Abstract
Osteomyelitis is a disease which is heterogeneous in its pathophysiology, clinical presentation and management. It is considered to be one of the most difficult-to-treat infectious diseases. Progressive bony destruction and the formation of sequestra are hallmarks of osteomyelitis. We hereby report a rare case of maxillary osteomyelitis, which had actinomycotic osteomyelitis like presentation but was histopathologically diagnosed as a severe form of chronic suppurative osteomyelitis.
Keywords: Actinomycotic osteomyelitis, chronic suppurative osteomyelitis, osteomyelitis
INTRODUCTION
Osteomyelitis is an inflammatory condition of bone, involving the medullary cavity and the adjacent cortex. It occurs more frequently in the mandible than in the maxilla;[1] although most of the cases of osteomyelitis of the jaws are of odontogenic origin, other sources of infection are also reported.[2]
The condition was originally described by Rees in 1947.[3] It is an inflammatory reaction of bone to infection which originates from either a tooth, fracture site, soft tissue wound or surgical site. The dental infection may be from a root canal, a periodontal ligament or an extraction site. Suppurative osteomyelitis can involve all three components of bone: periosteum, cortex and marrow. Osteomyelitis of the maxilla is much less frequent than that of the mandible because the maxillary blood supply is more extensive. Thin cortical plate and a relatively rare paucity of medullary tissue in the maxilla preclude confinement of infection within bone and permit the dissipation of edema and pus into the soft tissue and paranasal sinuses.[4]
The maxilla rarely undergoes necrosis, due to its rich vascularity. Maxillary necrosis can occur due to bacterial infections such as osteomyelitis, viral infections such as herpes zoster or fungal infections such as mucormycosis, aspergillosis, etc.[5]
In established suppurative osteomyelitis, symptoms include deep pain, malaise, fever and anorexia. Within 10–14 days after onset, teeth in the involved area begin to loosen and become sensitive to percussion. Pus exudes around the gingival sulcus or through mucosal and cutaneous fistulae. Firm cellulitis of the cheek, enlargement of the dimensions of the bone from increased periosteal activity, abscess formation with localized warmth, erythema and tenderness to palpation may be noted. Osteomyelitis of the jaws usually requires both medical and surgical treatment.
CASE REPORT
We hereby report a rare case of osteomyelitis in an otherwise healthy patient who reported to us with complaints of multiple pus discharging sinuses [Figure 1] as is usually seen in actinomycotic conditions, associated with pain in the upper jaw. On examination, there was generalized mobility of all the maxillary teeth, associated with bone exposure (sequestrum) in the left molar region on the buccal aspect [Figure 2]. Orthopantomogram (OPG) was advised, which showed [Figure 3] areas of bone loss in the maxilla around the teeth from first molar of one side to the first molar of the other side. The patient was again advised to get a computed tomography (CT) scan done to know the nature and extent of the disease. CT scan [Figure 4] of the patient revealed osteolytic destruction of the maxilla on both sides of the midline.
Figure 1.
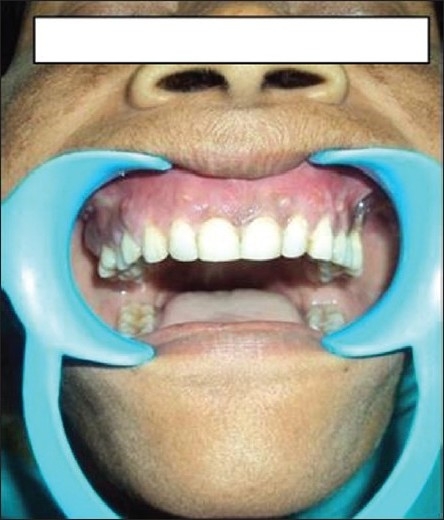
Multiple pus discharging sinuses
Figure 2.
