Abstract
Sleep disordered breathing (SDB) in children is common. The impact of SDB on the growth and development of child may have detrimental effects on health, neuropsychological development, quality of life, and economic potential; therefore, SDB in children should be recognized as a public health problem as in the adult population. The coexistence of obesity and obstructive sleep apnea (OSA) not only appears to yield increased morbidity rates and poorer responses to therapy, but also is altogether associated with a distinct and recognizable clinical phenotype. Therapeutic options have somewhat expanded since the initial treatment approaches were conducted, to include not only surgical extraction of hypertrophic adenoids and tonsils, but also nonsurgical alternatives such as continuous positive air pressure, anti-inflammatory agents and oral appliances (OAs). Now, American academy of sleep medicine (AAOSM) has recommended OAs for OSA, hence the therapeutic interventions that are directed at the site of airway obstruction in the maxillofacial region are within the scope of dentistry. Among the physicians treating the children, dentists are more likely to identify adenotonsillar hypertrophy. Hence, the dentist can play an important role in identifying and treating those cases with OAs, who refuse the surgery, or those with structural abnormality in which myofunctional appliances are beneficial.
Keywords: Obstructive sleep apnea, oral appliances, polysomnography
INTRODUCTION
Sleep is a major physiological drive. An average child spends almost one-half of his or her life asleep. A newborn sleeps for as much as 16 hours a day, which plays an important role in children's development. Sleep disorders can impair child's health and lead to negative consequences. Thus, respiratory disorders during sleep like obstructive sleep apnea (OSA) are of particular importance during childhood. OSA is characterized by repeated episodes of airway obstruction for more than 10 seconds during sleep, resulting in pauses in breathing. OSA is the most common condition among a group of disorders called sleep disordered breathing (SDB) that can affect both adults and children. Recently, increasing attention has been paid to OSA among children. Epidemiologic studies have shown that the prevalence of SDB is about 2% among children[1,2] and about 2.5–6% among adolescents.[3] Goodwin and others[4] observed that boys are more likely to have OSA, which is consistent with the tendency for overweight adult males to have OSA. OSA in children has emerged not only as a relatively prevalent condition but also as a disease that imposes a large array of morbidities, some of which may have long-term implications, well into adulthood. Among the physicians treating children, dentists are most likely to identify adenotonsillar hypertrophy; thus, it may be in the patient's best interests if dentists act as “gatekeepers” in identifying children with adenotonsillar hypertrophy. This review is attempted to provide the role of the oral health professional in the diagnosis and management of OSA.
PATHOPHYSIOLOGY OF OBSTRUCTIVE SLEEP APNEA
The etiology of childhood OSA is quite different from that of the adult condition. In adults, OSA is usually associated with obesity and other causes. Obese children are also at risk for OSA, and the degree of OSA is proportional to the degree of obesity.[5] However, most children with OSA are not obese. In fact, they may have failure to thrive. Instead, the vast majority of cases of OSA in children are associated with adenotonsillar hypertrophy [Figure 1]. The peak prevalence of childhood OSA is at 2–8 years, which is the age when the tonsils and adenoids are the largest in relation to the underlying airway size; endoscopy has shown that the site of collapse is most often at the level of the adenoid[6] and most children with OSA improve following tonsillectomy and adenoidectomy (T and A).[7] OSA also occurs in children with upper airway narrowing [Figure 2] due to malocclusion and craniofacial anomalies or those with neuromuscular abnormalities such as hypotonia (e.g., muscular dystrophy)[8] or muscular incoordination (e.g., cerebral palsy).[9]
Figure 1.
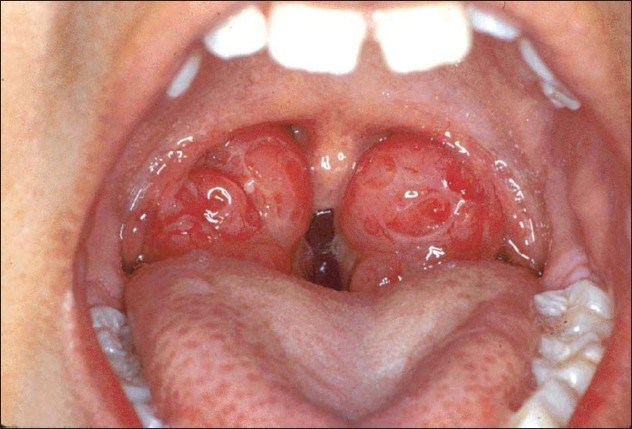
Massive tonsils could obstruct airway
Figure 2.
