In summary, this mechanistic targeted prodrug strategy, to enhance oral absorption via intestinal membrane carriers such as hPepT1, followed by activation to parent drug (active pharmaceutical ingredient or API) in the mucosal cell, significantly improves the intestinal epithelial cell permeability of zanamivir and has the potential to provide the high oral bioavailability necessary for oral zanamivir therapy.
Keywords: Prodrugs, carrier-mediated transport, hPepT1, zanamivir
Introduction
Influenza is an acute viral infection of the human respiratory tract. Four drugs are recommended for the treatment and prophylaxis of the influenza infection: the ion channel inhibitors (amantadine and rimantadine) and the neuraminidase (NA) inhibitors (zanamivir and oseltamivir). Amantadine and rimantadine act by interfering with the viral coating process and are effective against only influenza A. Additionally; there has been a rapid increase in the resistance of influenza A virus against these ion channel inhibitors, notably, including the bird flu virus H5N1 responsible for the influenza outbreak in Asia.1 The neuraminidase inhibitors act via a different mechanism, by inhibiting the neuraminidase enzyme essential for viral propagation. Among the recommended drugs to treat influenza infection, neuraminidase inhibitors are considered to be the drugs of choice principally due to their low toxicity and low incidences of resistance.2
Zanamivir and oseltamivir are the two NA inhibitors approved by the FDA for clinical use. Zanamivir has been shown to be a potent inhibitor of both influenza A and influenza B as well as active against emerging resistant strains.3 There are reported incidences of resistance against oseltamivir,4 however, there are no reports of resistance to zanamivir to date. This lack of resistance development for zamamivir is thought to be due to the fact that zanamivir is structurally very similar to sialic acid, the natural substrate of NA. Thus, any drug-resistant mutations in NA would likely compromise the binding of sialic acid to NA and is likely compromise the viral propagation.5
The absolute oral availability of zanamivir is very low, approximately 2%6 and zanamivir is administrated clinically by inhalation. The major drawback with this route of administration is lack of patient compliance, and therapy is not recommended in patients with chronic respiratory conditions such as asthma. It is also difficult to administer this drug by inhalation to the pediatric population which is at high risk for influenza infection. Thus, the poor oral bioavailability limits the clinical utility of zanamivir to treat influenza infections.
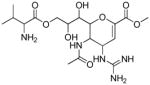
The principle reason for the poor oral availability of zanamivir is its polar nature, contributed particularly by the guanidine, carboxylic, and hydroxyl functional groups in the molecule (Figure 1). A common approach to overcome this type of oral delivery problem is to chemically modify zanamivir to make a more lipophilic molecule, and thus potentially increasing its mucosal membrane permeability and oral bioavailability. An analogue approach to modification of zanamivir’s polarity, generating a new chemical entity (NCE) has the obvious limitation of requiring full safety and efficacy testing and development of a NCE. Since zanamivir itself has a well established toxicity profile, excellent anti-viral properties, and has shown little or no resistance development, we developed a prodrug approach targeting the intestinal epithelial cell hPepT1 transporter to orally deliver zanamivir.7 The prodrug approach has the advantage of preserving the safety and efficacy of the parent zanamivir. However, both prodrug transport8 and activation to parent9 have to occur for a prodrug strategy to be successful. Amino acid prodrugs of zanamivir were chosen based on our prior studies with carrier mediated transport of prodrug. 7b, 10
Figure 1.
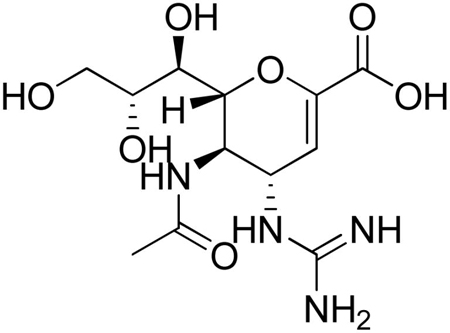
Zanamivir
Here we report the synthesis and transport of prodrugs of zanamivir linked to amino acids. The acyloxy group is often used as linker in prodrug strategies in order to improve the biopharmaceutical and/or pharmacokinetic properties of the drug. Examples of successful acyloxy prodrugs include pivampicillin and cefuroxime axetil. Another example is tranexamic acid, a clinically used anti-fibrinolytic agent that is not well absorbed orally due to the amphoteric nature of the drug. Acyloxy esters of tranexamic acid have shown increased absorption compared to the parent drug.11 In this manuscript we report the synthesis and permeability evaluations of acyloxyester prodrugs of zanamivir. We have evaluated the cellular transport and activation of the prodrugs, their ability to compete with [3H]Gly-Sar uptake in Caco-2 cells and in direct uptake in HeLa/hPEPT1 cells. We also report the chemical and enzymatic (cell homogenates) stability of the prodrugs. Furthermore, several of the prodrugs that exhibited good [3H]Gly-Sar uptake inhibition and uptake in HeLa/hPepT1 cells were studied for transmembrane permeability in Caco-2 monolayers and the in situ rat perfusion system that is highly correlated with human jejunal permeability12.
Materials and Methods
Boc-zanamivir was synthesized from N-Acetylneuraminic acid (sialic acid) purchased from TCI America Ltd. Zanamivir was purchased from Waterstone Technology (Carmel, IN). The tert-butyloxycarbonyl (Boc) protected amino acids, Boc-L-Val-OH, Boc-L-Ile-OH, and Boc-D-Val-OH were obtained from Calbiochem-Novabiochem (San Diego, CA). HPLC (High-Performance Liquid Chromatography) grade acetonitrile and LC-MS (Liquid Chromatography–Mass Spectrometry) grade methanol was obtained from Fisher Scientific. All other reagents were purchased from Sigma Aldrich (Milwaukee, WI) unless otherwise mentioned. All solvents used for chemical syntheses were anhydrous and was obtained in sure seal bottles unless otherwise mentioned. Deuterated solvents for Nuclear Magnetic Resonance (NMR) spectroscopy were purchased from Cambridge Isotopes, Inc. (Andover, MA). Valacyclovir was a gift from GlaxoSmithKline, Inc. (Research Triangle Park, NC). Cell culture reagents were purchased from Invitrogen (Carlsbad, CA) and the cell culture supplies were obtained from Corning (Corning, NY) and Falcon (Lincoln Park, NJ). All the NMRs were taken using Varian 500MHz NMR spectrometer. The HPLC analyses were done using Agilent 1200 Series HPLC system (Agilent Technologies, Inc. Santa Clara CA). The LC-MS studies were carried out using Shimadzu LC-MS System. The molecular weights of the compounds were confirmed by positive-mode electrospray ionization mass spectra (ESI-MS) on Waters electronspray ionization spectrometer.