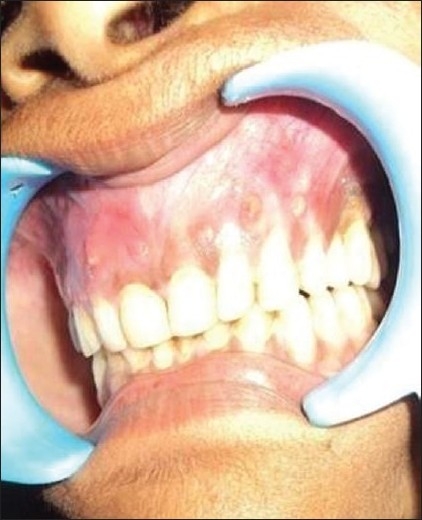
Exposed bone
Figure 3.
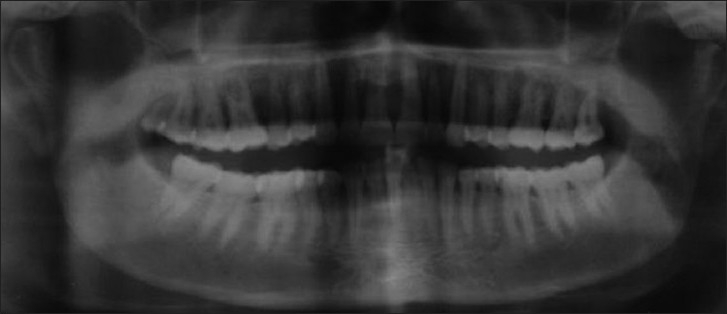
Preoperative OPG
Figure 4.
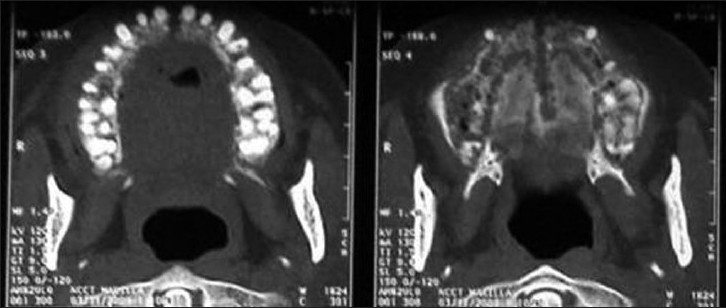
Preoperative CT scan
The provisional diagnosis was actinomycotic osteomyelitis of the maxilla with spontaneous sequestration. An incisional biopsy and a culture and sensitivity test were performed under local anesthesia, after getting the blood examination done and under antibiotic coverage (amox + clav and metrogyl). The exposed sequestrum was removed and histopathologic diagnosis was chronic suppurative osteomyelitis. Culture showed the growth of Staphylococcus organisms. Since it was a suppurative lesion and was associated with sinus formation, the patient was kept on antibiotic coverage for 2 weeks, which drastically improved the condition [Figure 5].
Figure 5.

After administering a course of antibiotic
But since the condition was osteomyelitis, surgery was planned under general anesthesia with endotracheal intubation to remove the lesion totally as the final treatment. After anesthetizing the patient, ideal part preparation was done both intraorally and extraorally and the patient was draped with sterile drapes. Local anesthetic agent was infiltrated and crevicular incision was given on both buccal and palatal aspects. The flap was reflected [Figure 6]. Sequestrectomy and curettage was performed along with total extraction of the maxillary teeth and maxillary alveolectomy. Hemostasis was achieved and closure was done with suction drain [Figure 7]. The postoperative period was uneventful. Patient was kept under antibiotic coverage. Regular irrigation with betadine was being performed on a daily basis and drain was removed on 4th postoperative day and suture was removed on 8th postoperative day. The excision biopsy report confirmed the lesion to be chronic suppurative osteomyelitis of maxilla, which is obviously a rare condition. The healing was uneventful [Figure 8] and prosthetic rehabilitation was done with removable maxillary complete denture. The patient is under regular follow-up [Figure 9].