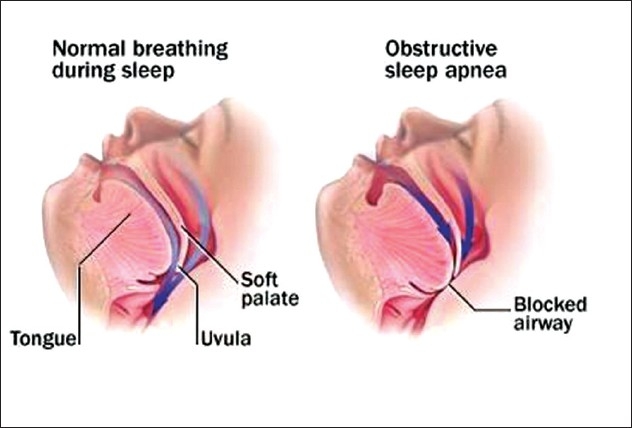
Blocked airway in OSA
Guilleminault and colleagues reported a cohort of children who were cured of their OSA by adenotonsillectomy, but developed a recurrence during adolescence.[10] Thus, it appears that childhood OSA is a dynamic process resulting from a combination of structural and neuromotor abnormalities, rather than from structural abnormalities alone.
McNamara and coworkers[11] found that obstructive apneas were associated with arousal in less than half of the apneas in children and only 18% of apneas in infants. As a result, sleep architecture is preserved in children with OSA,[12,13] and therefore, excessive daytime sleepiness, the cardinal symptom of OSA in adults, is uncommon in children.[14] However, although apnea-related electroencephalogram (EEG) arousals are less common in children than in adults, subcortical arousals, as demonstrated by movement[15,16] or autonomic changes,[17] occur frequently. It is also possible that subtle disturbances in sleep architecture, which cannot be detected on routine polysomnography (PSG), are present.[18] These factors may contribute to neurobehavioral and autonomic complications.
DIAGNOSIS
Diagnosis of OSAs is based on clinical suspicion, history and physical findings, and confirmation is made by PSG.
History and physical evaluation
Nocturnal symptoms
Snoring and difficulty in breathing during sleep are the most common complaints of parents of children with OSAs, with reports of such symptoms in more than 96% of cases.[19,20] However, the history of snoring alone cannot distinguish between children with OSA and children with primary snoring.[21]
Children appear to be very restless during the night, frequently changing sleep positions[22] and may prefer sleeping while sitting upright or propped upon pillows [Figure 3]. Other common nocturnal findings include increased diaphoresis and enuresis. Chronic sleep apnea may lead to cor pulmonale and pulmonary hypertension.
Figure 3.

Characteristic sleeping position of child with sleep apnea
Daytime symptoms
Although respiration in children with OSA is typically unremarkable during wakefulness, some children with severe OSA may manifest difficulty in breathing when awake, albeit less so than when asleep. Excessive daytime somnolence in children has been shown to correlate with severity of OSA and with increased body mass index.[23] However, in contrast to reports in adults with OSA, excessive daytime somnolence is less common in children with OSA, being present in 7–10% of children with OSA.[23,24]
Behavioral manifestations of children with OSA may be very similar to those with attention deficit hyperactivity disorder.[19,20,25] Both the disorders may present with symptoms of hyperactivity, inattentiveness and poor academic performance.
Physical examination
Physical examination begins with a general observation of the patient. Mouth breathing and adenoidal facies should be noted. Hyponasal voice is a clue of nasal obstruction and a muffled voice is suggestive of adenotonsillar enlargement. The lateral facial profile should be inspected for retrognathia, micrognathia [Figure 4] or midfacial hypoplasia. All these can affect the nasopharyngeal and oropharyngeal passages and are key findings for diagnosis. The oral cavity should be observed for tongue and soft palate size and appearance: a large tongue and/or a high-arched or elongated palate, or a low dependent palate may predispose to SDB.
Figure 4.

Child with OSA associated with mandibular retrognathia
Upper airway evaluation
Upper airway evaluation can be done with endoscopy/laryngoscopy,pharyngometry and radiographic evaluation [computed tomography (CT) or magnetic resonance imaging (MRI)].