Boc-zanamivir and Prodrugs Synthesis
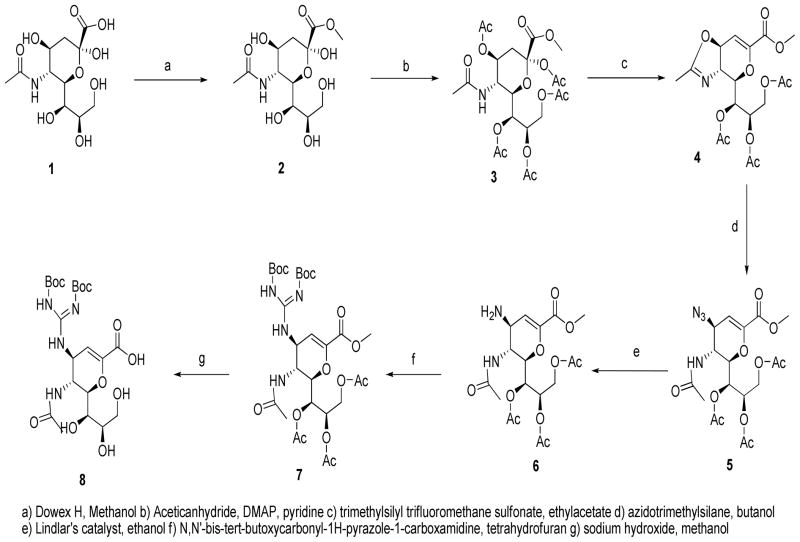
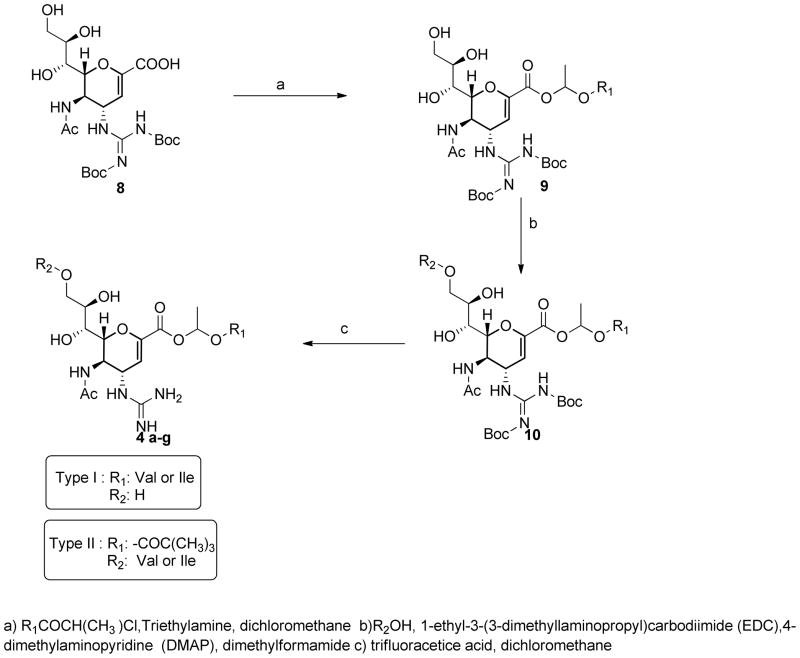
Boc-zanamivir was synthesized from sialic acid according to the procedures mentioned in the literature. Briefly, sialic acid 1, was converted to the methyl ester 2, in presence of Dowex H+.13 The hydroxyl groups of 2 were protected with acetyl groups to give compound 3, which was then converted to the oxazoline derivative 4 in the presence of trimethyltrifluoromethanesulfonate.14 Azide 5 was synthesized from 4 in presence of azidotrimethylsilane.14 The azide is reduced to the corresponding amine 6 by using Lindlar’s catalyst; the amine (6) is then converted to the guanidine derivative 7. 15 The final step involved the deprotection of the methyl ester and acetyl groups in the presence of methanolic sodium hydroxide to give Boc-protected zanamivir 8. 15. The synthetic procedure is shown in Scheme 1. Acyloxy ester prodrugs of zanamivir, 4a–g, were synthesized from intermediate 8 and α-chloro methylester of respective R group.16 The alkyl α-chloro methylester was synthesized from respective carbonyl chloride in the presence of zinc chloride and acetaldehyde.16 For the compounds with amino acid substitution instead of an alkyl group, the α-chloro methylester was synthesized from the cesium salt of respective Boc-protected amino acid in presence of 1-chloro-1-bromoethane.17 The α-chloro methylester of amino acid was reacted with Boc-protected zanamivir in presence of triethylamine in dimethylformamide (DMF) at 50°C for 4 days. The reaction mixture was concentrated in vacuo and the crude mixture was purified using flash column chromatography with silica gel (60 A°, 230–400 mesh) by eluting with chloroform: methanol (20:1) to yield the pure compound as oil. The Boc-protected prodrugs were deprotected by reacting with 50% trifluroacetic acid (TFA) in dichloromethane and stirring for 2 hours at room temperature, the reaction mixture was concentrated in vacuo and the residues were constituted in water and were lyophilized. The TFA salts of aminoacid prodrugs of zanamivir were obtained as white hygroscopic amorphous powder. The synthetic steps for prodrugs, 4a–d are summarized in Scheme 2.
Scheme 1.
Synthesis of Boc-zanamivir
Scheme 2.
Synthesis of acyloxy ester prodrugs of zanamivir.
Boc-Zanamivir (8)
1H NMR (CD3OD) δ (ppm) 5.6 (d, J = 2.0 Hz, 1H), 5.01 (dd, J = 9.6, 2.1 Hz, 1H), 4.25 (dd, J = 10.8, 1.1 Hz, 1H), 4.18 (dd, J = 10.6, 9.6 Hz, 1H), 3.89 (ddd, J = 9.4, 6.2, 2.7 Hz, 1H), 3.84 (dd, J = 11.3, 2.8 Hz, 1H), 3.67 (dd, J = 11.3, 5.8 Hz, 1H), 3.57(d, J = 9.3 Hz, 1H), 1.9 (s, 3H), 1.55 (s, 9H), 1.50 (s, 9H); ESI-MS: 533 (M+H)+.
Zan-L-Val (4a)
1H NMR (CD3OD) δ (ppm) 6.9 (q, 1H), 5.8(d, J = 2.0 Hz, 1H), 5.2(m, 1H), 4.9 (m, 1H), 4.2(m, 2H), 4.02(m, 2H), 3.9(m, 1H), 3.7(m, 1H), 2.14(m, 1H), 2.08(s, 3H), 2.01(s, 3H), 0.98(d, J = 6.8 Hz, 3H), 0.90(d, J = 6.5 Hz, 3H); ESI-MS: 476 (M+H)+.
Zan-L-Ile (4b)
1H NMR (CD3OD) δ (ppm) 7.0(m, 1H), 5.9 (d, J = 2.0 Hz, 1H), 5.5(m, 1H) 4.9(m, 1H) 4.22 (m, 1H) 4.07(m, 1H), 3.85 (m, 2H), 3.70(m, 2H) 3.2(q, 1H), 2.03(s, 6H), 1.3(m, 2H), 1.02–1.03(m, 6H) ; ESI-MS: 490.21 (M+H)+.
Zan-D-Val (4c)
1H NMR (CD3OD) δ (ppm) 6.88 (q, 1H), 5.85(d, J = 2.0 Hz, 1H), 5.2(m, 1H), 4.9 (m, 1H), 4.3(m, 2H), 4.1(m, 2H), 3.9(m, 1H), 3.7(m, 1H), 2.22 (m, 1H), 2.1(s, 3H), 2.0(s, 3H), 0.96(d, J = 6.0 Hz, 3H), 0.92(d, J = 6.0 Hz, 3H); ESI-MS: 476 (M+H)+.
Cell Culture
Caco-2 cells (passage 22–34) and HeLa cells (passage 20–33) from American Type Culture Collection (Rockville, MD) were cultured in Dulbecco’s modified Eagle’s medium (DMEM) containing 10% FBS, 1% nonessential amino acids, 1mM sodium pyruvate and 1% L-glutamate. Cells were grown in an atmosphere of 5% CO2 and 90% relative humidity at 37°C.