Figure 6.
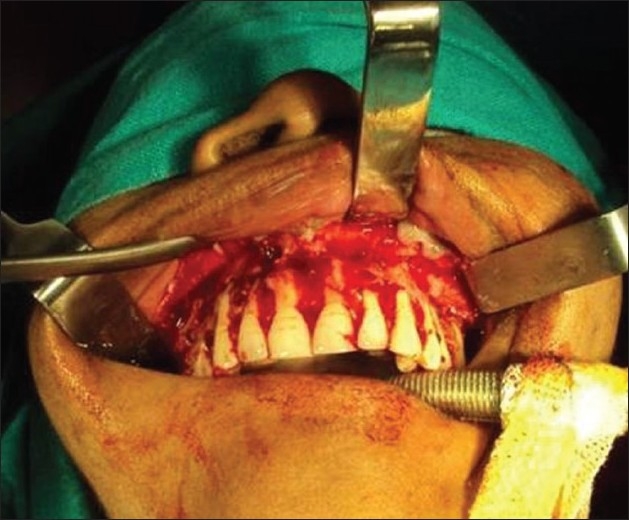
Intraoperative – Flap elevation and exposure of the lesion
Figure 7.
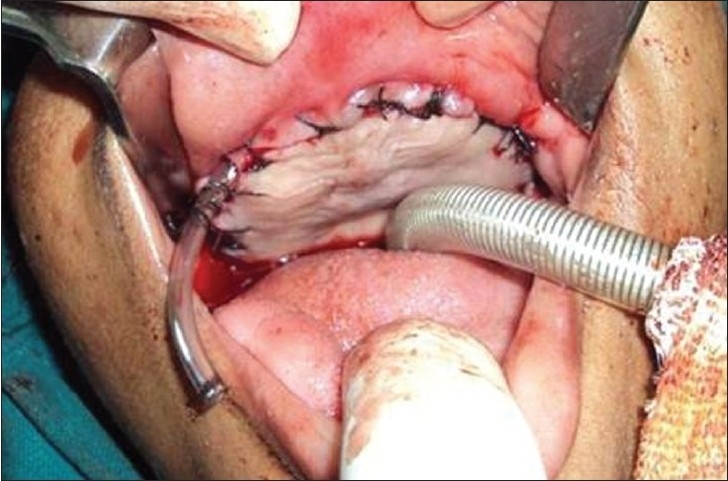
Closure with suction drain
Figure 8.

Postoperative healing
Figure 9.

Prosthetic rehabilitation
DISCUSSION
Osteomyelitis is a disease which is heterogeneous in its pathophysiology, clinical presentation and management. It is considered to be one of the most difficult-to-treat infectious diseases. Progressive bony destruction and the formation of sequestra are hallmarks of osteomyelitis. Osteomyelitis can result from hematogenous seeding, contiguous spread of infection, or direct inoculation of microorganism(s) into intact bone.[6]
Diminished host defenses, both local and systemic, can contribute significantly to the emergence and clinical course of the disease. Osteomyelitis has been associated with multiple systemic disease including diabetes, autoimmune status, malignancies, malnutrition and acquired immunodeficiency syndrome.[7] The medications linked to osteomyelitis are steroids, chemotherapeutic agents and bisphosphonates,[7,8] whereas in our case the patient was absolutely free of the above-mentioned conditions and the source of infection seemed to be rather of periodontal origin.
Infection of the maxilla can cause serious complications for the patient such as infection of cranial cavity and brain. Thus, it is essential that any maxillary osteomyelitis be treated aggressively by the surgeon to avoid subsequent dreaded consequences.