Home monitoring
Unattended home studies in children with OSA have been improving in quality. In one study using a comprehensive methodology including cardiorespiratory and 8 hours of video recording, results obtained were very similar to those obtained by PSG in the laboratory.[26]
Polysomnography
PSG is the gold standard in the diagnosis of OSA. PSG involves the overnight recording of sleep breathing patterns and oxygen saturation. PSG provide apnea hypopnea index (AHI) score. AHI scores are an estimation of apneic-hypopneic episode per hour of sleep. Among children, an AHI >1 and oxygen desaturations ≥ 4% are indicators of mild OSA.[27–29] In comparison, an AHI of 5 (or sometimes 10) among adults generally indicates mild OSA.
TREATMENT OF OBSTRUCTIVE SLEEP APNEA IN CHILDREN
treatment of OSA in children depends largely on the underlying cause of the problem and may include one of the following.
Surgical treatment of obstructive sleep apnea
Adenotonsillectomy (T and A) is generally considered to be the standard treatment of childhood sleep apnea with normal craniofacial features and uncomplicated medical status. T and A is curative of sleep apnea in a majority of the pediatric cases.[30] However, not all children who undergo T and A for OSA are cured.[31–33] In a meta-analysis of the published literature, the success rate for T and A in the context of OSA was observed to be approximately 85%.[34] This figure may actually be lower, particularly among obese children with OSA[35–39] or among children with severe OSA.[35,38]
Diet and medications
For obese children, weight loss and maintaining a healthy diet might prove to be the ultimate treatment for their OSA.[40] Antibiotic medication,[41] topical intranasal application of corticosteroids,[42] leukotriene receptor antagonist[43] and anti-inflammatory therapy[44] can be used for mild or residual OSA after surgery.
Positive airway pressure treatment
Continuous positive airway pressure (CPAP) is the first-line therapy for adult sleep apnea and is considered the second-line therapy in children since surgical therapy is generally curative. CPAP has been studied in children[45,46] and has been found to be effective for the treatment of OSA.[47] CPAP has been approved by the US Food and Drug Administration for use in children >7 years of age in the United States.
Oral appliances
The role of oral appliances (OAs) in the treatment of patients with OSA has gained prominence since their introduction in 1982. Recently, the American Academy of Sleep Medicine published practice parameters for the treatment of snoring and OSA with OA, establishing a first-line role for OA in the treatment of adult patients with mild-to-moderate OSA, and a second-line role for patients with severe OSA.[48] While these practice parameters recommend that an OA should be prescribed by experienced dental personnel knowledgeable in sleep medicine and/or sleep-related breathing disorders, relatively few dentists have the necessary training to accurately identify OSA or treat the entity with an OA [Figure 5 and Algorithm 1 showing the mode of action of OAs in OSA].
Figure 5.
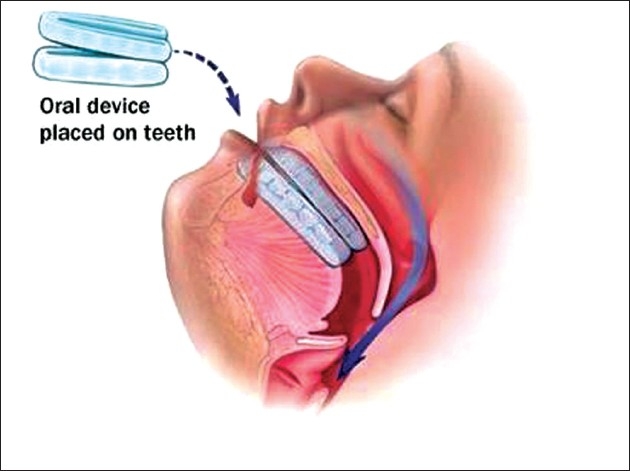
Mode of action of OAs
Algorithm 1.