[3H] Gly-Sar uptake inhibition
Caco-2 cells were grown to be confluent in 12 well plates. The cells were grown for 10 days after seeding. On the day of experiment, cells were washed with uptake buffer (pH 6.0, 145 mM NaCl, 3 mM KCl, 1 mM NaH2PO4, 1 mM CaCl2, 0.5 mM MgCl2, 5 mM D-glucose, and 5 mM MES) and incubated with 10 μmol/L [3H]Gly-Sar (9.94 μmol/L Gly-Sar and 0.06 μmol/L [3H]Gly-Sar) and different concentrations (0.05–5mM) of zanamivir or its prodrugs in 0.3mL of the uptake buffer for 30 minutes at 37°C. After 30 min, the drug solution was aspirated and the cells were washed with ice cold uptake buffer. Methanol: water (50:50) (500 μL) was added to each well and the cells were scrapped and dissolved in the scintillation cocktail (ScintiVerse* LC Cocktail, Fisher Chemicals). The radioactivity was measured by scintillation counter (Beckman LS-9000, Beckman Instruments, Fullerton, CA). IC50 values were determined using nonlinear data fitting (Graph Pad Prism v4.0).
Uptake Studies
Carrier mediated prodrug transport was evaluated in HeLa/hPepT1 as described earlier.7b HeLa cells were transfected by adenovirus containing hPepT1 as described previously.18 Two days post infection the cell culture medium was removed and washed with uptake buffer (pH 6.0) and was incubated with 0.5ml of test compounds (1mM) in uptake buffer at 37°C for 45 min. After 45 min the drug solutions were removed and the cells were washed with ice-cold uptake buffer. Methanol: water (50:50) (500 μL) was added to each well and the incubated at room temperature for 1 hour. The cells were collected after one hour and were vortexed and centrifuged. The supernatant was filtered (0.22 μm) and analyzed by LC-MS. Control experiments were performed in non-transfected HeLa cells. The protein amount of each sample was determined with the Bio-Rad DC Protein Assay using bovine serum albumin as the standard.
Hydrolysis in Caco-2 homogenates
Caco-2 cells 22 days after seeding were washed with phosphate buffer saline (pH 7.4). The cells were scrapped from the plate using a cell scraper (Corning® Small Cell Scraper). The cells were collected in phosphate buffer (pH 7.4, 100mM) and spun down by centrifugation. The cells were re-suspended in phosphate buffer and were lysed by sonication. The cell lysate was centrifuged at 7150 g for 15 min and the supernatant was collected. The protein amount of supernatant was determined with the Bio-Rad DC Protein Assay using bovine serum albumin as the standard. The hydrolysis reactions were carried out in eppendorf tubes with total reaction volume of 1mL containing 1mM drug solution and cell lysate corresponding to 500μg/mL protein concentration in 100mM pH7.4 phosphate buffer. The assay mixture was incubated at 37°C and 100 μL of the reaction mixture was removed at various time points (0, 5, 10, 15, 20 and 30min) and was quenched with 100μL of ice-cold TFA (10%w/v). The samples were filtered (0.45μM) and the filtrate was assayed for prodrug and parent drug by HPLC. The extent of hydrolysis for the prodrug at each time point was calculated. The measurements were done in triplicates.
Chemical Stability
The hydrolysis profiles of the prodrugs were determined in 100mM hydrochlorate buffer (pH 1.2), 100mM acetate buffer (pH 4), and 100mM phosphate buffer (pH 6.5, and 7.4) corresponding to physiologically relevant pHs. The choice of buffer types and strength was based on information from the data published earlier.19 Hydrolysis of the prodrugs were studied in respective buffers at 37°C for a period of 4 hours. At every time point, 50 μL aliquots of the samples were taken and diluted with 0.1% ice cold trifluoroacetic acid and was analyzed by HPLC.
Caco-2 Monolayer Permeability
The Caco-2 permeability for the prodrugs and parent drug was determined as previously described.7b Briefly, Caco-2 cells were seeded on 6-well format collagen-coated transwell inserts (Corning, NY, 0.4μm pore size: area 4.7 cm2) at a density of 100,000 cells/mL and cultured in DMEM containing 10% FBS, 1% nonessential amino acids, 1mM sodium pyruvate and 1% L-glutamine (Invitrogen, Carlsbad CA). Cells were grown in 5% CO2 and 90% relative humidity at 37°C. The culture medium was replaced as needed. Transendothelial electrical resistance (TEER) measurements were performed on all monolayers. Monolayers with TEER values > 250 Ω/cm2 were used for the study. 1.5 mL of MES buffer pH 6.0 (5 mM D-glucose, 5 mM MES, 1 mM CaCl2, 1 mM MgCl2, 150 mM NaCl, 3 mM KCl and 1 mM NaH2PO4) was applied to the apical side and 2.6 mL HEPES buffer pH 7.4 (1mM CaCl2, 1mM MgCl2, 150mM NaCl, 3mM KCl and 1mM NaH2PO4) was applied to the basolateral side. The plates were incubated at 37°C for 15 minutes for equilibration. After 15 minute the apical layer medium was aspirated and replaced with 1.5mL of drug (0.25mM) solution in MES buffer (pH 6.0) and the basolateral medium was replaced with fresh 2.6 mL HEPES buffer. At every 15 minutes interval 200 μL aliquot of the basolateral receiving chamber and was replaced with equal amount of fresh HEPES buffer. The degradation of prodrugs due to monolayer or buffer in the apical layer was determined by taking 10 μL aliquots of the apical solution and quenching with 90 μL of 0.1% (w/v) TFA in acetonitrile. The epithelial integrity of the representative monolayers was checked by monitoring TEER values at the end of the experiment. Both aliquots from apical and basolateral sides were analyzed by LC-MS.
Rat Perfusion
All animal experiments were conducted using protocols approved by the University Committee of Use and Care of Animals (UCUCA), University of Michigan, and the animals were housed and handled according to the University of Michigan Unit for Laboratory Animal Medicine guidelines. Male albino Wistar rats (Charles River, IN) weighing 250–280 g were used for all perfusion studies. Prior to each experiment, the rats were fasted over night (12–18 hr) with free access to water. Animals were randomly assigned to the different experimental groups.
The procedure for the in situ single-pass intestinal perfusion followed previously published reports.12, 20 Briefly, rats were anesthetized with an intra-muscular injection of 1 ml/kg of ketamine-xylazine solution (9%:1%, respectively) and placed on a heated surface maintained at 37°C (Harvard Apparatus Inc., Holliston, MA). The abdomen was opened by a midline incision of 3–4 cm. A proximal jejunal segment, mid-small intestine, or a distal ileal segment, of approximately 10 cm was carefully exposed and cannulated on two ends with flexible PVC tubing (2.29 mm i.d., inlet tube 40 cm, outlet tube 20 cm, Fisher Scientific Inc., Pittsburgh, PA). Care was taken to avoid disturbance of the circulatory system, and the exposed segment was kept moist with 37°C normal saline solution. The perfusate was incubated in a 37°C water bath to maintain temperature, and a perfusion solution containing 10 mM MES buffer, pH 5.5, 135 mM NaCl, 5 mM KCl, and 0.1 mg/ml phenol red with an osmolarity of 290 mosm/l was pumped through the intestinal segment (Watson Marlow Pumps 323S, Watson-Marlow Bredel Inc, Wilmington, MA). The isolated segment was rinsed with blank perfusion buffer, pH 5.5 at a flow rate of 0.5 ml/min in order to clean out any residual debris.