The clinical presentation of multiple pus discharging sinuses were typical of actinomycotic infection, which was ruled only out after culture of the pus sample. The actinomycotic infection forms external sinuses that discharge distinctive sulfur granules and spreads unimpeded by anatomical barriers.[4] Nearly every structure and space of the head and neck may be the initial site of involvement.[9]
Despite important medical and surgical advances in the management of patients with osteomyelitis, this disease remains extremely difficult to treat. The relapse rate can be as high as 20%. The usual goal of therapy is the eradication of the infection and restoration of function. Treatment of established osteomyelitis requires aggressive surgical debridement and prolonged antimicrobial therapy in the majority of cases.[6] Cohen et al,[10] successfully used the combination of antibiotic therapy and surgery when treating a patient with chronic jaw osteomyelitis The authors administered vancomycin and surgical debridement was performed until the underlying bone started bleeding. Antibiotic therapy was administered for an additional month and the lesion was cured. Chronic osteomyelitis is usually treated by the combination of antibiotic therapy and surgical debridement of the lesion.[11]
CONCLUSION
Adult osteomyelitis remains difficult to treat, with considerable morbidity and costs to the health care system. Osteomyelitis is now such a rare entity that when presented, the maxillofacial surgeon should consider the possibility underlying pathology and investigate appropriately. The term “cure” is not used for osteomyelitis because the infection may recur years after apparent successful treatment of the disease, if the patient suffers new trauma to the involved area, or the host response to the infection is suppressed. The goal of treatment is to arrest osteomyelitis, rather than achieve cure and so the patient is being followed up till date with no signs of recurrence.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
REFERENCES
- 1.Moose SM, Marshall KJ. In: Textbook of oral and maxillofacial surgery. Kruger GO, editor. St. Louis: CV Mosby; 1979. pp. 204–7. [Google Scholar]
- 2.Sivapathasundharam B. Shafer's Textbook of oral pathology. 6th ed. Noida: Elsevier; 2009. p. 492. [Google Scholar]
- 3.Mccash CR, Rowe NL. Acute osteomyelitis of maxilla in infancy. J Bone Joint Surg Br. 1953;35:22–32. doi: 10.1302/0301-620X.35B1.22. [DOI] [PubMed] [Google Scholar]
- 4.Topazian RG. Oral and maxillofacial infections. 4th ed. Philadelphia, Pennsylvania: W. B. Saunders and Company; 2002. [Google Scholar]
- 5.Auluck A. Maxillary necrosis by mucormycosis: A case report and literature review. Med Oral Patol Oral Cir Bucal. 2007;12:E360–4. [PubMed] [Google Scholar]
- 6.Sia IG, Berbari EF. Infection and musculoskeletal conditions: Osteomyelitis. Best Pract Res Clin Rheumatol. 2006;20:1065–81. doi: 10.1016/j.berh.2006.08.014. [DOI] [PubMed] [Google Scholar]
- 7.Marx RE. Chronic osteomyelitis of the jaws. Oral Maxillofac Clin North Am. 1991;3:367–81. [Google Scholar]
- 8.Marx RE. Pamidronate and zoledronate induced avascular bone necrosis. J Oral Maxillofac Surg. 2003;61:1115–8. doi: 10.1016/s0278-2391(03)00720-1. [DOI] [PubMed] [Google Scholar]
- 9.Lerner PI. The lumpy jaw.Cervicofacial actinomycosis. Infect Dis Clin North Am. 1988;2:203–20. [PubMed] [Google Scholar]
- 10.Cohen MA, Embil JM, Canosa T. Osteomyelitis of the maxilla caused by methicillin-resistant Staphylococcus aureus. J Oral Maxillofac Surg. 2003;61:387–90. doi: 10.1053/joms.2003.50076. [DOI] [PubMed] [Google Scholar]
- 11.Harvey BR, Ephros H, Defalco RJ. Tetracycline bone labeling in surgical management of chronic osteomyelitis: A case report. J Oral Maxillofac Surg. 2004;62:752–4. doi: 10.1016/j.joms.2003.08.036. [DOI] [PubMed] [Google Scholar]