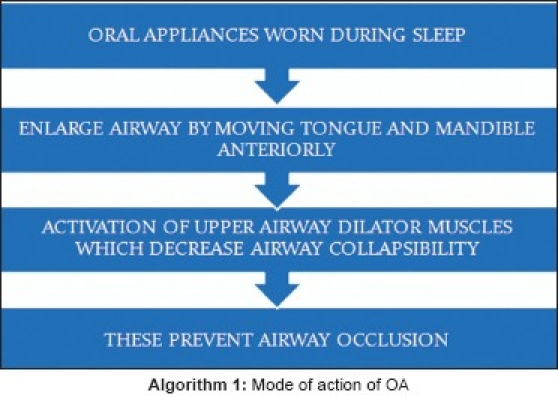
Mode of action of OA
Finally, OAs [Figure 6], which are primarily provided by dentists, have become increasingly popular within the past few years for the treatment of OSA.[49–51] OAs are of particular interest to people who opt not to have surgery and cannot tolerate CPAP treatment. OAs provide effective treatment for many patients and, in one study, were shown to be effective in as many as 50% of patients with OSA.[50] Researchers investigating the use of OAs for children[52–54] have found certain types to be particularly effective in treating OSA. For example, according to Cozza and colleagues,[53,54] a new orthodontic appliance, a modified monobloc, not only is effective in reducing apneic events during sleep, but also improves subjective sleep quality and daytime performance among children. Recently, a study published by Etsuko Miyao and others who conducted orthodontic treatment using an OA for a child with mandibular retrusion and sleep apnea syndrome (SAS), reported that it was cured following orthodontic treatment.[55] The present study shows that patients with skeletal problems such as maxillary protrusion, mandibular micrognathia and mandibular retrusion can expect a significant improvement of snoring and SAS due to the forward movement or growth of the mandible [Figure 7]. Various orthodontic appliances have been used to move or make the mandible grow forward in patients with micrognathia or mandibular retrusion. The use of OAs has involved dentists in the treatment of OSA among both adults and children.
Figure 6.
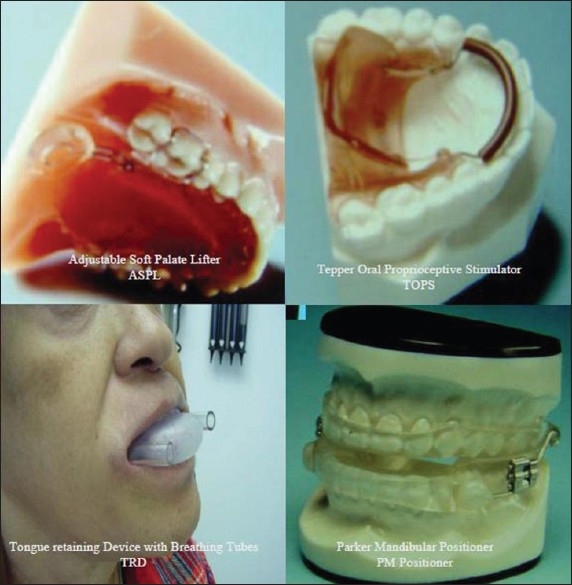
Various OAs used in OSA
Figure 7.

Pretreatment and post treatment lateral head cephalogram showing mandibular advancement
ROLE OF DENTISTS IN DIAGNOSIS AND TREATMENT OF SLEEP APNEA IN CHILDREN
According to Brouillette and colleagues,[25] increasing awareness of OSA and examination of sleeping patients should result in earlier treatment and less morbidity for infants and children with OSA. As adenotonsillar hypertrophy is one of the main causes of OSA among children, investigating the prevalence of OSA among children with adenotonsillar hypertrophy is an important research task. There is evidence that physicians may not always recognize childhood OSA.[56] According to Konno and colleagues,[57] an average delay of 23 months occurred between identification of pediatric patients with large tonsils and their referral to a sleep clinic.
Among the physicians treating children, dentists are most likely to identify adenotonsillar hypertrophy; thus, it may be in the patient's best interests if dentists act as “gatekeepers” in identifying children with adenotonsillar hypertrophy. As discussed above, dentists are becoming increasingly aware of sleep apnea in adults, as some are involved in using OAs to treat this disorder. Once dentists identify children with adenotonsillar hypertrophy, they should inform the parents about the risk of OSA and further inform their family physician about the importance of sleep assessment in children with enlarged tonsils. Involvement of dentists in this process can contribute significantly to the health of patients, as OSA, with such significant developmental consequences, can be diagnosed and treated at an early stage, preventing later problems and complications.