At the start of the study, perfusion solution containing the tested drug was perfused through the intestinal segment at a flow rate of 0.18 ml/min. Phenol red was added to the perfusion buffer as a nonabsorbable marker for measuring water flux. Metoprolol was co-perfused with the other test compounds as well, as a compound with known permeability that serves as a marker for the integrity of the experiment, and as a reference standard for permeability in close proximity to the low/high permeability class boundary. The concentrations of the test compounds used in the perfusion studies were determined by dividing the highest prescribed oral dose by 250 ml, the accepted gastric volume, in order to represent the maximal drug concentration present in the intestinal segment, and were within their intrinsic solubility reported at pH 5.5. The perfusion buffer was first perfused for 1 hr, in order to assure steady state conditions (as also assessed by the inlet over outlet concentration ratio of phenol red which approaches 1 at steady state). Following reaching to steady state, samples were taken in 10 min intervals for 1 hour (10, 20, 30, 40, 50, and 60 min). All samples including perfusion samples at different time points, original drug solution, and inlet solution taken at the exit of the syringe were immediately assayed by HPLC. Following the termination of the experiment, the length of the perfused intestinal segment was accurately measured.
HPLC Analysis
The samples from enzymatic and chemical stability studies of zanamivir and its prodrugs were analyzed by Agilent 1200 Series HPLC system (Agilent Technologies, Inc. Santa Clara CA) equipped with two Agilent 1200 pumps, an Agilent autosampler and a Agilent UV detector. The system was operated by Agilent 1100 software. Waters Xterra® C18 reversed-phase column (5 μm, 4.6 × 250 mm) was used for sample analysis. The analytes were eluted using a gradient method. The mobile phases (water and acetonitrile) contained 0.1% TFA as modifier.
LC-MS Analysis
The prodrug and parent drug samples from uptake and transepithelial permeability studies were analyzed using a LC-MS 2010A system (Shimadzu Scientific Instruments, Columbia MD). The LC-MS unit consisted of two pumps (LC-20AD), autosampler (SIL 20A HT) and QoQ Optical System. Positive-mode Electrospray Ionization (ESI) was used to ionize the molecules. The system was operated by LCMSsolution Ver. 3 software. The CDL temperature used was 250°C and the detector voltage was maintained at 1.5kV. Samples were analyzed by Restek Allure Aqueous C18 column (5 μm, 2.1 × 50 mm) equipped with a guard column. The compounds were eluted using a gradient system. Mobile phases (water and methanol) contained 0.1% formic acid as modifier and the flow rate was 0.2mL/min.
Data Analysis
Hydrolysis Studies
Apparent first order kinetics and rate constants were determined by using initial rates of hydrolysis. The apparent first-order degradation rate constants of zanamivir prodrugs at 37°C were determined by plotting the logarithm of prodrug remaining as a function of time. The relation between the rate constant, k, and slopes of the plots are explained by the equation:
| (1) |
The degradation half-lives were then calculated by the equation:
| (2) |
Caco-2 Monolayer Permeability
The apparent permeability (Papp) was calculated using the following equation:
where Vr is the receiver volume, A is the surface area of the exposed monolayer, C0 is the concentration of the prodrug in the donor solution and dCr/dt is the rate of change of concentration in the receiver solution. The concentration of zanamivir and its prodrugs is analyzed by LC-MS.
The stability of the prodrugs in apical layer was analyzed by taking samples in the beginning, during and at the end of the experiments and the concentration was determined by LC-MS.
Rat in situ Perfusion
The net water flux in the single-pass intestinal perfusion studies, resulting from both water absorption and efflux in the intestinal perfused segment, was determined by measurement of phenol red, a nonabsorbed, nonmetabolized marker. Phenol red (0.1 mg/ml) was included in the perfusion buffer and co-perfused with the tested compound. The measured Cout/Cin ratio was corrected for water transport (to obtain the corrected ratio C′out/C′in) according to the following equation:
where Cin phenol red is equal to the concentration of phenol red in the inlet sample, and Cout phenol red is equal to the concentration of phenol red in the outlet sample.
The effective permeability (Peff) through the rat gut wall in the single-pass intestinal perfusion studies was determined assuming the “plug flow” model expressed in the following equation. 21
where Q is the perfusion buffer flow rate (0.18 ml/min), C′out/C′in is the ratio of the outlet concentration and the inlet or starting concentration of the tested compound that has been adjusted for water transport, R is the radius of the intestinal segment (set to 0.2 cm), and L is the length of the intestinal segment.
Results
Synthesis of Zanamivir Prodrugs
Boc-protected zanamivir was synthesized from sialic acid following well established synthetic procedures from the literature (Scheme 1) and then was used as the starting material for prodrug syntheses. For acyloxyester prodrugs the ethyl bridge was chosen over methyl bridge as our studies with the model compounds have shown that the ethyl bridge imparts more chemical stability to the prodrugs as compared to the methyl bridge (results not shown). The amino acid starting material was synthesized from corresponding aliphatic amino acid and 1-chloro-1-bromo-ethane to give amino acid α-chloromethyl ester. The amino acid α-chloromethyl ester was reacted with Boc-protected zanamivir. Boc-protected prodrug of zanamivir was purified using flash column chromatography and the Boc-group was deprotected using TFA. The final product was lyophilized to yield the desired compounds as amorphous powder. The overall yield of the prodrug was 20–25%. The purity of the compounds was determined by HPLC and all the prodrugs showed >90% purity. Although TLC showed presence of a single spot, the HPLC chromatogram showed two peaks for the prodrugs due to presence of two isomers resulting from the formation of a chiral center at the acyloxy ethyl linker. The racemic mixture of the prodrug was used for the studies. The starting material and intermediates were sterically pure as evidenced by observation of single peak in HPLC and LC-MS systems. Zanamivir also showed a single peak in HPLC. The structural identities of the prodrugs were confirmed by positive- mode ESI mass spectrometry (ESI-MS) and 1H NMR. ESI-MS spectra showed single molecular ion peak for all the prodrugs and 1H NMR spectra was in complete agreement with the structure of the compounds.
[3H] Gly-Sar Uptake Inhibition Studies
An inhibition constant of the acyloxyester prodrugs of zanamivir for hPepT1 was determined by studying their ability to inhibit the uptake of [3H]Gly-Sar in Caco-2 cell lines. All prodrugs showed competition with [3H]Gly-Sar while zanamivir, exhibited no competition in the tested concentration range (0.05mM–5mM). All the experiments were compared with the positive control, valacyclovir, a known, well absorbed hPepT1 substrate. The valyl acyloxyester prodrug of zanamivir (Zan-L-Val) showed an IC50 comparable to that of valacyclovir. The isoleucyl prodrug of zanamivir (Zan-L-Ile) showed slightly higher IC50 value compared to valacyclovir but still significantly better than that of zanamivir which did not demonstrate any inhibition. The remaining prodrugs noted in Table 1 showed inhibitory constant in the range of 1–3 mM. The substitution with promoiety groups at different positions of zanamivir to did not markedly improve the [3H]Gly-Sar uptake inhibition of the prodrugs. We chose Zan-L-Val, Zan-D-Val and Zan-L-Ile for further studies. Zan-L-Val had the lowest IC50 of all the prodrugs tested while Zan-L-Ile exhibited a roughly 3 fold higher IC50 than Zan-L-Val, so it was deemed to be interesting how they would fare in permeability and uptake studies. Zan-D-Val was also chosen for further studies to see the effect of stereochemistry of the promoiety on uptake and permeability of the prodrugs. Compounds 4d–g mentioned in Table 1 were not chosen for further evaluations as they were double prodrugs and presence of additional promoiety did not enhance their affinity for hPepT1 transporter. However, compounds 4d–g are important as they offered important structure activity relationship insights on zanamivir prodrugs. The significant affinity for the hPepT1 transporter by the prodrugs is in marked contrast to the parent drug itself which lacked any apparent affinity for the transporter.