CONCLUSION
SDB in children is common. The impact of SDB on the growth and development of a child may have detrimental effects on health, neuropsychological development, quality of life and economic potential; therefore, SDB in children should be recognized as a public health problem as it is in the adult population. In identifying and treating OSA among children with adenotonsillar hypertrophy, dentists can play an important role by noting the size of the tonsils when looking into child's mouth and informing the child's parents and the primary care physician when enlarged tonsils are observed.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
REFERENCES
- 1.Wildhaber JH, Moeller A. Sleep and respiration in children: Time to wake up! Swiss Med Wkly. 2007;137:689–94. doi: 10.4414/smw.2007.11986. [DOI] [PubMed] [Google Scholar]
- 2.Rosen CL, Larkin EK, Kirchner HL, Emancipator JL, Bivins SF, Surovec SA, et al. Prevalence and risk factors for sleep-disordered breathing in 8- to 11-year-old children: Association with race and prematurity. J Pediatr. 2003;142:383–9. doi: 10.1067/mpd.2003.28. [DOI] [PubMed] [Google Scholar]
- 3.Johnson EO, Roth T. An epidemiologic study of sleep-disordered breathing symptoms among adolescents. Sleep. 2006;29:1135–42. doi: 10.1093/sleep/29.9.1135. [DOI] [PubMed] [Google Scholar]
- 4.Goodwin JL, Kaemingk KL, Mulvaney SA, Morgan WJ, Quan SF. Clinical screening of school children for polysomnography to detect sleep-disordered breathing: The Tucson Children's Assessment of Sleep Apnea study (TuCASA) J Clin Sleep Med. 2005;1:247–54. [PMC free article] [PubMed] [Google Scholar]
- 5.Marcus CL, Curtis S, Koerner CB, Joffe A, Serwint JR, Loughlin GM. Evaluation of pulmonary function and polysomnography in obese children and adolescents. Pediatr Pulmonol. 1996;21:176–83. doi: 10.1002/(SICI)1099-0496(199603)21:3<176::AID-PPUL5>3.0.CO;2-O. [DOI] [PubMed] [Google Scholar]
- 6.Isono S, Shimada A, Utsugi M, Konno A, Nishino T. Comparison of static mechanical properties of the passive pharynx between normal children and children with sleep-disordered breathing. Am J Respir Crit Care Med. 1998;157:1204–12. doi: 10.1164/ajrccm.157.4.9702042. [DOI] [PubMed] [Google Scholar]
- 7.Suen JS, Arnold JE, Brooks LJ. Adenotonsillectomy for treatment of obstructive sleep apnea in children. Arch Otolaryngol Head Neck Surg. 1995;121:525–30. doi: 10.1001/archotol.1995.01890050023005. [DOI] [PubMed] [Google Scholar]
- 8.Khan Y, Heckmatt JZ. Obstructive apnoeas in Duchenne muscular dystrophy. Thorax. 1994;49:157–61. doi: 10.1136/thx.49.2.157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kotagal S, Gibbons VP, Stith JA. Sleep abnormalities in patients with severe cerebral palsy. Dev Med Child Neurol. 1994;36:304–11. doi: 10.1111/j.1469-8749.1994.tb11850.x. [DOI] [PubMed] [Google Scholar]
- 10.Guilleminault C, Partinen M, Praud JP, Quera-Salva MA, Powell N, Riley R. Morphometric facial changes and obstructive sleep apnea in adolescents. J Pediatr. 1989;114:997–9. doi: 10.1016/s0022-3476(89)80447-0. [DOI] [PubMed] [Google Scholar]
- 11.McNamara F, Issa FG, Sullivan CE. Arousal pattern following central and obstructive breathing abnormalities in infants and children. J Appl Physiol. 1996;81:2651–7. doi: 10.1152/jappl.1996.81.6.2651. [DOI] [PubMed] [Google Scholar]
- 12.Goh DY, Galster P, Marcus CL. Sleep architecture and respiratory disturbances in children with obstructive sleep apnea. Am J Respir Crit Care Med. 2000;162:682–6. doi: 10.1164/ajrccm.162.2.9908058. [DOI] [PubMed] [Google Scholar]