Table 1.
[3H]Gly-Sar uptake inhibition in Caco-2 cells.
| Compound Name | Structure | Mol Wt | (IC50) (mM) Mean±SDa |
|---|---|---|---|
| Zanamivir |
|
332 | No Inhibitionb |
| Zan-L-Val (4a) |
|
475.5 | 1.19±0.33 |
| Zan-L-Ile (4b) |
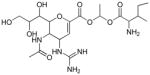
|
489.5 | 3.04±1.39 |
| Zan-D-Val (4c) |
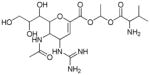
|
475.5 | 1.95±0.57 |
| Val-Zan-Pival (4d) |
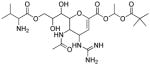
|
559.6 | 3.75±1.65 12 |
| BiVal-Zan-Pival (4e) |
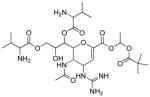
|
658.74 | 1.96±0.12 |
| Val-Zan-OMe (4f) |
|
445.4 | 1.9±0.08 |
| BiVal-Zan-OMe (4g) |
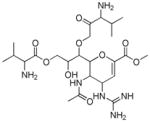
|
558.6 | 3.5±0.94 |
Mean and SD from 3 experiments.
No inhibition over concentration range of 0.05–5mM.
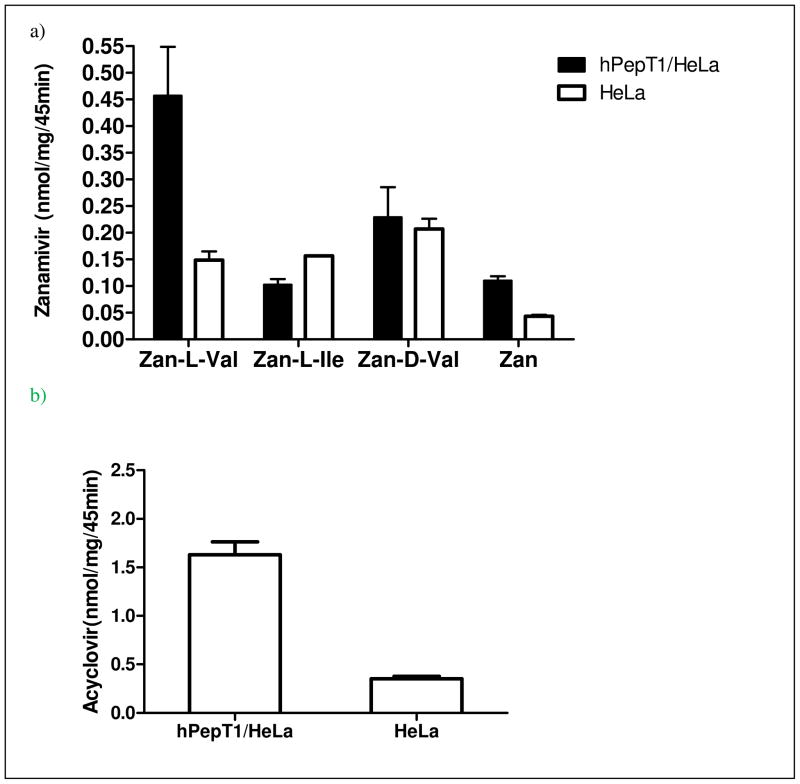
Uptake in HeLa/hPepT1 Cells
Increased hPepT1 mediated uptake in HeLa/hPepT1 cells was observed in case of Zan-L-Val (3 fold) compared to that of nontransfected HeLa cells (Figure 2a). The uptake of Zan-D-Val and Zan-L-Ile in HeLa/hPepT1 was not significantly enhanced as compared to the non-transfected cells. However, in most cases the uptake of the prodrugs in the cells was higher than the uptake of parent drug under similar experimental conditions. Valacyclovir used as the positive control, showed enhanced uptake in HeLa/hPEPT1 cells (~5 fold) compared to that in non-transfected HeLa cells (Figure 2b).
Figure 2.
a. Comparison of zanamivir prodrugs uptake in hPepT1 transfected and non-transfected HeLa cells. The uptake is measured as the concentration of zanamivir/mg of protein over 45 minute period in the cell lysates. The results are expressed as mean ± SD (n=3), b. Comparison of valacylcovir uptake in hPepT1 transfected and non-transfected HeLa cells. The uptake is measured as the concentration of acyclovir /mg of protein over 45 minute period in the cell lysates. The results are expressed as mean ± SD (n=3).
Stability Studies. Buffer Hydrolysis
The estimated half lives (t1/2) obtained from the linear regression of prodrug concentration vs time for zanamivir prodrugs in various buffers at pH 1.2, 4, 6.5 and 7.4 at 37°C are shown in Table 2. As expected the pH had a significant effect on hydrolysis of the prodrugs. The prodrugs were significantly more stable at acidic pHs. The isoleucyl prodrug was modestly more stable compared to the valyl prodrug of zanamivir.
Table 2.
Estimated hydrolysis half-lives (t1/2) of zanamivir prodrugs determined in 100mM hydrochlorate buffer (pH 1.2), 100mM acetate buffer (pH 4), and 100mM phosphate buffer (pH 6.5, and 7.4) as well as in Caco-2 homogenate corresponding to 500μg/mL protein concentration in 100 mM of pH 7.4 phosphate buffer. All the values are expressed as mean ± SD, n=3.
| Prodrug | t1/2 (min) | ||||
|---|---|---|---|---|---|
| pH 1.2 | pH 4 | pH 6 | pH 7.4 | Caco-2 homogenate | |
| Zan-L-Val | >240 | >240 | 150±17.7 | 35 ± 4.2 | 15 ±3.3 |
| Zan-L-Ile | >240 | >240 | 165 ±17.0 | 48 ± 11.3 | 25 ± 4.2 |
| Zan-D-Val | >240 | >240 | 155± 15.4 | 36 ± 8.1 | 35 ± 7.3 |
Prodrug Hydrolysis in Caco-2 cell Homogenate
The hydrolysis of prodrugs in Caco-2 homogenate was determined at 37°C. The half lives (t1/2) were estimated from linear regression of prodrug concentrations vs time (Table 2). Zan-L-Val and Zan-L-Ile prodrugs were hydrolyzed at a faster rate when incubated with Caco-2 homogenate compared to buffer alone. There was no significant difference in hydrolysis for Zan-D-Val in Caco-2 homogenate and buffer. All prodrugs had half lives of less than 40 minutes in homogenates. Isoleucyl prodrug appeared somewhat more stable than the L-valyl prodrug.
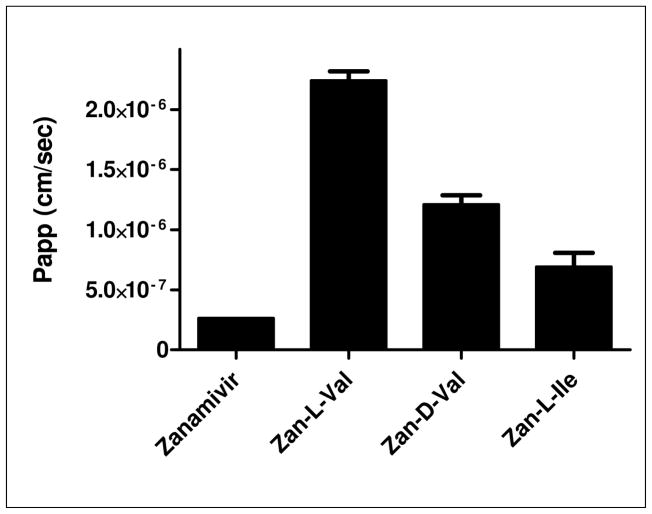
Caco-2 Permeability
The comparison of apparent transcellular permeabilities of zanamivir and the prodrugs in the apical to basolateral (AP to BL) direction (absorption direction) are shown in Figure 3. The permeability of L-valyl prodrug of zanamivir was approximately 9 fold higher than zanamivir whereas the isoleucyl prodrug showed more than a 2 fold increase in the apparent permeability. The hydrolysis of the prodrugs on the apical compartment side of the diffusion cell was less than 15% during the course of the experiment. Irrespective of the promoiety all the prodrugs were completely hydrolyzed following transport across the cell monolayers with only zanamivir detected on the basolateral membrane side of the diffusion cell.
Figure 3.
Apparent apical-to-basolateral permeability coefficient (Papp) across Caco-2 monolayers. All values are expressed as mean ± SD, n=3 at 37°C. Apical side concentration of prodrugs and zanamivir was 250 μM; only zanamivir was determined on basolateral side in case of prodrugs.
Rat in situ Perfusion
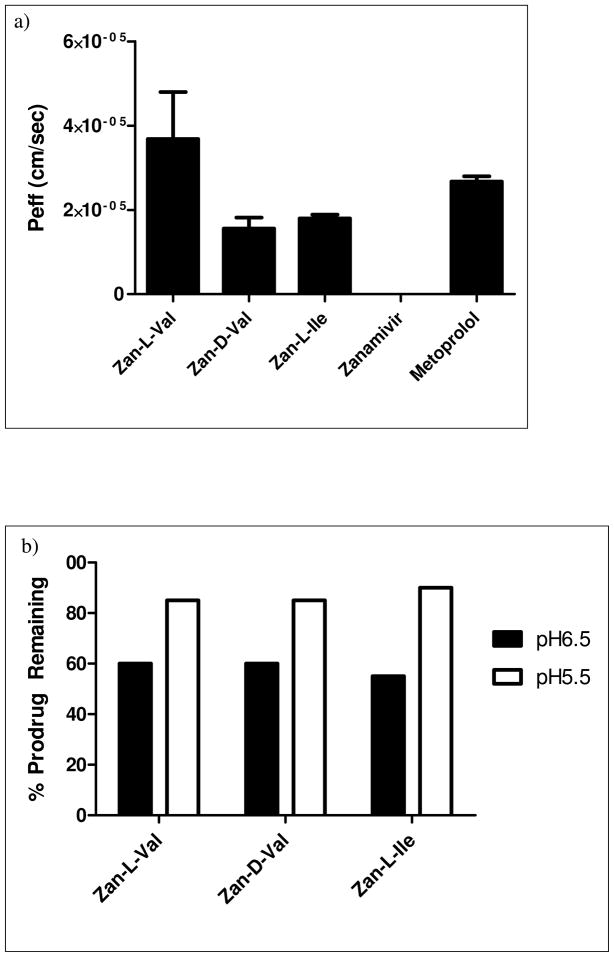
The effective permeabilities of zanamivir and its prodrugs were determined by the in situ single-pass intestinal perfusion system in rats. This experimental method is known to correlate very well with human intestinal permeability12. The effective permeability is measured as the disappearance of prodrug and parent drugs from the intestinal perfusate. The experiment was performed at pH 5.5 to minimize chemical hydrolysis of the prodrug (Figure 4b). Hydrolysis of the prodrugs by the intestinal epithelium was also taken into consideration when calculating the disappearance of the prodrugs from the intestinal perfusate in order to avoid overestimation of permeability of the prodrugs. Zanamivir showed absolutely no permeability in this in situ system whereas the valyl ester of zanamivir exhibited a significant permeability comparable to that of well absorbed, metoprolol. The isoleucyl prodrug also exhibited an increase in permeability compared to zanamivir. The comparison of effective permeabilities of zanamivir and its prodrugs are shown in Figure 4a.
Figure 4.
a: Comparison of effective permeabilities of drug and prodrugs in in situ rat perfusion studies. The results are expressed as mean ± SD (n=4), b: Percentage hydrolysis of prodrugs in perfusate at pH 6.5 and 5.5 respectively for 2 h at 37°C.
Discussion
Zanamivir has low absolute oral bioavailability which limits its clinical use despite being very effective against both Influenza A & B, with low toxicity and low incidences of resistance. However, the cumbersome mode and route of delivery of zanamivir by Diskhaler® limits compliance especially in patients with underlying pulmonary conditions and in children.
The prodrug approach has been used to address various drug delivery problems, ranging from poor bioavailability, low solubility and metabolic instability.22 The rationale for prodrug design to increase oral absorption is usually based on passive transport of a more lipophilic compound. This approach may in turn lead to solubility, dissolution and oral absorption limitations.23 Transporters in the intestinal epithelial cell membrane function to absorb polar nutrients. The endogenous transporters efficiently transport nutrients containing considerable polarity and aqueous solubility. Oligopeptide transporters, e.g hPepT1, are present in gastrointestinal tract and their apparently relatively broad substrate specificity makes them attractive targets for oral drug delivery.10b, 24 The improved oral bioavailability of valacyclovir in humans has been shown to be the result of enhanced intestinal transport by the hPepT1 peptide transport systems.7b, 8, 25 In this report, the linked amino acid prodrugs of zanamivir exhibited affinity for the hPepT1 transporter in [3H]Gly-Sar uptake inhibition experiments, indicating binding but not (yet) transport, while zanamivir itself, did not exhibit any affinity or inhibition at all the tested concentrations. The inhibitory constant for [3H]Gly-Sar uptake inhibition for the ethoxy linked L-valyl ester of zanamivir was comparable to valacyclovir, while the isoleucyl prodrug exhibited a somewhat higher IC50 (~3mM). This observation is consistent with previous results on prodrugs targeted to this transporter.26
Direct uptake studies in hPepT1 transfected HeLa cells compared to the non transfected HeLa cells indicated that the L-valyl prodrug of zanamivir exhibited an approximately 3 fold increase in permeability (membrane transport) in transfected cells compared to the non transfected cells; while the uptake of isoleucyl prodrug was not (statistically) significant different between transfected and non-transfected HeLa cells. However, in most cases the uptake was higher for prodrugs in both cell types when compared to the uptake of parent drug.