- 13.Marcus CL, Carroll JL, Koerner CB, Hamer A, Lutz J, Loughlin GM. Determinants of growth in children with the obstructive sleep apnea syndrome. J Pediatr. 1994;125:556–62. doi: 10.1016/s0022-3476(94)70007-9. [DOI] [PubMed] [Google Scholar]
- 14.Carroll JL, Loughlin GM. Obstructive sleep apnea syndrome in infants and children: Clinical features and pathophysiology. In: Carroll JL, Loughlin GM, editors. Principles and practice of sleep medicine in the child. Philadelphia: W. B. Saunders Company; 1995. pp. 163–91. [Google Scholar]
- 15.Praud JP, D’Allest AM, Nedelcoux H, Curzi-Dascalova L, Guilleminault C, Gaultier C. Sleep-related abdominal muscle behavior during partial or complete obstructed breathing in prepubertal children. Pediatr Res. 1989;26:347–50. doi: 10.1203/00006450-198910000-00012. [DOI] [PubMed] [Google Scholar]
- 16.Mograss MA, Ducharme FM, Brouillette RT. Movement/arousals.Description, classification, and relationship to sleep apnea in children. Am J Respir Crit Care Med. 1994;150:1690–6. doi: 10.1164/ajrccm.150.6.7952634. [DOI] [PubMed] [Google Scholar]
- 17.Aljadeff G, Gozal D, Schechtman VL, Burrell B, Harper RM, Ward SL. Heart rate variability in children with obstructive sleep apnea. Sleep. 1997;20:151–7. doi: 10.1093/sleep/20.2.151. [DOI] [PubMed] [Google Scholar]
- 18.Bandla HP, Gozal D. Dynamic changes in EEG spectra during obstructive apnea in children. Pediatr Pulmonol. 2000;29:359–65. doi: 10.1002/(sici)1099-0496(200005)29:5<359::aid-ppul4>3.0.co;2-o. [DOI] [PubMed] [Google Scholar]
- 19.Guilleminault C, Korobkin R, Winkle R. A review of 50 children with obstructive sleep apnea syndrome. Lung. 1981;159:275–87. doi: 10.1007/BF02713925. [DOI] [PubMed] [Google Scholar]
- 20.Brouilette R, Hanson D, David R, Klemka L, Szatkowski A, Fernbach S, et al. A diagnostic approach to suspected obstructive sleep apnea in children. J Pediatr. 1984;105:10–4. doi: 10.1016/s0022-3476(84)80348-0. [DOI] [PubMed] [Google Scholar]
- 21.Carroll JL, McColley SA, Marcus CL, Curtis S, Loughlin GM. Inability of clinical history to distinguish primary snoring from obstructive sleep apnea syndrome in children. Chest. 1995;108:610–8. doi: 10.1378/chest.108.3.610. [DOI] [PubMed] [Google Scholar]
- 22.Stradling JR, Thomas G, Warley AR, Williams P, Freeland A. Effect of adenotonsillectomy on nocturnal hypoxaemia, sleep disturbance, and symptoms in snoring children. Lancet. 1990;335:249–53. doi: 10.1016/0140-6736(90)90068-g. [DOI] [PubMed] [Google Scholar]
- 23.Gozal D, Wang M, Pope DW., Jr Objective sleepiness measures in pediatric obstructive sleep apnea. Pediatrics. 2001;108:693–7. doi: 10.1542/peds.108.3.693. [DOI] [PubMed] [Google Scholar]
- 24.Rosen CL. Clinical features of obstructive sleep apnea hypoventilation syndrome in otherwise healthy children. Pediatr Pulmonol. 1999;27:403–9. doi: 10.1002/(sici)1099-0496(199906)27:6<403::aid-ppul7>3.0.co;2-8. [DOI] [PubMed] [Google Scholar]
- 25.Brouillette RT, Fernbach SK, Hunt CE. Obstructive sleep apnea in infants and children. J Pediatr. 1982;100:31–40. doi: 10.1016/s0022-3476(82)80231-x. [DOI] [PubMed] [Google Scholar]
- 26.Jacob SV, Morielli A, Mograss MA, Ducharme FM, Schloss MD, Brouillette RT. Home testing for pediatric obstructive sleep apnea syndrome secondary to adenotonsillar hypertrophy. Pediatr Pulmonol. 1995;20:241–52. doi: 10.1002/ppul.1950200407. [DOI] [PubMed] [Google Scholar]
- 27.Marcus CL, Omlin KJ, Basinki DJ, Bailey SL, Rachal AB, Von Pechmann WS, et al. Normal polysomnographic values for children and adolescents. Am Rev Respir Dis. 1992;146:1235–9. doi: 10.1164/ajrccm/146.5_Pt_1.1235. [DOI] [PubMed] [Google Scholar]
- 28.Uliel S, Tauman R, Greenfeld M, Sivan Y. Normal polysomnographic respiratory values in children and adolescents. Chest. 2004;125:872–8. doi: 10.1378/chest.125.3.872. [DOI] [PubMed] [Google Scholar]
- 29.Montgomery-Downs HE, O’Brien LM, Gulliver TE, Gozal D. Polysomnographic characteristics in normal preschool and early school-aged children. Pediatrics. 2006;117:741–53. doi: 10.1542/peds.2005-1067. [DOI] [PubMed] [Google Scholar]
- 30.Brietzke SE, Gallagher D. The effectiveness of tonsillectomy and adenoidectomy in the treatment of pediatric obstructive sleep apnea/hypopnea syndrome: A meta-analysis. Otolaryngol Head Neck Surg. 2006;134:979–84. doi: 10.1016/j.otohns.2006.02.033. [DOI] [PubMed] [Google Scholar]
- 31.Rosen GM, Muckle RP, Mahowald MW, Goding GS, Ullevig C. Postoperative respiratory compromise in children with obstructive sleep apnea syndrome: Can it be anticipated? Pediatrics. 1994;93:784–8. [PubMed] [Google Scholar]
- 32.Tal A, Bar A, Leiberman A, Tarasiuk A. Sleep characteristics following adenotonsillectomy in children with obstructive sleep apnea syndrome. Chest. 2003;124:948–53. doi: 10.1378/chest.124.3.948. [DOI] [PubMed] [Google Scholar]
- 33.Mitchell RB, Kelly J. Outcome of adenotonsillectomy for severe obstructive sleep apnea in children. Int J Pediatr Otorhinolaryngol. 2004;68:1375–9. doi: 10.1016/j.ijporl.2004.04.026. [DOI] [PubMed] [Google Scholar]
- 34.Lipton AJ, Gozal D. Treatment of obstructive sleep apnea in children: Do we really know how? Sleep Med Rev. 2003;7:61–80. doi: 10.1053/smrv.2001.0256. [DOI] [PubMed] [Google Scholar]
- 35.Tauman R, Gulliver TE, Krishna J, Montgomery-Downs HE, O’Brien LM, Ivanenko A, et al. Persistence of obstructive sleep apnea syndrome in children after adenotonsillectomy. J Pediatr. 2006;149:803–8. doi: 10.1016/j.jpeds.2006.08.067. [DOI] [PubMed] [Google Scholar]
- 36.Guilleminault C, Huang YS, Glamann C, Li K, Chan A. Adenotonsillectomy and obstructive sleep apnea in children: A prospective survey. Otolaryngol Head Neck Surg. 2007;136:169–75. doi: 10.1016/j.otohns.2006.09.021. [DOI] [PubMed] [Google Scholar]
- 37.Mitchell RB, Kelly J. Outcome of adenotonsillectomy for obstructive sleep apnea in obese and normal-weight children. Otolaryngol Head Neck Surg. 2007;137:43–8. doi: 10.1016/j.otohns.2007.03.028. [DOI] [PubMed] [Google Scholar]
- 38.Shine NP, Lannigan FJ, Coates HL, Wilson A. Adenotonsillectomy for obstructive sleep apnea in obese children: Effects on respiratory parameters and clinical outcome. Arch Otolaryngol Head Neck Surg. 2006;132:1123–7. doi: 10.1001/archotol.132.10.1123. [DOI] [PubMed] [Google Scholar]
- 39.Mitchell RB. Adenotonsillectomy for obstructive sleep apnea in children: Outcome evaluated by pre- and postoperative polysomnography. Laryngoscope. 2007;117:1844–54. doi: 10.1097/MLG.0b013e318123ee56. [DOI] [PubMed] [Google Scholar]
- 40.Benninger M, Walner D. Obstructive sleep-disordered breathing in children. Clin Cornerstone. 2007;9:S6–12. doi: 10.1016/s1098-3597(07)80004-4. [DOI] [PubMed] [Google Scholar]
- 41.Sclafani AP, Ginsburg J, Shah MK, Dolitsky JN. Treatment of symptomatic chronic adenotonsillar hypertrophy with amoxicillin/clavulanate potassium: Short- and long-term results. Pediatrics. 1998;101:675–81. doi: 10.1542/peds.101.4.675. [DOI] [PubMed] [Google Scholar]