The chemical stability analysis showed that the prodrugs are more stable at acidic pHs and as expected, the stability decreases with increase in pH. While the prodrugs have half life of less than 1 hour at pH 7.4, the half-life at pH=6 is nearly 3 hours, sufficient half-life to allow good oral absorption in the upper small intestine. The isoleucyl prodrug was shown to be somewhat more stable than the L-valyl prodrug in buffer. Activation (hydrolysis) studies of the prodrugs by Caco-2 cell homogenates indicates that the prodrugs, with the exception of Zan-D-Val, are more rapidly activated to parent drug in tissue. The Caco-2 homogenate results show the half lives for the prodrugs to be less than 40 minutes, somewhat faster than the hydrolysis results in buffer at pH=7.4. At any given time the hydrolysis of the prodrugs (Zan-L-Val and Zan-L-Ile) in Caco-2 homogenate was significantly higher than the corresponding buffer hydrolysis at pH 7.4, suggesting that these prodrugs are effectively activated by the enzymes present in Caco-2 cells. Using the previously identified recombinant valacyclovirase enzyme, the hydrolysis kinetics of the prodrugs by valacyclovirase indicates that the prodrugs are not as good substrates for this enzyme as valacyclovir. However, the rapid hydrolysis of prodrugs in the Caco-2 cell homogenate suggests that there are additional cellular enzymes capable of activating the zanamivir prodrugs in vivo.
The comparison of apparent permeabilities of zanamivir and its prodrugs in Caco-2 monolayers indicates that the L-valyl prodrug had a significantly higher apparent permeability than the parent zanamivir. Most significantly, only the parent drug zanamivir appeared in the receiver compartment, indicating complete hydrolysis during transport through the mucosal cell. The L-valyl prodrug was approximately 3 fold more permeable than the isoleucyl prodrug, which was consistent with the [3H]Gly-Sar uptake inhibition results where there was an approximately 3 fold difference between the affinities of L-valyl and isoleucyl prodrugs. The D-Val prodrug had a lower permeability compared to its L-Val counterpart, indicating a significant stereochemical dependence of the carrier mediated transport mechanism.
The in situ rat perfusion system has best correlation with human oral jejunal mucosal transport for carrier mediated compounds.12 The transport results in this system indicated that zanamivir, as expected, has a very low permeability while the L-valyl prodrug was much more permeable. The isoleucyl and D-valyl prodrugs also showed an increase in permeability though lower than that of L-valyl prodrug. Thus the carrier mediated transport and the cellular activation of the amino acid linked prodrugs of zanamivir have considerable promise in improving the oral bioavailability of zanamivir.
In conclusion, the in vitro and in situ permeation results has shown that the prodrug strategy of targeting a carrier mediated transport pathway in the intestinal epithelial cell developed and described in this work has been very successful in markedly improving the transport, uptake and membrane permeability of zanamivir. The increase in transport and uptake of prodrugs appears to be mediated by the PepT1 transporter, the design target. However, role of other transporters in facilitating membrane transport cannot be ruled out. The in situ intestinal perfusion results demonstrating an intestinal membrane permeability of the linked valine ester of zanamivir comparable to that of metoprolol, combined with the significant mucosal cell hydrolysis (activation) suggest that both good oral absorption and cellular (first-pass, intestinal) activation may result in good systemic availability in humans.
Acknowledgments
This work was supported by NIH RO1 GM 037188.
References
- 1.(a) Moscona A. Neuraminidase inhibitors for influenza. N Engl J Med. 2005;353(13):1363–73. doi: 10.1056/NEJMra050740. [DOI] [PubMed] [Google Scholar]; (b) Masuda H, Suzuki H, Oshitani H, Saito R, Kawasaki S, Nishikawa M, Satoh H. Incidence of amantadine-resistant influenza A viruses in sentinel surveillance sites and nursing homes in Niigata, Japan. Microbiol Immunol. 2000;44(10):833–9. doi: 10.1111/j.1348-0421.2000.tb02571.x. [DOI] [PubMed] [Google Scholar]
- 2.Monto AS. Vaccines and antiviral drugs in pandemic preparedness. Emerg Infect Dis. 2006;12(1):55–60. doi: 10.3201/eid1201.051068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Wetherall NT, Trivedi T, Zeller J, Hodges-Savola C, McKimm-Breschkin JL, Zambon M, Hayden FG. Evaluation of neuraminidase enzyme assays using different substrates to measure susceptibility of influenza virus clinical isolates to neuraminidase inhibitors: report of the neuraminidase inhibitor susceptibility network. J Clin Microbiol. 2003;41(2):742–50. doi: 10.1128/JCM.41.2.742-750.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Le QM, Kiso M, Someya K, Sakai YT, Nguyen TH, Nguyen KH, Pham ND, Ngyen HH, Yamada S, Muramoto Y, Horimoto T, Takada A, Goto H, Suzuki T, Suzuki Y, Kawaoka Y. Avian flu: isolation of drug-resistant H5N1 virus. Nature. 2005;437(7062):1108. doi: 10.1038/4371108a. [DOI] [PubMed] [Google Scholar]
- 5.Zurcher T, Yates PJ, Daly J, Sahasrabudhe A, Walters M, Dash L, Tisdale M, McKimm-Breschkin JL. Mutations conferring zanamivir resistance in human influenza virus N2 neuraminidases compromise virus fitness and are not stably maintained in vitro. J Antimicrob Chemother. 2006;58(4):723–32. doi: 10.1093/jac/dkl321. [DOI] [PubMed] [Google Scholar]
- 6.Cass LM, Efthymiopoulos C, Bye A. Pharmacokinetics of zanamivir after intravenous, oral, inhaled or intranasal administration to healthy volunteers. Clin Pharmacokinet. 1999;36(Suppl 1):1–11. doi: 10.2165/00003088-199936001-00001. [DOI] [PubMed] [Google Scholar]
- 7.(a) Han HK, Amidon GL. Targeted prodrug design to optimize drug delivery. AAPS PharmSci. 2000;2(1):E6. doi: 10.1208/ps020106. [DOI] [PMC free article] [PubMed] [Google Scholar]; (b) Han H, de Vrueh RL, Rhie JK, Covitz KM, Smith PL, Lee CP, Oh DM, Sadee W, Amidon GL. 5′-Amino acid esters of antiviral nucleosides, acyclovir, and AZT are absorbed by the intestinal PEPT1 peptide transporter. Pharm Res. 1998;15(8):1154–9. doi: 10.1023/a:1011919319810. [DOI] [PubMed] [Google Scholar]
- 8.Han HK, Oh DM, Amidon GL. Cellular uptake mechanism of amino acid ester prodrugs in Caco-2/hPEPT1 cells overexpressing a human peptide transporter. Pharm Res. 1998;15(9):1382–6. doi: 10.1023/a:1011945420235. [DOI] [PubMed] [Google Scholar]