- 42.Alexopoulos EI, Kaditis AG, Kalampouka E, Kostadima E, Angelopoulos NV, Mikraki V, et al. Nasal corticosteroids for children with snoring. Pediatr Pulmonol. 2004;38:161–7. doi: 10.1002/ppul.20079. [DOI] [PubMed] [Google Scholar]
- 43.Goldbart AD, Goldman JL, Veling MC, Gozal D. Leukotriene modifier therapy for mild sleep-disordered breathing in children. Am J Respir Crit Care Med. 2005;172:364–70. doi: 10.1164/rccm.200408-1064OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Goldbart AD, Krishna J, Li RC, Serpero LD, Gozal D. Inflammatory mediators in exhaled breath condensate of children with obstructive sleep apnea syndrome. Chest. 2006;130:143–8. doi: 10.1378/chest.130.1.143. [DOI] [PubMed] [Google Scholar]
- 45.Marcus CL, Rosen G, Ward SL, Halbower AC, Sterni L, Lutz J, et al. Adherence to and effectiveness of positive airway pressure therapy in children with obstructive sleep apnea. Pediatrics. 2006;117:e442–51. doi: 10.1542/peds.2005-1634. [DOI] [PubMed] [Google Scholar]
- 46.McNamara F, Harris MA, Sullivan CE. Effects of nasal continuous positive airway pressure on apnoea index and sleep in infants. J Paediatr Child Health. 1995;31:88–94. doi: 10.1111/j.1440-1754.1995.tb00753.x. [DOI] [PubMed] [Google Scholar]
- 47.McNamara F, Sullivan CE. Obstructive sleep apnea in infants and its management with nasal continuous positive airway pressure. Chest. 1999;116:10–6. doi: 10.1378/chest.116.1.10. [DOI] [PubMed] [Google Scholar]
- 48.Kushida CA, Morgenthaler TI, Littner MR, Alessi CA, Bailey D, Coleman J, Jr, et al. Practice parameters for the treatment of snoring and obstructive sleep apnea with oral appliances: An update for 2005. Sleep. 2006;29:240–3. doi: 10.1093/sleep/29.2.240. [DOI] [PubMed] [Google Scholar]
- 49.Bian H. Knowledge, opinions, and clinical experience of general practice dentists toward obstructive sleep apnea and oral appliances. Sleep Breath. 2004;8:85–90. doi: 10.1007/s11325-004-0085-4. [DOI] [PubMed] [Google Scholar]
- 50.Ng A, Gotsopoulos H, Darendeliler AM, Cistulli PA. Oral appliance therapy for obstructive sleep apnea. Treat Respir Med. 2005;4:409–22. doi: 10.2165/00151829-200504060-00005. [DOI] [PubMed] [Google Scholar]
- 51.Hoffstein V. Review of oral appliances for treatment of sleep-disordered breathing. Sleep Breath. 2007;11:1–22. doi: 10.1007/s11325-006-0084-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Schessl J, Rose E, Korinthenberg R, Henschen M. Severe obstructive sleep apnea alleviated by oral appliance in a three-year-old boy. Respiration. 2008;76:112–6. doi: 10.1159/000098407. [DOI] [PubMed] [Google Scholar]
- 53.Cozza P, Gatto R, Ballanti F, Prete L. Management of obstructive sleep apnoea in children with modified monobloc appliances. Eur J Paediatr Dent. 2004;5:24–9. [PubMed] [Google Scholar]
- 54.Cozza P, Polimeni A, Ballanti F. A modified monobloc for the treatment of obstructive sleep apnoea in paediatric patients. Eur J Orthod. 2004;26:523–30. doi: 10.1093/ejo/26.5.523. [DOI] [PubMed] [Google Scholar]
- 55.Miyao E, Nakayama M, Noda A, Miyao M, Arasaki H. Oral appliance therapy for a child with sleep apnea syndrome due to palatine tonsil hypertrophy. Sleep Biol Rhythms. 2007;5:288–90. [Google Scholar]
- 56.Tamay Z, Akcay A, Kilic G, Suleyman A, Ones U, Guler N. Are physicians aware of obstructive sleep apnea in children? Sleep Med. 2006;7:580–4. doi: 10.1016/j.sleep.2006.04.004. [DOI] [PubMed] [Google Scholar]
- 57.Konno A, Hoshino T, Togawa K. Influence of upper airway obstruction by enlarged tonsils and adenoids upon recurrent infection of the lower airway in childhood. Laryngoscope. 1980;90:1709–16. [PubMed] [Google Scholar]