- 9.Lai L, Xu Z, Zhou J, Lee KD, Amidon GL. Molecular basis of prodrug activation by human valacyclovirase, an alpha-amino acid ester hydrolase. J Biol Chem. 2008;283(14):9318–27. doi: 10.1074/jbc.M709530200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.(a) Vig BS, Lorenzi PJ, Mittal S, Landowski CP, Shin HC, Mosberg HI, Hilfinger JM, Amidon GL. Amino acid ester prodrugs of floxuridine: synthesis and effects of structure, stereochemistry, and site of esterification on the rate of hydrolysis. Pharm Res. 2003;20(9):1381–8. doi: 10.1023/a:1025745824632. [DOI] [PubMed] [Google Scholar]; (b) Oh DM, Han HK, Amidon GL. Drug transport and targeting. Intestinal transport. Pharm Biotechnol. 1999;12:59–88. doi: 10.1007/0-306-46812-3_3. [DOI] [PubMed] [Google Scholar]; (c) Landowski CP, Song X, Lorenzi PL, Hilfinger JM, Amidon GL. Floxuridine amino acid ester prodrugs: enhancing Caco-2 permeability and resistance to glycosidic bond metabolism. Pharm Res. 2005;22(9):1510–8. doi: 10.1007/s11095-005-6156-9. [DOI] [PubMed] [Google Scholar]; (d) Song X, Lorenzi PL, Landowski CP, Vig BS, Hilfinger JM, Amidon GL. Amino acid ester prodrugs of the anticancer agent gemcitabine: synthesis, bioconversion, metabolic bioevasion, and hPEPT1-mediated transport. Mol Pharm. 2005;2(2):157–67. doi: 10.1021/mp049888e. [DOI] [PubMed] [Google Scholar]
- 11.Svahn CM, Merenyi F, Karlson L. Tranexamic acid derivatives with enhanced absorption. 1986;29:448–453. doi: 10.1021/jm00154a004. [DOI] [PubMed] [Google Scholar]
- 12.Kim JS, Mitchell S, Kijek P, Tsume Y, Hilfinger J, Amidon GL. The suitability of an in situ perfusion model for permeability determinations: utility for BCS class I biowaiver requests. Mol Pharm. 2006;3(6):686–94. doi: 10.1021/mp060042f. [DOI] [PubMed] [Google Scholar]
- 13.Martin R, Witte KL, Wong CH. The synthesis and enzymatic incorporation of sialic acid derivatives for use as tools to study the structure, activity, and inhibition of glycoproteins and other glycoconjugates. Bioorganic & Medicinal Chemistry. 1998;6(8):1283–1292. doi: 10.1016/s0968-0896(98)00121-7. [DOI] [PubMed] [Google Scholar]
- 14.Malcolm Chandler MJB, Conroy Richard, Lamount Brian, Patel Bina, Patel Vipulkumar K, Steeples Ian P, Storer Richard, Weir Naill G, Williamson Michael Wrightm Christopher. Synthesis of the potent influenza neuraminidase inhibitor 4-guanidino Neu5Ac2en. X-Ray molecular structure of 5-acetamido-4-amino-2,6-anhydro-3,4,5-trideoxy-D-erythro-L-gluco-nononic acid. J Chem Soc, Perkin Trans. 1995;1:1173–1180. [Google Scholar]
- 15.Masuda T, Yoshida S, Arai M, Kaneko S, Yamashita M, Honda T. Synthesis and anti-influenza evaluation of polyvalent sialidase inhibitors bearing 4-guanidino-Neu5Ac2en derivatives. Chemical & pharmaceutical bulletin. 2003;51(12):1386–98. doi: 10.1248/cpb.51.1386. [DOI] [PubMed] [Google Scholar]
- 16.Nudelman A, Gnizi E, Katz Y, Azulai R, Cohen-Ohana M, Zhuk R, Sampson SR, Langzam L, Fibach E, Prus E, Pugach V, Rephaeli A. Prodrugs of butyric acid. Novel derivatives possessing increased aqueous solubility and potential for treating cancer and blood diseases. Eur J Med Chem. 2001;36(1):63–74. doi: 10.1016/s0223-5234(00)01199-5. [DOI] [PubMed] [Google Scholar]
- 17.Gomes P, Santos MI, Trigo MJ, Castanheiro R, Moreira R. Improved Synthesis of Amino Acid and Dipeptide Chloromethyl Esters Using Bromochloromethane. Synthetic Communications. 2003;33(10):1683–1693. [Google Scholar]
- 18.Hsu CP, Hilfinger JM, Walter E, Merkle HP, Roessler BJ, Amidon GL. Overexpression of human intestinal oligopeptide transporter in mammalian cells via adenoviral transduction. Pharm Res. 1998;15(9):1376–81. doi: 10.1023/a:1011993303397. [DOI] [PubMed] [Google Scholar]
- 19.Gupta D, Gupta SV, Lee KD, Amidon GL. Chemical and enzymatic stability of amino acid prodrugs containing methoxy, ethoxy and propylene glycol linkers. Mol Pharm. 2009;6(5):1604–11. doi: 10.1021/mp900084v. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Amidon GL, Sinko PJ, Fleisher D. Estimating human oral fraction dose absorbed: a correlation using rat intestinal membrane permeability for passive and carrier-mediated compounds. Pharm Res. 1988;5(10):651–4. doi: 10.1023/a:1015927004752. [DOI] [PubMed] [Google Scholar]
- 21.Fagerholm U, Johansson M, Lennernas H. Comparison between permeability coefficients in rat and human jejunum. Pharm Res. 1996;13(9):1336–42. doi: 10.1023/a:1016065715308. [DOI] [PubMed] [Google Scholar]
- 22.(a) Sinkula AA, Yalkowsky SH. Rationale for design of biologically reversible drug derivatives: prodrugs. J Pharm Sci. 1975;64(2):181–210. doi: 10.1002/jps.2600640203. [DOI] [PubMed] [Google Scholar]; (b) Ettmayer P, Amidon GL, Clement B, Testa B. Lessons learned from marketed and investigational prodrugs. J Med Chem. 2004;47(10):2393–404. doi: 10.1021/jm0303812. [DOI] [PubMed] [Google Scholar]; (c) Rautio J, Kumpulainen H, Heimbach T, Oliyai R, Oh D, Jarvinen T, Savolainen J. Prodrugs: design and clinical applications. Nat Rev Drug Discov. 2008;7(3):255–70. doi: 10.1038/nrd2468. [DOI] [PubMed] [Google Scholar]; (d) Beaumont K, Webster R, Gardner I, Dack K. Design of ester prodrugs to enhance oral absorption of poorly permeable compounds: challenges to the discovery scientist. Curr Drug Metab. 2003;4(6):461–85. doi: 10.2174/1389200033489253. [DOI] [PubMed] [Google Scholar]; (e) Stella VJ, et al., editors. Prodrugs, Challenges and Rewards part 1 and Part 2. Springer; New Yord: 2007. [Google Scholar]
- 23.Fleisher D, Bong R, Stewart BH. Improved oral drug delivery: solubility limitations overcome by the use of prodrugs. Advanced Drug Delivery Reviews. 1996;19(2):115–130. [Google Scholar]
- 24.(a) Rubio-Aliaga I, Daniel H. Mammalian peptide transporters as targets for drug delivery. Trends Pharmacol Sci. 2002;23(9):434–40. doi: 10.1016/s0165-6147(02)02072-2. [DOI] [PubMed] [Google Scholar]; (b) Herrera-Ruiz D, Knipp GT. Current perspectives on established and putative mammalian oligopeptide transporters. J Pharm Sci. 2003;92(4):691–714. doi: 10.1002/jps.10303. [DOI] [PubMed] [Google Scholar]
- 25.Faria TN, Timoszyk JK, Stouch TR, Vig BS, Landowski CP, Amidon GL, Weaver CD, Wall DA, Smith RL. A novel high-throughput pepT1 transporter assay differentiates between substrates and antagonists. Mol Pharm. 2004;1(1):67–76. doi: 10.1021/mp034001k. [DOI] [PubMed] [Google Scholar]
- 26.Landowski CP, Vig BS, Song X, Amidon GL. Targeted delivery to PEPT1-overexpressing cells: acidic, basic, and secondary floxuridine amino acid ester prodrugs. Mol Cancer Ther. 2005;4(4):659–67. doi: 10.1158/1535-7163.MCT-04-0290. [DOI] [PubMed] [Google Scholar]